NPB101 Renal Physiology
1/121
Earn XP
Description and Tags
NPB101 Hamada SQ2025
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
122 Terms
Where does urine in the human body come from?
The blood
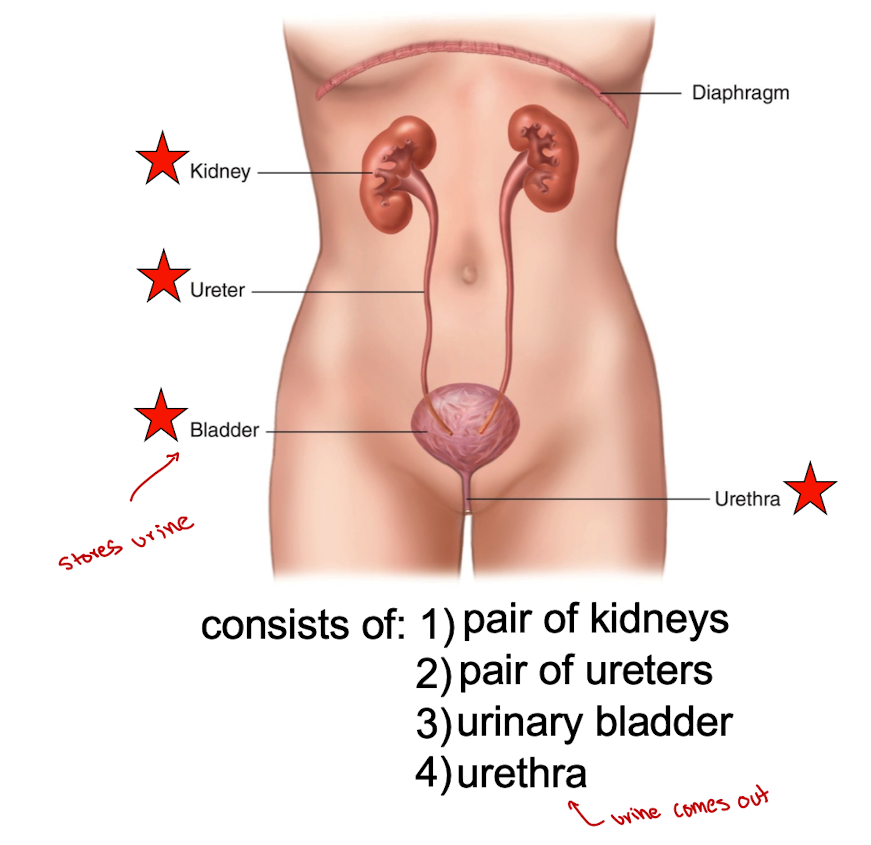
What does the urinary system consist of?
pair of kidneys
pair of ureters
urinary bladder
urethra
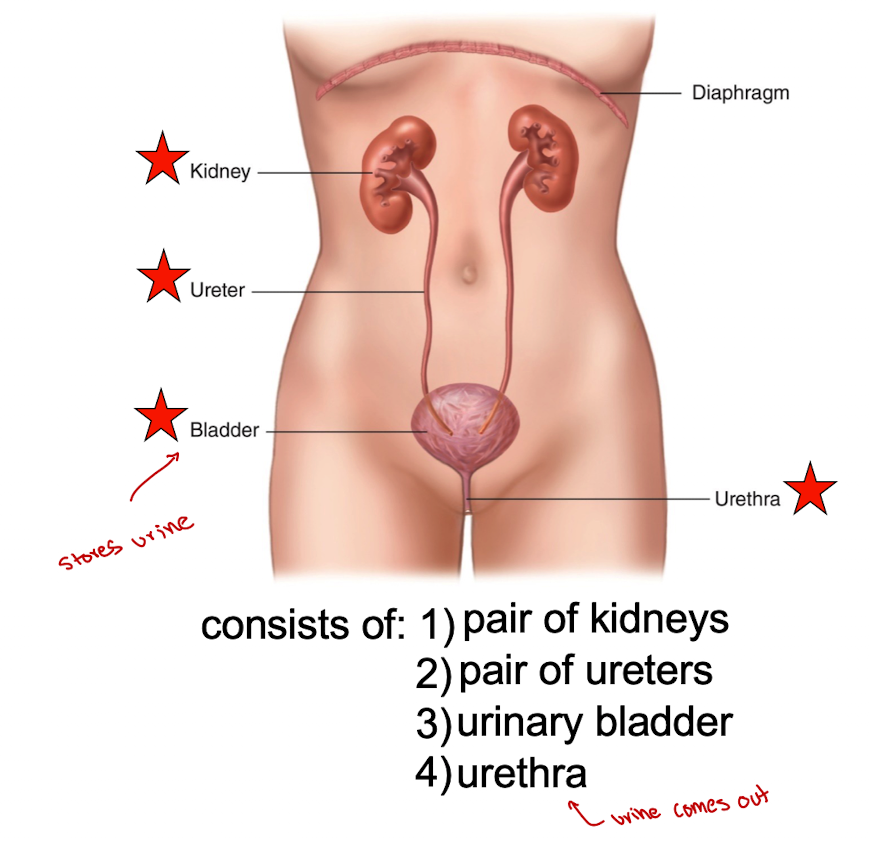
Ureters
Transport urine from kidneys to bladder
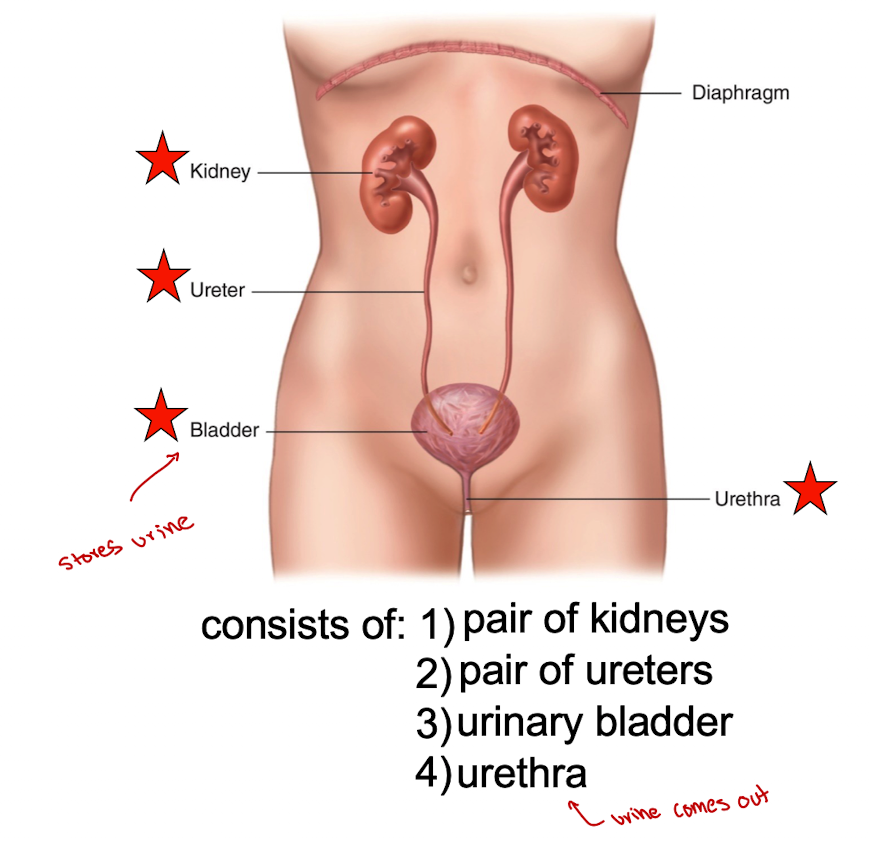
Bladder
stores urine until voided from body
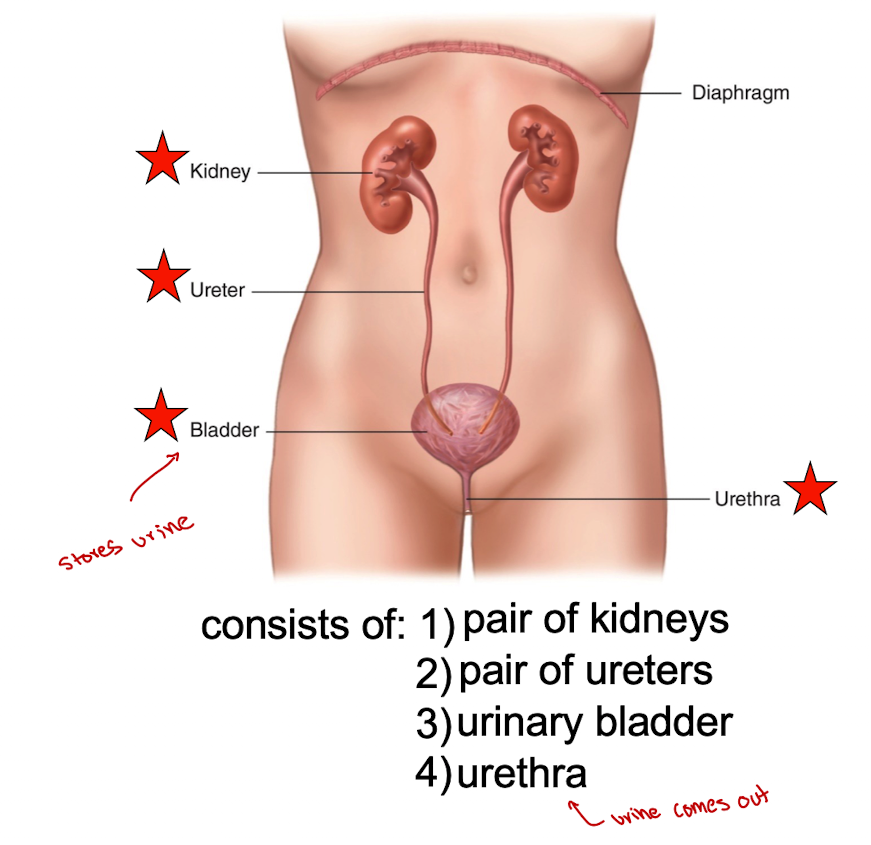
Urethra
carries urine from bladder to the outside of the body
Blood enters and exits the kidneys
enters the kidneys via the renal artery (connected to the aorta)
exits the kidneys via the renal vein (connected to the inferior vena cava)
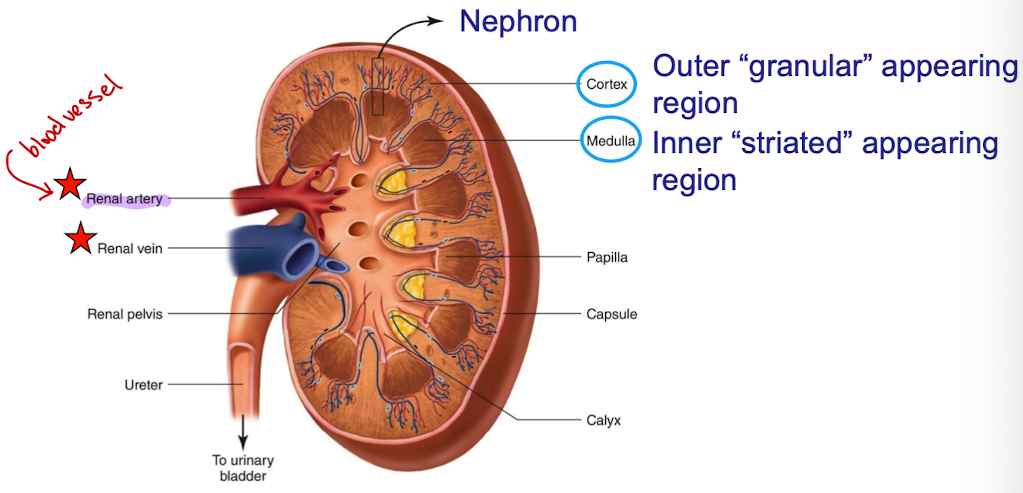
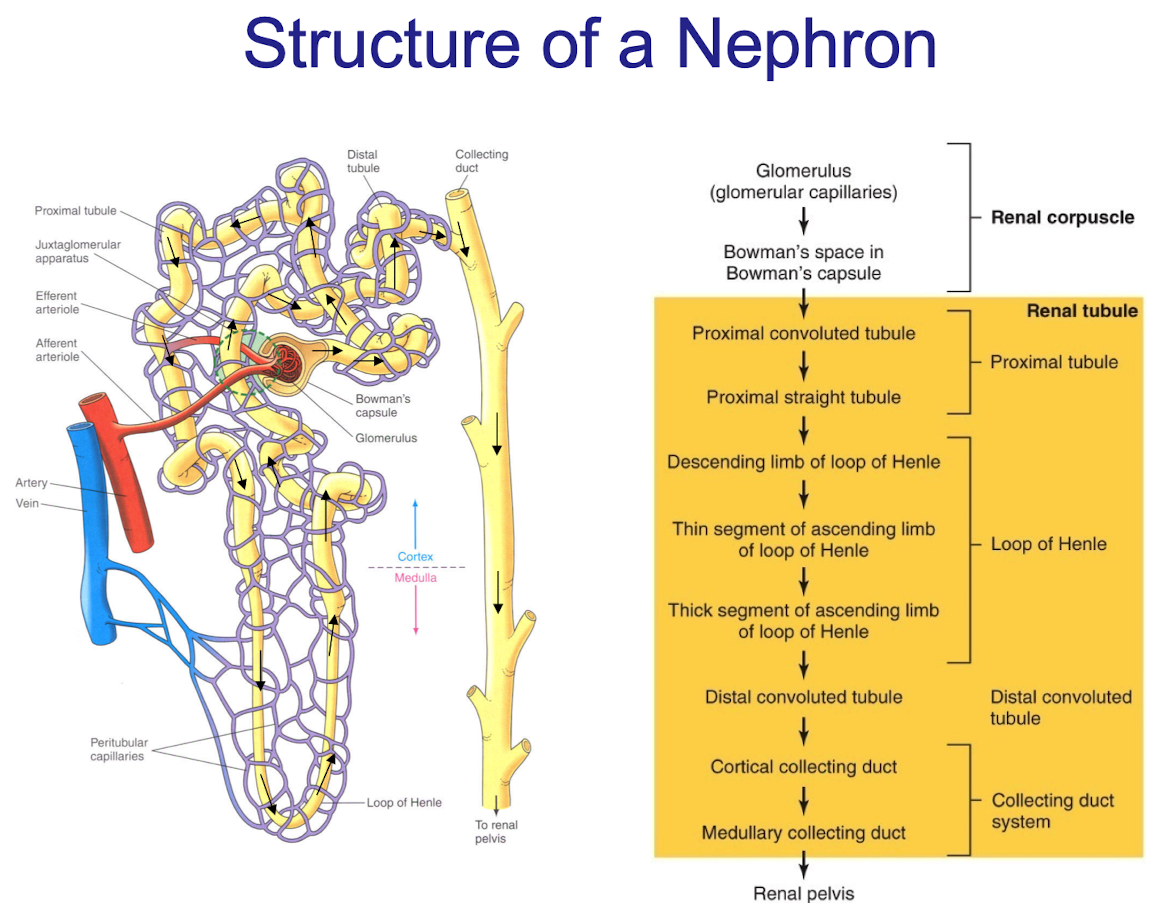
Nephrons, what are they and what they consist of
structural and functional units of the kidney (functional unit is the smallest unit capable of performing all of the tasks of an organ)
Each kidney has over 1 million of these units
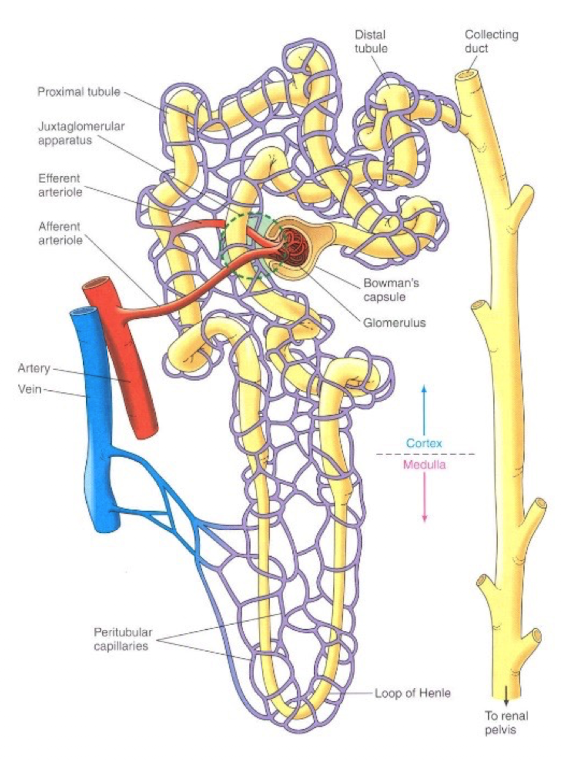
Each nephron consists of a renal corpuscle, which contains the glomerulus (which is a tuft of capillaries) and a renal tubule
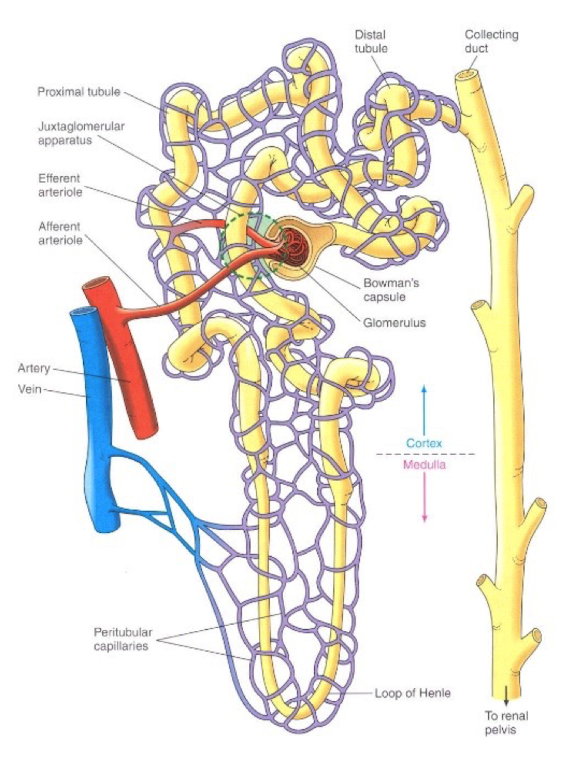
Bowman’s capsule
the tubule forms a cup shape around the glomerulus called the glomerular capsule. Filters glucose, urea, NaCl, but NOT blood cells or proteins
How is urine produced?
Glomerulus (glomerular capillaries)
Bowman’s space in Bowman’s capsule
Proximal convoluted tubule
Proximal straight tubule
descending limb of loop of Henle
Thin segment of ascending limb of loop of Henle
Distal convoluted tubule
cortical collecting duct
medullary collecting duct
renal pelvis
_% of the plasma that enters the glomerulus is not filtered and leaves through the efferent arteriole
80
_% of the plasma that enters the glomerulus is filtered
20
Approx __ liters of glomerular filtrate formed each (collectively)
180
Average plasma volume is ___ liters
2.75
The entire plasma volume is filtered by the kidneys about ___ times per day
65
Of the 180 liters of plasma filtered each day, ___ liters are reabsorbed
178.5
3 basic processes involved in the formation of urine
glomerular filtration (GF)
tubular reabsorption (TR)
tubular secretion (TS)
Glomerular filtration
non-discriminant filtration (except for red blood cells) of a protein-free plasma from the glomerulus into Bowman’s capsule (amount filtered)
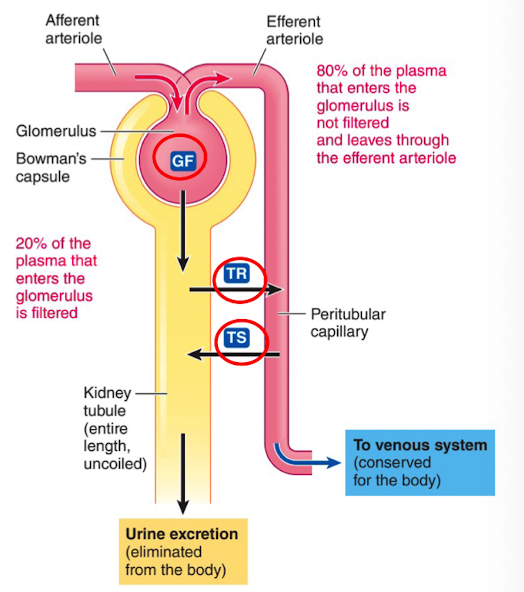
Tubular reabsorption
selective movement of filtered substances from the tubular lumen into the peritubular capillaries (amount reabsorbed)
Tubular secretion
selective movement of non filtered substances from the peritubular capillaries into the tubular lumen (amount secreted)
Amount Excreted Equation
Amount excreted = Amount filtered - Amount reabsorbed + Amount secreted
2 Capillaries in Renal Physiology
Glomerular
Peritubular
Glomerular Capillary
Specialized for filtration. These are the only capillaries in the body that are fed and drained by an arteriole (afferent and efferent)
Allows the blood pressure in the capillary bed to be very high and forces fluid and solute out of the blood into the glomerular capsule
Peritubular capillaries
Most of the filtrate is reabsorbed in the renal tubule cells and returns to the blood through the peritubular capillaries
Each nephron consists of 2 components
Vascular component
Tubular component
Vascular components
afferent arteriole
Glomerulus
Efferent arteriole
Peritubular capillaries
Tubular component
Bowmans capsule
Proximal tubule
Loop of Henle
Distal tubule and collecting duct
What is a more efficient filter in the kidney ?
Glomeruli due to membrane having a large surface area and very permeable to water and solutes
What factors are NOT filtrated at the Bowman’s capsule?
Protein
Blood cells
Glucose
Urea
NaCl
Protein
Blood Cells
Where does glucose go after its filtered at the bowman’s capsule
reabsorbed at proximal tubule
Where does urea go after its filtered at the bowman’s capsule
partially reabsorbed at proximal tunnel and collecting duct
Where does NaCl go after its filtered at the bowman’s capsule
reabsorbed at proximal tubule, loop of Henle and distal tubule
What do glomerular capillaries allow blood pressure in the capillary bed do?
Allows it to be very high and forces fluid and solute out of the blood into the glomerular capsule
What is a common finding when there is a problem with the filtration membrane?
Blood cells or protein in the urine (protinuria) which is common in diabetes and hypertension
3 forces involved in glomerular filtration
glomerular capillary blood pressure
plasma-colloid osmotic pressure
bowman’s capsule hydrostatic pressure
Glomerular capillary blood pressure
the fluid pressure within the glomerular capillaries.
Favors filtration
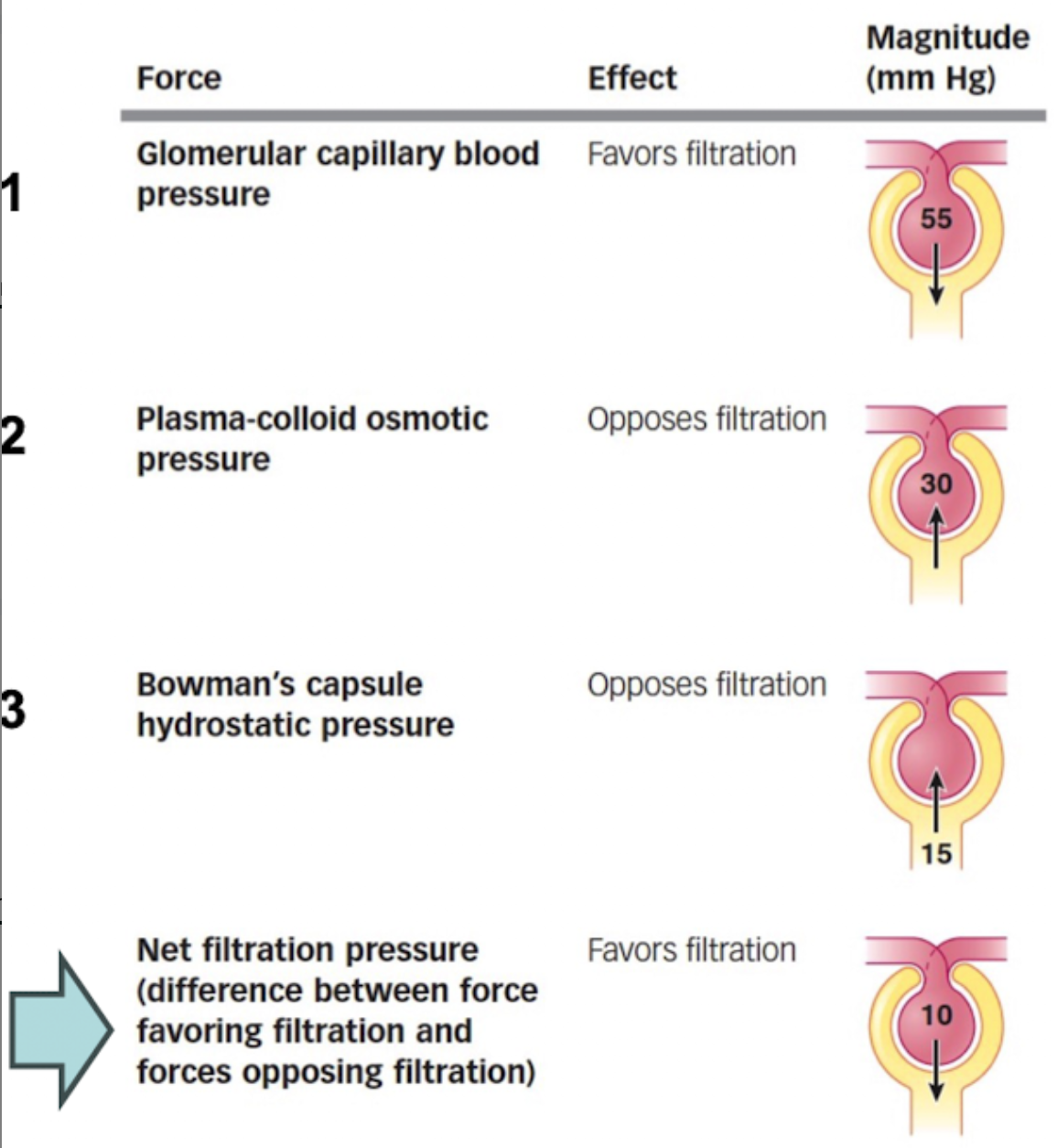
Plasma-colloid osmotic pressure
caused by unequal distribution of protein btwn plasma (contains proteins) and glomerular filtrate (no protein). H2O wants to move down osmotic gradient into glomerulus.
Opposes filtration
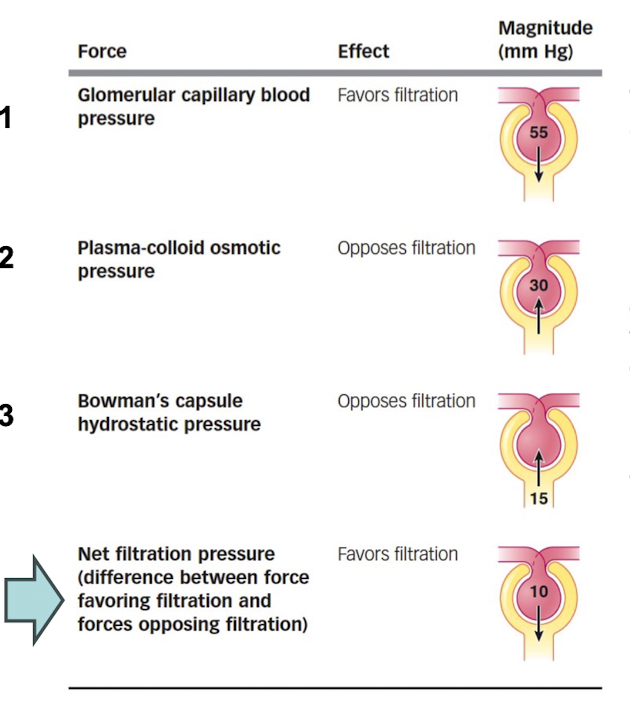
Bowman’s capsule hydrostatic pressure
The fluid pressure by the filtrate in Bowman’s capsule.
Opposes filtration
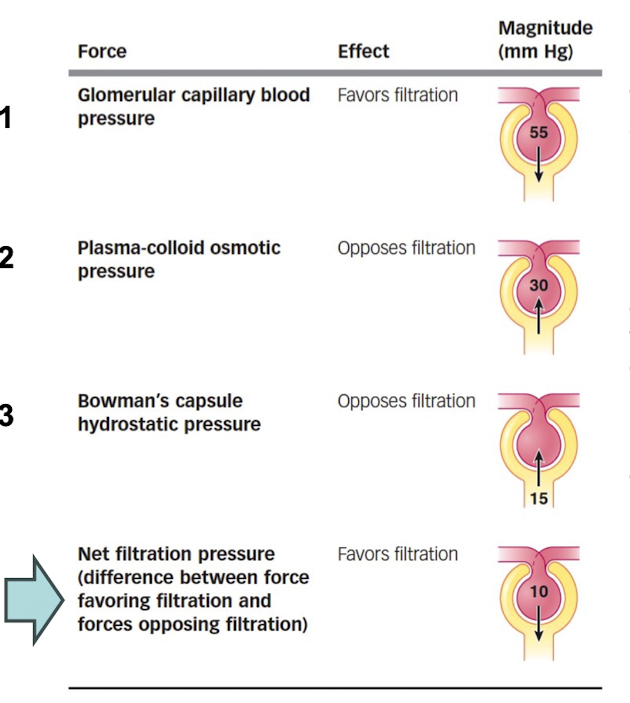
What is the major force that causes glomerular filtration?
Glomerular capillary blood pressure
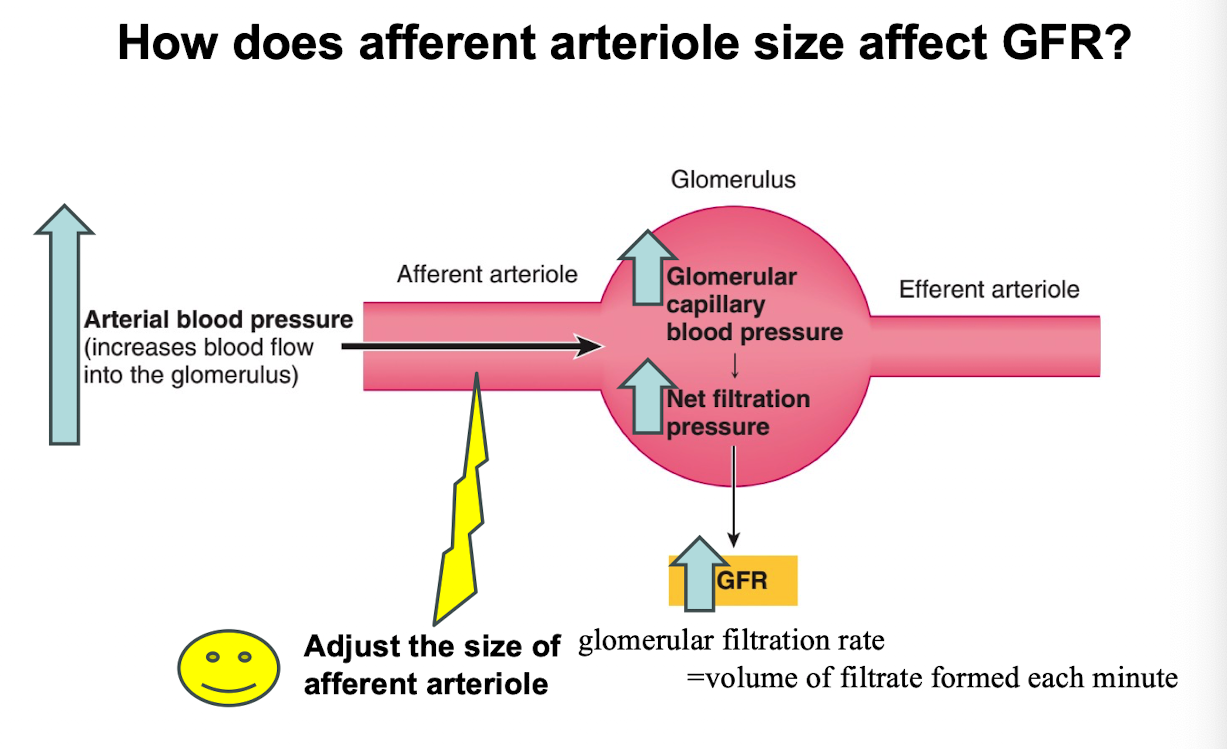
What is the glomerular filtration rate (GFR)
Volume of filtrate formed each minute
What is GFR affected by?
The volume of surface available, filtration membrane permeability and net filtration (NFP), blood pressure/blood flow to the glomerular capillaries
What is GFR directly proportional to?
To the NFP (net filtration pressure). Increases in systemic blood pressure mean increases in GFR
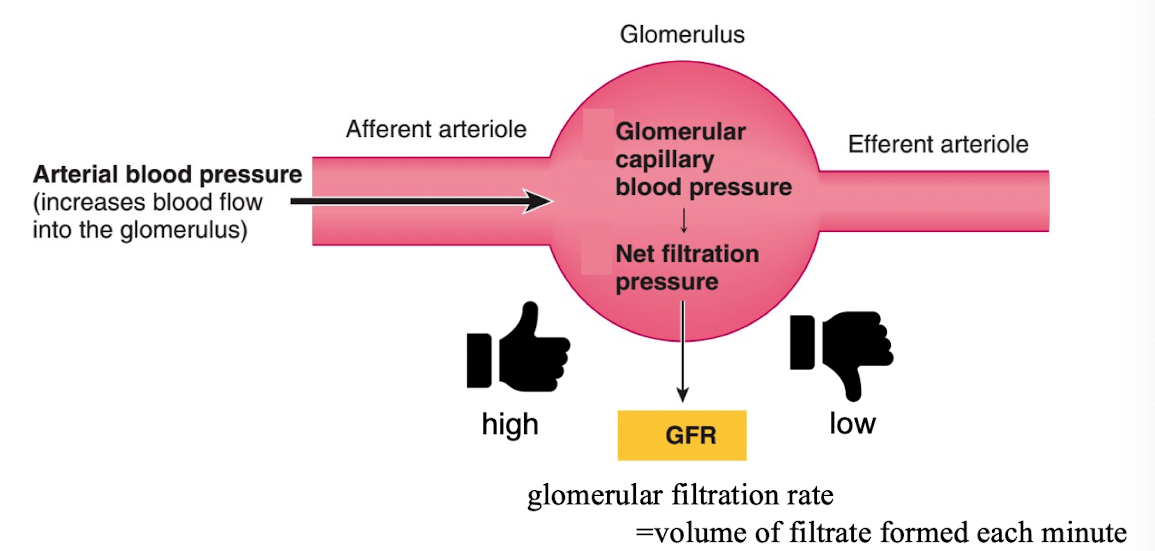
If blood pressure is elevated, is the GFR high or low?
high, changes in GFR. result mainly from changes in glomerular capillary blood pressure
How can the kidney adjust blood flow to maintain stable filtration?
Adjust the size of afferent artieole
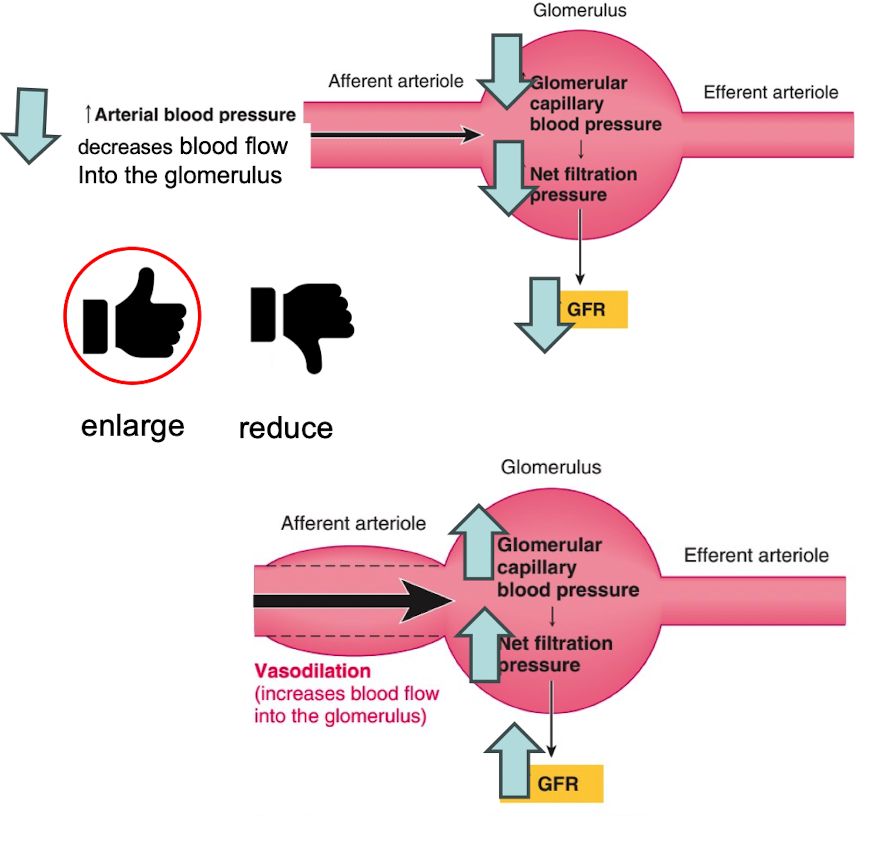
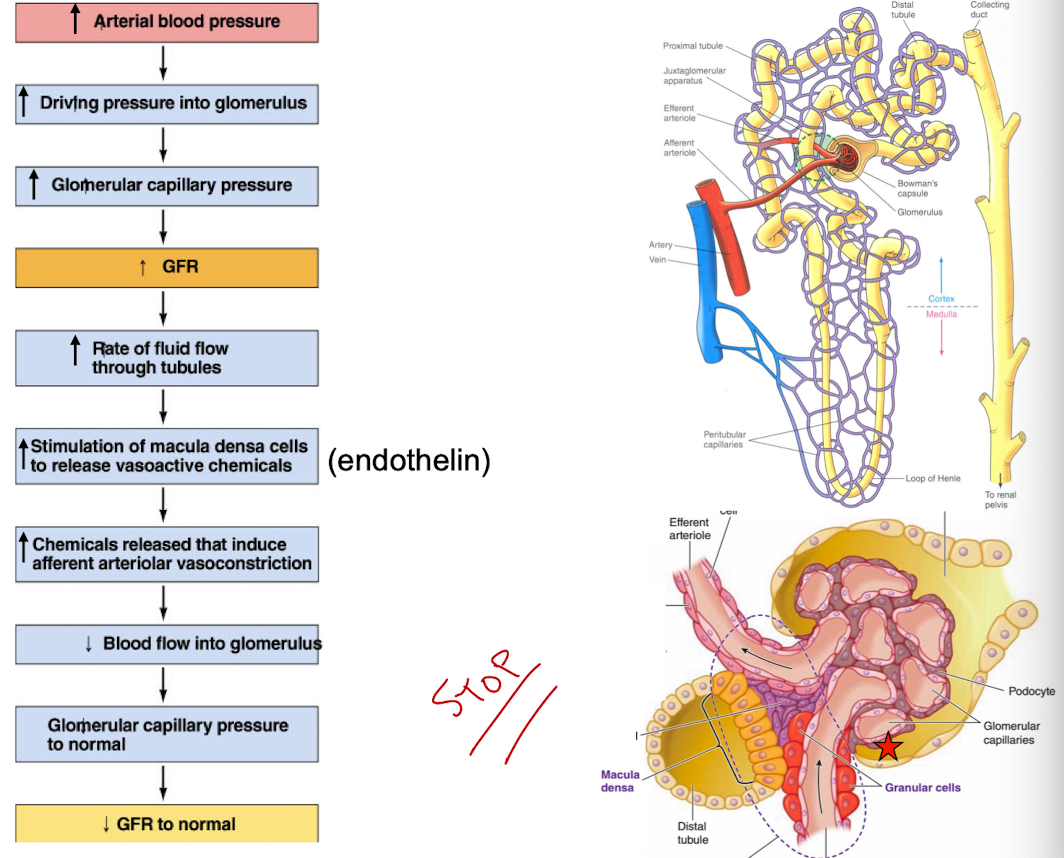
If GFR increases bc of a rise in arterial pressure, then…
reduces due to vasoconstriction (decreases blood flow into the glomerulus)
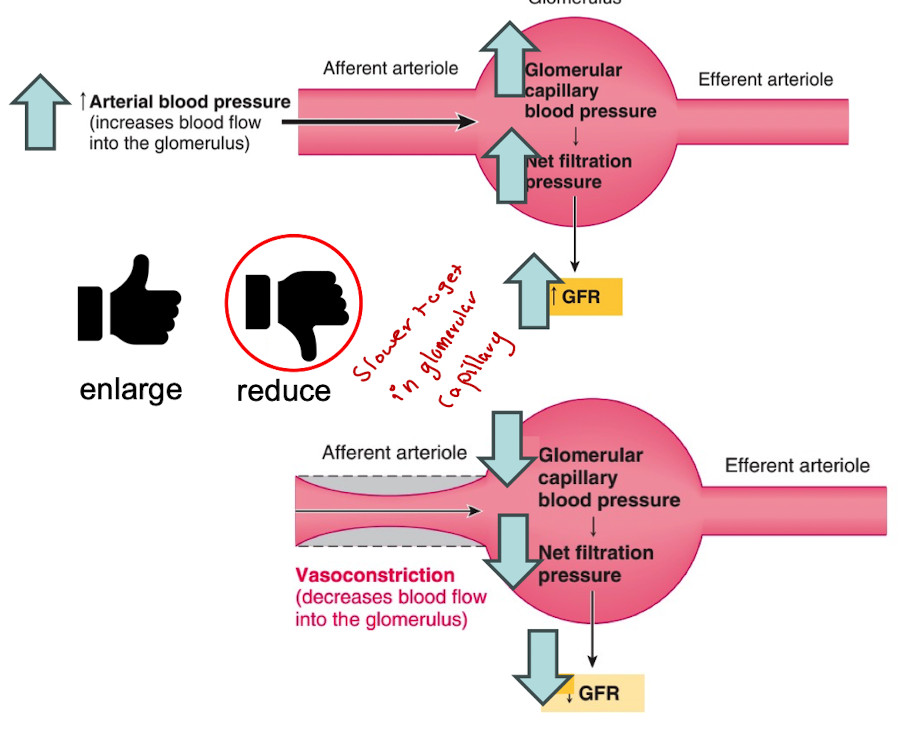
If GFR decreases bc of a fall in arterial pressure, then …
enlarge due to vasodilation (increases blood flow into the glomerulus)
what are the 2 mechanisms that keep GFR stable
autoregulation (intrinsic control)
sympathetic control (extrinsic control/uses nervous system)
Both work by changing caliber and resistance of afferent arterioles
Autoregulation of GFR
helps maintain a constant blood flow into the glomerular capillaries
done by changing the caliber of the afferent arterioles
2 mechanisms of GFR autoregulation
Myogenic mechanism
Tubuloglomerular feedback mechanism
Myogenic mechanism
a common property of vascular smooth muscle is to contract automatically in response to increased stretch and to relax in response to decreased stretch
tubuloglomerular feedback mechanism
allows the tubule of a nephron to monitor the rate of fluid movement and make adjustments to GFR to maintain appropriate flow
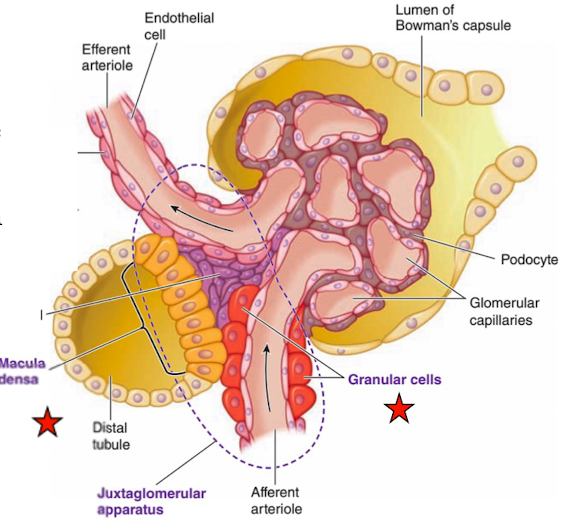
Juxtaglomerular apparatus
region near the glomerulus where the tubule passes through the fork formed by the afferent and efferent arterioles
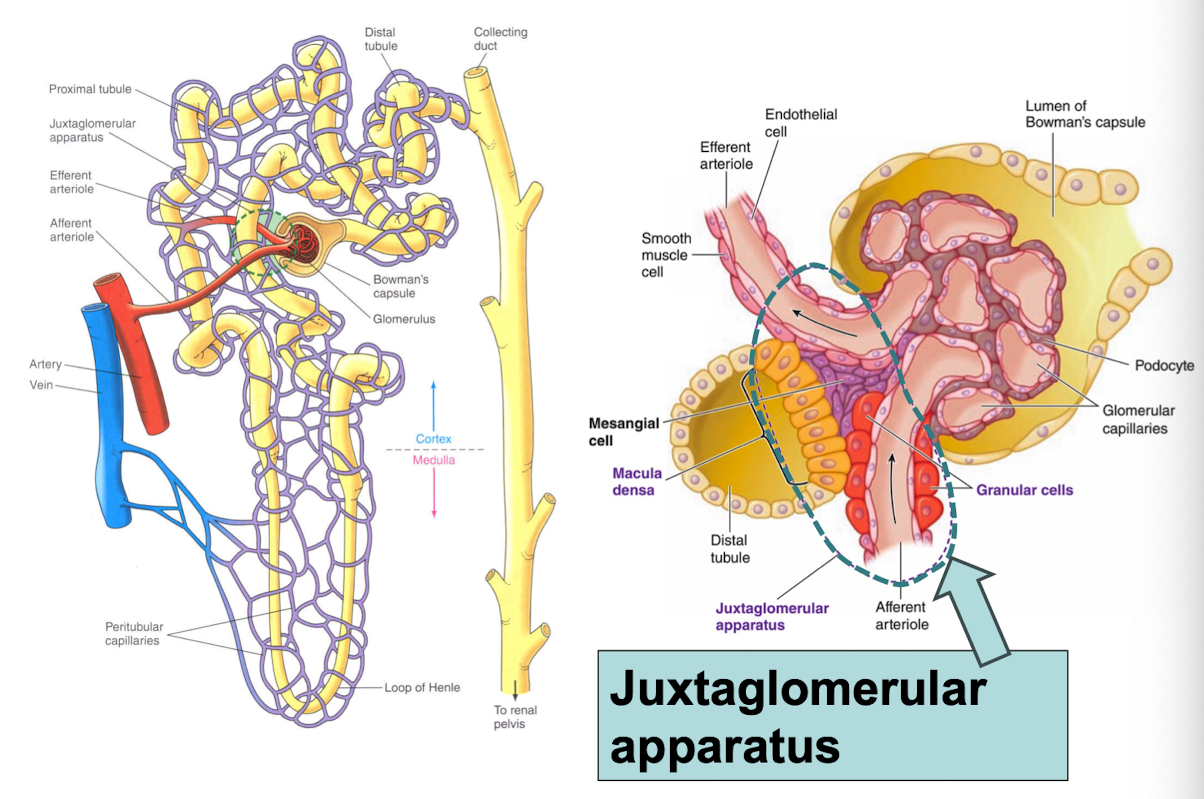
Tubuloglomerular feedback mechanism
involves the juxtaglomerular apparatus
allows the tubule of a nephron to monitor the rate of fluid movement and make adjustments to GFR to maintain appropriate flow
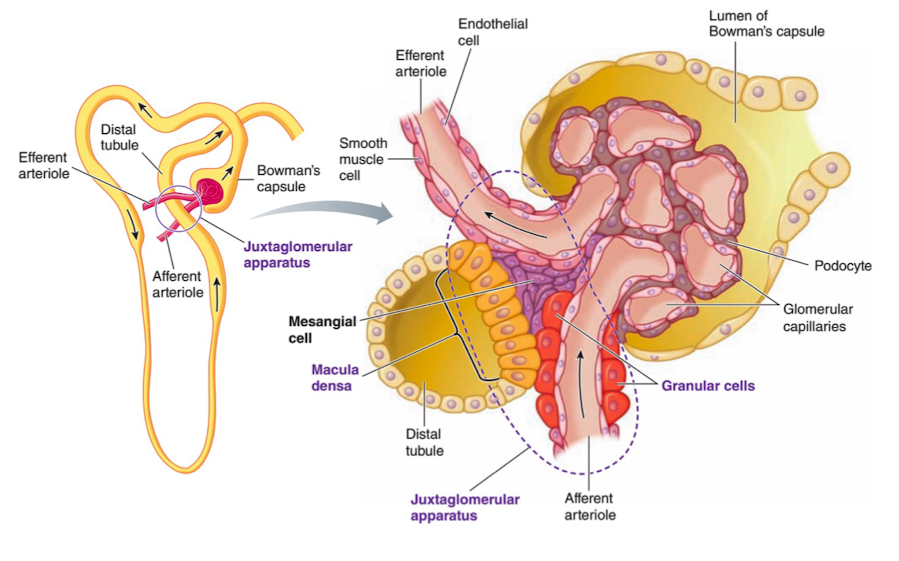
juxtaglomerular (granular) cells
enlarged smooth muscle cells that have secretory granules which contain the hormone renin
mechanoreceptors (sense blood pressure) in the afferent arteriole
Macula densa cells
group of tall, closely-packed cells that are adjacent to the granular JG cells
chemoreceptors that respond to changes in the NaCl content of the filtrate
detect changes in rate fluid is flowing and release
local acting vasoactive chemical
Glomerular Filtration
autoregulation via juxtaglomerular apparatus
What is the primary purpose of renal autoregulation?
a. To increase urine output during physical activity
b. To maintain a stable glomerular filtration rate (GFR) despite flunctatavions in blood pressure
c. To temporarily halt kidney function during periods of stress
d. To enhance blood supply to the bladder
B. To maintain a stable glomerular filtration rate (GFR) despite fluctuations in blood pressure
When blood pressure increases, how does the kidney auto regulate to maintain a stable glomerular filtration (GFR)?
a. The afferent arteriole dilates to increase blood flow
b. The afferent arteriole constricts to decrease blood flow
c. The efferent arteriole constricts to increase glomerular pressure
d. The glomerulus collapses to stop filtration
B. The afferent arteriole constricts to decrease blood flow
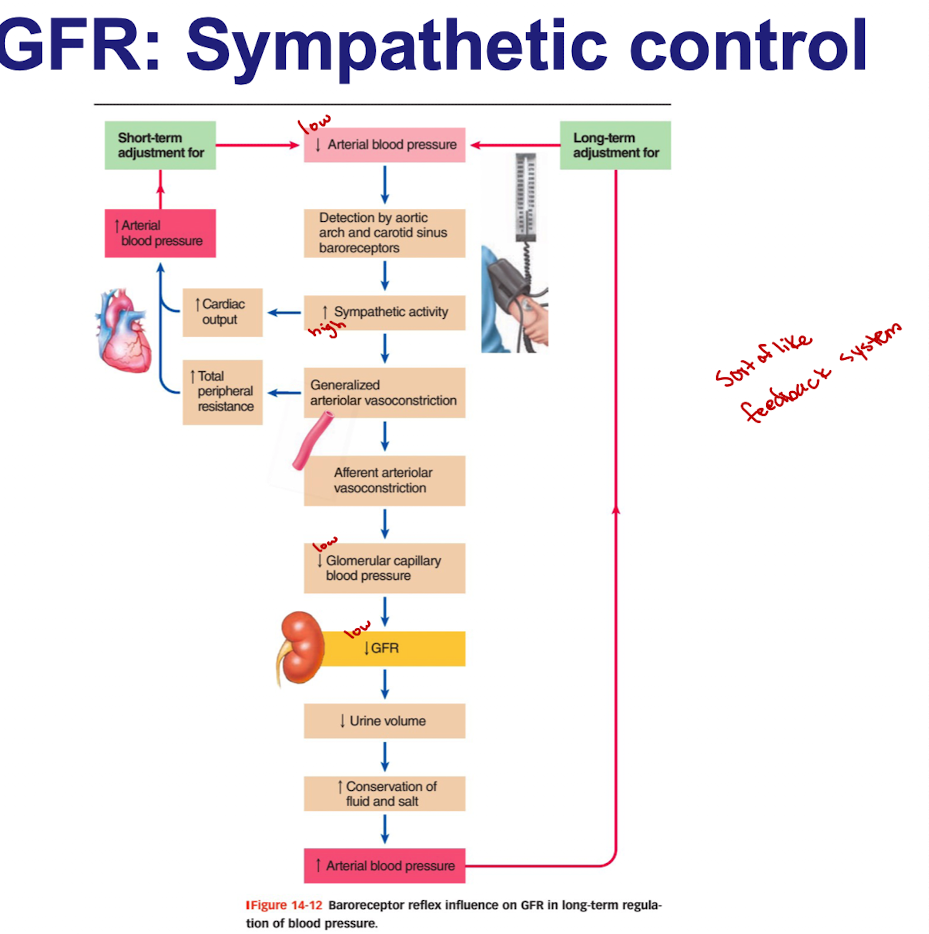
Baroreceptor reflex function (GFR: Sympathetic Control)
arterial carotid sinus and aortic arch baroreceptors detect rises and falls in arterial blood pressure
Sends signals to cardiovascular control center in brainstem which then adjusts levels of sympathetic activity
uses nervous system
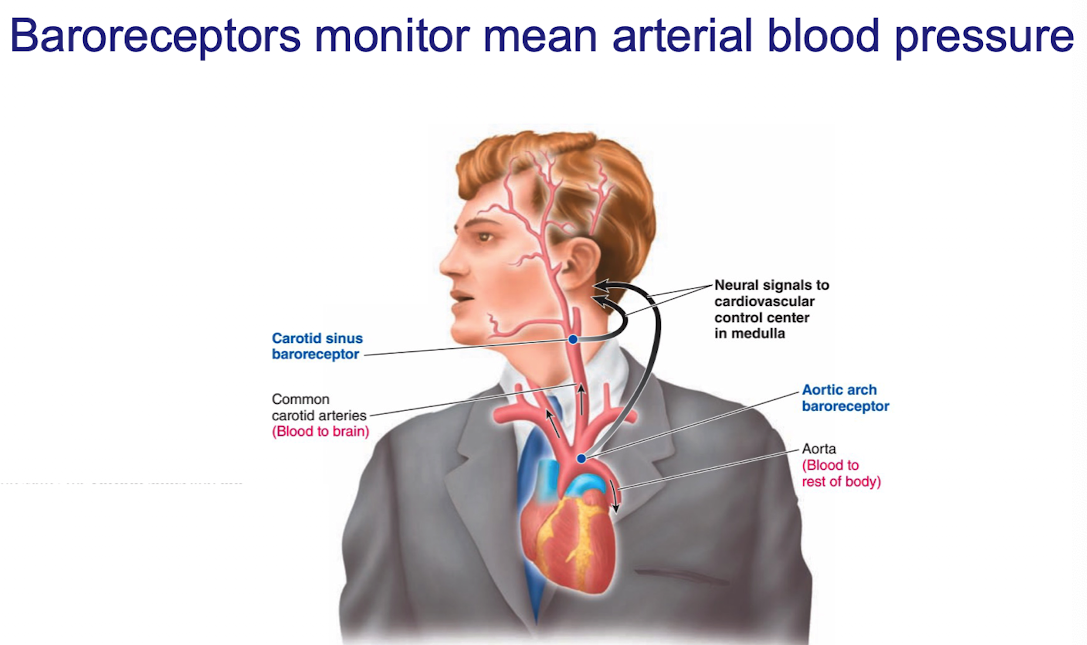
Sympathetic control Baroreceptor reflex example
If the plasma volume decreases bc of hemorrhage
baroreceptors detect drop in blood pressure
cardiovascular control center coordinates an increase in sympathetic activity
sympathetic activity not only increases cardiac output and total peripheral resistance but also decreases GFR (to maintain plasma volume by constricting afferent arterioles)
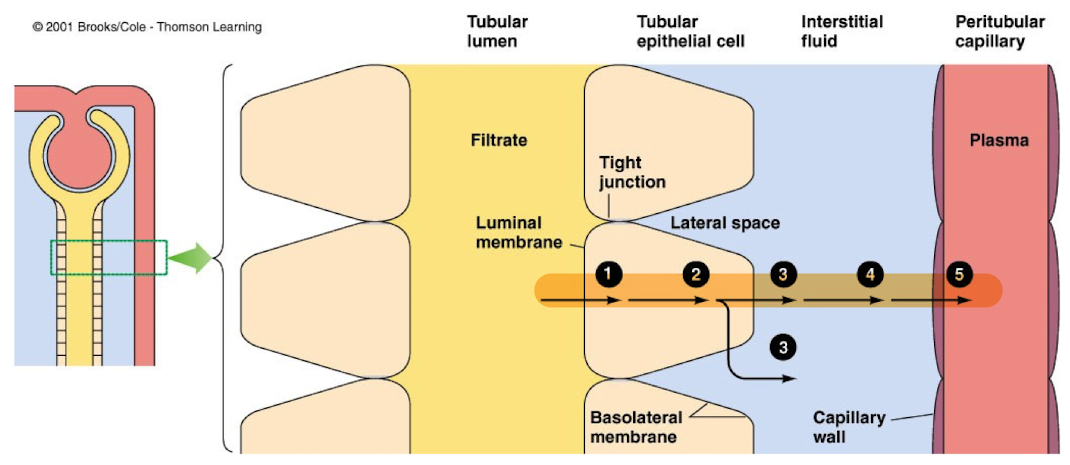
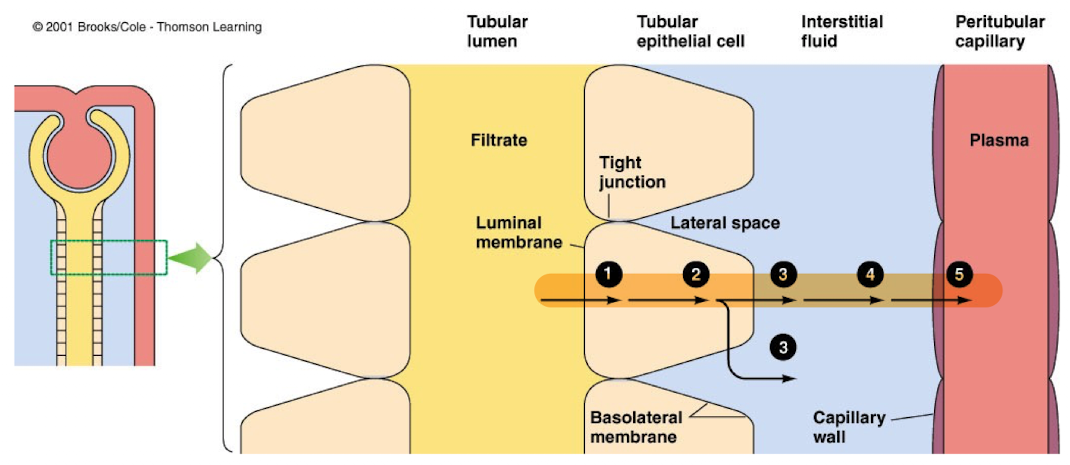
Transepithelial transport, how big and what do they contain
Throughout its entire length, tubule is one cell-layer thick
Tubular epithelial cells have a luminal membrane and a basolateral membrane. Adjacent tubular cells form tight junctions
Interstitial fluid fills the gaps (lateral spaces) btwn epithelial cells.
Except for water, materials must pass through the cells to leave tubular lumen and enter the blood
Extracellular fluid (ECF)
80% interstitial fluid
20% plasma
Five steps that requires a substance cross 5 barriers for trans-epithelial transport
The luminal membrane of the tubular cell
the cytosol of the tubular cell
the basolateral membrane of the tubular cell
the interstitial fluid
the capillary wall
Two type of tubular reabsorption
passive reabsorption
active reabsorption (requires energy)
Passive reabsorption
movement down an osmotic or electrochemical gradient
Active reabsorption (requires energy)
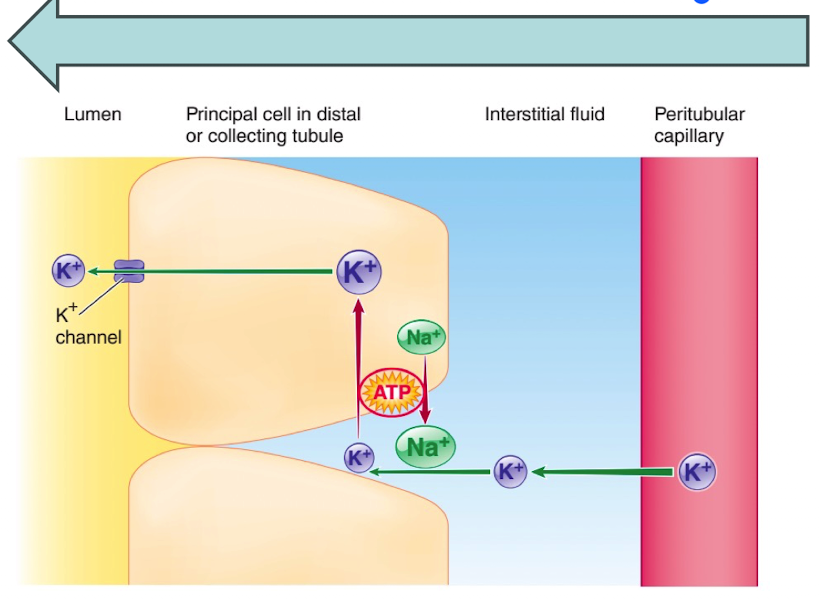
active step in Na+ reabsorption involves the energy-dependent Na+/K+ ATPase carrier located in the tubular cell’s basolateral membrane
includes glucose, amino acids, organic molecules, Na+ and other electrolytes
Na+ reabsorption
The intracellular concentration of Na+ is low (bc of the Na+/K+ ATPase), Na+ diffuses into the tubular cell down its concentration gradient
The interstitial concentration of Na+ is high (bc of the Na+/K+ ATPase), Na+ diffuses into the peritubular capillary down its conc. gradient
Where does reabsorption take place Na+?
Na+ reabsorption rate varies across the different location of the nephron; 99.5% of filtered Na+ is reabsorbed
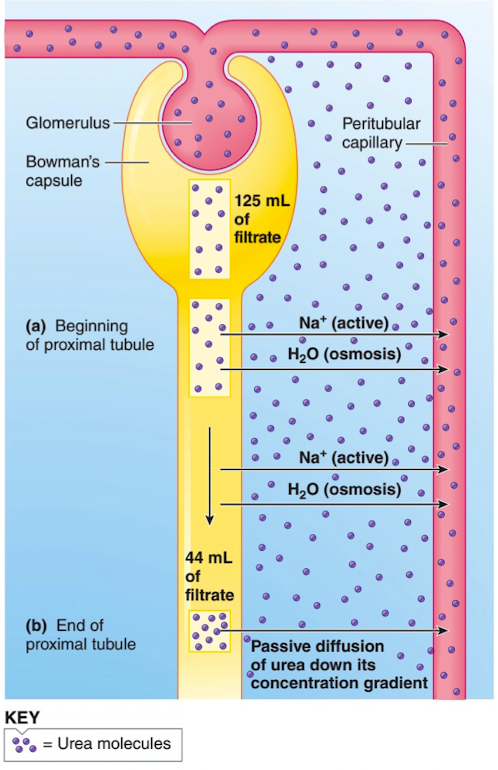
Proximal tubule Na+ reabsorbed
67% of filtered Na+ is reabsorbed, regardless of the amount of Na+ in the body fluids
reabsorption of glucose, amino acids, H2O, Cl- and urea
Loop of Henle Na+ reabsorbed
25% of filtered Na+ is reabsorbed, regardless of the amount of Na+ in the body fluids
H2O urine of varying conc and volumes
distal and collecting tubules Na+ reabsorbed
8% of filtered Na+ is reabsorbed, Na+ reabsorption subject to hormonal control, being important in the regulation of ECF volume
Distal and collecting tubules Hormonal control: Na+ reabsorption
aldosterone stimulates Na+ reabsorption
Atrial natriuretic peptide inhibits Na+ reabsorption
How does aldosterone increase Na+ reabsorption
In distal and collecting tubules by promoting the insertion of Na+ channels (luminal membranes) and Na+/K+ ATPase carriers (basolateral membranes)
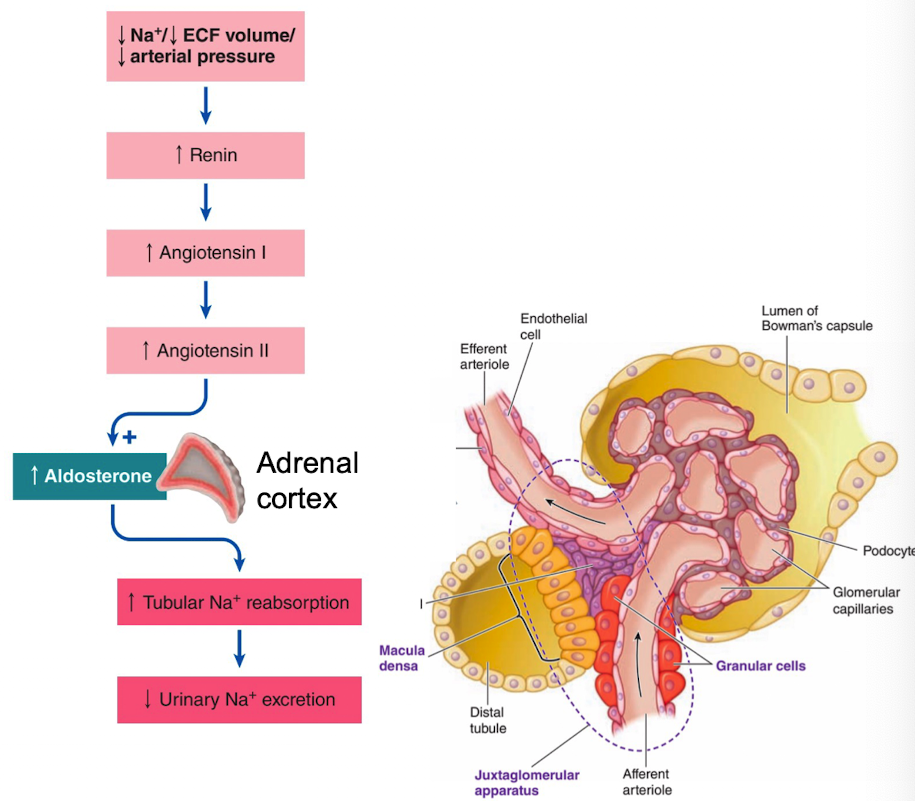
Angiotensinogen
synthesized in liver, always present in plasma
Renin
released from kidneys (granular cells) into plasma. Activates/converts angiotensinogen into angiotensin I
Angiotensin-converting enzyme (ACE)
enzyme present in the lungs that converts angiotensin I into angiotensin II
Angiotensin II
has many effects (stimulates vasopressin, thirst, arteriolar vasoconstriction). Also stimulates the adrenal cortex to release aldosterone
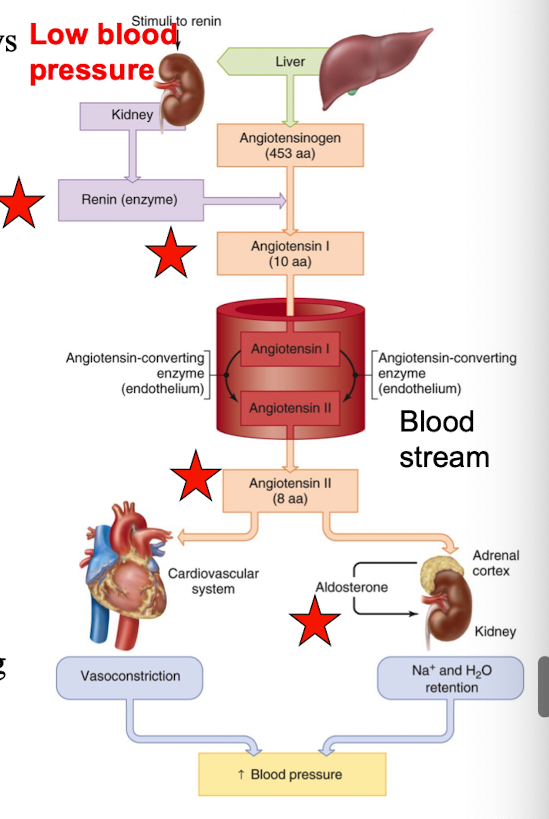
Renin-angiotensin-aldosterone system (RAAS)
Atrial Natriuretic peptide (ANP)
Hormone that serves to increase the excretion of Na+ in the urine
Specialized cardiac atrial cells produce and store ANP. ANP is released when they’re stretched due to expansion of the ECF volume
Actions of ANP: ___ Na+ reabsorption in the distal and collecting tubules
inhibit
Actions of ANP: ___ Renin secretion by the kidneys and aldosterone secretion from the adrenal cortex
inhibit
Actions of ANP: ___ smooth muscle of afferent arterioles (input to glomerulus). The leads to dilation of the afferent arterioles and an increase in the GFR
inhibit
Actions of ANP: ___ sympathetic nervous system, thereby decreasing cardiac output and total peripheral resistance
inhibit
Glucose and amino acids reabsorption
glucose and amino acids are reabsorbed in the proximal tube
Na+ is important role for the reabsorption
kidneys usually conserve all the glucose and protect against loss of the important nutrient in the urine
Active Na+ reabsorption
responsible for the passive reabsorption of Cl-, H2O, and urea
Chloride Reabsorption
Cl- ions are passively reabsorbed down the electrical gradient created by active reabsorption of Na+
Cl ions pass btwn (not through) tubular cells
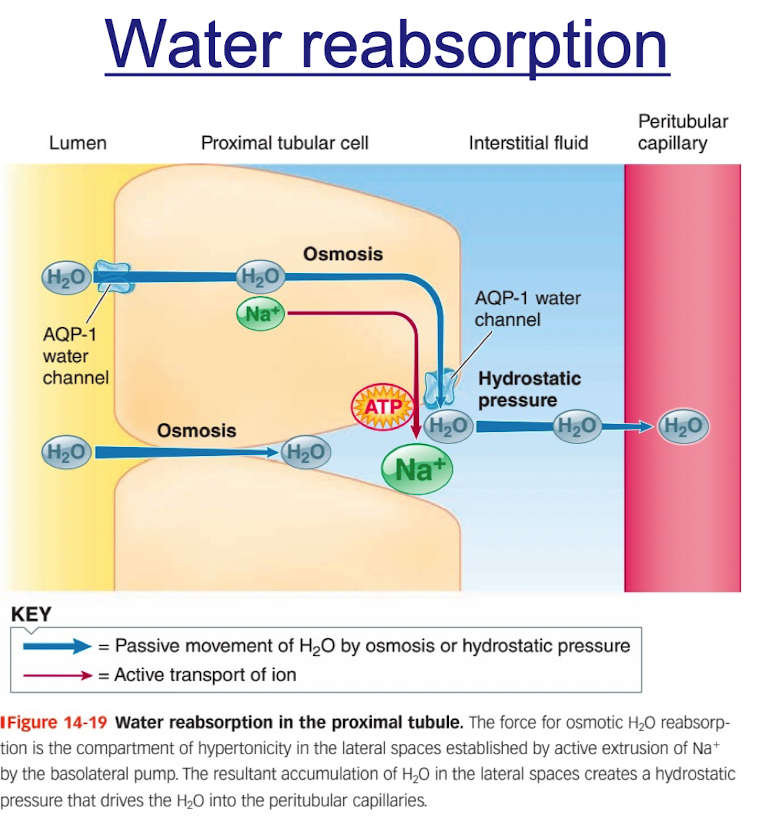
H2O Reabsorption
occurs passively by osmosis throughout the length of the tubule
80% is obligatory reabsorbed in the proximal tubules and loops of Henle; variable amounts of the remaining 20% are reabsorbed in the distal portions of the tubule (under hormonal control- vasopressin)
water channels “aquaporins” in the proximal tubule are always open; channels in the distal tubule are regulated by vasopressin
Urea Reabsorption
Indirectly linked to active Na+ reabsorption
Waste product from the breakdown of protein
Osmotically induced reabsorption of H2O in the proximal tubule secondary to active Na+ reabsorption produces a concentration gradient for urea that favors passive reabsorption of this waste
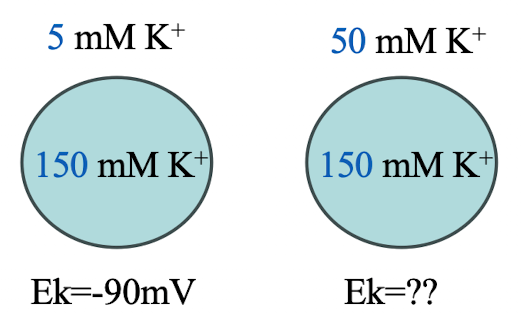
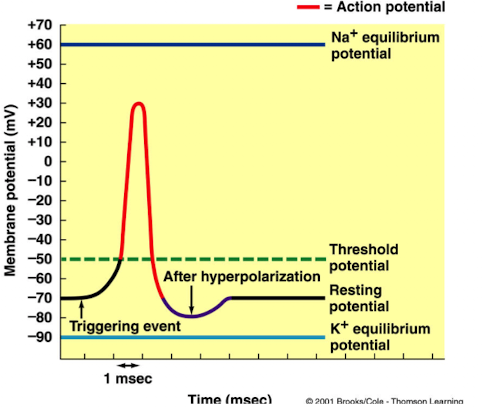
What happens to the cell’s equilibrium potential if the extracellular K+ concentration increases from 5 mM to 50 mM, while intracellular K+ remains at 150 mM?
Ek = -90mV (ECF: ICF = 5mM: 150mM)
1. The cell’s equilibrium potential is less polarized (less negative or closer to 0).
2. The cell’s equilibrium potential is more polarized (more negative or farther from 0).
3. Nothing changes
The cell’s equilibrium potential is less polarized (less negative or closer to 0)
What is tubular secretion an important mechanism for? (4)
disposing of drugs and drug metabolites
eliminating undesired substances or end products that have reabsorbed by passive processes (urea and uric acid)
removing excess K+
controlling blood pH
What are the most important substances secreted by the tubules in tubular secretion?
H+, K+, and organic anions, cations
Tubular Secretion: H+
the ability of the kidneys to secrete H+ is important for the acid-base balance of the body
extent of H+ secretion depends on the acidity of the body fluids (H+ con in the body fluids is too low → H+ secretion decreases)
H+ can be secreted by the proximal, distal, and collecting tubules
Tubular Secretion: K+ ions (where is it absorbed and secreted)
actively reabsorbed in the proximal tubule and actively secreted in the distal and collecting tubules
Tubular Secretion: K+ reabsorption (proximal tubule)
constant and unregulated; almost all filtered K+ is reabsorbed
Tubular Secretion: K+ Secretion (distal and collecting tubule)
subject to regulation; almost all K+ in the urine is K+ that was secreted
What happens if K+ levels are low?
K+ secretion in the distal portion of the nephron is reduced to a minimum
What happens if K+ are high?
K+ secretion in the distal portion of the nephron is increased
Nerst equation
equation describing the equilibrium potential for a particular ion
If the cell’s resting potential is moved towards threshold (depolarized), then…
the cell would be over excitable
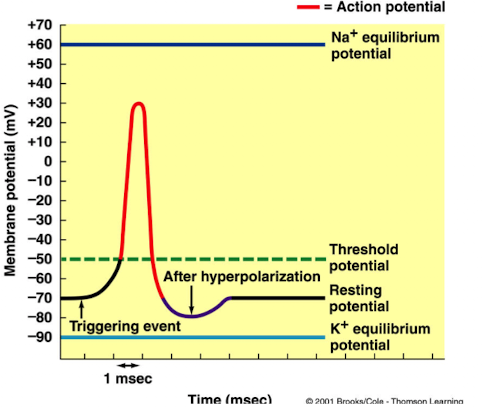
If the cell’s resting potential is moved away from threshold (hyper polarized), then …
the cell would be under excitable
What does the basolateral pump do in K+ secretion?
it simultaneously transports Na+ into the lateral space and K+ into the tubular cell