Respiratory
1/58
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
Newborn noses
very small nasal passages, making them more prone to obstruction; sinuses are not developed so less prone to sinus infection.
Infants
preferential nose breathers (only mouth breath when in distress), produce very little mucus, which starts to make them more susceptible to infections.
Infant throats
Infant tongues are larger (relative to oropharynx) than than adults
Placement of tongue (posterior) can lead to airway obstruction.
Children have enlarged tonsillar and adenoid tissue, which can lead to airway obstruction.
Pediatric trachea
Smaller width in infants & children than adults
Edema, mucus, bronchospasms – greatly diminish airway
Leads to increase in
Resistance to airflow
Work of breathing/metabolic rate
Leads to quicker decline
Pediatric larynx and glottis
Located higher in neck
Prone to aspiration of foreign bodies
Airway highly compliant/pliable
Prone to collapse in presence of obstruction
Pediatric lower airway structures
The bronchi and bronchioles of infants and children are narrower in diameter than the adult’s.
Increased risk for lower airway obstruction.
Fewer numbers of alveoli (major sites of gas exchange)
Higher risk of hypoxemia.
Continue to develop through age 7-8 years (numbers double from term infant )
Infant chest walls more compliant (pliable)
Can’t support lungs as well
Risk factors of respiratory issues
Prematurity
Chronic illness (diabetes, sickle cell anemia, cystic fibrosis, congenital heart disease, chronic lung disease)
Mobility disorders (cerebral palsy, muscular dystrophy)
Immune deficiency
Passive exposure to cigarette smoke
Crowded living conditions
Air pollution
Daycare attendance
Travel
Normal respirations across pediatric ages
Newborn (birth-4 weeks): 30 to 60/min
Infant (1-12 months): 25-30/min
Toddler (1-2 years): 25-30/min
Preschooler (3-5 years): 20-25/min
School aged (6-12 years): 20-25/min
Adolescent (13-18 years): 16-20/min
Respiratory assessment
Skin Color: pallor, cyanosis, acrocyanosis
Rate and depth of respirations: tachypnea
Nose and oral cavity (obstruction, drainage, etc.)
Cough: productive vs non –productive, what does it sound like?
Upper airway noises: stridor, croup
Respiratory effort: nasal flaring, head bobbing, retractions, grunting
Anxiety and restlessness/fussiness signs of air hunger (if late you can see lethargy)
Clubbing (chronic sign of pulmonary or cardiac dysfunction)
Hydration status (dehydration)
Retractions
Sign of respiratory distress (not normal!)
Note the location:
Supraclavicular
Clavicular
Suprasternal
Substernal
Subcostal
intercostal
Identify if they are mild, moderate or severe
Palpation and percussion during assessment
Palpate
sinuses for tenderness in older child
Enlargement/tenderness of lymph nodes of head/neck
Is tactile fremitus present? (pneumonia)
Percuss
Flat or dull sounds over consolidated lung tissue (pneumonia)
Tympanic sounds (over pneumothorax)
Hyperresonance with asthma-related air trapping
Auscultation
Listen to Anterior (Front) & Posterior (Back)
Bilaterally – should be equal
Different sounds on each side is concerning
Note Pitch, quality, volume
Inspiratory phase usually softer/longer than expiration
Smaller fields/thinner chest walls so determine if sounds are truly in lung fields or being transmitted
Also listen with the stethoscope against bare skin
Listen when the child is sleeping/calm if possible
Abnormal auscultation findings
Wheezing (inspiratory or expiratory)
atelectasis
diminished or absent lung sounds
crackles
coarse sounds
stridor
Signs of respiratory distress in children
Retractions
Tracheal tug
Nasal Flaring
Head bobbing
Tachypnea
Grunting
Wheezing
Stridor
Low oxygen saturation (hypoxia)
Positioning (tripod)
Not “fighting” with caregiver or HCP (ominous sign)
Lab tests for respiratory disorder
Arterial blood gases
complete blood count
sputum cultures
Nasal-pharyngeal Swabs: positive identification of RSV or other viral illness
Rapid strep testing via throat swab culture (oropharyngeal)
Other diagnostics for respiratory disorders
Pulse oximetry: oxygen saturation might be decreased significantly (continuous or intermittent monitoring)
Imaging/X-rays:
Might reveal hyperinflation and patchy areas of atelectasis or infiltration or pneumothorax
Chest x-ray, CT and MRI scans
Common medical treatments for respiratory disorders
Supplemental Oxygen (many different devices)
Suctioning
Oral
Nasopharyngeal
Tracheal/ETT/Tracheostomy
High humidity
Chest physiotherapy and postural drainage
Saline rinses, gargles or lavage
Mucolytic agents
Chest tubes – removal of air/fluid from pleural space
Bronchoscopy – tube w/ camera and light. Assess the airway, identify/remove foreign body + other interventions
Oxygen delivery devices
Nasal cannula – up to 4L/min, low oxygen concentration, risk for drying
Simple mask – 6-10L/min, can provide higher concentration than cannula, mouth breathers
Oxymask – wide range 1-15L/min – can deliver high oxygen concentration
High Flow Nasal Cannula – heated & humidified, wide range of flow, noninvasive/nonrestrictive
Very popular
Oxygen tent/hood – can provide more humidity (covers the head or the upper body) – losing favor
Non-rebreather mask - can provide high (95%) concentration, minimum 10-15L/min
Considerations for supplemental oxygen
Oxygen is Considered a drug – need order to administer (unless protocol for emergency situations)
Consult with respiratory therapists to determine best delivery method if questions
Select proper size mask if needed
Select delivery method based on flow of oxygen needed
With higher flows, use supplemental humidification
Tonsillitis
Inflammation and redness of the tonsils
Often occurs with pharyngitis
Infection: Viral or bacterial in nature
Group A Beta-Hemolytic Strep (common offender) but it is not limited to strep!
Can be Acute leading to Chronic
Tonsillitis risk factors
exposure to bacterial or viral illness
immature immune system
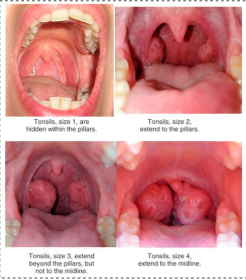
Tonsil grading
0 = no tonsils (due to past tonsillectomy)
1 = hidden behinds the pillars, barely visible
2 = extend to the pillars, visible and normal size
3 = extends beyond the pillars but they are not midline yet (enlarged, may partially obstruct airway)
4= midline, touching the uvula or each other (likely to cause airway obstruction, breathing and swallowing issues)
Tonsillitis nursing assessment
Ask:
History of pharyngitis or tonsillitis?
Fever?
Child’s voice hoarse or muffled?
Any difficulty/pain with swallowing?
Inspect mouth for redness, enlargement of tonsils
If Enlarged – child may experience difficulty breathing & swallowing
If touch at midline – airway can become obstructed
If adenoids enlarged as well – posterior nares become obstructed
Child may mouth breathe and/or snore
Mouth odor (bad breath)
Acute tonsillitis treatment
Viral – rest, warm fluids, salt-water gargles
Bacterial – same as viral PLUS Treat infection with antibiotics
Medications for symptom management:
Antipyretics to treat fever and manage pain
Antibiotics – make sure that caregivers are aware that they must complete the full course
Tonsillectomy
Surgical intervention is required for chronic, severe tonsillitis.
Tonsillectomy – for recurrent streptococcal tonsillitis or tonsillar hypertrophy
Adenoidectomy – for hypertrophied adenoids obstructing breathing
T&A = both of the above
Promoting airway clearance after tonsillectomy
Place side-lying or prone – promotes drainage of secretions
Elevate head when awake
Monitor for difficulty breathing related to oral secretions, edema or bleeding
Careful Suctioning – avoid trauma to surgical site
Risk for bleeding with tonsillectomy
High risk for hemorrhage in the post-op period.
Signs of Hemorrhage: frequent swallowing, clearing throat, restlessness, bright red emesis, tachycardia, pallor
Asses vital signs
Assess for continuing swallowing small amounts of blood – this could be early bleeding?
Dried blood may be present, spit may be blood tinged (but not frank blood)this is expected
Patient may re-bleed 4-10 days post-op when scabs come off (higher concern with fresh bleeding)
Prevention: Avoid straws, Discourage coughing, clearing throat, blowing nose
Comfort/pain relief after tonsillectomy
With or without narcotics
Liquid meds,
Tetracaine (numbing) lollipops
Popsicles with pain medication added
Ice chips/Ice collar
Round the clock for first 24 hours – even at night (wake up for meds!)
Fluid intake after tonsillectomy
Encourage fluids intake – popsicles, ice chips
Main purpose maintain fluid stats/hydration & keep throat moist
Having a moist environment will help with comfort and healing
Avoid acidic juices – may irritate the throat, painful
Avoid red/brown liquids – may be confused with blood if vomiting occurs
Family education post tonsillectomy
Care during recovery period (full recovery takes about 14 days):
Importance of pain control
On first night after surgery it is important to wake the child up for two reasons
1) to give pain medication
2) to check for any bleeding (child could be swallowing blood in their sleep)
Complications to be aware of– bleeding and infection
Importance of maintaining hydration during recovery
Activity / rest – limit activity
Reasons to contact provider after tonsillectomy discharge
Signs of hemorrhage (frequent swallowing, clearing throat, pallor, restlessness, bright red emesis or bleeding)
Signs of infection
Difficulty breathing
Lack of oral intake or signs of dehydration
Uncontrolled pain
Bronchiolitis
Bronchiolitis = Acute inflammation of bronchioles and small bronchi
Small airways become obstructed which allows adequate inspiration but not full expiration
leads to hyperinflation/atelectasis
Causes alterations in gas exchange – hypoxemia & CO2 retention, hypoventilation
#1 cause is respiratory syncytial virus (RSV)
At risk groups for bronchiolitis
infants & toddlers (usually seen in ages 0-2 years)
Severity inverse to age (younger = sicker, can be deadly)
Older kids and adults get RSV and it is like a cold -not too severe unless risk factors present
S/S of bronchiolitis at onset of illness
Rhinorrhea - clear runny nose (often profuse)
Pharyngitis.
Low-grade fever.
S/S of bronchiolitis progression
Development of cough 1 to 3 days into the illness, followed by a wheeze shortly thereafter.
Tachypnea & Retractions
Copious secretions
Poor feeding → dehydration
S/S of severe bronchiolitis illness
Worsening Tachypnea RR>70
Apnea
Quiet chest (wheezes disappear, hyper expansion and poor air exchange)
Bronchiolitis nursing assessment
HISTORY:
Ask about onset of respiratory symptoms – did the child initially have a profuse runny nose?
Any exposure to other sick people? Siblings with colds?
Day care attendance?
Has the child been eating normally?
OBSERVATION:
Does the child appear air hungry?
FOCUSED RESPIRATORY ASSESSMENTS:
Assess work of breathing – retractions, nasal flaring, tachypnea, etc.
Auscultation
Varying degrees of cyanosis & respiratory distress (see symptoms)
May have periods of apnea
VITAL SIGNS & MONITORING
evaluate effect of treatment, progression of illness
Full set of vitals
Expect to see tachypnea, tachycardia and fever, oxygen saturation may be low
Arterial Blood Gas – determine severity of respiratory acidosis
DIAGNOSTICS:
nasal swabs (detection of RSV antibodies/antigens)
Lethargy & Uninterested in feeds, surroundings or parents
Bronchiolitis nursing management
Course of illness is usually self-limited
If severe → Hospitalization for supportive care
Infants are the most likely to be hospitalized if they present with tachypnea, retractions, poor intake, lethargy
Treatment: focus on supportive treatments/care
Supplemental oxygen to maintain SpO2 >90%
Nasal/nasopharyngeal suctioning – maintain clear airway
Suctioning is a priority, provide as needed
Infants cannot blow their noses!
Oral/IV hydration
If the child is tachypneic or disinterested in feeding use IV fluids
High risk for aspiration with tachypnea – always assess respiratory system BEFORE feeding
Inhaled bronchodilator therapy (not recommended)
Ribavirin – antiviral, given via aerosol (no pregnant caregivers due to teratogenic effects), for only severe cases in immunocompromised children
Objectives of bronchiolitis management
#1 Maintain patent airway – elevate head of bed, suction PRN
#2 Promote adequate gas exchange – adjust O2 % as necessary, calm environment, avoid agitation/overstimulation
Reduce risk of infection – highly contagious (use isolation precautions), hand hygiene, PPE
Provide family education – recognize worsening symptoms if home, younger kids with increased risk, other chronic conditions?
RSV prevention
The RSV monoclonal antibodies, Beyfortus (nirsevimab) and Synagis (palivizumab), help protect infants from RSV disease by giving the infant antibodies.
Beyfortus available to all babies under 8mo, given once, more accessible (costs less than Synagis)
Synagis (Palivizumab) is available for at-risk populations (<2yo w/ prematurity, lung disease, immunocompromised), given monthly, VERY expensive
They are not vaccines, but Both of these injections makes the infection less severe and reduces the risk for hospitalization
RSV Vaccination is available for pregnant women who expect to deliever their child during RSV season
Education – hand washing, respiratory etiquette, avoiding crowds or individuals who are have respiratory s/s
Croup
Viral infection causing inflammation of larynx, trachea & bronchi (parainfluenza)
Edema results in airway obstruction
Mucus production
Narrowing of trachea results in audible inspiratory stridor (heard on auscultation or even without stethoscope)
Harsh ”barking” cough
Mild or no fever
Observe for suprasternal retractions
Most commonly affects children between 3 months & 3 years
Croup rarely occurs age 6
Symptoms appear suddenly + most often occur at night or become worse at night
Self-limiting : typically resolves within 3 to 5 days
Croup complications
Worsening respiratory distress
Hypoxia
Bacterial superinfection could develop (bacterial tracheitis)
Hospitalization if significant stridor at rest or severe retractions
Croup nursing management
Medications:
Corticosteroids – single dose to decrease inflammation
Racemic epinephrine – aerosol (inhaled), mucosal vasoconstriction
Education on medications if any are used
Educate parents on symptoms of respiratory distress
Expose child to humidified air
If seen in ED, treated and sent home be sure to explain child may worsen again.
Epiglottitis
Common Cause = Haemophilus influenzae type b
HIB vaccine has significantly reduced incidence
MEDICAL EMERGENCY
Occurs most frequently in 2-7 year olds
Signs & Symptoms:
Rapid onset of symptoms
High fever
Child appearance – appears “toxic”
Anxious, frightened appearance
Refusal to speak or speak softly
Refusal to lie down
Cough usually absent
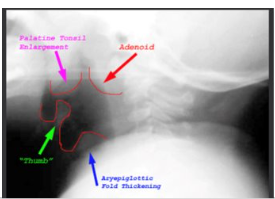
Epiglottitis on XRay
Careful positioning for x-rays
Lateral position is used
Not supine because airway occlusion could occur
Thumb Sign
Epiglottitis nursing management
Needs immediate attention and ICU monitoring
IV antibiotics to treat the infection
Provide 100% oxygen + respiratory support
Do Not try to visualize airway or stick anything in the child’s mouth!
You could compromise your airway!
Reflex laryngospasm may occur, precipitating immediate airway occlusion
If occlusion occurs- emergent tracheostomy required (better to proactively intubate with sedation before condition worsens)
Epiglottitis support & safety
Child should not be left unattended
Help child/parents remain calm
Position to provide maximum comfort to child (agitation can further increase the risk of airway occlusion
Foreign body aspiration
Younger children (infants and toddlers) at greatest risk
Unintended death related to suffocation (most common in children under 1 year old)
Causes:
Large food pieces
Small toys (legos, beads)
Found objects (coins, rocks)
Playing and running with objects or food in mouth
Object can lodge in upper or lower airways:
Upper – can often cough/blow it out
Lower – may need bronchoscopy to remove
Foreign body aspiration complications
Pneumonia, abscess formation, tissue damage
Hypoxia → respiratory failure → death
Foreign body aspiration nursing assessment
Sudden onset of cough, wheeze, stridor? Onset can also be gradual if it is not a complete obstruction
Universal choking sign in older children
Cyanosis, difficulty breathing, loss of consciousness
Foreign body aspiration nursing management
Key nursing intervention = prevention
Educate!!!
Anticipatory guidance for parents, at each health care visit through age 5
Avoid toys with small pieces, coins
Table food – Cut into small pieces in case child does not chew
Often recommend avoidance of foods, such as grapes/hot dogs/popcorn, completely until over age 3
If a child aspirates on your watch…
Follow AHA guidelines for a choking child or infant
Avoid blind sweeps of mouth
Infants = Alternating Back Blows and Chest Thrusts
Children and Adolescents = abdominal thrusts (Heimlich)
Teach family how to address choking and CPR
Apparent Life Threatening Event (ALTE)
A sudden event where an infant exhibits a combination of apnea or change in breathing, change in color, change in muscle tone and/or coughing, choking or gagging. May also include altered level of consciousness.
Serious event – needs evaluation even it if resolved without intervention
Brief, resolved, unexplained event (BRUE)
term that is being used more frequently in practice and is recommended as a replacement for ALTE by the AAP
Apnea
Absence of breathing for longer than 20 seconds (may or may not be accompanied by bradycardia)
Can be chronic or acute
Seen often when a patient presents with ALTE/BRUE
Other Potential Causes:
Central (unrelated to other cause – due to lack of signals from the brain to tell body to breathe while asleep)
Secondary to other illnesses/conditions (prematurity, sepsis, respiratory infection, hypothermia, metabolic disorders, neuro disorders, severe GERD etc.)
Administer caffeine or theophylline (respiratory stimulants) if a chronic problem (ex. Apnea of prematurity)
ALTE/BRUE Nursing assessment
Ask parents and document findings of infant’s position & activities prior to event
Obtain detailed description of the event
How long was the event?
Did the infant start breathing on their own again?
If yes, Were any interventions (stimulation, CPR) needed to regain breathing?
Assessment of Risk factors;
prematurity, anemia, metabolic disorders
Family history of seizures?
Sleep environment
Exposures (illness, toxins, smoke)
ALTE/BRUE nursing management
If you are present for the event:
1. Provide Stimulation to trigger infant to take breath
2. Rescue breathing & Bag-valve-mask ventilation if child has a pulse (most cases of a child going into cardiac arrest are due to a respiratory problem)
3. CPR if pulseless
Monitor for recurrent events
Provide thermal neutral environment
Prepare family for Laboratory & Diagnostic testing per provider orders
Identify or Rule out causes of the event
ECG, EEG, MRI, Sleep Study
Family Education:
Infant/Child CPR training
Use & education of home apnea monitoring in hospital/at home
Sudden infant death syndrome (SIDS)
The sudden – unpredictable – death of an infant without an identified cause, even after investigation & autopsy
More than 90% of all SIDS deaths occur before 6 months of age.
Often occurs during sleep
A baby can die during sleep from causes other than SIDS.
Sleep itself does not cause SIDS or other sleep-related deaths.
Preventative measures are key:
education to families about risk factors & interventions
Safe sleep!
SIDS risk factors
Co-sleeping
Soft/non-standard bedding
Prone or side-lying position while sleeping
Overheating during sleep
Maternal smoking during pregnancy
Exposure to second-hand smoke after birth
Parental substance use/abuse
Poverty (consider resources, education, environment)
Prematurity/low-birth weight
Low Apgar scores
Limited prenatal care
Family History of SIDS
Viral Illness
Twin/Multiple Birth
Reducing risk of SIDS
ABC’s of safe sleep: alone, on back, in a crib
ALONE – avoid co-sleeping, no extra “stuff” in the crib
on BACK – supine positioning for sleep
CRIB – avoid other sleeping locations. Use a firm mattress. No loose/thick/fluffy blankets
Avoid exposure to smoke (cigarette and other)
Prevent overheating: adjust room temperature, don’t add extra layers of clothing or extra blankets
Use pacifier during naps & at night– associated with reduced risk for SIDS
Keep immunizations up-to-date
Encourage Breastfeeding