Endocrine Pancreas
1/26
Earn XP
Description and Tags
A comprehensive set of flashcards covering essential topics from the Endocrine Pancreas lecture for VETM442, including drug therapy, diabetes types, insulin preparations, complications of treatment, and therapeutic goals.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
27 Terms
What are the three primary goals of drug therapy in the endocrine system?
Replace a hormone deficiency
Reduce the formation of excess hormone
Reduce the effects of excess hormone
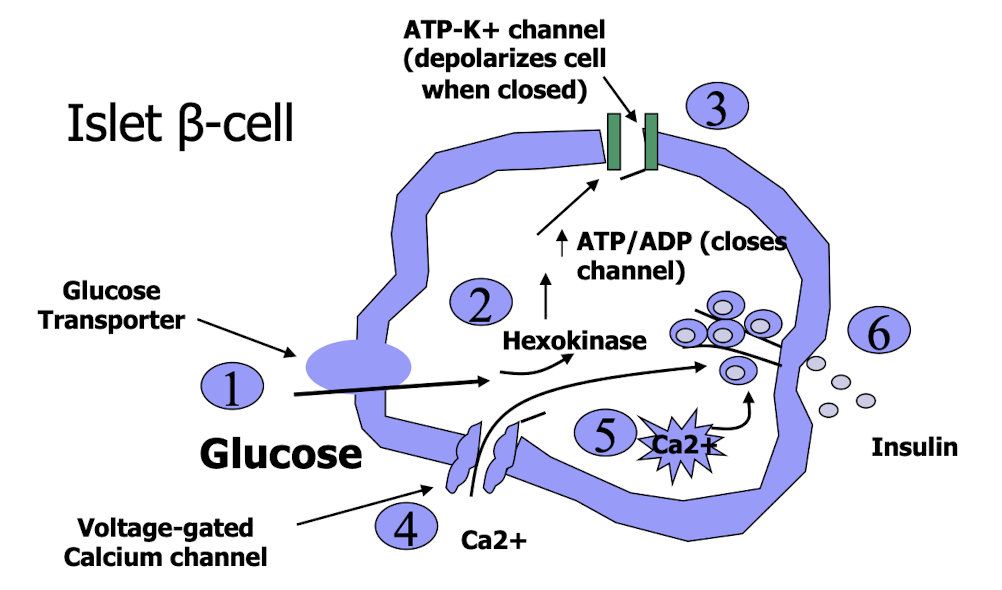
How does glucose stimulate insulin release from pancreatic β-cells?
Glucose enters the β-cell through transporters
It is phosphorylated by hexokinase
Increased ATP closes ATP-sensitive K⁺ channels
Cell depolarizes, opening voltage-gated Ca²⁺ channels
Ca²⁺ influx triggers insulin release
What is the pathogenesis of Diabetes Mellitus Type 1?
Intracellular glucose deficiency → net energy shortage
Body shifts to fat metabolism → ketosis
The animal enters a catabolic state with tissue breakdown
Extracellular hyperglycemia → hyperosmotic plasma yielding cell dehydration → glucosuria yielding polyuria, diuresis, polydipsia
What does glucose toxicity cause?
reduce insulin release
susceptibility to infections
cataracts
peripheral neuropathy
What clinical signs indicate diabetes mellitus symptoms?
Extracellular hyperglycemia, hyperosmotic plasma, cell dehydration, glycosuria, polyuria, polydipsia, and glucose toxicity.
What are the aims of therapy in diabetes mellitus management?
Abolish clinical signs, restore lost condition/weight, reduce risk of complications(hyperglycemia, ketoacidosis, peripheral neuropathy), and enhance quality of life
Therapeutic approaches for diabetes?
Insulin
Oral hypoglycemics
Diets formulated for diabetic cats
Weight reduction if obese
Cessation of diabetogenic drugs
Control of other disorders
What does 1 IU of insulin equal
36 µg insulin
100 IU/mL
Why are insulin formulas mixed with zinc, buffers, or protamine?
To prolong insulin action and stability → ensure that the distribution is not too quick and to provide a sustained release of insulin into the bloodstream
What are the types of insulin preparations mentioned?
Short-acting → Regular & Rapid acting. (Humulin, Novolin)
clear, zinc, no added protein, buffer (pH 7.2-7.4) used as initial insulin therapy until stable
IV, IM, SC, CRI → for DKA emergency
Intermediate-acting → Lente (Caninsulin)
U40
cloudy, zinc, acetate buffer
purified porcine insulin
30% amorphous ~8hrs
70% crystalline ~24hrs
SC
Long-acting insulin → Glargine (Lanus)
clear, no buffer pH 4
produce flat line and stop the liver from pushing out glucose
2 arginine residues added to insulin B-chain and asparagine is replaced with glycine residue in a-chain
used in cats
Determir (Levemir)
fatty acid bound to lysine on B-chain, after absorption binds to albumin in blood and slowly dissociates
more potent
SC in dogs
Protamine zinc insulin (PZI)
cloudy, zinc, protamine, phosphate
SC in cats
What is the most common insulin product we use in veterinary medicine?
Regular insulin (e.g., Humulin, Novolin) is the most commonly used insulin product in veterinary medicine, typically for initial therapy and managing diabetes
What is the key characteristic of Glargine insulin (Lantus)?
It produces a consistent flat blood glucose profile and has a pH of 4.0 important for long duration.
How long do we use intermediate acting insulin?
1-2 daily in dogs
BID in cats
How long do we use long acting insulin?
Typically once daily in dogs and cats(can be BID)
Why would we do BID inj of insulin vs once daily?
Greater control of BG
less swings in glucose
less complications with hypoglycemia
What do we need to monitor for dosing control?
Blood glucose curves
Clinical signs: water intake, polyphagia
Fructosamine levels
Urine monitoring
What is type 2 diabetes in cats?
A common metabolic disorder characterized by insulin resistance and relative insulin deficiency, leading to high blood glucose levels. It is often associated with obesity and can be managed with diet and insulin therapy
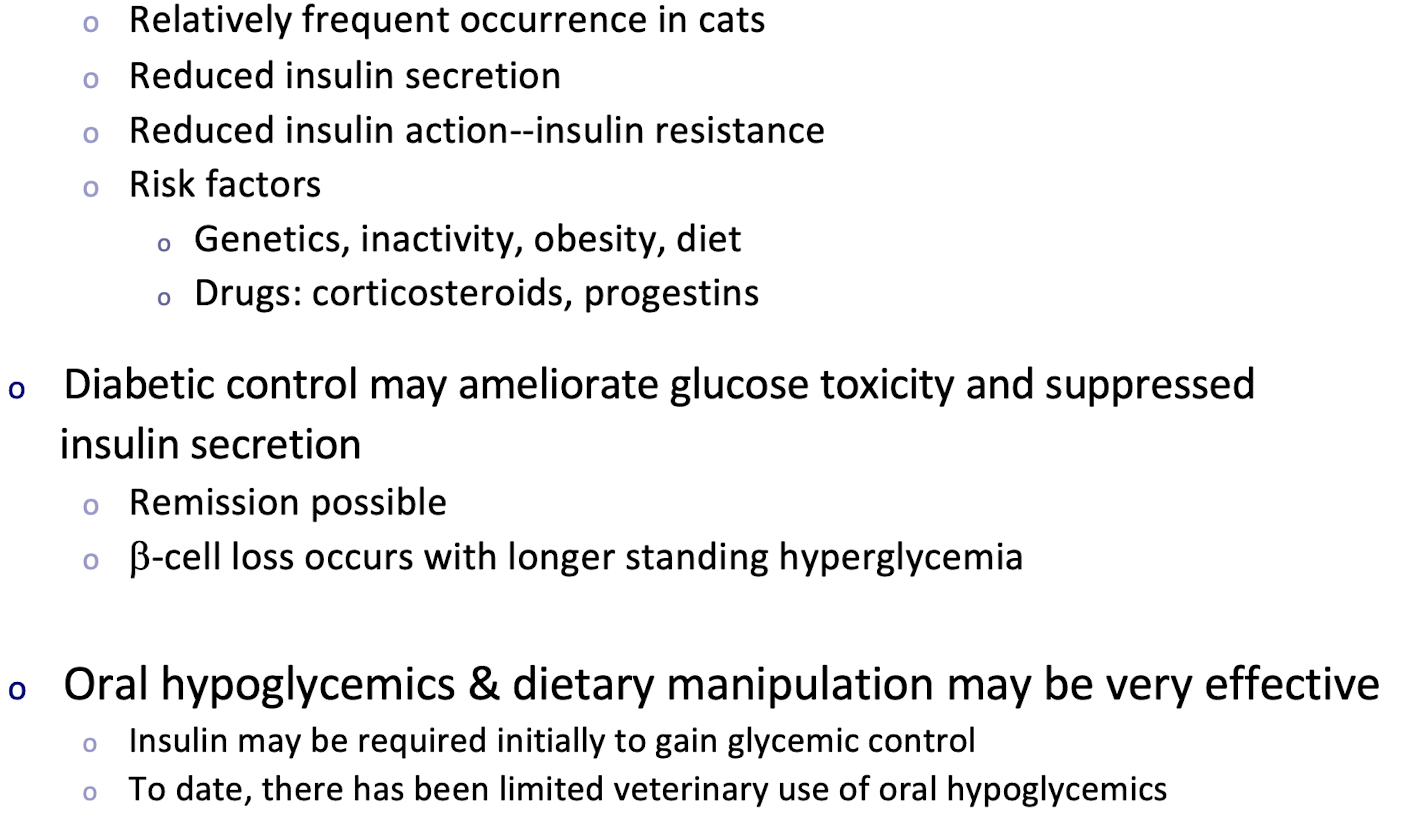
Insulin secretagogues
Oral hypoglycemics → stimulate insulin secretion from the pancreas. Assumes B-cell function present
give with meal
caution with potential for hyopglycemia, may produce amalyoid deposition
Sulfonylureas → Oral Hypoglycemics
Glipizide (Glucotrol) → insulin secretagues
Increase release of insulin by blocking ATP-sensitive-K+ channel on β-cells
give with meal
may accelerate NIDDM to IDDM
MOA Insulin sensitizers
Requires insulin but does not promote release of insulin from the pancreas. These agents improve insulin sensitivity in target tissues, primarily muscle and liver, helping to lower blood glucose levels.
Biguanides → Oral Hypoglycemics
Metformin (glucophages) → insulin sensitizers
Reduces hepatic gluconeogenesis
Increase insulin utilization by peripheral target cells (muscle, fat)
Used alone or in combination with the secretagogues
Also used with insulin therapy in humans
Less likely to produce hypoglycemia
a-glucosidase Inhibitors → Oral Hypoglycemics
Acarbose (Prandase®) → insulin sensitizers
Inhibits intestinal alpha-glucosidases and post-prandial digestion
and absorption of starches and disaccharides
Generally used in combination with sulfonylureas or insulin
Adverse effects include abdominal pain, flatulence, diarrhea
Velagliflozin (Senvelgo™), Bexagliflozin (Bexacat™)
SGLT2-Sodium-Glucose Cotransporter Inhibitors → diuretics that prevent glucose reabsorption in the kidneys, leading to increased urinary glucose excretion and reduced blood glucose levels
Transporters are found on the proximal convoluted tubules where they prevent glucose from being excreted in the urine
Blockage of the transporter results in glucose being removed in the urine (reduces renal threshold for reuptake of glucose by blood)
Both products are available as tablets
Licensed for use in cats with Type 2 diabetes mellitus
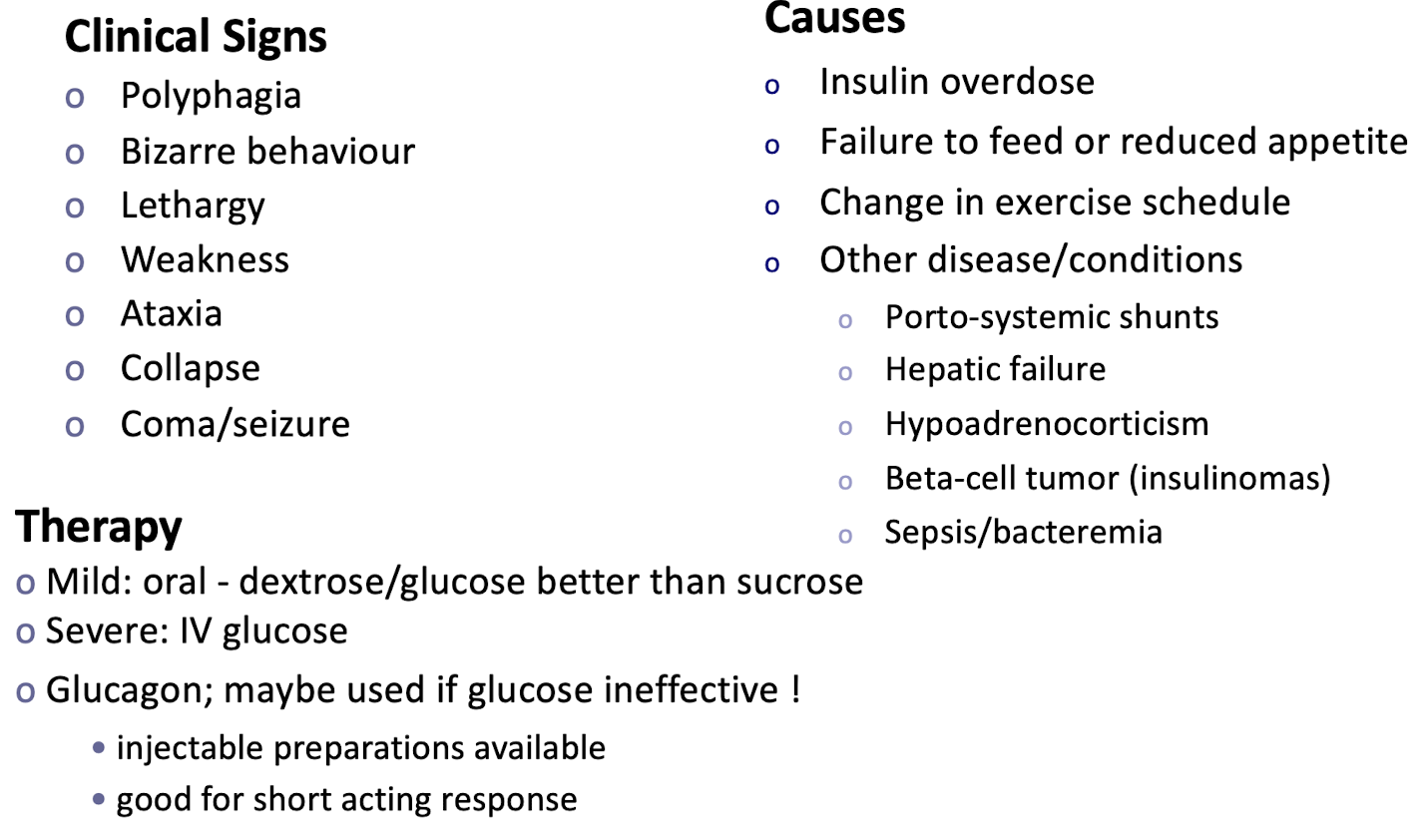
What complications can arise from insulin therapy?
Hypoglycemia is most common, Insulin overdose, failure to feed, change in exercise schedule, and other disease conditions
What is the function of SGLT2 inhibitors in diabetes treatment?
They block sodium-glucose co-transporters to reduce glucose reuptake by blood and increase glucose excretion in urine.
What should be administered for mild hypoglycemia?
Oral dextrose/glucose is preferred over sucrose.
What factors may cause problems with regulation of insulin therapy?
Administration problems, antibodies to insulin, metabolic variability, other diabetogenic hormones(corticosteroids, progestins), and the Somogyi effect(rebound hyperglycemia)