N470: Central lines
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Indications for a central venous catheter (9)
1) poor peripheral access
2) long term-IV therapeutics
3) high volume infusion
4) frequent blood sampling
5) infusion of irritant drugs- electrolytes, abx, chemo
6) blood transfusions
7) vasopressors
8) TPN
9) dialysis/apheresis
what factors influence the selection of CVCs?
1) pt characteristics and preferences
2) pt hx and comorbidities
3) infusion needs
4) CVC options- non/tunneled, implanted port
what are the main types of vascular access devices? (3)
- non-tunneled
- implanted
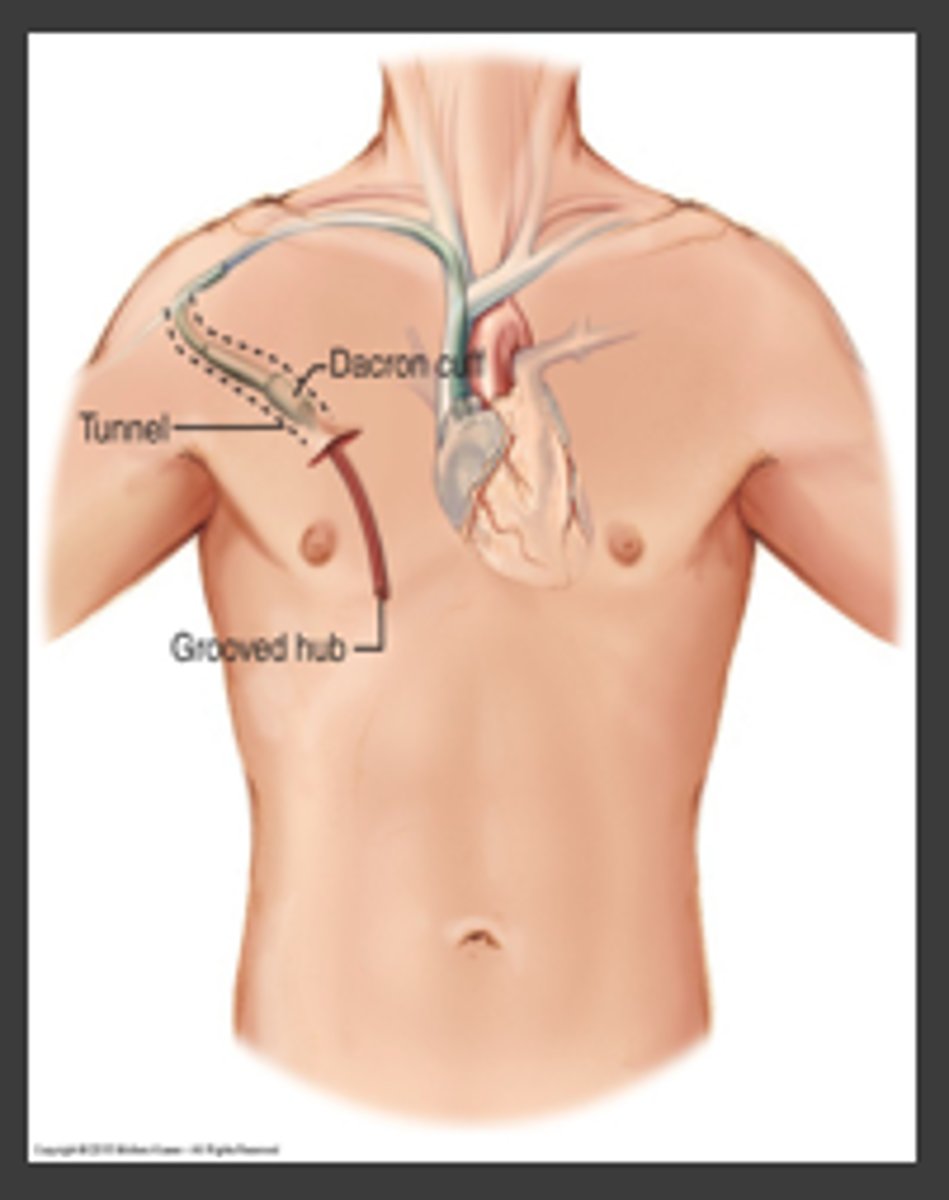
- tunneled
Examples of non-tunneled lines (4)
- PICC
- IJ
- subclavian
- Vascath
Examples of tunneled lines (5)
- hickman
- broviac
- PICC
- subclavian
- permcath
Example of an Implanted line
port-a-cath
What can be given through a peripheral IV? (4)
- high flow IV fluids
- blood products
- IV push drugs
- electrolyte replacement
What type of dressing does a peripheral IV require?
an occlusive dressing (air- and water-tight
Who inserts a IJ central line? In what setting is it done?
By an MD at the bedside
What are some qualities of an IJ central line?
- used in acute care
- multi-lumen- flush unused lines with heparin
- sutured in place
- sterile dressing
- uncomfy

Qualities of a PICC line
- non-tunneled
- anchored with suture or statlock
- used in many settings
- used for infusions and blood draws
Who can insert a PICC line?
A specially trained RN/ RT/ MD
What is a risk of using a PICC line?
higher risk for venous thrombosis- assess for pain, swelling, heat
Why would a femoral catheter be placed?
when the upper torso sites are not available or accessible; in trauma or emergency situations
in what setting can a femoral catheter be placed?
at the bedside
what are some qualities of a femoral central line? (6)
- temporary
- secured with sutures
- requires sterile dressing
- site must be monitored closely
- limits pt mobility- cannot bend at hip
- uncomfy

in what setting is a PAC placed?
in interventional radiology
Qualities of a PAC (6)
- located under the skin
- can be in place for years
- often used for chemo
- requires non-coring needle
- flushed at least once a month
- sterile procedure to a access
How long can a PAC be accessed with the same needle?
7 days
In what setting is a tunneled central line inserted?
in interventional radiology or OR (also removed in OR)
A tunneled central line is anchored by 1-2 ______
cuffs
Qualities of a dialysis line
- can be tunneled or non-tunneled (permcath/vascath/pheresis catheter)
- double or triple lumen (trialysis)
- red and blue lumens (red is for dialysis)
Assessment pieces for a central line (6)
- look at insertion and exit site for redness/swelling
- assess patency of each line
- integrity of each line (fluid leaks)
- clamps and caps present
- crepitus of chest
- pain in arm/shoulder/neck?
What does an exit site infection look like on a CVC?
localized erythema and edema at exit sire
What does a tunneled infection look like on a CVC?
inflammation along the subq track of the device greater than 2cm from exit site
Nursing management of a CVC (4)
- only access with 10 ml syringe
- all IV fluids must be on a pump
- ensure secured connections (aka luer lock tubing/syringes/caps)
- clamp line when not in use
Potential complications of CVC insertion (5)
- pneumothorax (rare)
- hematoma
- infections
- air embolism
- wrong vein
what is the #1 complication of CVCs
infection
Vascular catheter-associated infections are considered a _______ ________
never event
Central line bundle for preventing CVC infections
1) hand hygiene
2) maximum barrier precautions during insertion
3) chlorhexidine antisepsis on skin
4) optimal catheter site selection (avoid femoral)
5) daily review of need for central line
best practices for prevention of catheter-related bloodstream infection pertain to what aspects of CVCs? (3)
- dressings
- flushing
- connectors
best practices for CVC dressings (6)
- change when damp/loose/soiled
- change transparent dressing Q7days
- change gauze dressing Q24H
- use sterile dressing changes
- use biopatch at exit site
- chlorhexidine/alcohol prep with friction before new dressing
when to flush a CVC (3)
- after blood draw
- before med administration
- before and after administration if hep-locked
best practices for CVC connectors (2)
- scrub the hub for 15-30 sec, then allow to dry
- change caps per hospital policy
other complications of a CVC (4)
- intraluminal occlusion
- fibrin formation
- venous thrombosis
- drug precipitation
What is intraluminal occlusion?
a lack of blood return; looks like only itty bitty flecks of blood with draw back or flushing well but not drawing back
How to treat a fibrin formation in a central line
low dose TPA fibrinolytic (2 mg/2 ml)
where on the patient should we look first for signs of a CVC venous thrombosis?
on the arm closest to CVC placement
what is drug precipitation in a CVC?
when incompatible IV fluids or drugs go through the same line causing occlusion (the line cannot be used now)
discharge teaching for a pt. going home with a PICC
- s/s of infection
- don't play with it
- scrub hub before accessing
- clamps should be closed when not in use
- s/s of DVT
What can an implanted port be used for?
a) chemo
b) blood draws
c) anti-infectives
d) all of the above
d) all of the above
A patient asks, "after my tunneled central line is healed, what activities can I do?" The correct response by the nurse would be...
a) swim
b) play volleyball
c) shower
d) sit in the hot tub
c) shower