CLASS 1 (Perinatal Nursing and Reproductive Health)
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
87 Terms
What is the definition of perinatal?
time from when you become pregnant up to a year after giving birth.
Who do perinatal nurses care for?
patients, newborns, children, and families.
in what aspects of life does perinatal care expnad to?
Care spans the entire childbearing continuum:
Preconception → pregnancy → birth → postpartum → family transition.
In what settings of care do perinatal nurses practice
Hospital-based care (Labour & delivery units, Antenatal units, Postpartum units, Women’s health ICU, Lactation consultants)
Community & home-based care (Primary care, Public health programs, Home visits)
Virtual/telehealth (Ontario Telehealth breastfeeding line, Online/virtual prenatal classes)
what is the Calgary Family Assessment Model (CFAM)
CFAM is a framework nurses use to understand family dynamics and guide interventions.
What categories and subcategories doe the CFAM look at
It looks at structure (internal, external, context), development (stages, tasks, attachments), and functional (instrumental, expressive).
Why is the CFAM important
This framework helps perinatal nurses assess not only the pregnant person but also the entire family system that will support them during pregnancy, birth, and postpartum.
What is the Goal/Objective of perinatal nursing
A healthy person giving birth to a healthy baby.
How is this goal acheived?
Respect & cultural safety
Involvement and participation of families
Information sharing and collaboration
Active involvement in decision-making
What are the 7 Values guiding perinatal nursing according to The Canadian Association of Perinatal and Women’s Health Nurses (CAPWHN)
caring
health and well being
justice
informed desision making
dignity
confidentiality
acccountability
What are the 2 main Guiding Principles of Family-Centred Maternity & Newborn Care From Public Health Agency of Canada out of the 17 discussed in class
Care close to home is ideal (esp. important for remote/rural communities - but may be challenging to fufill).
Attitudes and language of providers impact experience (avoid harmful terms like “incompetent cervix” or “failure to progress”).
What the 5 main issues/barriers that may impact the individuals quality of care?
indigenous women
unhoused populations and pregnancy
Lgbtq population
global concerns
social determinants of health
What is GTPAL?
The GTPAL system is a standardized way of documenting a pregnant person’s obstetrical history
What does the G stand for in GTPAL?
Definition: Total number of pregnancies, regardless of outcome.
Includes:
Current pregnancy (if pregnant).
Pregnancies that ended in miscarriage, abortion, stillbirth, or live birth.
Does not matter whether the pregnancy ended at term, preterm, or in loss — it is still counted.
**twins = 1 pregnancy
What does the T stand for in GTPAL?
Gravida: Number of delivered pregnancies that reached ≥ 37 weeks gestation.
Counts pregnancies, not babies.
**twins = 1 pregnancy
Stillbirths (if delivered ≥ 37 weeks) are included in term births.
What does the P stand for in GTPAL?
Preterm: Number of delivered pregnancies that ended between 20 and 36+6 weeks gestation.
Like term, this counts pregnancies, not number of babies.
**twins = 1 pregnancy
Includes live births and stillbirths in that gestational range.
What does the A stand for in GTPAL?
Abortions: Number of pregnancies that ended before 20 weeks gestation.
Includes:
Spontaneous abortions (miscarriages).
Induced abortions (elective terminations).
**twins = 1 pregnancy
What does the L stand for in GTPAL?
Livimg: Number of living children at the time of documentation.
Multiple births (twins, triplets) are each counted here.
This number can change over time if a child passes away.
PRACTICE: Patient is currently pregnant.
She had one miscarriage at 10 weeks.
She delivered twins at 35 weeks, both alive.
G: 3 T:0 P1: A:1 L:2
PRACTICE: Patient is not currently pregnant.
Vaginal delivery at 39 weeks, 1 healthy child.
C-section at 29 weeks, baby survived.
One miscarriage at 12 weeks
G: 3 T:1 P:1 A:1 L:2
What is preconception
The period before pregnancy, focusing on optimizing health for future conception.
What is the goal of preconception? what components are included in preconception care?
Goal: Improve health status of women and men before conception to reduce risks and prevent poor maternal/fetal outcomes.
Health Promotion
Risk Assessment
Interventions
What are Determinants of Health in Preconception (impact pregnancy outcomes) (8)
Income & social status – ability to access care & nutrition.
Education & literacy – health literacy affects choices.
Social environment – partner/family/community support.
Physical environment – housing, pollution, workplace safety.
Healthy behaviours – diet, exercise, substance use.
Biology/genetics – inherited conditions.
Access to health services – availability & affordability.
Culture – beliefs about pregnancy, food, and healthcare.
Is nutrition and weight important during preconception and pregnancy? why?
YES: modifiable risk factor → directly influences maternal & fetal outcomes.
What risks do being over weight/ underweight give
preterm birth
diabetes
hypertension
growth restriction
low birth weight***
What BMI is underweight, normal, overweight and obese? what is the typical weight gain weekly?
underweight = less than 18.5 BMI (1lb weekly gain)
normal = 18.5 BMI - 24.9 BMI (1lb weekly gain)
overweight = 25 BMI to 29.9 BMI (0.6 lb weekly gain)
obese = more than 30 BMI (0.5 lb weekly gain)
What is NTD
In pregnancy, NTD stands for Neural Tube Defect, a birth defect of the brain, spine, or spinal cord that occurs when the neural tube fails to close properly in the early weeks of pregnancy
Why do NTDs sometimes occur. What is essential to prevent this from occuring
The neural tube closes within the first month of gestation, often before pregnancy is recognized.
Folic Acid is Essential for closure of the neural tube → prevents spina bifida, anencephaly.
What is the Supplementation Recommendations for someone who is LOW RISK to ntd
LOW RISK (healthy, no risk factors):
0.4 mg folic acid daily
Begin 2–3 months before pregnancy and continue throughout pregnancy.
What is the Supplementation Recommendations for someone who is MODERATE RISK to ntd
MODERATE RISK (diabetes, epilepsy, obesity, family history of NTD):
1 mg Folic acid daily,
Begin 3 months before pregnancy, continue through the 1st trimester → then reduce to 0.4 mg second trimester.
What is the Supplementation Recommendations for someone who is HIGH RISK to ntd
HIGH RISK (personal ntd/partner ntd/previous NTD baby):
4 mg Folic acid daily
Begin 3 months before pregnancy, continue through the 1st trimester → then reduce to 0.4-1 mg second trimester.
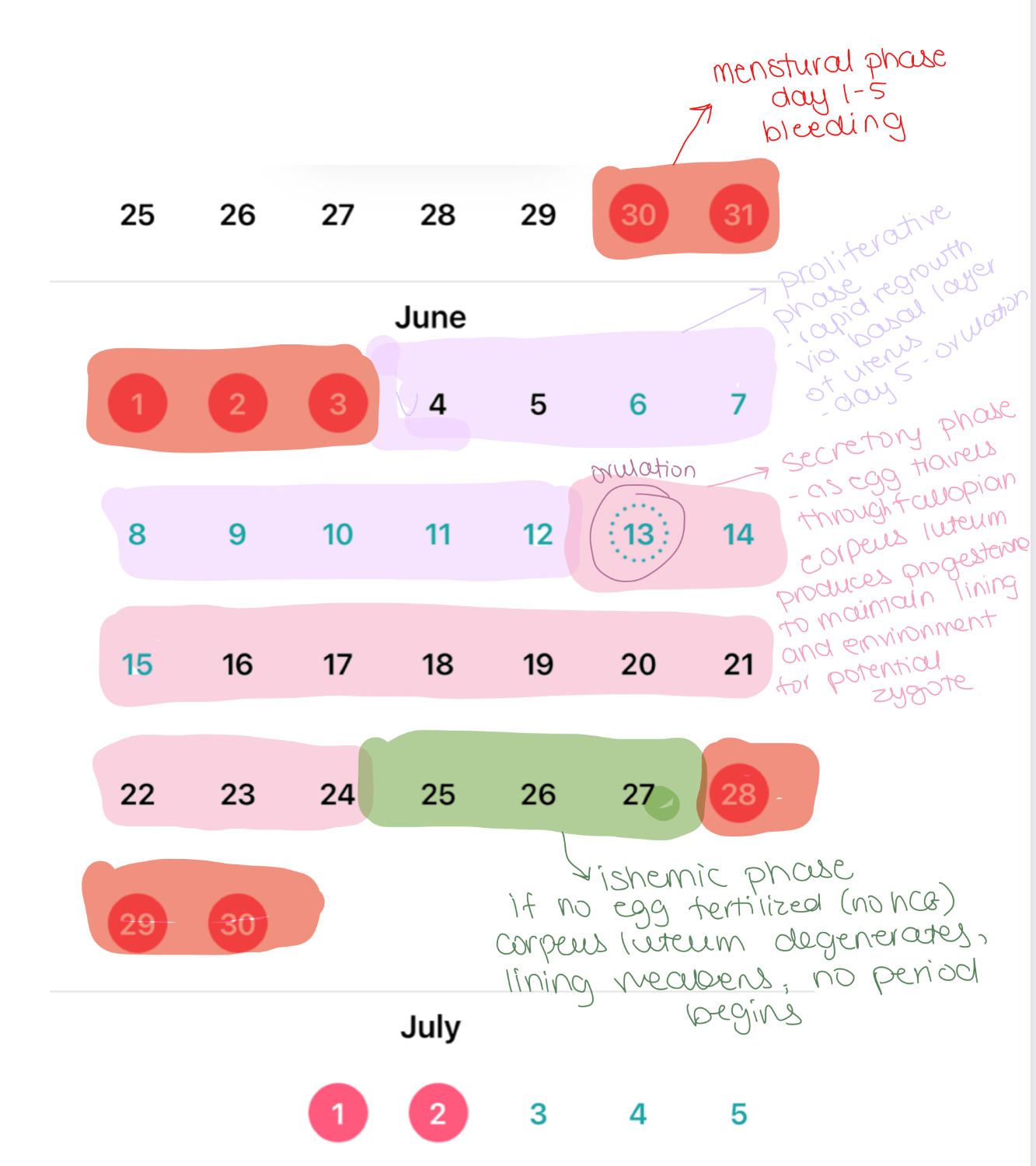
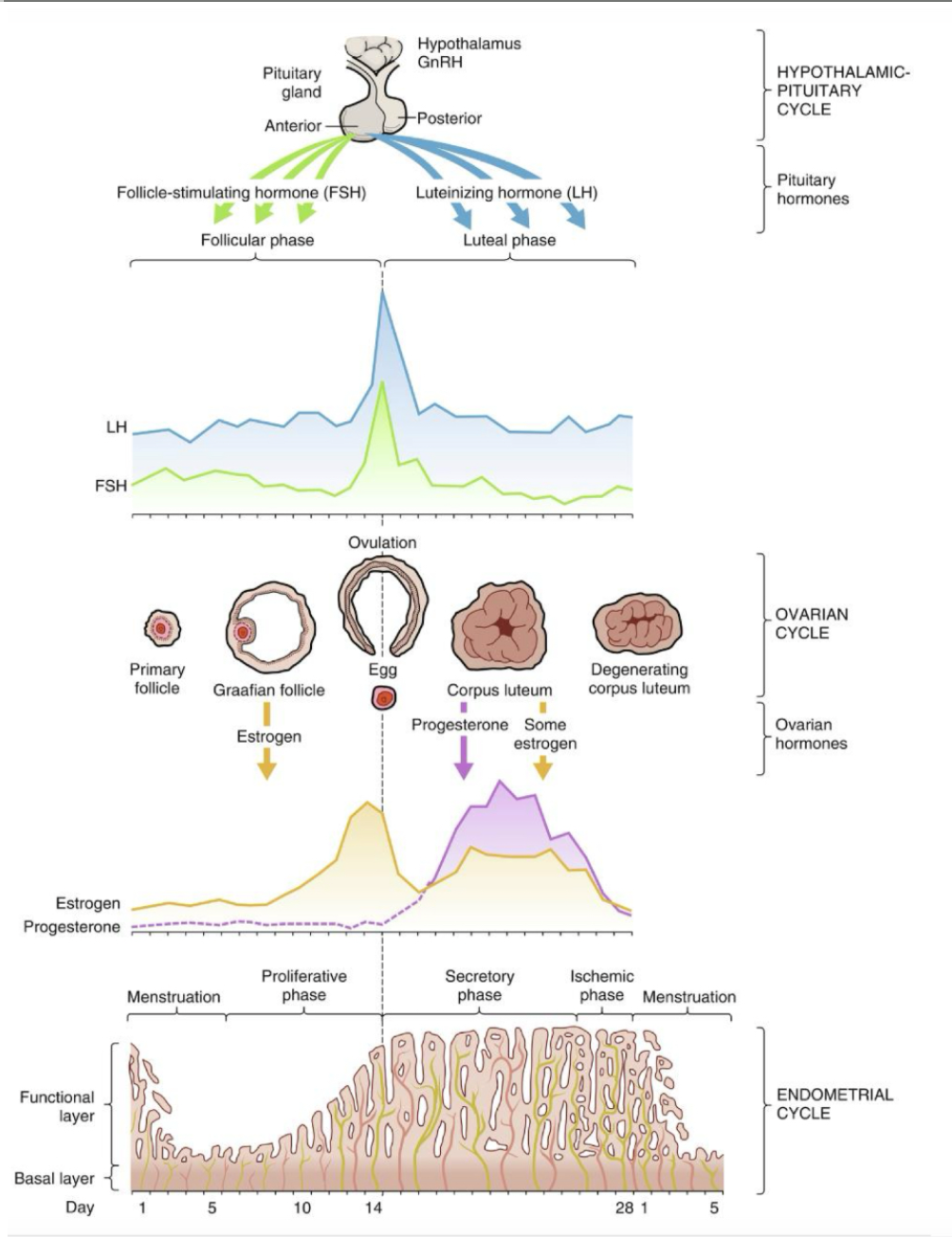
What are the 3 interconnected cycles all making up the mentstrual cycle
Endometrial cycle (uterine lining changes)
Hypothalamic-pituitary cycle (hormonal regulation)
Ovarian cycle (ovary follicle maturation & ovulation)
ENDOMETRIAL CYCLE: What Is the first phase of the endometrial cycle - what are the key events
MENSTRUAL
shedding of the functional layer of endometrium
menstrual bleeding
Days 1-5
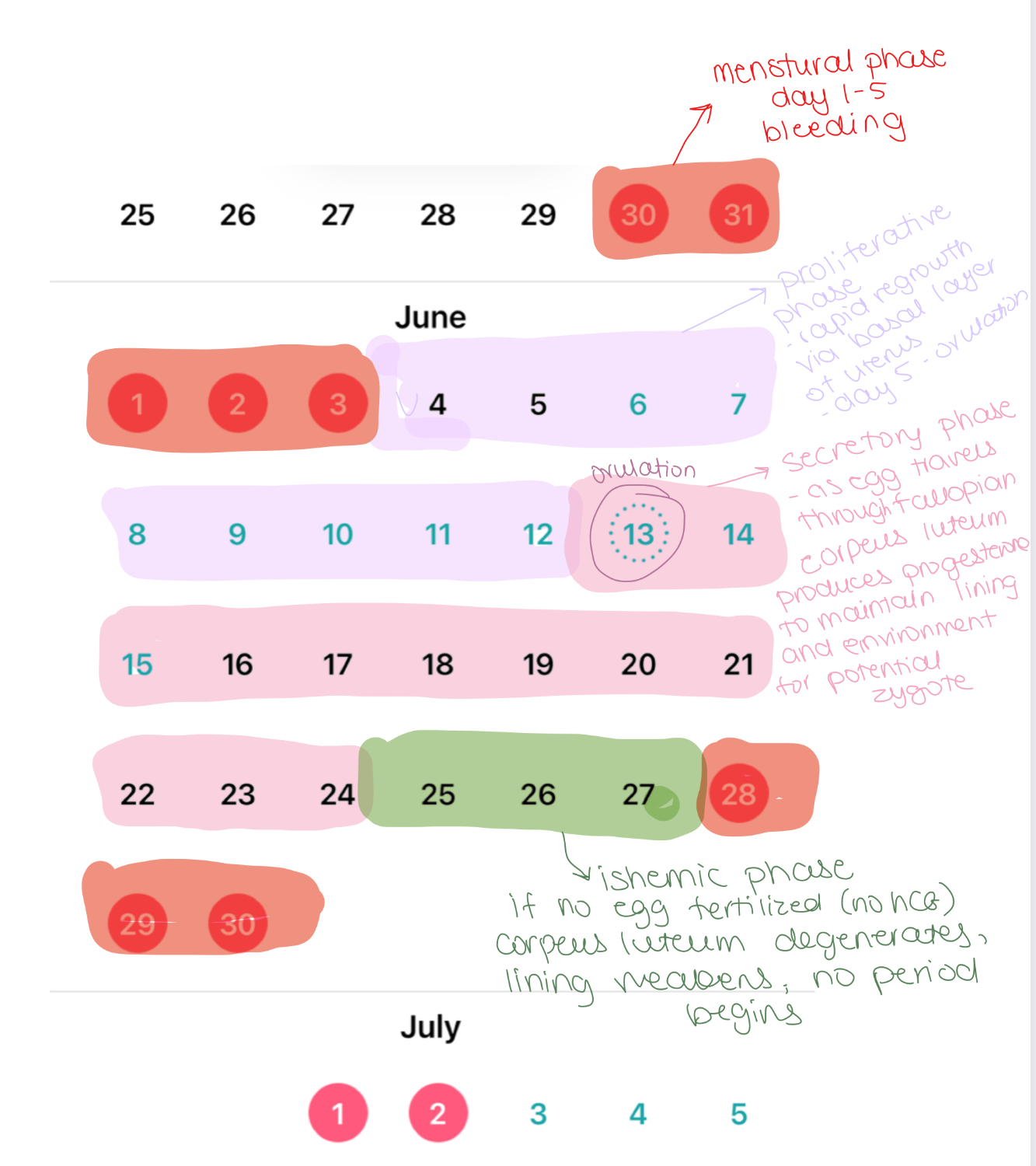
ENDOMETRIAL CYCLE: What Is the second phase of the endometrial cycle - what are the key events
PROLIFERATIVE
rapid regrowth of the endometrium via the basal layer
prepares for potential implantation
Days 5 - ovulation
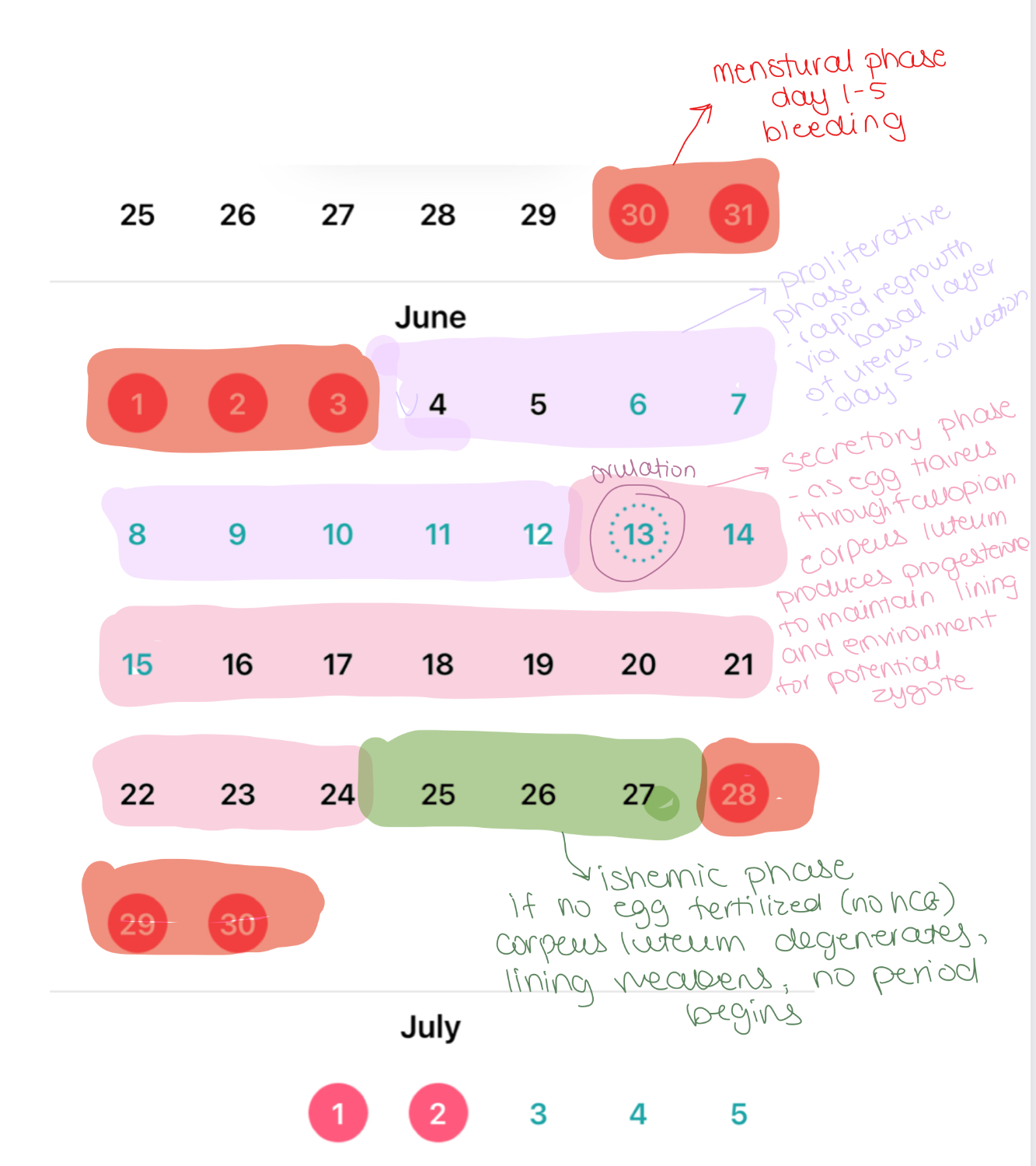
ENDOMETRIAL CYCLE: What Is the third phase of the endometrial cycle - what are the key events
SECRETORY
as endometrium thickens, progesterone is secreted from corpus luteum to maintain that thickness
gives a good environment for potential implantain
Ovulation - 3 days before next period
Around 8 - 11 day period - at this time is when fertilization could happen
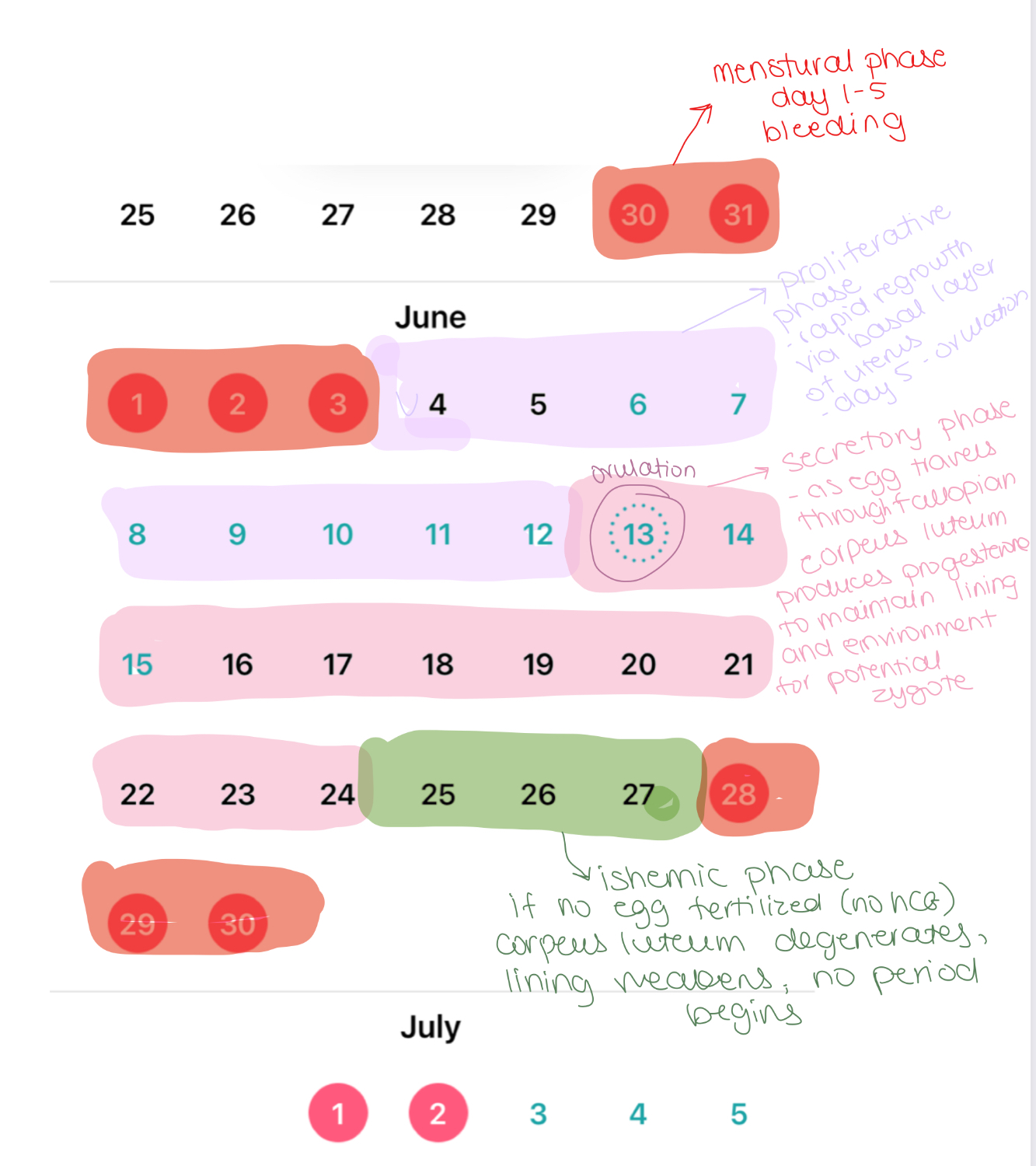
ENDOMETRIAL CYCLE: What Is the fourth phase of the endometrial cycle - what are the key events
ISCHEMIC
corpeus luteum degenerates
estrogen and progesterone droop
endometrial blood supply stop therefore no cell dividing or regrowth therefore necrosis
necrosis = shedding tissue (aka menstruation begins again)
Last 3 days of the cycle
ENDOMETRIAL CYCLE: what are the 2 layers of the uterus called and its function
Functional Layer (Stratum Functionalis): Outer 2/3 of the endometrium - Grows each cycle in response to estrogen and progesterone
Basal Layer (Stratum Basalis): Inner 1/3 of endometrium - Provides regrowth for the functional layer in the next cycle
HYPOTHALAMIC-PITUITARY CYCLE: What happens during stage 1 of the cycle beginning at menstruation
Hypothalamus starts the cycle
After menstruation, progesterone and estrogen levels are very low.
Hypothalamus recognizes this and in turn releases GnRH to the anterior pituitary
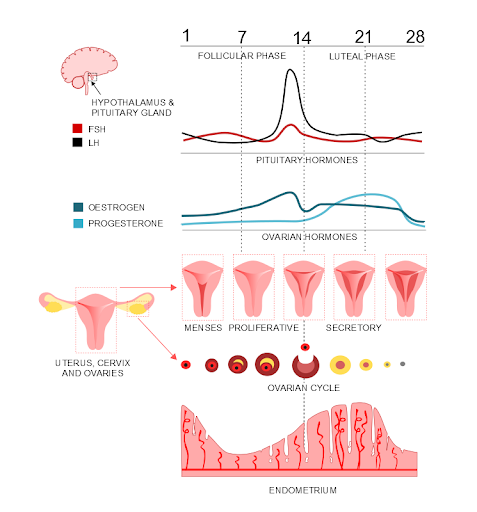
HYPOTHALAMIC-PITUITARY CYCLE: What happens during stage 2 of the cycle
Pituitary gland responds
The anterior pituitary FIRST releases FSH
this stimulates a bunch ovarian follicles (each with one egg) to start maturing
these follicles in turn produce estrogen
**the estro is what causes the proliferative phase (growth of endo lining)
THEN
when the estrogen levels meet the threshold. the anterior pituitary THEN release LH
The LH surges causes ovulation - the release of one dominant egg from its follicle
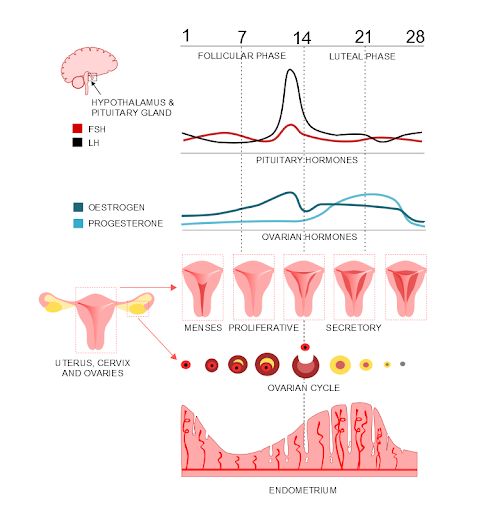
HYPOTHALAMIC-PITUITARY CYCLE: What happens during stage 3 of the cycle
Corpus luteum and luteal phase
Hormones stop here
After ovulation the leftover follicle become the corpus luteum
the corpus luteum then secretes progesterone (and some estrogen) - aka secretory phase
this progesterone prepare uterine lining for preg
If fertilization
corpeus luteum recognizes the hcg produced by the developing embyo and stops producing progesterone
hCG “rescues” the corpus luteum, keeping it alive.
The corpus luteum continues producing progesterone (and some estrogen) to maintain the endometrium and support the pregnancy in the first trimester.
If no fertilization
there’s no hCG (human chorionic gonadotropin).
Without hCG, the corpus luteum degenerates → corpus albicans → progesterone and estrogen drop → functional layer of the endometrium sheds = menstruation.
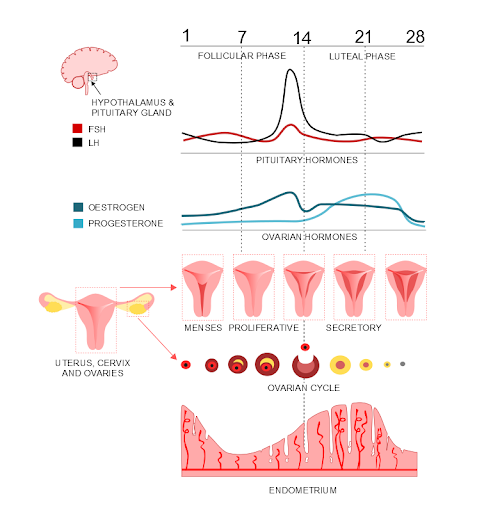
OVARIAN CYCLE: What happens during stage 1 of the cycle
FOLLICULAR PHASE
Days 1-14
Multiple follicle mature
One becomes dominant (Graafian follicle)
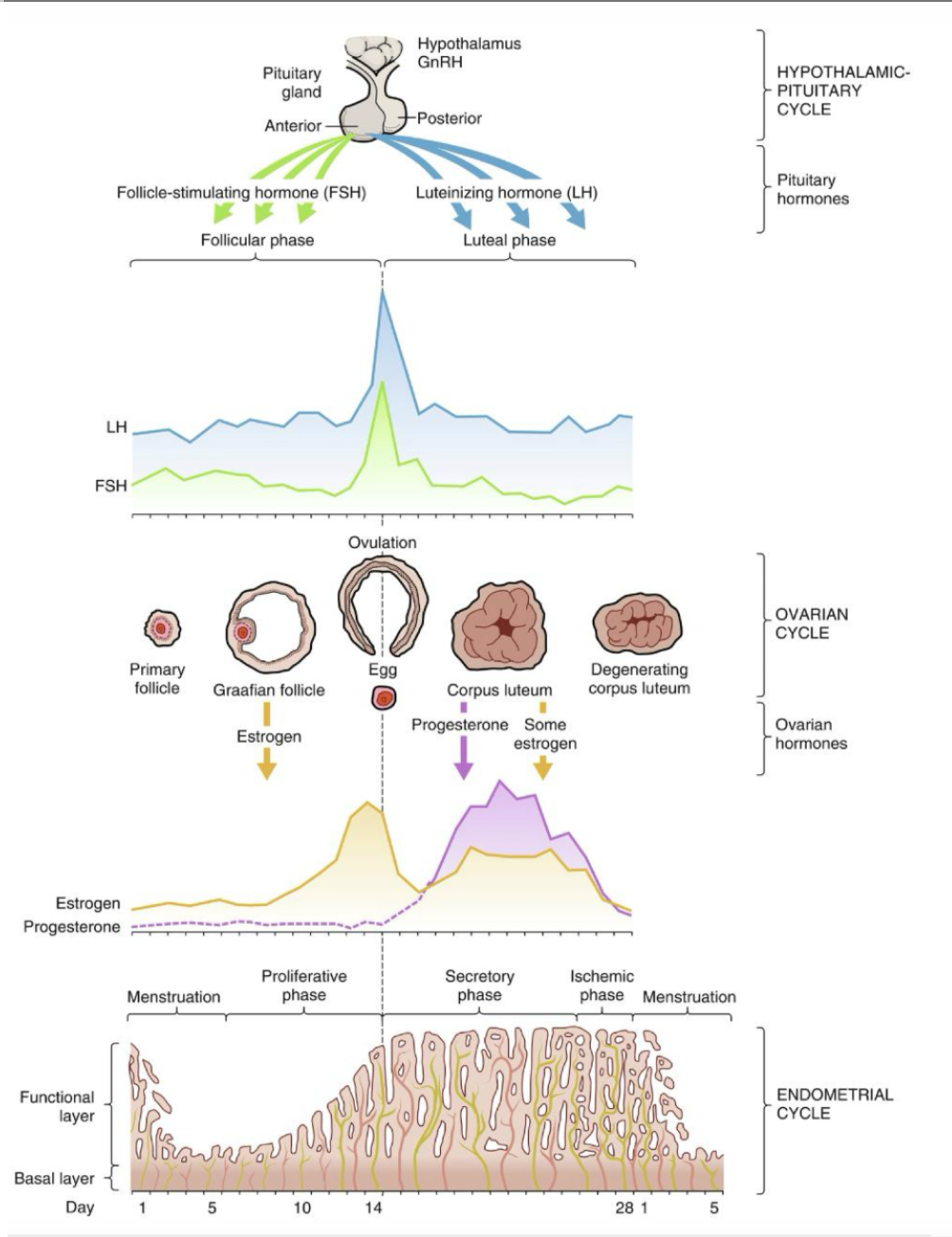
OVARIAN CYCLE: What happens during stage 2 of the cycle
OVULATION
Day 14
LH surge releases oocyte from ovary
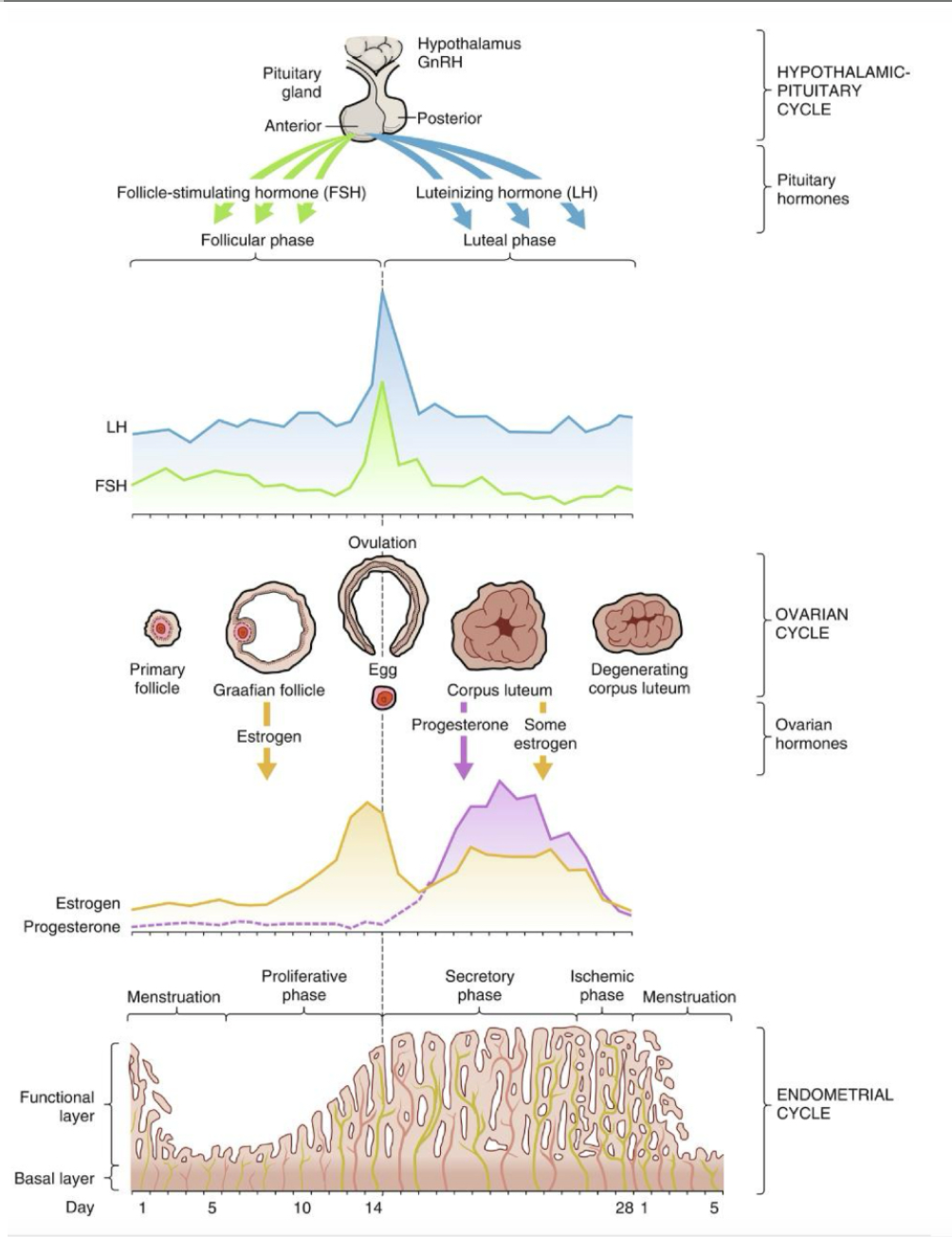
OVARIAN CYCLE: What happens during stage 3 of the cycle
LUTEAL PHASE
post ovulation
empty follicle turns into corpus luteum
corpus luteum secretes progesterone and some estrogen to support endometrium
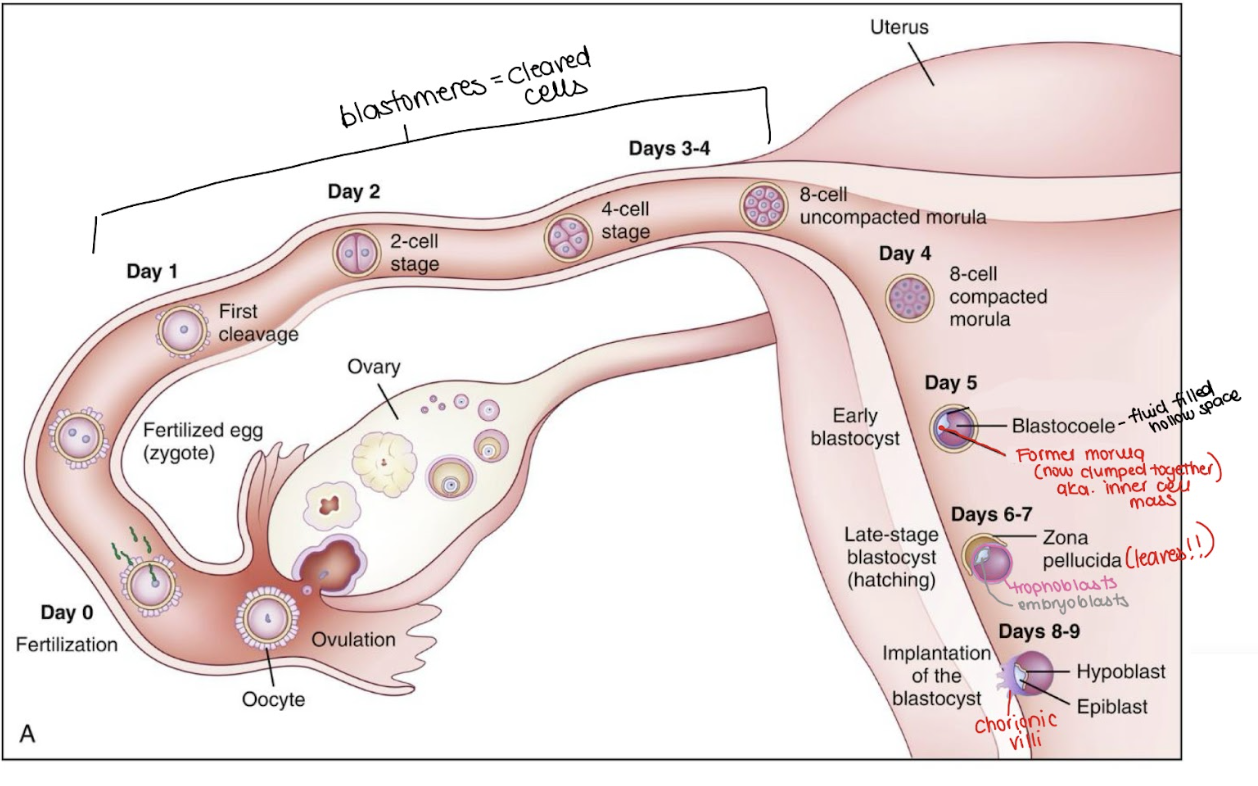
After ovulation, fertilization and early development begins. what are the 5 stages?
Ovulation
Fertilization
Zygote firmation
Celldivision
implantation
what happens during OVULATION
🥚 Ovulation
Around day 14 in a 28-day cycle (after the LH surge), the mature egg is released from the ovary.
The egg enters the fallopian tube, specifically the ampulla, which is where fertilization usually occurs.
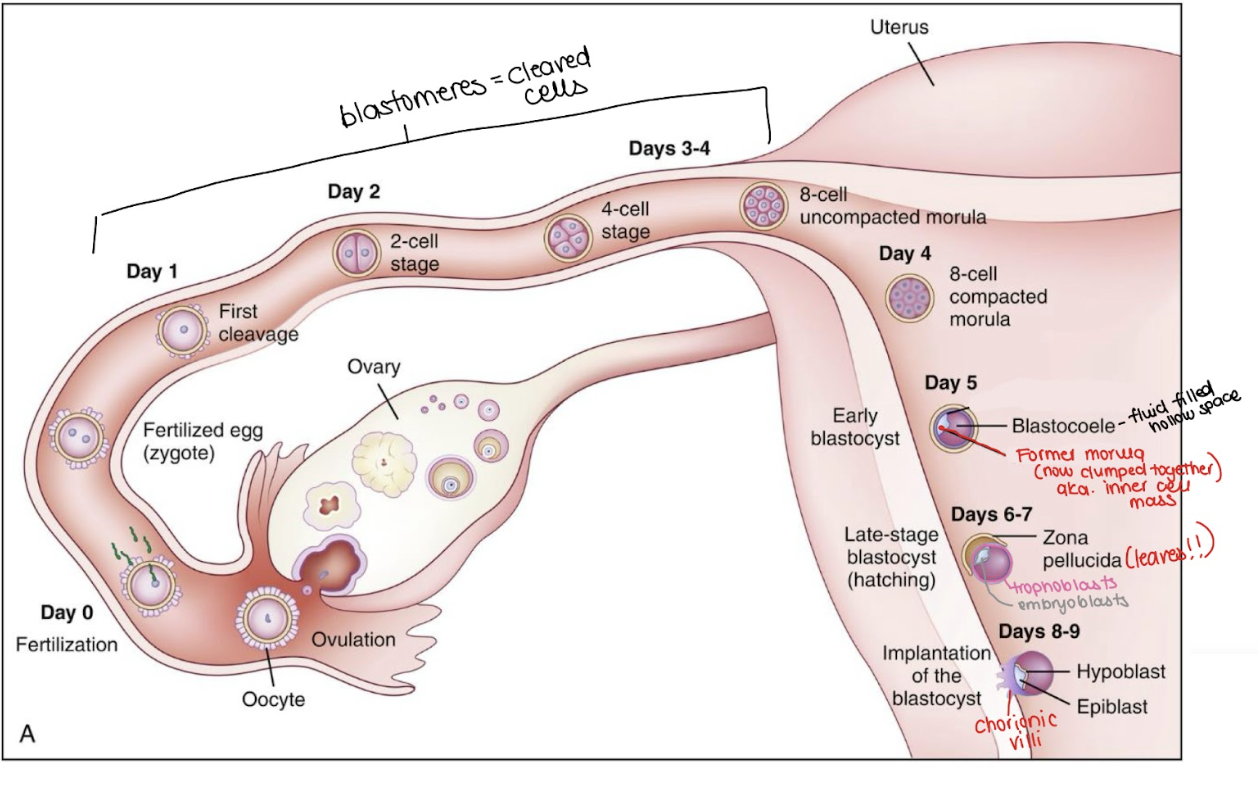
what happens during FERTILIZATION
💞 Fertilization
Sperm meets egg in the ampulla.
Sperm must penetrate the zona pellucida (protective layer around the egg).
This triggers the zona reaction, which makes the egg impenetrable to other sperm—only one sperm should fertilize the egg.
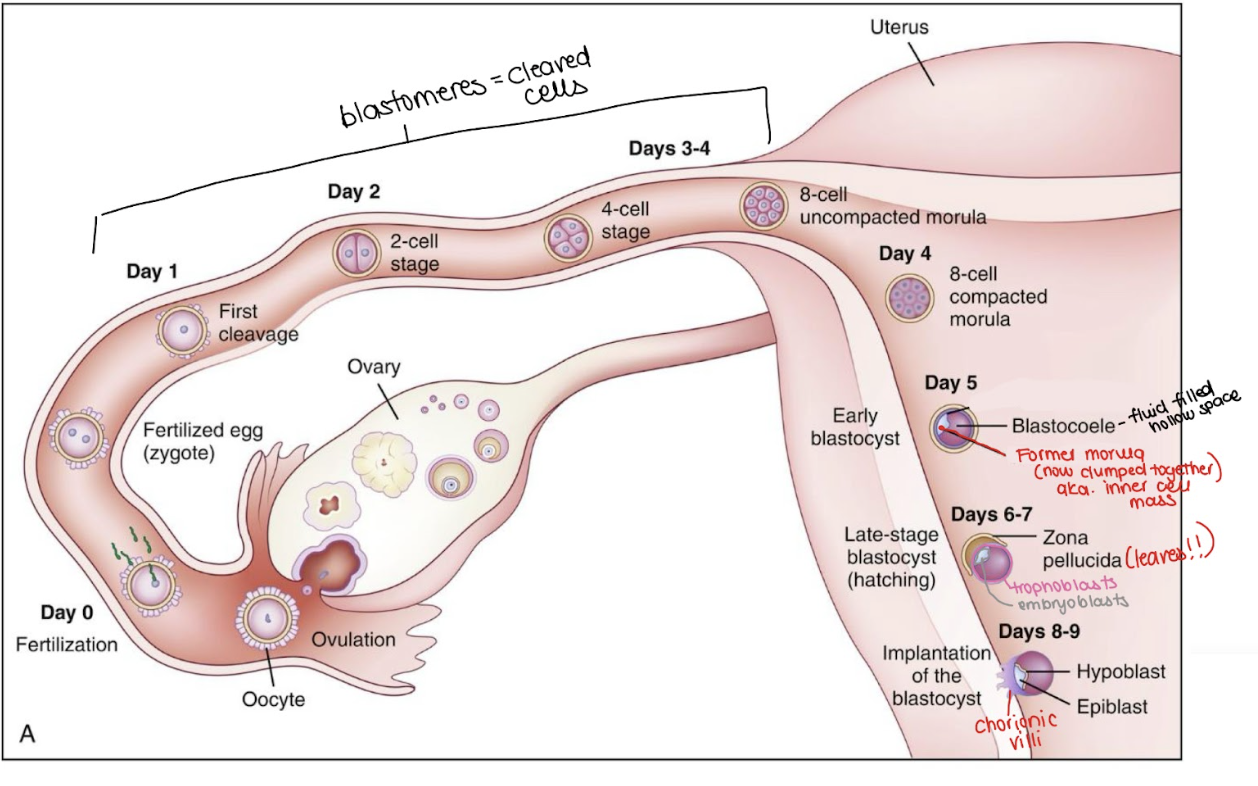
what happens during ZYGOTE FORMATION
🧬 Zygote Formation
The nuclei of the egg and sperm unite, forming a zygote (fertilized egg).
This marks the biological beginning of pregnancy.
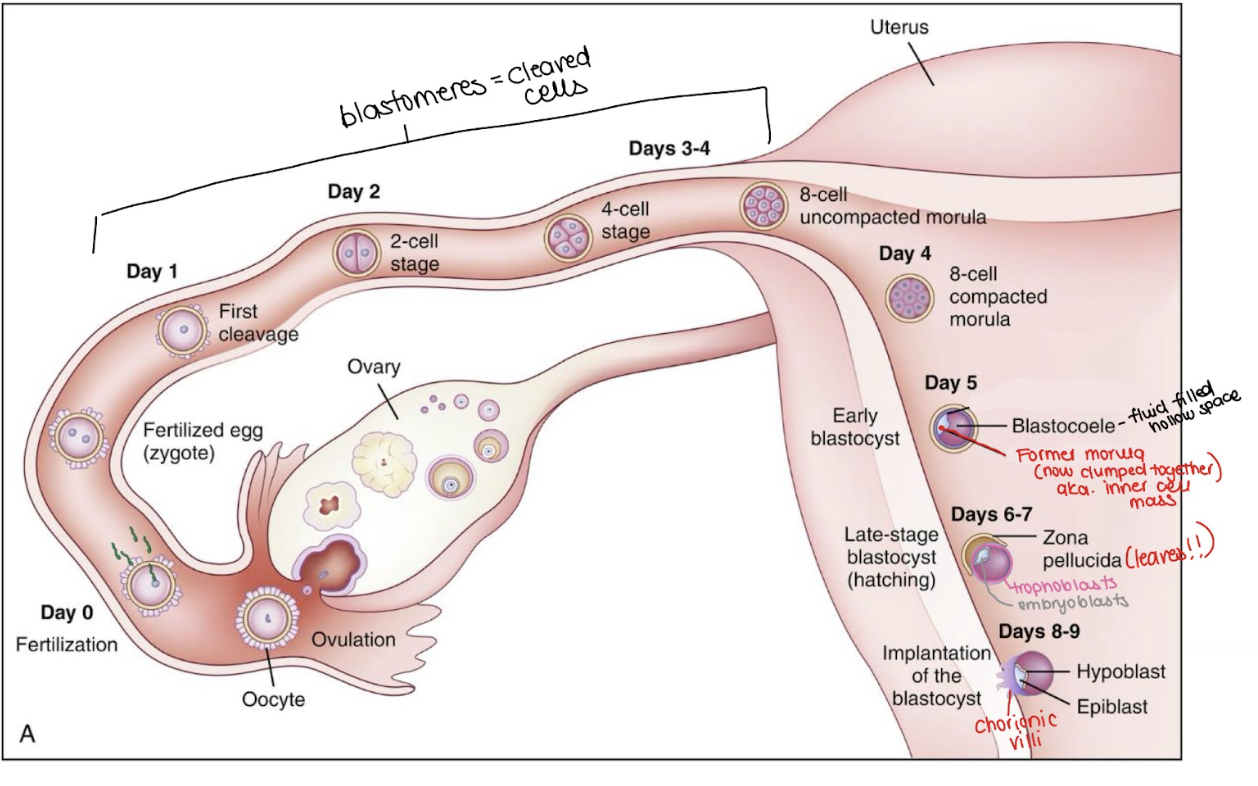
what happens during CELL DIVISION
Cell Division (Cleavage)
As the zygote moves from the tubes to the uterus it begins rapid cell division without increasing in size.
The resulting smaller cells are called blastomeres.
Around day 4–5, the cells form Morula = solid ball of cells
Fluid starts to collect inside the morula, creating a hollow cavity - At this point, it’s called a blastocyst (inner cell mass of blastomere surrounded by fluid).
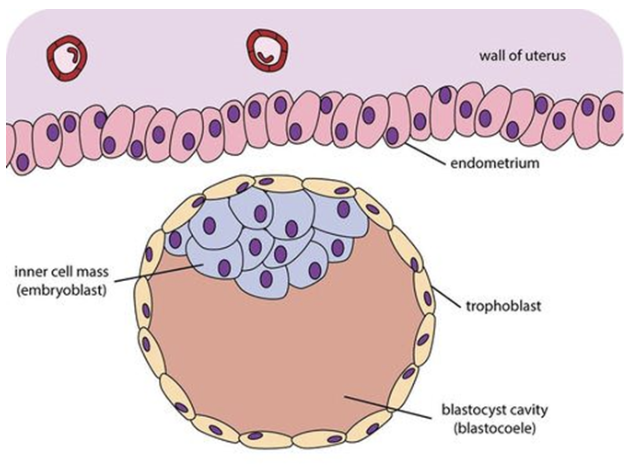
All the blastomeres are “general-purpose” at first. Then, by around day 5, some of them self-organize into groups with different jobs:
Trophoblasts = the outer layer → placenta & membranes.
Embryoblasts = the inner cell mass → the actual embryo (baby).
The zona pellucida is like a “shell” around the early embryo.
Around day 5–6, just before implantation, the blastocyst has to “hatch” out of the zona pellucida.
Only then can the trophoblast cells directly touch the endometrium and implant.
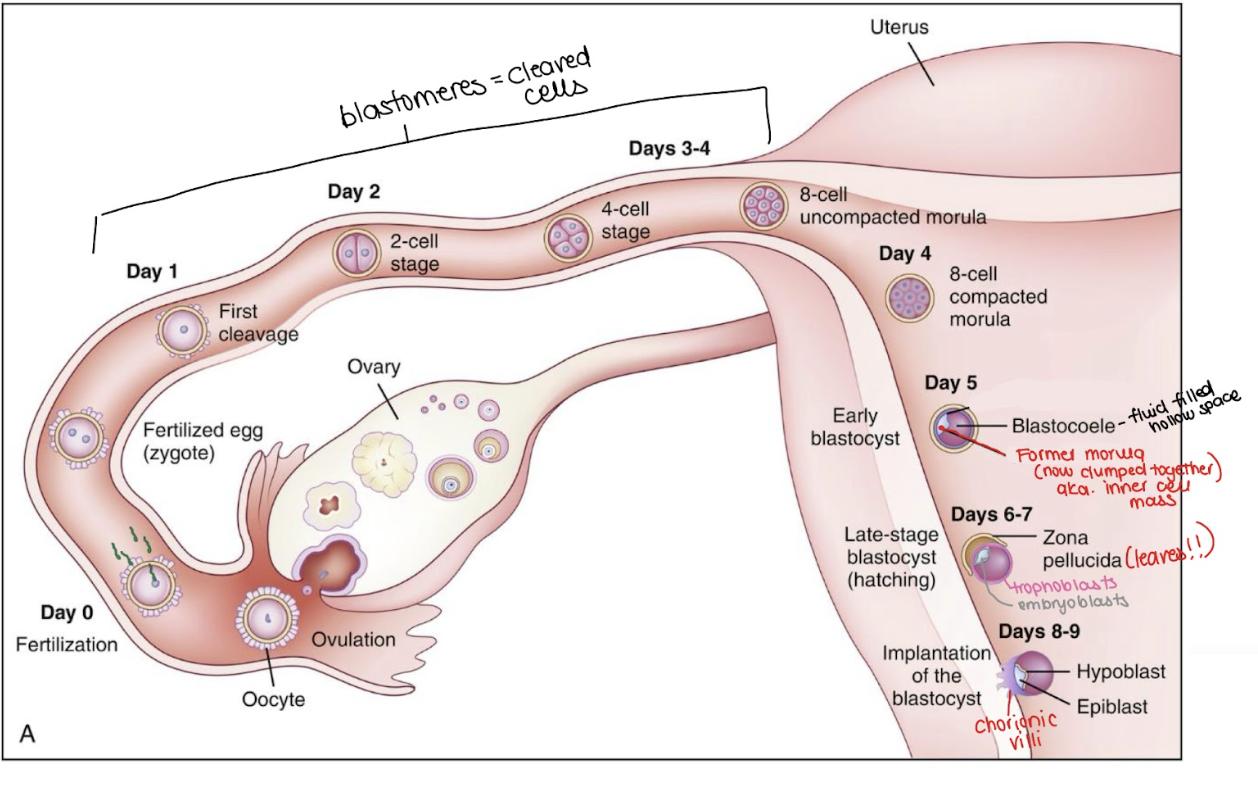
what happens during IMPLANTATION
Around days 6-10
The blastocyst attaches and embeds into the endometrium (uterine lining).
Trophoblast cells secrete enzymes to help the blastocyst burrow into the endometrium.
Chorionic villi (from the trophoblasts) form → finger-like projections that allow maternal-fetal exchange (oxygen, nutrients, waste).
Some people may notice light spotting or cramping, which is normal.
What is the first biochemical marking of pregnancy
First Biochemical marker of pregnancy: β-hCG (Human Chorionic Gonadotropin)
how is the marker produced? key info?
Produced by trophoblast cells at implantation
Detectable: 8–10 days after conception (usually missed period)
Rises but peaks ~9–10 weeks
stabilizes ~20 weeks
what is its relevance in terms of teaching?
Pregnancy tests (the urine ones you buy at the store, and the blood ones done in clinic) detect hCG.
That’s why pregnancy tests work after implantation — before then, there’s no hCG to detect.
what are the 3 signs of pregnancy one can see?
Presumptive (subjective): fatigue, nausea, breast changes, missed period
Probable (objective): positive pregnancy test, abdominal changes
Positive (definitive): fetal heartbeat on Doppler, visualization on ultrasound
**A positive pregnancy test alone is not a positive sign; could be false positive/negative
why is knowing Estimated date of birth important?
Why important: Accurate dating is essential for:
Timing of prenatal screening
Assessing fetal growth
Planning for post-dates care or interventions
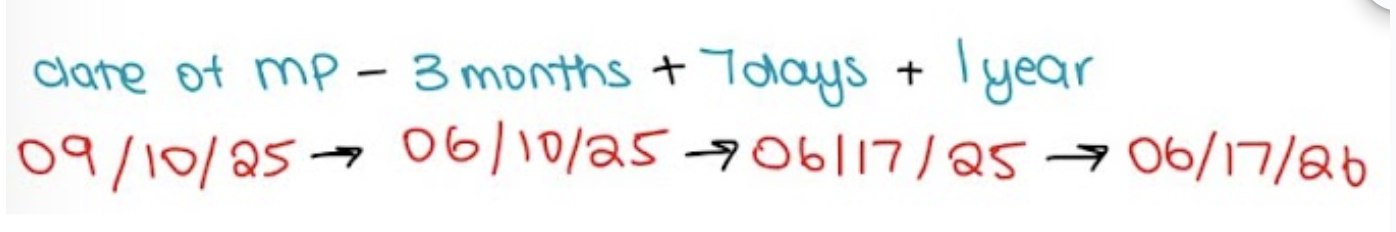
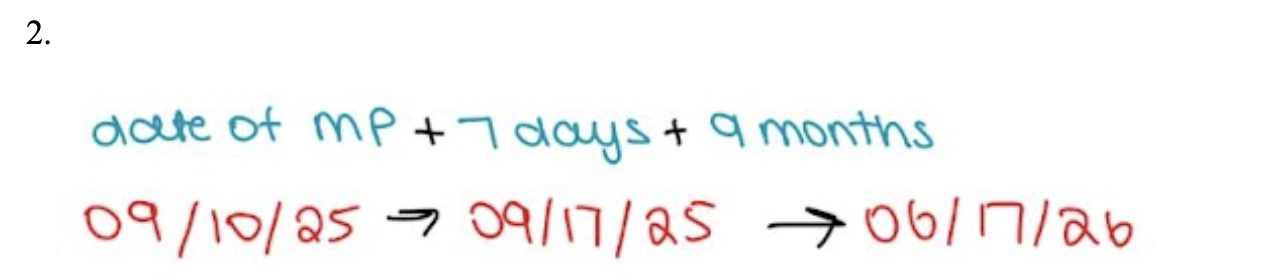
what are the 2 formulas (Nagele’s Rule) for EDB Calculation
Formula 1: LMP – 3 months + 7 days + 1 year
Formula 2: LMP + 7 days + 9 months
PRACTICE using formula 1: Ren tells you that she got a positive pregnancy test, and her LMP was September 10th , 2025. She asks you what the baby's due date will be
LMP = sep 10/25
-3 = june 10/25
+7 = june 17/25
+1 = june 17/26
PRACTICE using formula 2: Ren tells you that she got a positive pregnancy test, and her LMP was September 10th , 2025. She asks you what the baby's due date will be
LMP = sep 10/25
+7 = sep 17/25
+9 = june17/26
ANATOMY OF THE UTERUS: what location and shape is the uterus
Muscular organ, upside-down pear shape.
Lies midline in the pelvis, between bladder (front) and rectum (back), above the vagina.
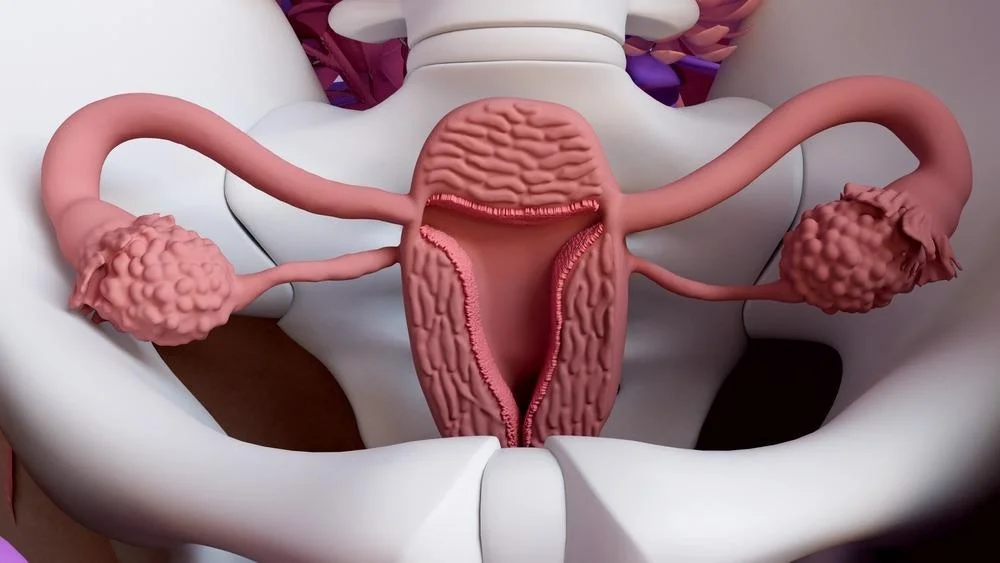
ANATOMY OF THE UTERUS: what are the main functions of the uterus (4+1)
Reception, implantation, retention, and nutrition of fertilized ovum/fetus. (RIRN)
Contracts to expel a fetus during birth.
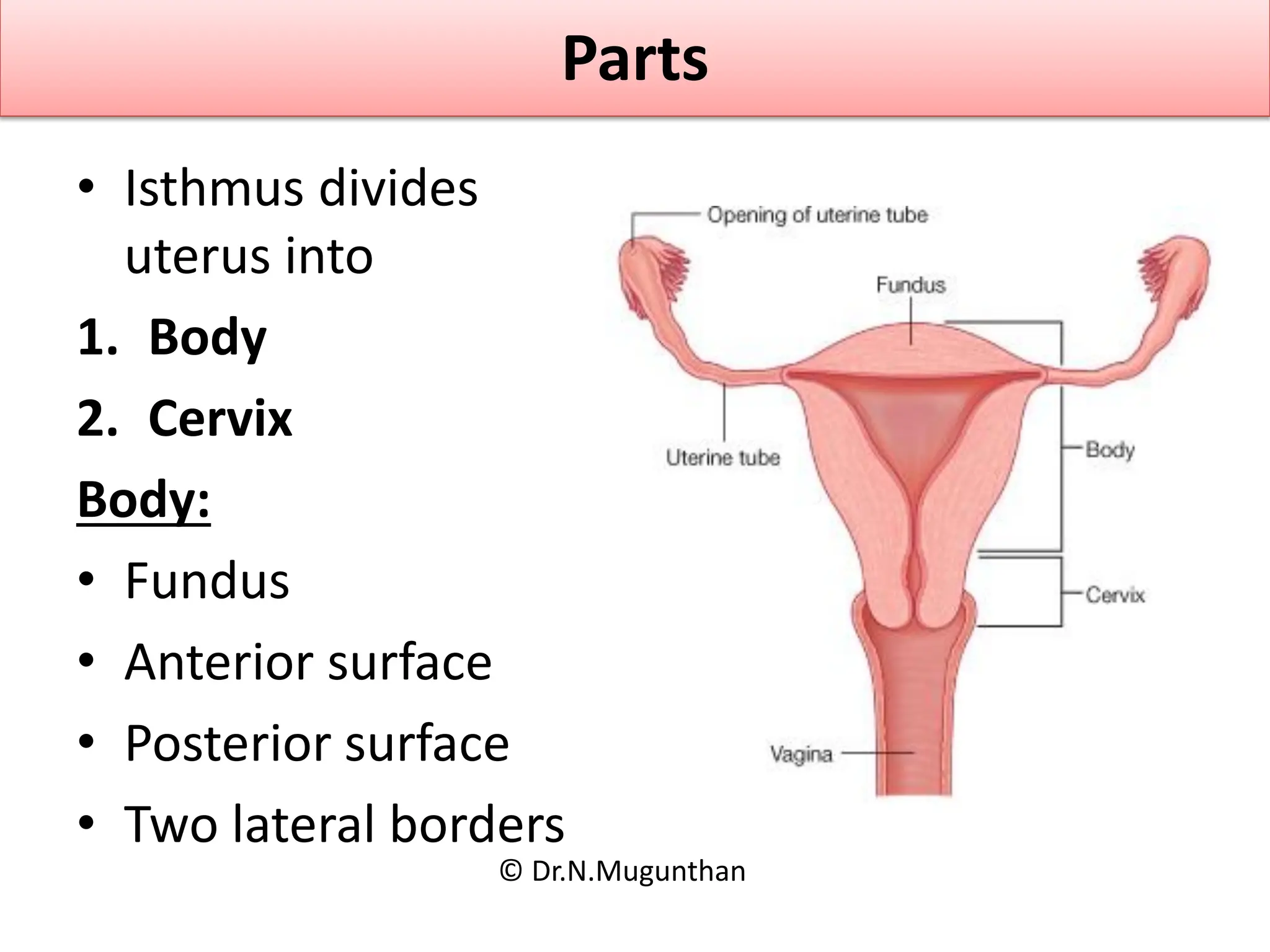
ANATOMY OF THE UTERUS: what are the main parts of the uterus
Parts:
Corpus = upper 2/3 (includes Fundus + body)
Cervix = lower cylindrical portion.
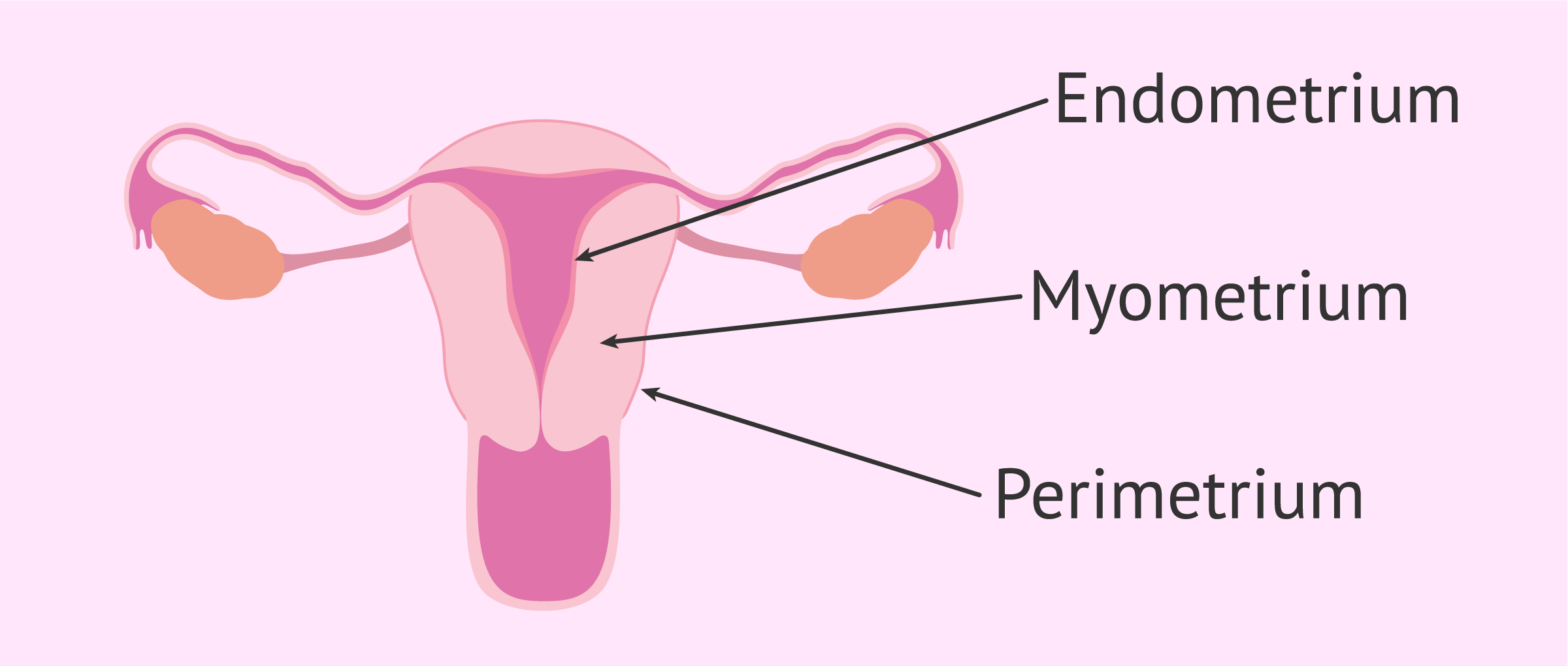
ANATOMY OF THE UTERUS: what are the main walls of the uterus
Uterine Wall Layers:
Endometrium – inner vascular lining, sheds in menstruation, thickens for implantation.
Myometrium – smooth muscle fibers arranged in 3 directions: longitudinal, transverse, oblique.
Continuous with supportive ligaments (adds strength & elasticity).
Crucial for powerful contractions in labor.
Peritoneum – outer serosal layer.
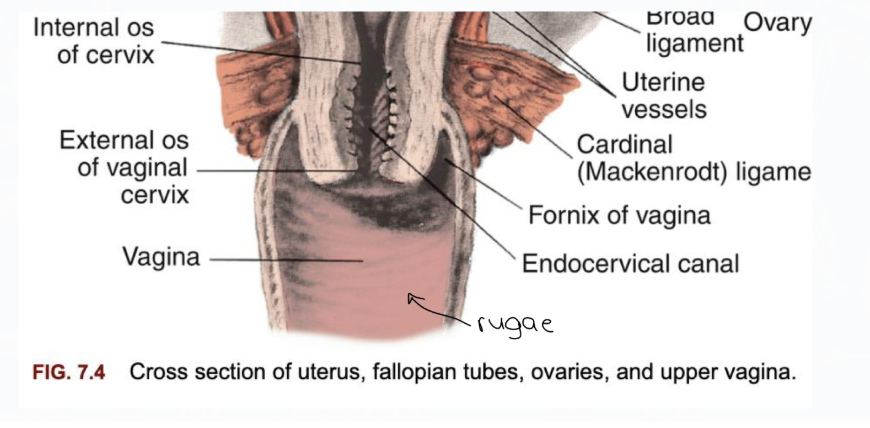
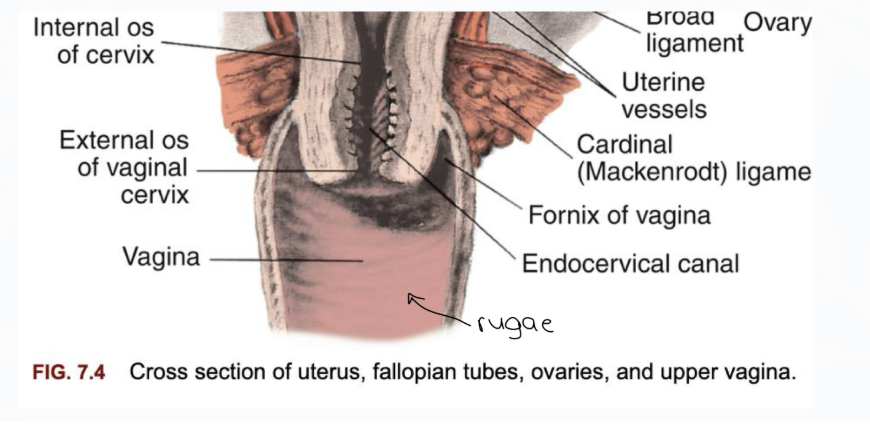
ANATOMY OF THE CERVIX: what are the main structures (+openings) of the cervix
Structure:
Made of fibrous connective & elastic tissue → flexible but strong.
Allows significant stretching during childbirth (like cartilage).
Openings (os):
Internal os – connects uterine cavity to cervical canal.
External os – connects cervical canal to vagina.
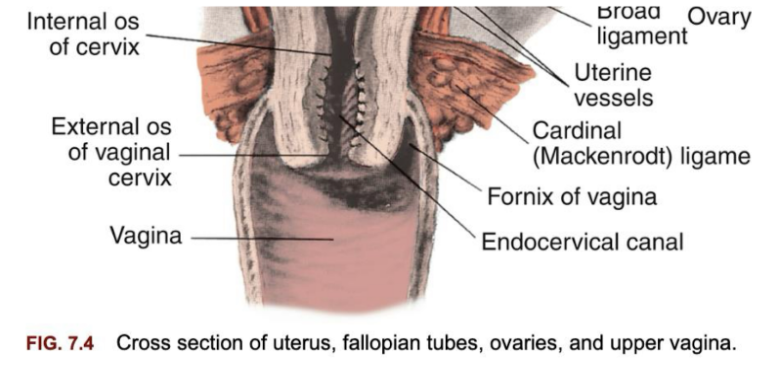
ANATOMY OF THE CERVIX: what is the function/clinical relevance of the cervix
Clinical Relevance:
Cervical dilation (widening of external os) measured in cm during labor.
Cervix consistency & effacement (thinning) are key signs of readiness for birth.
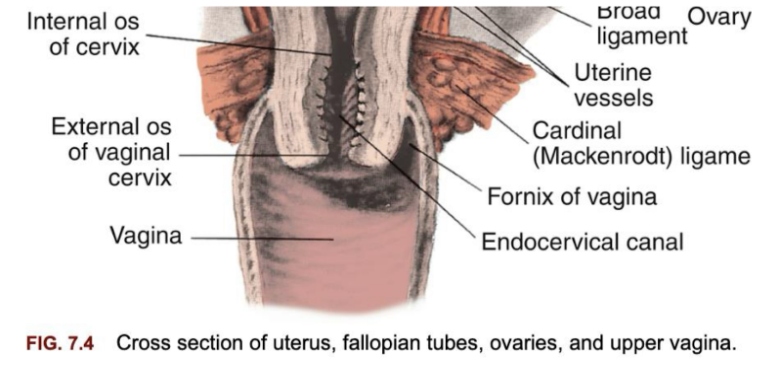
ANATOMY OF THE VAGINA: what are the main structures of the vagina
Structure:
Fibromuscular, tubular canal (~7–10 cm).
Located between bladder (anterior) & rectum (posterior).\
Extends from vulva → cervix/uterus.
Lining:
Mucosa with transverse folds (rugae) → allow stretching during childbirth.
Estrogen-dependent thickening during reproductive years.
ANATOMY OF THE VAGINA: what is the function/clinical relevance of the vagina
Functions:
Passage for menstrual flow.
Organ of copulation (sexual intercourse).
Part of birth canal.
ANATOMY OF THE PELVIS: what are the main structures of the pelvis
Bones:
Ilium, ischium, pubis, sacrum, coccyx.
United at joints: symphysis pubis, sacrococcygeal, sacroiliac joints.
Divisions:
False pelvis – upper, above pelvic brim; supports uterus as it enlarges.
True pelvis – lower curved bony canal; dimensions critical for childbirth.
Key Landmarks (True Pelvis):
Pelvic inlet (brim) → entry for fetal head.
Pelvic cavity → curved canal pathway.
Pelvic outlet → exit; bounded by
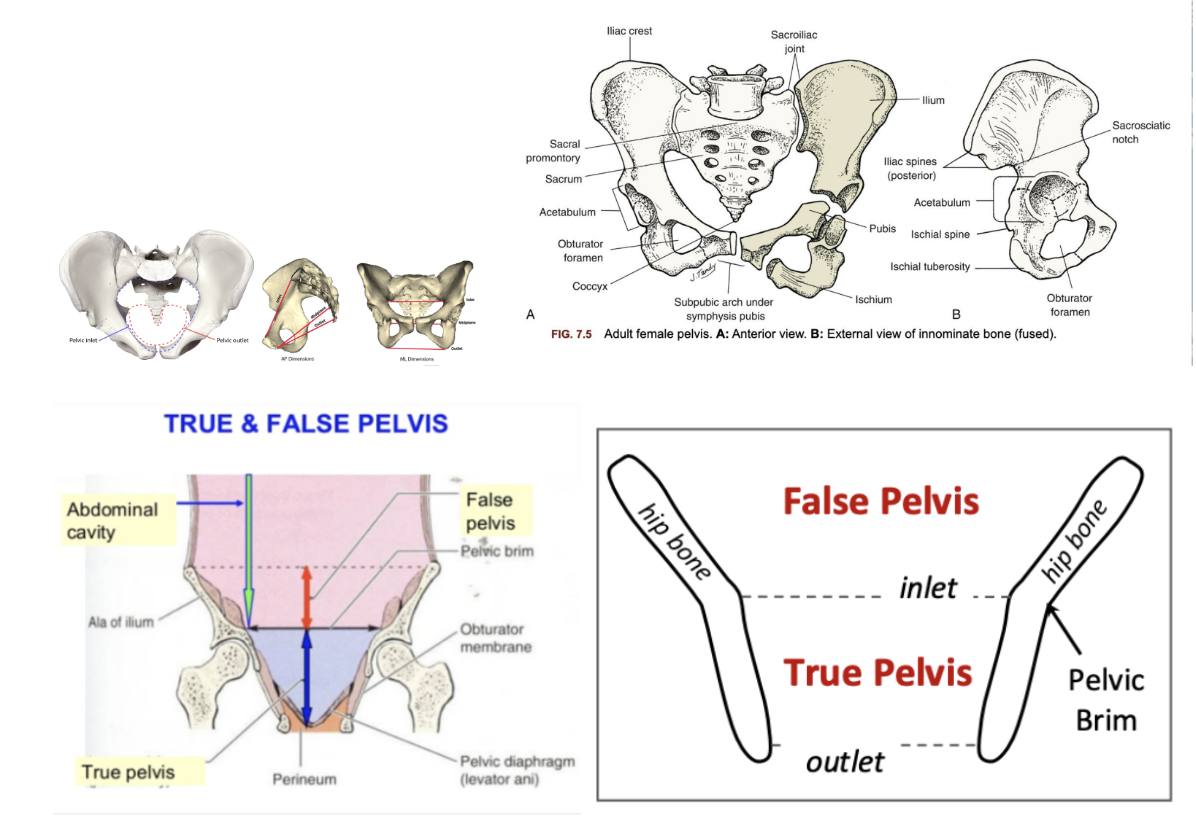
ischial tuberosities & coccyx.
ANATOMY OF THE PELVIS: what are the function/clinical relevance of the pelvis
Functions:
Protects pelvic organs.
Supports & shifts to accommodate fetus.
Anchors pelvic support structures (ligaments, muscles).
RECALL: Trophoblasts = the outer layer → placenta & membranes.
blastomeres
morula
blastocyst (with inner ball of blastomere and fluid surrounding)
blastomere reorganize to be Trophoblasts OR Embryoblasts
How to the trophoblasts further develop durung placental development
The placenta starts when the trophoblast (outer cells of the blastocyst) attach to the uterine lining - creating chorionic villi.
These cells differentiate into types of trophoblast that dig deeper into the uterus, creating a strong blood supply for the baby.
Cytotrophoblast (inner cellular layer) - keeps dividing to replenish syncytiotrophoblast.
Syncytiotrophoblast (outer multinucleated layer) → invasive, allows embedding into endometrium, Produces hCG, progesterone, estrogen. (just like the corpus luteum)
a third type is also differentiated; Extravillous trophoblast (EVT) = Special cells that leave the villi and invade into mom’s uterus. Two types:
Interstitial EVT → invade into the decidua basalis (endometrium maternal lining) & even part of myometrium → anchor placenta.
Endovascular EVT → invade maternal spiral arteries, breaking down their walls so blood flows directly into intervillous spaces (big maternal blood pools around villi).
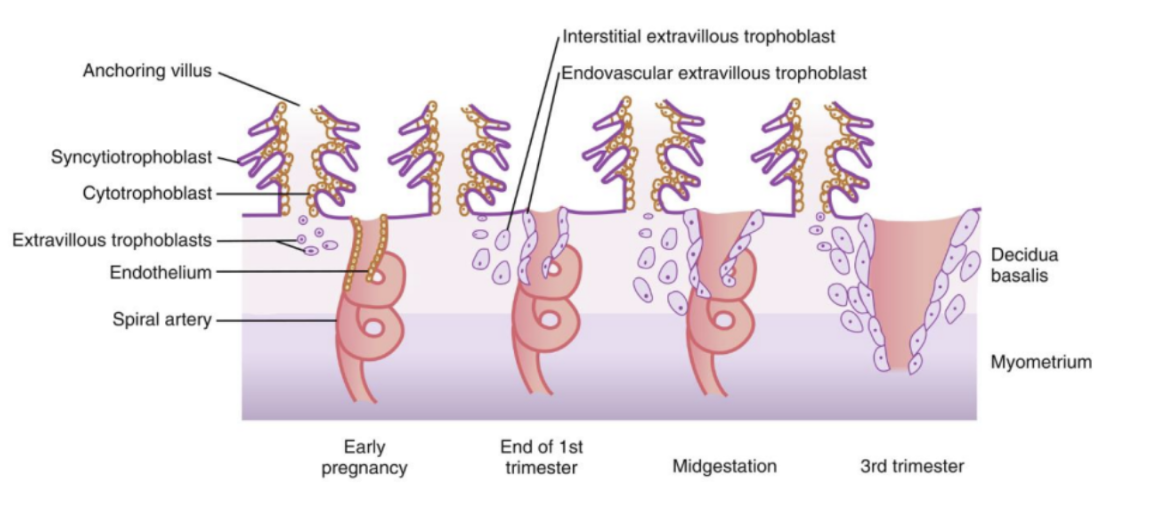
what is Decidua basalis
maternal side of placenta (the modified endometrium where implantation occurred).
what is Spiral arteries
coiled maternal arteries that supply blood to uterus; remodelled by EVTs so blood gushes freely to nourish baby.
what is Endothelium
inner lining of mom’s blood vessels.
what is Cotyledons
Placenta organized into lobes (functional units) each with fetal blood vessels.
when is circulation established in mother + baby
Maternal–placental–fetal circulation established by day 17, when fetal heart starts beating.
when is the placenta done growing
Structure complete by week 12.
Grows until 20 weeks, then thickens rather than enlarges.
what are the 3 main functions of the placenta
Endocrine Gland
Produces hormones to maintain pregnancy:
hCG (beta-hCG): maintains corpus luteum until placenta takes over. Basis of pregnancy tests.
Progesterone & Estrogen: support uterine lining, suppress contractions, promote growth.
Miscarriage can occur if corpus luteum fails before placenta (hormone production is sufficient)
Metabolic Functions
Respiration: O₂ to fetus, CO₂ back to mother
Nutrition: Transfers glucose, amino acids, fatty acids, vitamins, minerals.
Excretion: Removes fetal waste (urea, bilirubin, CO₂).
Storage: Stores nutrients (iron, protein, glycogen, calcium) for fetal use.
Transport of Substances
Good: O₂, water, nutrients.
Bad (can cross): alcohol, nicotine, drugs, viruses (e.g. HIV, rubella), carbon monoxide.
Glucose requires active transport because the fetus uses it so rapidly.
What is the formation of the umbilical cord
Formation:
Early pregnancy → connecting stalk links embryo to trophoblast.
By week 5 → stalk pulled to ventral side → becomes umbilical cord.
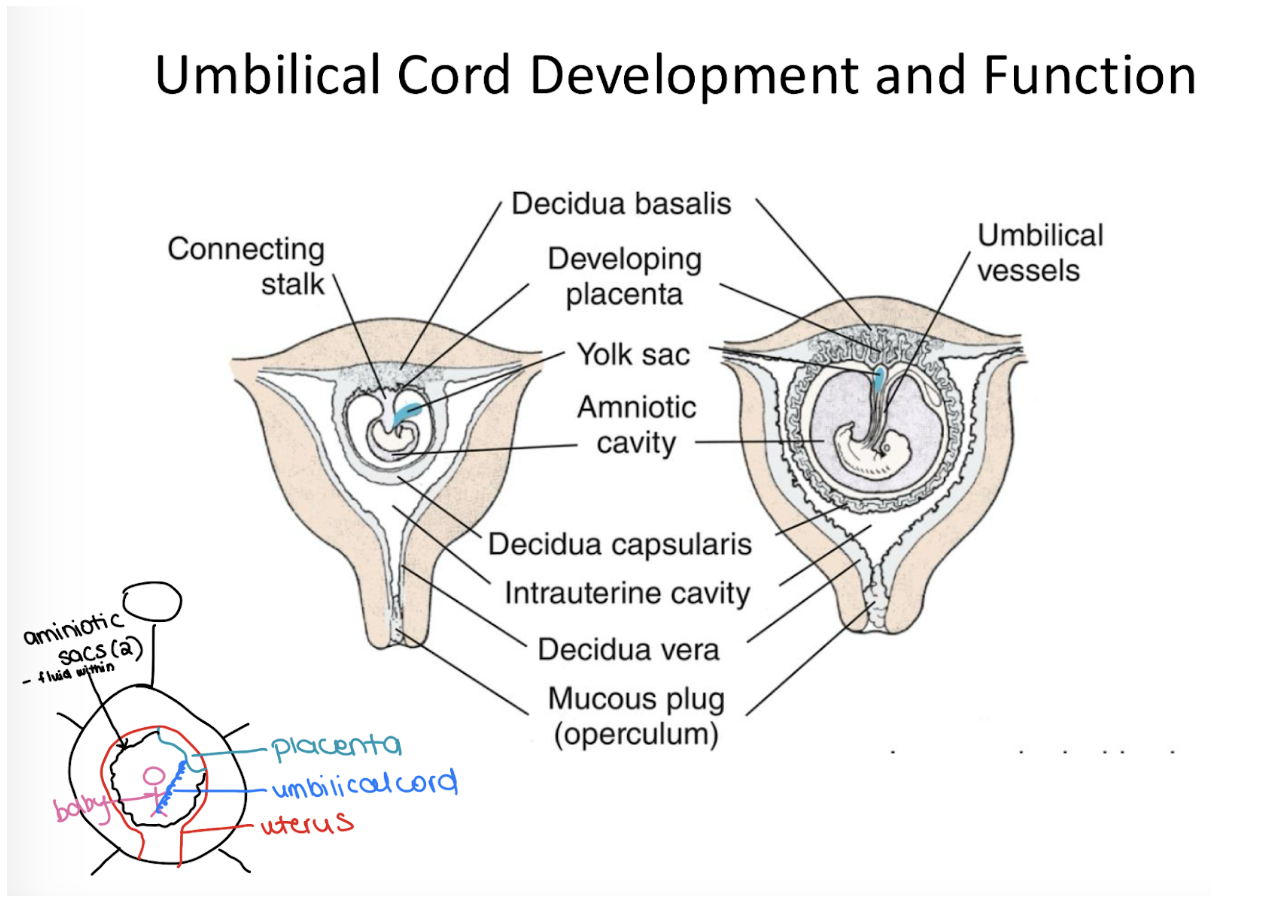
How many vessels in the umbiical cord? how it is protected?
Vessels:
2 arteries → carry deoxygenated blood AWAY from fetus.
1 vein → carries oxygenated blood TO fetus.
Protected by Wharton’s jelly (thick connective tissue preventing vessel compression).
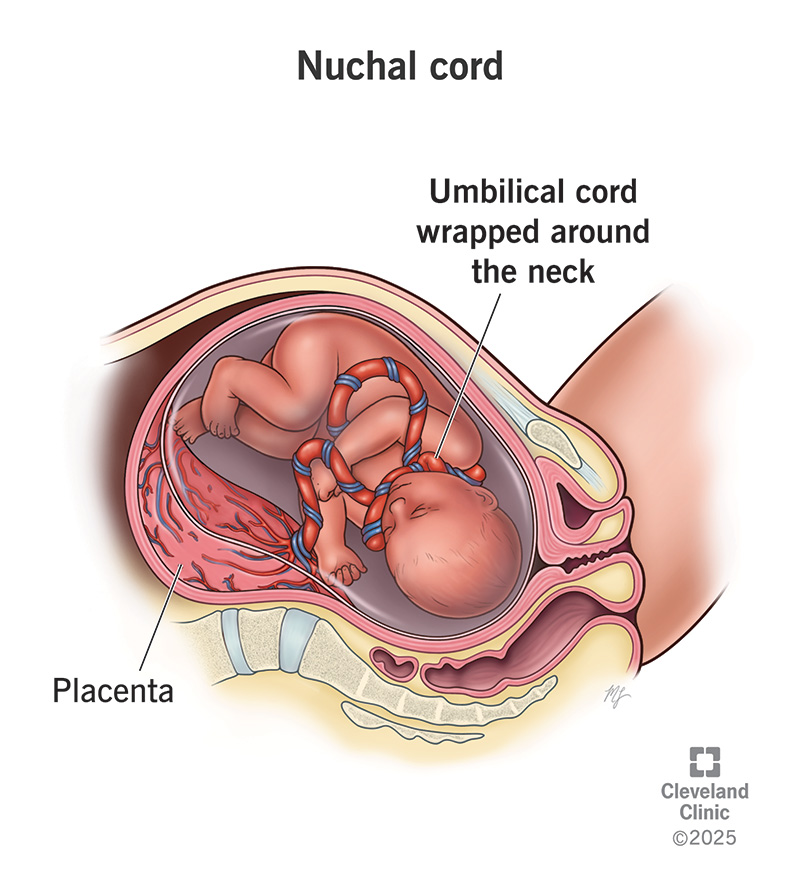
variation/issues of the umilical cord
Variations/Issues:
Two-vessel cord (instead of 3) → may signal anomalies.
Knots:
True knot (rare, can cut circulation).
False knot (appearance only).
Nuchal cord: Cord wrapped around neck — common, usually not harmful unless tightly constricting.
What is the aminotic fluid
Amniotic Fluid (700–1000 mL at term):
Early: formed from maternal blood plasma (diffusion).
After 11 weeks: fetus contributes by urination and lung fluid secretion.
Constantly circulates as fetus swallows and “breathes” it.

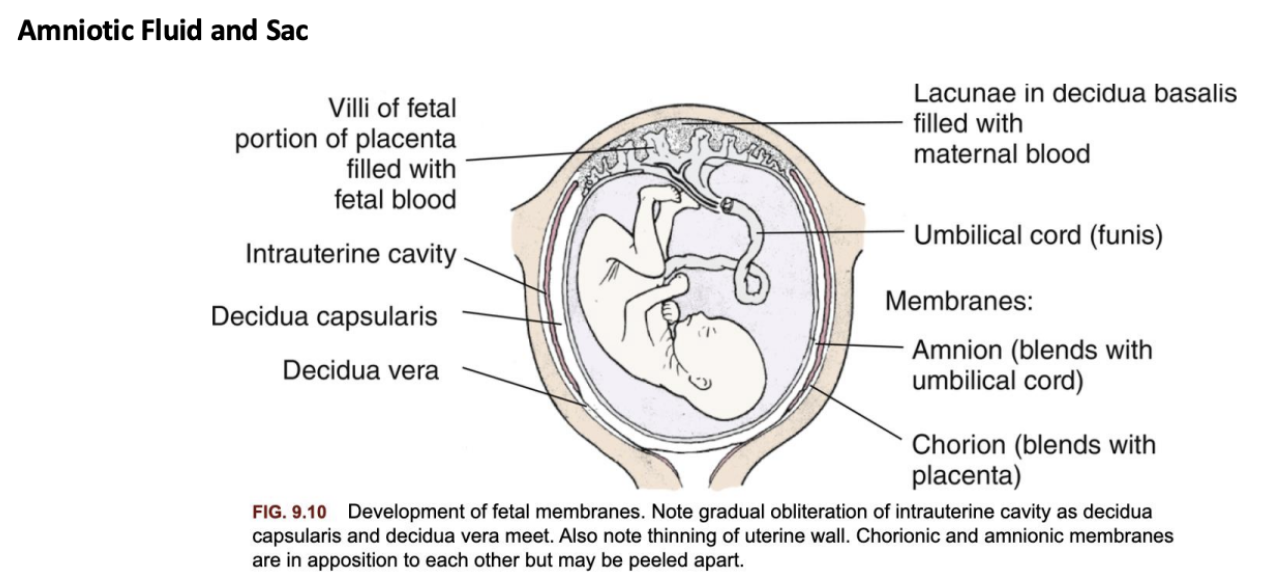
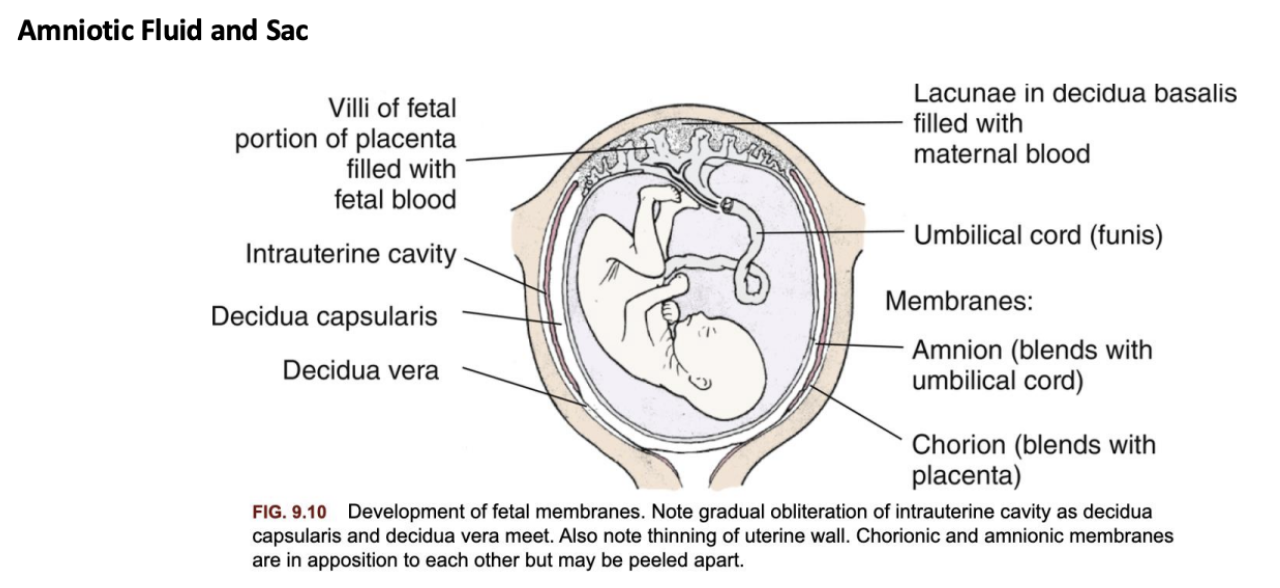
What are the main structures/membranes of the amniotic sac
Membranes:
Chorion: outer membrane, merges with placenta.
Amnion: inner membrane, lines amniotic cavity and covers umbilical cord.
By 2nd trimester → chorion + amnion fuse.
what is the function of amniotic fluid
Functions:
Maintains constant temperature.
Cushions fetus from trauma.
Provides freedom of movement → muscle & skeletal development.
Barrier to infection.
Supports lung development (fetal “practice breathing”).
Prevents amniotic band syndrome (entanglement in membranes).
What are abnormal volumes of amniotic fluid at term
Oligohydramnios (<300 mL): associated with renal problems, growth restriction.
Polyhydramnios (>2000 mL): linked to GI malformations (baby can’t swallow fluid properly), maternal diabetes
What are the 5 tasks to maternal adaptation during pregnancy
Tasks of Maternal Adaptation:
Accepting the Pregnancy
First step in emotional adaptation.
May feel ambivalent (mixed emotions), especially early on.
Acceptance increases as pregnancy becomes more visible and movements are felt.
Identifying with the Role of Mother
Begins imagining herself as a mother.
Draws on own childhood experiences, cultural norms, and role models.
May feel conflict between personal identity and new maternal role.
Reordering Relationships
Must renegotiate dynamics with partner, family, and friends.
Supportive relationships reduce stress, while strained ones may increase anxiety.
Establishing Relationship with the Unborn Child
Quickening (first fetal movement, ~16–20 weeks) often deepens bonding.
Talking to baby, imagining the baby’s features, preparing for baby’s arrival.
Preparing for Birth
Gathering information about labor, delivery, and postpartum.
Attending prenatal classes, birth plans, hospital tours.
Involves both practical (packing, shopping) and emotional preparation.
What are the 5 tasks to paternal adaptation during pregnancy
Accepting the Pregnancy
Reactions vary: excitement, pride, worry, or even denial at first.
Involvement often grows as the pregnancy becomes more tangible.
Identifying with the Father Role
Begins to imagine himself as a caregiver and protector.
May recall own experiences with his father.
Reordering Relationships
Adapts relationship with partner as attention shifts to pregnancy.
May feel pressure to be provider, supporter, or “strong” for the mother.
Establishing Relationship with the Fetus
Bonding increases after hearing heartbeat or feeling baby move.
Talking/singing to the baby, attending ultrasounds.
Preparing for Childbirth
Learning about labor, pain management, and support roles.
Worries about being helpful during delivery.
what are the 3 things sibling adaptation is based on
The arrival of a baby can feel like a crisis for children, leading to feelings of jealousy or fear of being replaced. Adaptation depends on:
Child’s age
Parental attitudes and preparation
Separation from mother during hospital stay
How might children react (by age group age 1-teen)
1 year old → Largely unaware of pregnancy.
2 years old → Notices changes in mother’s body but needs routine/sameness, so may not fully grasp it.
3–4 years old → Curious; enjoy hearing about their own birth, listening to heartbeat, or feeling fetus move.
School-aged (6–12 yrs) → Show clinical interest; may role-play being mother or father
Early/Middle Adolescents → Preoccupied with own identity/sexuality; may see parents as “too old” to be having a baby.
Late Adolescents → More mature; often comforting and supportive toward parents.