Endocrinology
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
Thyroid antibodies?
TSH receptor - Graves
Anti-TPO - Hashimoto’s, graves
Anti-Tg - graves, hashimoto’s, thyroid cancer
Types of thyroiditis? Is thyroiditis hyper or hypothyroidism?
Hypothyroidism (can cause hyper in acute phase)
De Quervain’s
Hashimoto’s
Post-partum
Drug-induced - lithium, amiodarone
Riedel’s - painless goitre
De Quervain’s thyroiditis signs? Investigation? Management?
3 phases – hyperthyroid phase has flu-like illness.
Associated with painful goitre and raised ESR.
Ix thyroid scintigraphy – globally reduced uptake of iodine-131.
Usually self-limiting, can give NSAIDs or steroids if severe.
Hashimoto’s thyroiditis - associated conditions?
T1DM, Addison’s, pernicious anaemia, coeliac, vitiligo, development of MALT lymphoma
Subclinical hypothyroidism - TFTs? Management as per NICE?
High TSH, normal T4 - “on the way” to developing hypothyroidism (would also get same results in poor thyroxine compliance)
If TSH above 10 on 2 occasions 3 months apart – consider offering levo
If TSH 5.5-10 on 2 occasions 3 months apart and there are symptoms and pt under 65 – consider 6-month trial levo. If older or asymptomatic – watch and wait, repeat TFTs in 6 months
Sick euthyroid TFTs?
T3 and T4 low, TSH usually normal, but inappropriately normal given low thyroxine and T4
Hypothyroidism treatment? Following dose change, when should TFTs be checked? If woman becomes pregnant how should dose be adjusted?
Levothyroxine
Following change in dose – TFTs should be checked in 8-12 weeks.
If woman becomes pregnant – dose should be increased by 25-50 micrograms.
Hyperthyroidism treatment? Main SE of treatment?
Propranolol to control symptoms.
Carbimazole (usually for 6 weeks until euthyroid then dose reduced) – agranulocytosis
Thyroid cancer most common type? Prognosis of this? Monitoring for papillary/follicular carcinoma? Monitoring for medullary carcinoma?
Most common is papillary – young females - excellent prognosis
For papillary/follicular carcinoma, after treatment – yearly thyroglobulin levels to detect early recurrent disease.
For medullary carcinoma – check calcitonin and CEA to monitor.
Thyroid storm treatment? Myxoedema coma treatment?
Thyroid storm - hydrocortisone, IVI, PTU
Myxoedema coma - confusion and hypothermia. IV thyroid replacement, IVI, IV steroids until possibility of coexisting adrenal insufficiency excluded.
Cushing’s syndrome blood gas findings? Basic tests?
General findings – hypokalaemic metabolic alkalosis, impaired glucose tolerance
Can do 24hr urinary free cortisol or bedtime salivary cortisol – need 2 measurements for both
Cushing’s syndrome dexamethasone suppression tests?
Low dose overnight test – 1st line
- 1mg at night. Check 9am cortisol and ACTH. If ACTH suppressed – non-ACTH dependent cause likely.
Low dose 48hr test
- 0.5mg every 6 hours 8 doses starting 9am. Check cortisol before and end. Normal = suppressed.
High dose 48hr test – to determine cause once confirmed
- Same as last one but 2mg instead. High enough to suppress Cushing’s disease but not adrenal adenoma or ectopic ACTH.
· Check ACTH – low in adrenal tumour, high in pituitary/ectopic ACTH
What is pseduo Cushing’s? How to differentiate between this and actual Cushing’s?
Pseudo Cushing’s – alcohol excess, severe depression. Causes false positive dexamethasone suppression test or 24hr urinary free cortisol.
Insulin stress test may be used to differentiate.
Hyperaldosteronism - causes of primary and secondary? Tests to diagnose? Management?
Primary – bilateral adrenal hyperplasia, adrenal adenoma (conn’s), familial
Secondary – RAS, HF, LF
1st line – aldosterone:renin ratio – high aldosterone, low renin (negative feedback due to sodium retention from aldosterone)
Following this, CT abdo and adrenal vein sampling used to differentiate between unilateral and bilateral cause. If CT normal, AVS can be used to distinguish between unilateral adenoma and bilateral hyperplasia.
Management – adrenal adenoma = adrenalectomy. Bilateral adrenocortical hyperplasia – spironolactone.
Adrenal insufficiency - primary vs secondary vs tertiary? Test? What to do in acute illness?
Primary = Addison’s (autoimmune) – 21-hydroxylase antibodies
Secondary = low ACTH
Tertiary = low CRH – exogenous steroids
Short synacthen test
- Check cortisol before and 30 and 60mins after – should double
- If not, primary AI or adrenal atrophy due to secondary AI
- Check ACTH directly to distinguish
Acute illness – double dose of glucocorticoid, same dose of fludrocortisone
Acromegaly tests? Treatment?
IGF-1 raised → then confirm with following test
GH suppression test – 75g glucose drink – check GH before and 2 hours after. Failure to suppress = acromegaly.
Trans-sphenoidal surgery is first-line treatment
Pegvisomant – GH receptor antagonist – daily subcut injection
Somatostatin analogues (octreotide) and dopamine agonists block GH release
(Prolactinoma – dopamine agonists before surgery)
Hyperparathyroidism - blood results in primary vs secondary vs tertiary?
Primary – tumour – high PTH (can be normal), high calcium
(Patients not suitable for surgery may be treated with cinacalcet)
Secondary – low vit D/CKD causing hypocalcaemia – high PTH, low/normal calcium
Tertiary – hyperplasia – very high PTH, moderately high calcium
Hypoparathyroidism - what is primary? Symptoms? Treatment? What is pseudo…? How to diagnose? What is pseudopseudo…?
Primary – decreased PTH secretion. Low PTH, low calcium, high phosphate. Treated with alfacalcidol.
Sx secondary to hypocalcaemia – tetany, perioral paraesthesia, Trousseau’s sign, Chvostek’s sign. Prolonged QT on ECG.
Pseudohypoparathyroidism – target cells insensitive to PTH. High PTH, low calcium, low phosphate.
- Diagnosis – measure urinary cAMP and phosphate levels following PTH infusion. In hypoparathyroidism – will cause increase in cAMP and phosphate, In pseudo type I neither increased and pseudo type II only cAMP rises.
Pesudopseudohypoparathyroidism – similar to above but normal biochemistry.
SIADH urine and serum osm? Main causes? Ix? Management?
Euvolemic hyponatremia
Main causes – post-op, SSRI, SCLC
CXR – if no cause – CT TAP
High urine osmolality, high urine sodium, low serum osmolality
Fluid restrict
Correct sodium slowly – osmotic demyelination syndrome – no more than 10mmol/L change in 24 hours
Demeclocycline
Diabetes insipidus - urine and serum osm? Causes of the 2 types? Test to diagnose?
Polyuria >3L a day
Low urine osmolality, high/normal serum osmolality
Nephrogenic – lithium can cause
Cranial – sheehan’s syndrome can cause
Desmopressin stimulation test
- No fluids for 8 hours → measure urine osmolality
- If low – give desmopressin and measure 2-4 hours later
- Primary polydipsia – after WD, urine osmolality high – no need to continue
- Cranial DI – after WD, urine osmolality low. After desmopressin – high.
- Nephrogenic DI – after WD, urine osmolality low. After desmopressin – still low.
Diabetes Mellitus diagnosis? Antibodies? When would you do C-peptide/antibody testing?
DM – fasting glucose >7, random glucose >11.1 and symptomatic = diagnosis. If asymptomatic then same numbers but on 2 separate occasions.
Antibodies in T1DM – anti-GAD, Islet cell antibodies, insulin autoantibodies (correlates with age)
C-peptide/antibody testing if suspecting T1DM but atypical features e.g. age over 50, BMI over 25, slow hyperglycaemia
What is impaired fasting glucose? What is impaired glucose tolerance?
Impaired fasting glucose = 6.1-7
Impaired glucose tolerance = fasting less than 7 and OGTT 2-hour value 7.8-11.1
If IFG then do OGTT. If result 7.8-11.1 then IGT, but no diabetes.
What would cause lower than expected and higher than expected levels of HbA1c?
Lower than expected levels of HbA1c = sickle-cell anaemia, G6PD def, hereditary spherocytosis, haemodialysis
Higher than expected levels of HbA1c = vitamin B12/folic acid def, IDA, splenectomy
In T1DM when would you consider adding metformin?
If BMI >25
Diabetes Ramadan rules for metformin, sulfonylureas and pioglitazone?
Metformin – 1/3 before suhoor, 2/3 after iftar
Switch OD sulfonylureas to after iftar. If taking BD preps take larger proportion after iftar
No adjustment needed for pioglitazone
DKA diagnosis criteria? Management?
Hyperglycaemia >11 or known DM, ketosis >3, acidosis pH <7.3, bicarb <15
Fluids, initially isotonic saline – 1L in first hour, then 1L every 2 hours
IV insulin infusion 0.1 unit/kg/hr
Once BG <14 start 10% dextrose infusion at 125mls/hr in addition to the saline
May need potassium up to 20 per hour unless cardiac monitoring
Continue long acting insulin, stop short acting
DKA resolution? When would you request senior endocrine review? When can you switch to SC insulin?
DKA resolution:
- pH >7.3 AND blood ketones <0.6 AND bicarb >15
If ketonemia and acidosis don’t resolve within 24hrs – senior endo review
If above criteria met and patient eating and drinking – switch to SC insulin
T2DM stepwise management 1st, 2nd , 3rd line? What if triple therapy fails?
Lifestyle modifications
HbA1c target is 53 if on any drug which can cause hypoglycaemia
Metformin
Once settled, add SGLT2-I if existing CVD/HF or high risk CVD
If HbA1c then rises to 58 – need further treatment
Add sulfonylurea, pioglitazone, DPP4-I, SGLT2-i
Triple therapy – metformin + 2 of above or insulin
If fails and BMI >35 or <35 but insulin would severely affect occupation or weight loss would be very beneficial – switch one to GLP-1 mimetic – liraglutide (should only be added to insulin under specialist care)
If starting insulin continue metformin but review need for other drugs. Start with isophase, intermediate-acting
Metformin - how does it work? SEs? Does it cause hypos?
- Biguanide
- Increases insulin sensitivity and decreases glucose production
- No weight gain or hypoglycaemia
- SEs – GI sx – can switch to modified release
SGLT2-i - how does it work? SEs? Does it cause hypos?
- Blocks proximal tubule transporter that reabsorbs glucose
- Can cause hypoglycaemia
- SEs – glycosuria, thrush, increased urinating, DKA, Fournier’s gangrene
Sulfonylureas - example? How does it work? SEs? Does it cause hypos?
E.g. gliclazide
Stimulates insulin release from pancreas
SEs – weight gain and hypoglycaemia
Avoid in pregnancy and breastfeeding
Thiazolidinediones - example? How does it work? SEs? Does it cause hypos? CIs?
E.g. pioglitazone
Reduce insulin resistance and reduced glucose production
No hypoglycaemia
Weight gain, HF, fractures, small risk bladder cancer
CI in heart failure and fractures!
DPP-4 inhibitors - example? How does it work? SES? Does it cause hypos?
E.g. sitagliptin
Increase incretin activity
No hypoglycaemia
Headaches, low risk pancreatitis
GLP-1 mimetics - examples? SE? Justifying ongoing prescription?
Subcut injections 60 mins before morning and evening meals (liraglutide OD)
Reduce appetite, weight loss, GI sx, pancreatitis
Can be used in obese, non-diabetics to lose weight
1% reduction in HbA1c and 3% weight loss after 6 months to justify ongoing prescription
Meglitinides - how do they work? SEs? When are they used?
Increase insulin secretion
Often used if erratic lifestyle
SEs – weight gain, hypoglycaemia
Other drugs given in diabetes - erectile dysfunction? Gastroparesis?
ACE-i if ACR above 3 (30 in non-diabetics)
SGLT2-i if T2DM and CKD ACR >30
Phosphodiesterase-5 inhibitors – sildenafil – erectile dysfunction
Prokinetics for gastroparesis
Hyperosmolar hyperglycaemic state - how does it occur? Management?
Typically elderly with T2DM
Hyperglycaemia → increased serum osmolality → osmotic diuresis → severe volume depletion
Onset over days
Management – IV NaCl 0.5-1L per hour +/- potassium, insulin not given unless blood glucose stops falling, VTE prophylaxis as risk of thrombosis due to hyperviscosity
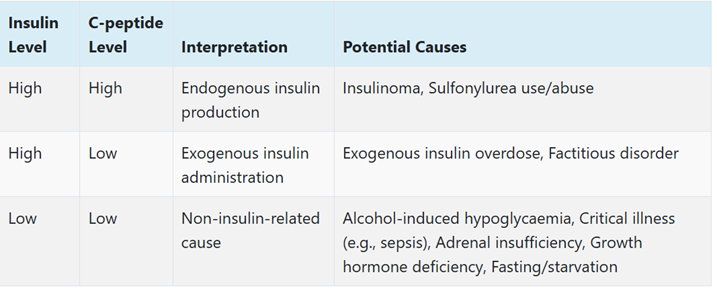
Hypoglycaemia causes - high insulin + high C-peptide? High insulin + low C-peptide? Low insulin + low C-peptide?
Phaeochromocytoma - investigation? Treatment?
Measure plasma free metanephrines and 24hr urinary metanephrines
Alpha blockers (phenoxybenzamine) then beta blockers – symptom control before surgery
MEN inheritance pattern? MEN 1 vs MEN 2a vs MEN 2b?
MEN 1 – 3Ps – Parathyroid (increased calcium), Pituitary, Pancreas (insulinoma, carcinoma – recurrent ulcers). Also adrenal and thyroid.
MEN 2a – medullary thyroid cancer and 2 Ps – parathyroid and pheochromocytoma
MEN 2b – medullary thyroid cancer and 1 P – pheochromocytoma, marfanoid body habitus, neuromas
Carcinoid syndrome symptoms/signs? Treatment?
Diarrhoea, flushing, hypotension, R sided heart murmurs
Treat with octreotide
Orlistat - how does it work? When can it be used? SEs?
Pancreatic lipase inhibitor
SEs – faecal urgency/incontinence, flatulence
BMI >28 with associated risk factors or BMI >30 or wt loss 5% at 3 months, normally used for <1 year.
Kallman syndrome inheritance pattern? Symptoms? Management?
- Hypogonadotropic hypogonadism. X-linked recessive.
- Delayed puberty, anosmia, LH/FSH levels low/normal, sex hormones low
- Management – testosterone supplementation
Klinefelter syndrome inheritance pattern? Symptoms? Diagnosis?
- 47, XXY
- Tall, lack of secondary sexual characteristics, small, firm testes, infertile, gynaecomastia
- Elevated gonadotropic levels, low testosterone
- Diagnosis – karyotype