ABO and H Blood Group Systems and Secretor Status
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
Landsteiner’s Rule (law)
Healthy individuals possess ABO antibodies to the ABO blood group antigens ABSENT from their RBCs
ABO Antigen
can be intrinsic to the RBC membrane or soluble (body fluids)
detected in the embryo as early as 5 to 6 weeks’ gestation
Newborns’ RBCs have fewer numbers and partially developed antigens
Full expression occurs at about 2 to 4 years of age
ABO and H Antigen Genetics
Genes at 3 separate loci influence presence of ABO antigens: ABO, H, Se
presence or absence of ABH antigens on RBC membrane = H gene
presence or absence of ABH antigens in secretions = Se gene
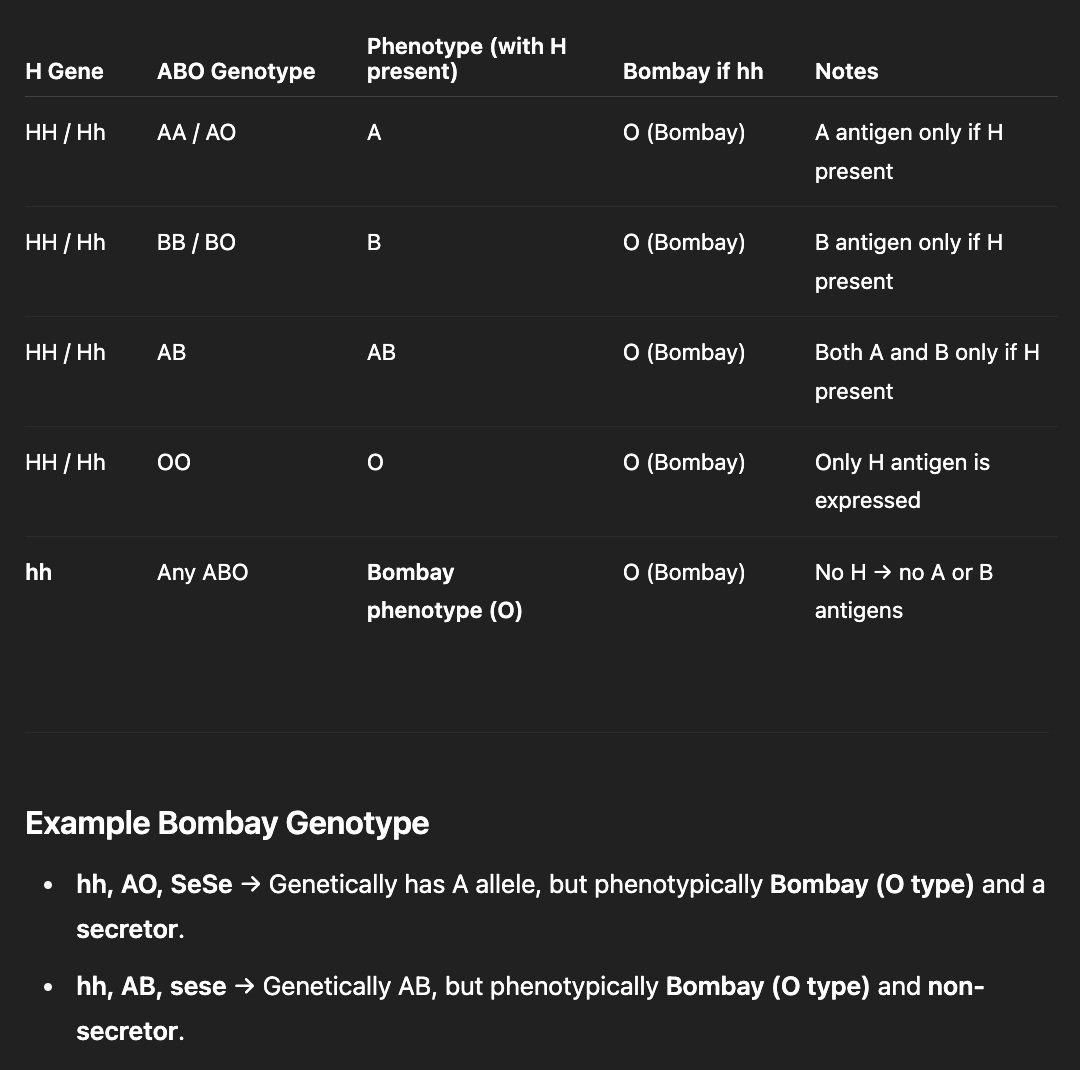
Genetics: H, Se, ABO genes
H Gene: H and h alleles (h is an amorph)
Bombay phenotype lacks H antigen (hh)
Se gene: Se & se alleles (se is an amorph)
ABO genes: A, B and O alleles
What is the basic precursor for RBC antigens, A, B and H?
Oligosaccharide Chain
Attached to a protein or lipid carrier molecule
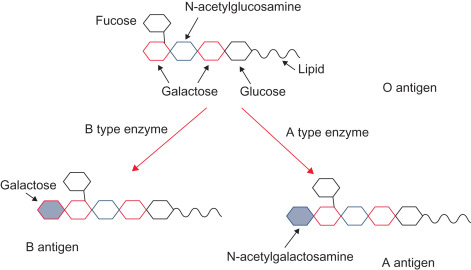
H Antigen
Foundation for A and/or B antigens
codes for glucosyltransferase
transfers the immunodominant sugar, L-fucose
A and B Antigens
“A” gene = transferase adds the immunodominant sugar, N-acetylgalactosamine, to H antigen (terminal sugar)
Gene Product: N-acetylgalactosaminyltransferase
“B” gene = transferase adds the immunodominant sugar, D-galactose, to H antigen (terminal sugar)
Gene Product: D-galactosyltransferase
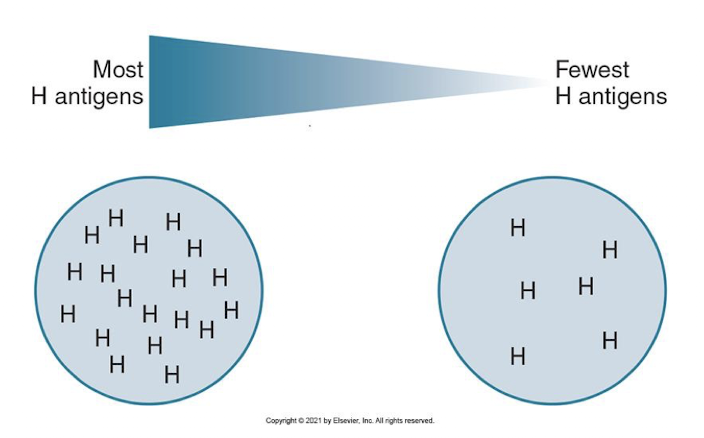
Antigen Concentration
Certain blood types possess more H antigen than others
Group O individuals have many H antigen sites because they have no A or B antigens
O > A2 > B > A2B > A2 > A1B
Subgroups of A Type: A1 and A2
Both react strongly w/ reagent anti-A (3+ to 4+)
Lectin Dolichos biflorous distinguishes A1 from A2 red cells
Agglutinates w/ A1, but NOT A2
80% of A or AB individuals are A1
20% are A2 & A2B
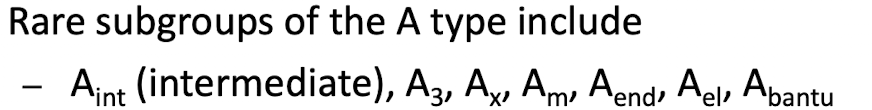
Rare subgroup of the A type may be present if:
Weak or no agglutination with commercial anti-A and anti-A,B occurs
Anti-A1 is present
Anti-H causes strong agglutination
What is more common, A or B subgroups?
A subgroups are more common than B subgroups; B subgroups typically react weakly with anti-B reagents.
Why is it important to identify subgroups?
Preventing transfusion rxns
If a weak subgroup is missed in a donor, the incorrect blood group could be given to the recipient
a group A subgroup in the donor is classified as group O. the group O recipient receives the unit, what will occur?
a transfusion reaction; the recipient’s anti-A antibody reacts with the donor cells
ABO Antibodies
Non-RBC stimulated, or naturally occurring
Ab production is unrelated to an RBC Ag
Results from exposure to A and B like Ags in the environment (e.g., normal bacterial flora)
When are ABO Abs detected?
may not be detected until 3 to 6 months of age
Titers reach max. levels by 5 to 10 yrs of age and DECREASE as an individual grows older
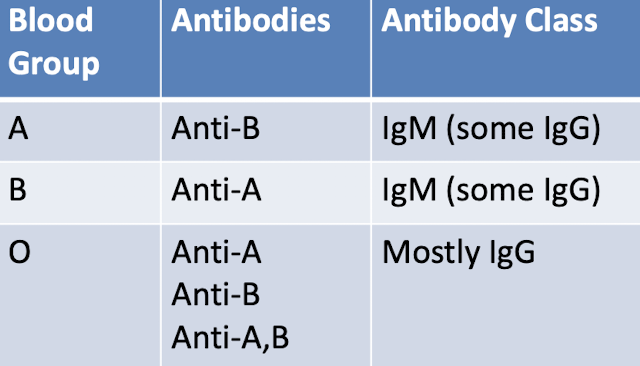
Clinical Significance of ABO Abs
most anti-A & anti-B in group A or B individuals are predominantly IgM → clinically significant bc they are able to bind complement
React optimally during immediate-spin (IS) crossmatching
Anti A,B antibody found in group O individuals
Cross reacts w/ both A and B Ags
ABO Antibody Class
Anti-A1 Antibody
Produced by subgroups of the A type
Has SPECIFICITY to the A1 antigen but will not agglutinate A2
Not clinically significant
May cause incompatible crossmatches on IS testing
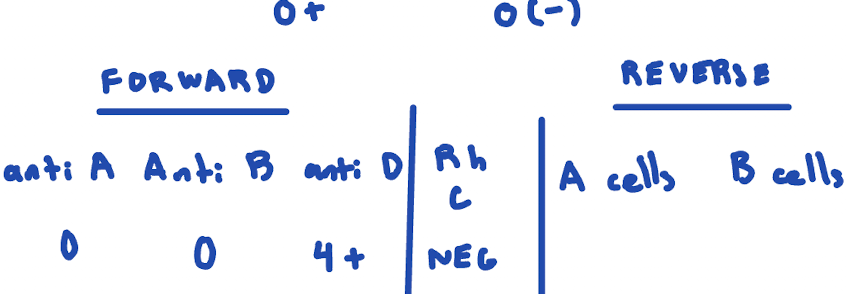
Routine ABO Phenotyping
Two components of ABO phenotyping, required testing on donor and recipient blood
Forward grouping
RBCs are tested for ABO antigens
Determines ABO phenotype
Reverse grouping
Serum or plasma is tested for ABO antibodies
Acts as a control for RBC testing
ABO Phenotype Reactions
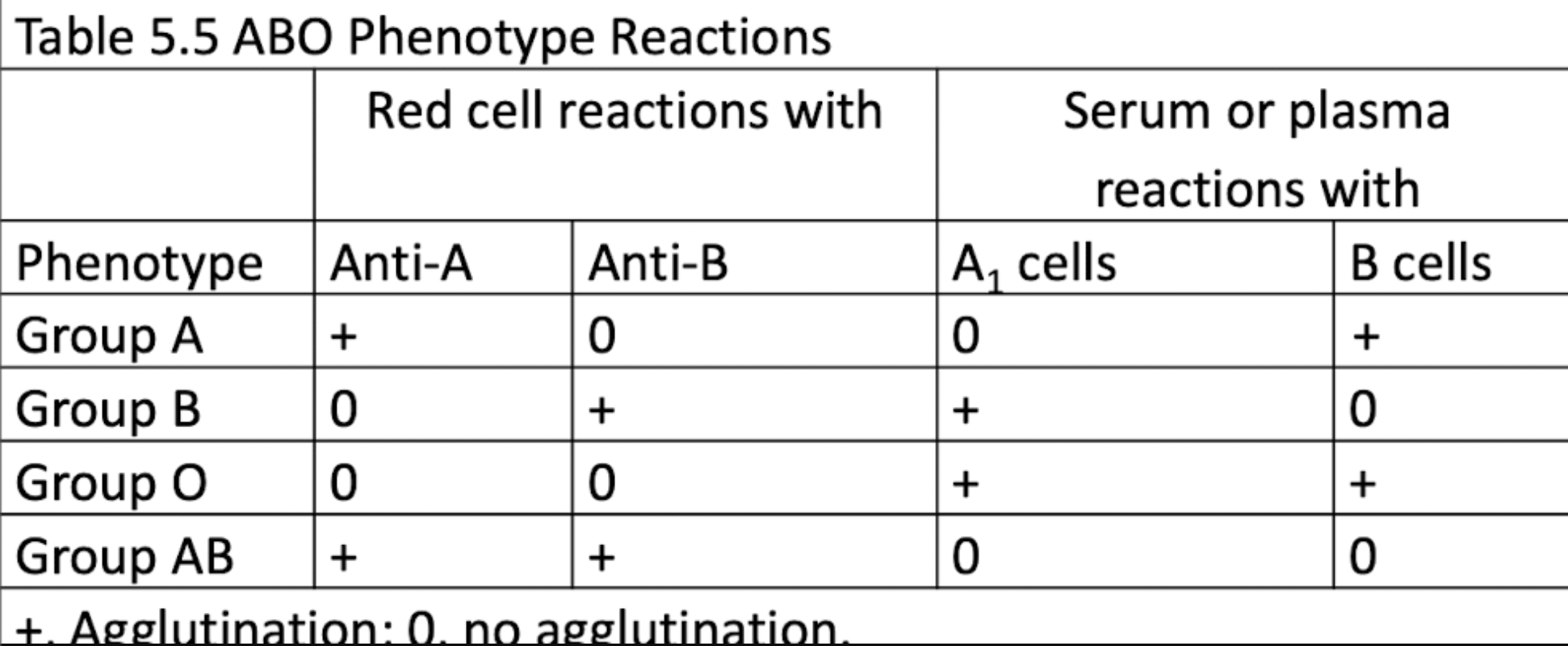
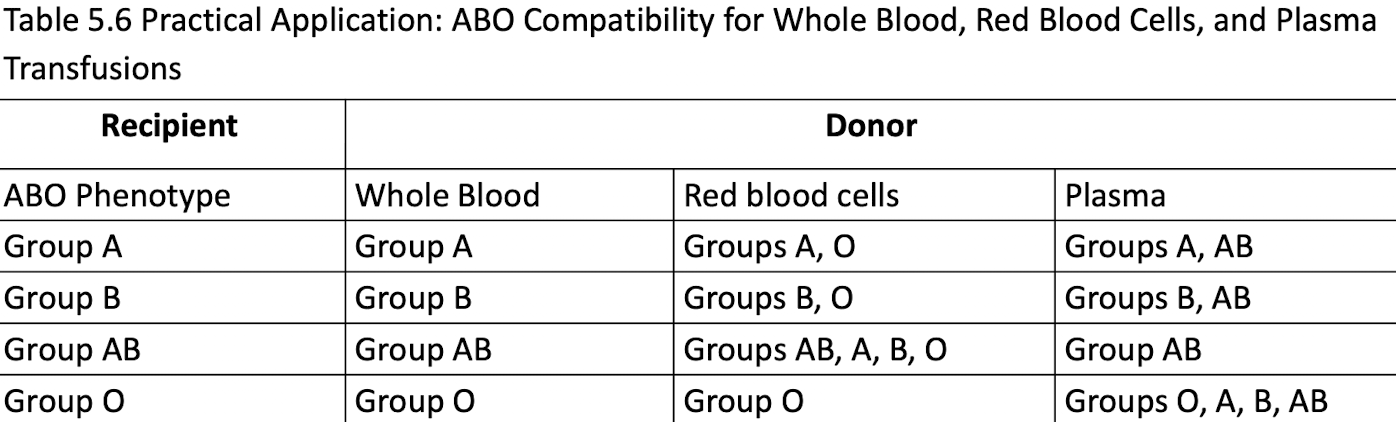
Transfusion Selection: RBC vs Plasma
RBC:
Group O: universal donor
Group AB: universal recipient
Plasma:
Group AB: universal donor
Group O: universal recipient
RBC transfusion
ABO-identical unit is preferred, followed by ABO-compatible unit for RBC transfusions
Incompatible RBCs can cause an acute
hemolytic transfusion reaction
ABO-identical unit is required in whole blood transfusions
Plasma transfusion
ABO-identical unit is preferred or compatible (reverse of RBC transfusions)
Donor unit antibodies must be compatible w/ recipient’s RBCs
ABO Compatibility
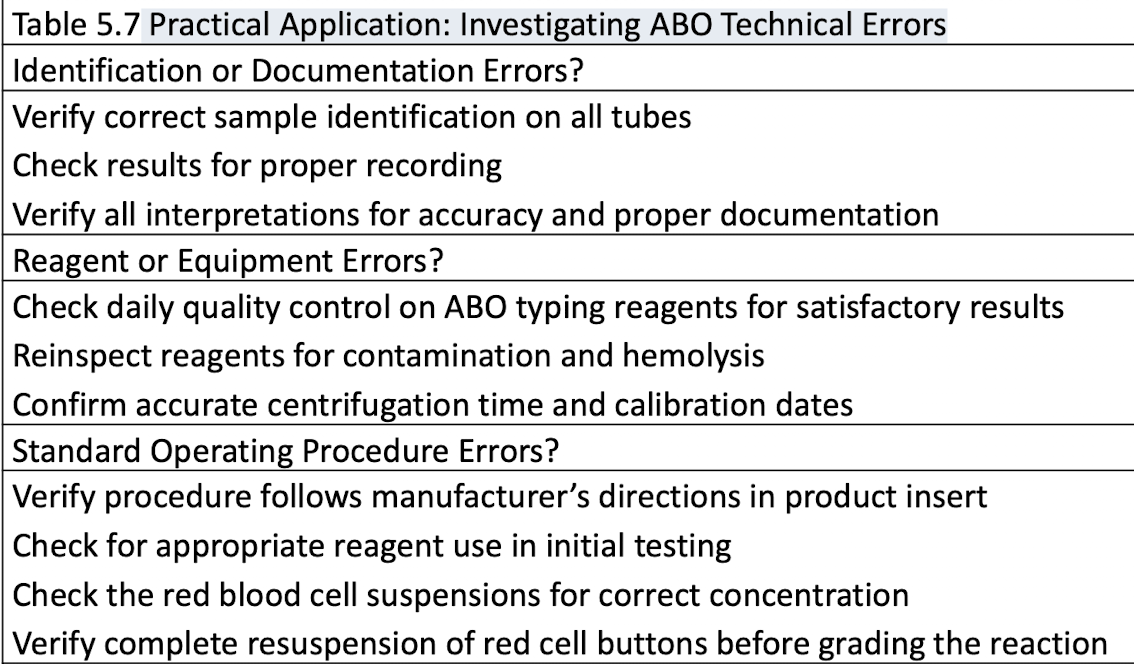
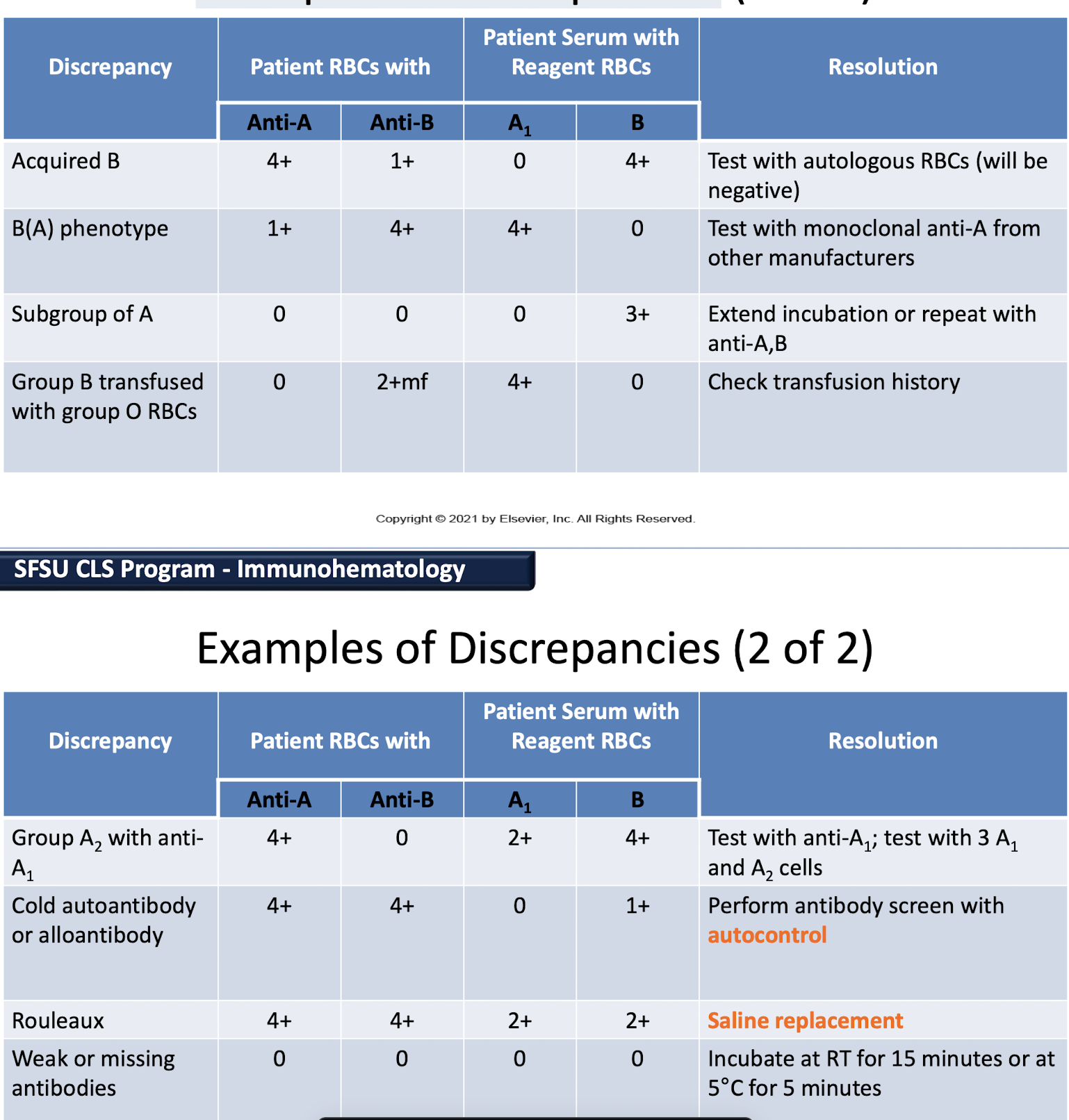
ABO Discrepancies
occur when the forward grouping does not agree with the reverse grouping
A discrepancy may be present if:
Agglutination is weaker than expected
Expected reactions are missing
Extra reactions are noted
Practical Application: Investigating ABO Technical Errors
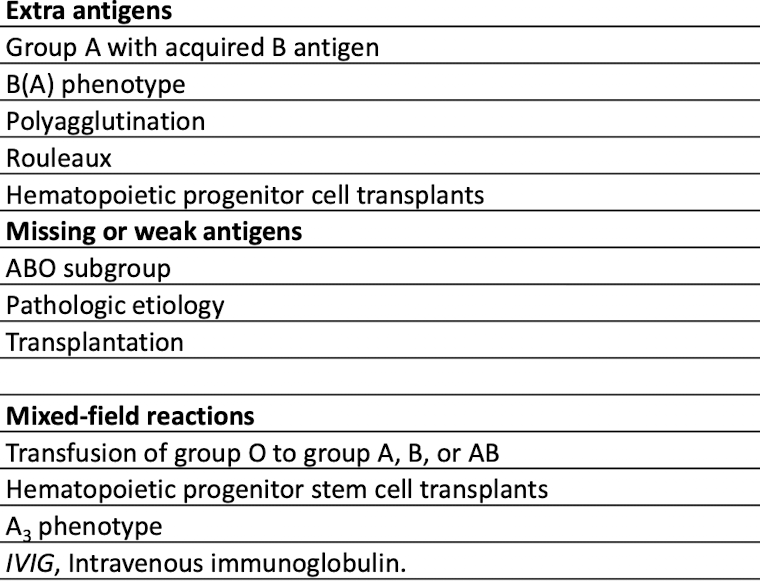
Sample-Related Discrepancies: Red Cell Testing Problems
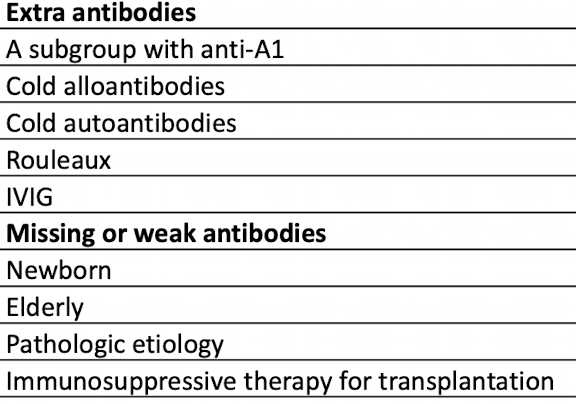
Sample-Related Discrepancies: Serum/Plasma Testing Problems
Extra Antigens
Group A with acquired B
Deacytlating Enzyme
B(A) phenotype:
similar to acquired B (pt is group B)
Polyagglutination
Hidden Ags
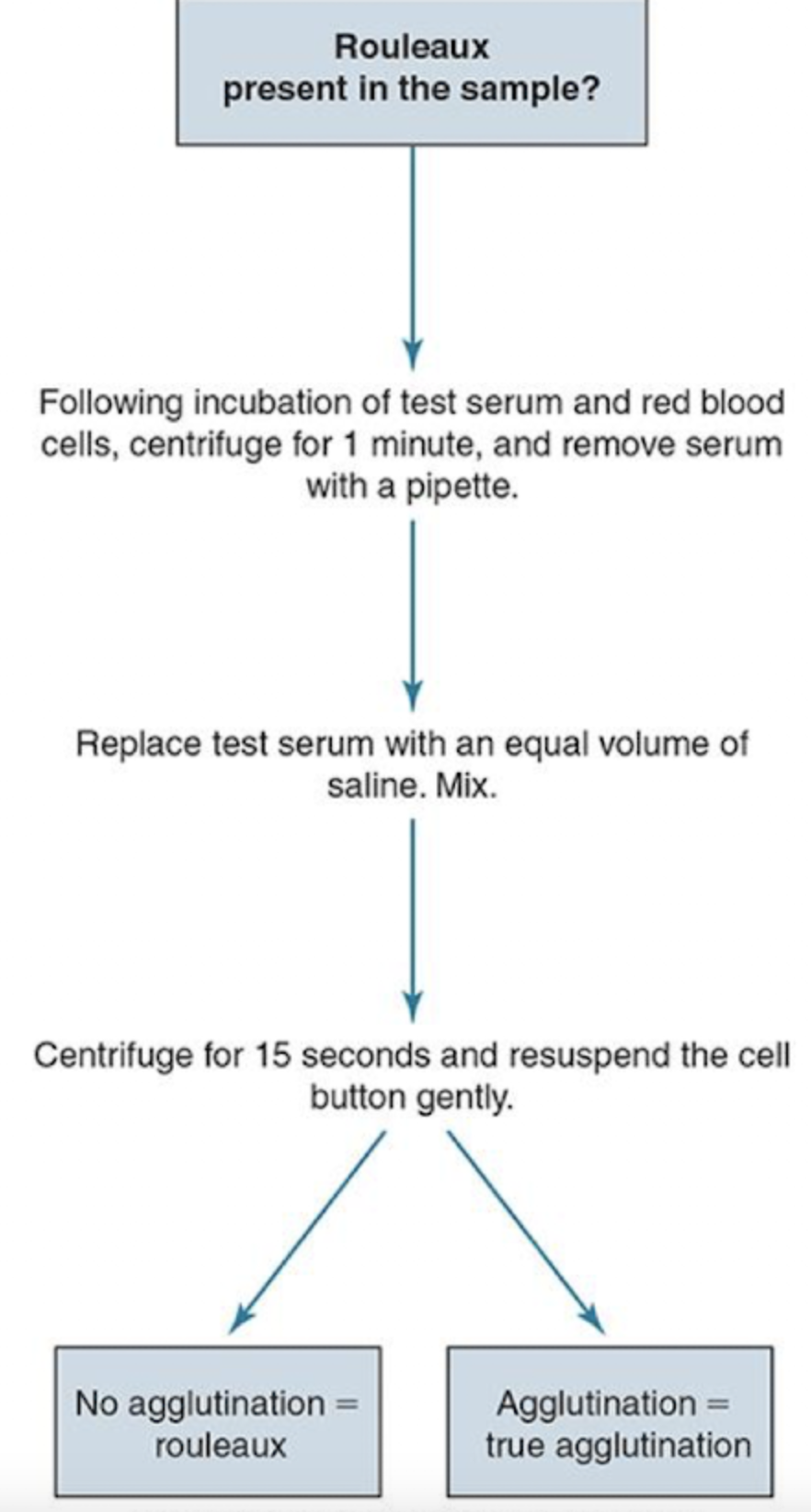
Non-specific aggregation causes
rouleaux and Wharton’s jelly
Group A with acquired B and B(A) phenotype: Extra Antigens
group A immunodominant sugar is altered by a bacterial deacetylating enzyme
Resembles group B and cross-reacts with anti-B
B(A) phenotype: group B patient
Polyagglutination and Nonspecific aggregation cause: Extra Antigens
Polyagglutination: A hidden antigen on the RBCs is exposed and reacts with most human sera
Nonspecific aggregation causes
Rouleaux: abnormal amounts of serum protein
Wharton’s jelly: gelatinous tissue contaminant in cord blood
Missing or Weak Antigens
ABO subgroups: weak/no reactivity with anti-A/anti-B reagents.
Leukemia/Hodgkin’s disease: weakened A and B antigen expression.
Resolution: Check patient history, repeat with anti-A,B to enhance subgroup
Mixed-Field Reactions Causes
contain both agglutinated and unagglutinated cells and is caused by
Two distinct cell populations (group O RBCs transfused to a group A, B, or AB individual)
Bone marrow transplant
Stem cell transplant
A3 phenotype
– Tn-polyagglutinable RBC
Extra Antibodies Causes
occur as extra agglutination reactions in the reverse testing because
Anti-A1
Cold alloantibodies
Abs specific for autologous Ags that react at room temp. or below
Cold autoantibodies
Abs specific for human RBC Ags that react at room temp. or below
Rouleaux: false-positive agglutination
Resolving Rouleaux
When are Missing or Weak Antibodies shown?
Show weak or negative agglutination in the reverse phase of testing
rxn may be explained by investigating the patient history, age, diagnosis, and immunoglobulin levels
Newborns and elderly people have reduced Abs
Pathologic states that lower immunoglobulin levels
Examples of Discrepancies
Bombay Phenotype
RBCs lack the H antigen (hh).
Classified as group O (no H, A, or B antigens present).
Serum contains anti-H, anti-A, and anti-B.
Transfusion:
Only autologous units or rare donor files can be used
Group O RBCs cannot be given because the H antigen present
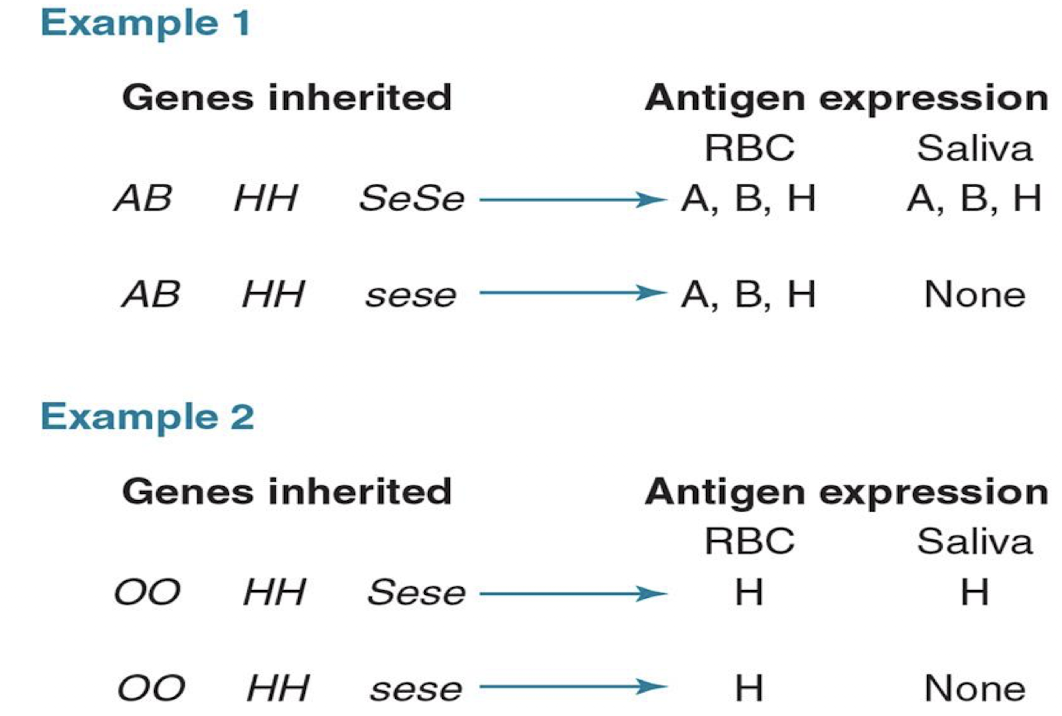
Secretor Status
Two allele genes at this locus: Se and se
Se is responsible for H substance in body secretions (e.g., saliva)
H is converted to A or B by glycosyltransferases
80% of the population are secretors
SeSe (homozygous)
Sese (heterozygous)
20% are nonsecretors (sese)
Secretor Status