NUR 305 Neurological Disorders II
1/114
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
115 Terms
Increased Intracranial Pressure (Intracranial Hypertension)
Increased intracranial pressure due to increased volume in the cranial.
Inc vol in cranium → Inc ICP
When blood escapes vasculature, inflammatory response occurs, causing leaky vessels that cause swelling/edema.
Brain occupies 80% of the skull
CSF and blood vol. make up other 20%.
Monro-Kelli Hypothesis
Volume increase in brain is compensated for by shifts in CSF & blood volume.
CSF and blood gets shifted out, blood vessels constrict.
Monro-Kellie Hypothesis
Increase in volume of one component must be compensated by a decrease in volume of another.
Difference between Adult and Child Skull
Adult Skull
Rigid, does not expand.
Child Skull
Softer.
The fontanelles close by age 3 years usually (skull can expand somewhat)
Causes of Increased Intracranial Pressure
Cerebral Edema
Inflammation
Traumatic Brain Injury
Brain Tumors
Hydrocephalus
Intracranial & Intracerebral Hemorrhage
Cerebral Edema (Causes of Increased Intracranial Pressure)
3 types — Vasogenic, Cytotoxic, Interstitial
Inflammation (Causes of Increased Intracranial Pressure)
Blood vessels become permeable, “leaky”, leading to edema.
Contusions may cause damage/necrosis.
Traumatic Brain Injury (Causes of Increased Intracranial Pressure)
Can lead to inflammation or bleeding (cerebral hemorrhage).
Blunt or penetrating injury.
Brain Tumors (Causes of Increased Intracranial Pressure)
Excess tumor tissue changes the equilibrium of the ICP’s components.
Occupies space.
Compresses vessels → diminishes blood flow → venous congestion & increased hydrostatic pressure → edema.
Walls of veins are weaker than arteries.
Can be caused by benign or malignant tumors.
Hydrocephalus (Causes of Increased Intracranial Pressure)
Occupies space.
Accumulation of excess CSF — forms blockages/slowing of drainage of CSF — Usually in the 3rd ventricle.
CSF fluid overload is specific to Hydrocephalus.
Intracranial/Intracerebral Hemorrhage (Causes of Increased Intracranial Pressure)
Blood that forms a space-occupying lesion within the closed cranium.
Blood is toxic to brain cells and places pressure on brain tissue, which rapidly increases ICP.
Toxicity causes inflammatory response.
Vasogenic Cerebral Edema
Caused by trauma and shearing stress.
Occurs due to changes in the volume of brain tissue.
Cerebral vessel walls have abnormal permeability which allows protein-rich plasma to leak into the extracellular space of the brain.
Cytotoxic Cerebral Edema
Result of a hypoxic injury.
Caused by cardiac arrest, unrelieved respiratory distress and failure, shock.
Brain is depleted of oxygen.
Begins using anaerobic metabolism.
Sodium pump fails.
Sodium enters the cell and pulls water with it.
Results in an abnormal accumulation of fluid in the brain cells.
Interstitial Cerebral Edema
Occurs with acute brain swelling.
Severe hypertension.
Leads to hypertensive stroke.
Associated with elevated blood pressure or increased CSF pressure.
Must lower BP, decrease CSF pressure, or increase the CPP >70 mmHg.
Diagnosing Intracranial Hypertension (Intracranial Pressure)
History & Physical Exam
Neuro issues, congenital vs. acquired.
Glasgow Coma Scale
V/S, Pupillary response
Head CT
MRI
Better to inspect smaller bleeds.
Treatment for Intracranial Hypertension (Intracranial Pressure)
Depends on the cause (bleed, tumor, hydrocephalus, meningitis).
General Treatment
Rest the brain
Any noxious stimulus can exacerbate ICP.
Prevent increases in ICP
Limit coughing.
Prevent complications
Prevent bed sores.
Keep HOB at 30-45 degree angle (keeps ICP stable)
Keep neck neutral (prevents blood flow from getting blocked).
Manifestations of Intracranial Hypertension (Intracranial Pressure)
Decreasing level of consciousness.
Vomiting (often projectile).
Rising blood pressure (compensation).
Makes sure there is adequate perfusion to the brain.
Increasing pulse pressure.
SBP-DBP = Pulse Pressure
Bradycardia.
Papilledema.
Look at optic disc → Diffuse look is inflammation = Inc ICP
Swelling around the optic nerve.
Fixed and dilated pupils.
Posturing.
Decorticate (to the core). Brings limbs inwards toward body.
Decerebrate is worse. Bends limbs outwards away from body.
Cushing's Triad (Increased ICP)
A late sign of intracranial hypertension, indicates impending herniation.
Increased blood pressure.
Bradycardia
Cheyne-Stokes respiratory pattern.
What are the compensatory mechanisms to Cushing’s Triad?
Autoregulation
Cushing’s Reflex
Autoregulation (Compensatory → Cushing’s Triad)
Involves the aortic arch and baroreceptors.
The blood vessels either:
Dilate to increase blood flow
Constrict if ICP increases.
This only acts up to a certain point.
Cushing's Reflex (Compensatory → Cushing’s Triad)
The hypothalamus increases sympathetic stimulation when the mean arterial pressure drops below the ICP.
MAP < ICP
Causes:
Vasoconstriction in the periphery.
Increased cardiac contractility.
Increased cardiac output.
These mechanisms increase perfusion to the brain.
Herniation
Feared complication of increased ICP.
Refers to displacement of brain tissue.
Can be fatal quickly.
In Transtentorial (Central) Herniation
Leads to Impairment In:
Cerebral blood flow
CSF
Reticular Activation System
Respirations
Uncal Herniation
Puts Pressure On:
Cranial Nerve III
Posterior Cerebral Artery
Reticular Activation System
Cerebellar or Tonsillar (Intrafratentorial) Herniation
Compresses the brain stem and vital centers, causing death.
Hydrocephalus
Excess CSF accumulation within the skull.
Causes pressure on cerebral blood vessels and brain tissues.
Usually occurs in the narrow 3rd ventricle.
CSF flow becomes blocked or poorly reabsorbed.
Often fatal if left untreated.
Risk Factors of Hydrocephalus
Pregnancy-related problems
CNS abnormalities
Illness
Tumors
Especially in adults
In brain or spinal cord
Manifestations of Hydrocephalus in Infants
Increase in head size
Bulging fontanel
Vomiting(often projectile)
Lethargy, irritability, high-pitched cry (pain!)
Feeding difficulties
Seizures
Eyes that gaze downward
Development delays if untreated
Manifestations of Hydrocephalus in Older Children and Adults
Signs & symptoms same as those for increased ICP
These changes can progress to urinary incontinence and self-care deficits.
Diagnosing Hydrocephalus
History
What happened during the pregnancy?
Physical examination
Skull X-rays
CT
MRI
Prenatal Ultrasound
Treatment of Hydrocephalus
Surgery to repair the blockage.
Ventriculoperitoneal (VP Shunt) Placement.
Surgical procedure that diverts excess cerebrospinal fluid (CSF) from the brain's ventricles into the abdominal cavity.
T/F: Hypertonic Solutions are effective for treating hydrocephalus.
False; Hypertonic solutions are not effective for treating hydrocephalus.
Why are hypertonic solutions not effective for treating hydrocephalus?
CSF flows AROUND the brain and spinal cord.
Hypertonic solutions work by drawing fluid through osmotic action across the blood-brain barrier into the intravascular space (ie. Bloodstream).
CSF does not flow through each neuron, but instead serves as a cushion for the brain and spinal cord.
Nutrients move from CSF into cells but CSF DOES NOT FLOW THROUGH THE BRAIN TISSUE ITSELF.
Traumatic Brain Injury (TBI)
A traumatic insult to the brain possibly producing physical, intellectual, emotional, social, and vocational changes.
Causes
50% are motor vehicle accidents.
21% are falls.
Others: Violence and Sports
What are the types of TBIs?
General
Blunt
Concussion
Open Trauma
Focal
Coup (Whiplash effect)
Contrecoup (Whiplash effect)
Fractures
Linear Skull Fractures
Comminuted Skull Fractures
Depressed Skull Fractures
Compound Fractures
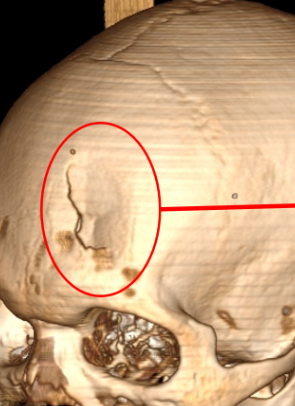
Basilar Skull Fractures
Blunt (Closed) Trauma (TBI)
The dura remains intact.
Brain tissues not exposed.
Include:
Focal (local) brain injuries.
Diffuse (general) brain injuries.
Open (Penetrating) Trauma (TBI)
Injury breaks the dura.
Exposes the cranial contents.
Risk of infection is high.
Ex) Gunshot wounds.
Concussion (TBI)
Momentary interruption of brain function.
Signs/Symptoms (Depends on Severity)
Amnesia
Confusion
Sleep disturbances
Headaches that may occur for weeks or months.
Focal Injuries (TBI)
Localized to the site of impact.
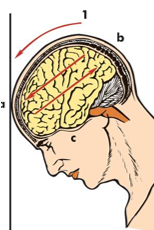
Coup Injury (TBI)
Injury directly below the point of impact.
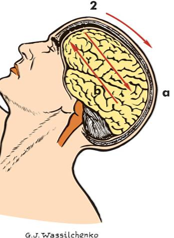
Contrecoup Injury (TBI)
Injury on the pole opposite the site of impact.
Compound Fractures (TBI)
Open fracture, going through the skin.
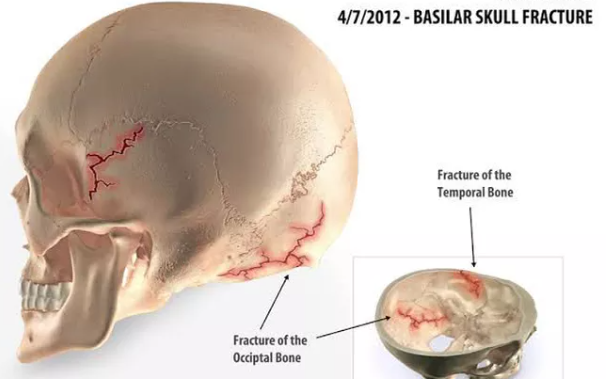
Basilar Skull Fracture (TBI)
Fracture at the base of the skull.
Extending into the anterior, middle, or posterior fossa.
Results in CSF leakage from nose or ears.
Check if glucose is present in drainage from nose/ears → If glucose present = CSF
Battle’s Sign
Mastoid area bruising indicates basilar skull fracture.
Linear Skull Fracture (TBI)
Simple clean break in skull.
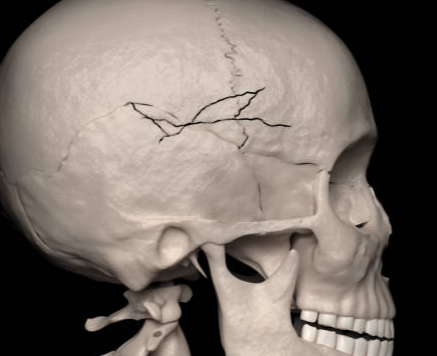
Comminuted Skull Fracture (TBI)
Fragmentation of bone in skull.
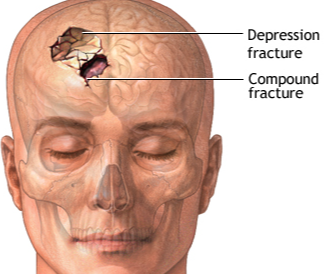
Depressed Skull Fracture (TBI)
Bone is pressed inward into the brain tissue.
Complications of Skull Fractures
Infections and Disability
Manifestations of TBI (Physical)
Fracture of skull/face
Scalp wound
Swelling of injury site
Facial bruising
Rhinorrhea
Clear nasal drainage.
Otorrhea
Clear drainage from the ears.
Pupil changes
Unequal pupil size (Rising ICP)
Manifestations of TBI (Neurological)
Seizures
Inability to recall event details
Irritability
Personality changes
Unusual behavior
Restlessness
Loss of consciousness
Poor coordination
Loss of movement
Lethargy
Stiff neck
Positive Brudzinski’s sign
Meningeal irritation
Slow respirations (bradypnea)
Look out for Cushing’s Triad
Hypotension
Vomiting
Impaired hearing, smell, taste, speech, or vision
When examining for Neurological TBI Manifestations, what should the nurse consider?
Meningeal irritation and increased ICP.
Slow respirations and hypotension may indicate Cushing’s Triad.
Diagnosing TBIs
History & Physical Exam
What happened?
Neuro Exam
Glasgow Coma Scale
Head CT or MRI
MRI allows for more detail to be seen (like small bleeds) that cannot be captured by CT.
ICP Monitoring
Placed surgically to monitor ICP
Goal range (5-15mmhg)
Treatment for TBIs
Rest the Brain!
Decrease stimuli
Reduce Cerebral Edema
Osmotic diuretics
Ex) Hypertonic 3% NaCl, Albumin, Mannitol
Pulls fluid from brain into vasculature
Decrease Energy Expenditure
Sedatives
Control Fever
If uncontrolled, can lead to brain damage
Prevent Seizures
Can lead to brain damage.
Acute TBI Management
ABCs (airway, breathing, circulation)
Assessment of vital signs to detect increased ICP
Prevent Cushing's triad!
Reduce/Prevent Increased ICP
How can the nurse help Reduce/Prevent Increased ICP during Acute TBI Management?
Positioning
Avoid Trendelenburg position → Causes Inc ICP
Avoid bearing down → Causes Inc ICP
Keep neck in neutral position
Avoid lateral twisting/turning head to the side.
May block blood flow to brain.
Prevent buildup of secretions in the lungs.
Encourage pt. to cough.
Maintain homeostasis
Ensure optimal body functions, vital signs, arterial blood gases, etc…
Prevent Complications
Pneumonia
Infections
Decubitus ulcers
TBI Complications
Changes in thinking, sensation, language, or emotions
Long-term
Seizures
Memory decline
Depression
Concussions
Alzheimer’s disease
Parkinson’s disease
What are the 4 arteries that perfuse the brain?
2 Posterior Vertebral Arteries
2 Anterior Carotid Arteries
TBI Prevention
Seat belt use
Appropriate child safety seats
Helmets (sports, biking, skating)
Home safety (prevent falls, injuries)
Elderly population.
Furniture, rugs, safety bars in bathroom.
Storing firearms in locked cabinets
Never driving impaired/distracted
Phone or drugs.
Child supervision
Cerebral Hematomas/Bleeds
A collection of blood or a clot in an area inside or near the brain.
Left untreated may lead to inflammation and increased intracranial pressure.
Can lead to severe neurological injury or death.
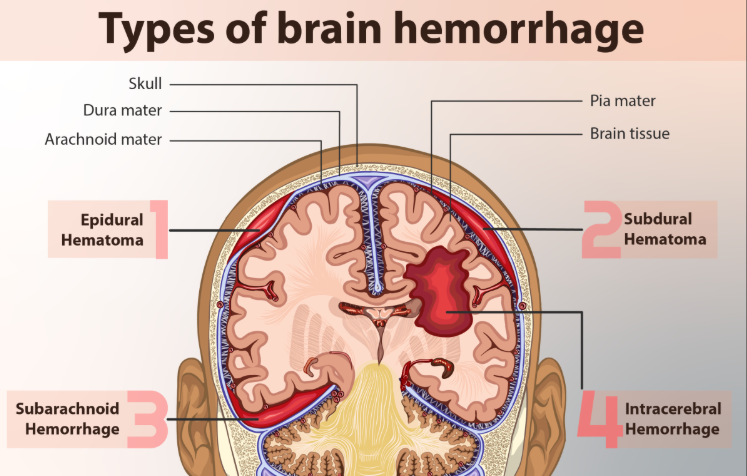
What are the 4 types of Cerebral Hematomas/Bleeds?
Epidural
Subdural
Intracerebral
Subarachnoid
What are the differences between the 4 types of Cerebral Hematomas/Bleeds?
Epidural
Arterial bleeding into space between dura and inner table of skull.
Subdural
Bleeding between the dura and arachnoid space.
Subarachnoid
Bleeding between the arachnoid space and pia.
Intracerebral
Bleeding in the brain tissue itself.
What methods can the nurse use to control Cerebral Hematomas/Bleeds?
Respiratory Support
Semi-Fowler's positioning
Decreases edema, swelling.
Prevent Seizures.
Reduce brain metabolism.
Limit activities that increase ICP.
Control glucose level.
Stress ulcer prevention.
Diagnosing Cerebral Hematomas
History and Physical Exam
Glasgow Coma Scale
Head CT, MRI
Cerebral Angiogram
Tracking vasculature of blood vessels in the brain w/ IV dye.
ICP monitoring
Treatment for Cerebral Hematomas
Surgical removal of the blood through a burr hole or a craniotomy.
Burr Hole = Drill hole in head to relieve pressure/drain blood.
Craniotomy = Take a piece of skull plate out.
Physical, speech, and occupational therapy.
Damage and ischemia may impair these functions.
Once O2 comes back, these functions may return.
Plasticity
Same treatment as for increased intracranial pressure.
Epidural Hematoma
Neurologic emergency with potentially catastrophic ICP elevation.
Caused By
Arterial bleeding into space between the dura and inner table of skull.
Most common cause.
Temporal bone fractures.
Tearing of the middle meningeal artery.
Common cause
What is an Important Sign of an Epidural Hematoma?
Momentary unconsciousness follows lucid interval within minutes of injury.
Subdural Hematoma
Bleeding develops between the dura and arachnoid space.
Frequently caused by a small venous tear.
Bleeds slower than an arterial tear b/c venous system is a lower pressure system.
Acute and Chronic types.
ICP increases over a period of about a week after the injury.
Acute Subdural Hematoma
Develops within 24 hours of injury.
Progresses rapidly.
Has a high mortality rate.
Chronic Subdural Hematoma
Develops several weeks after the injury due to slow leak.
More common in elderly adults because of brain atrophy.
Subarachnoid Hemorrhage
Bleeding in the space between the arachnoid and pia.
Causes
Most are from arterial bleeding.
80% are from ruptured cerebral aneurysms
20% are trauma induced.
Risk Factors for Subarachnoid Hemorrhage
Hypertension
Cigarette smoking
Family history
Alcohol abuse
Sympathomimetic drugs
Estrogen deficiency
Older age (>60 years)
Posterior circulation location
Atherosclerosis
Large Intra-arterial aneurysm (IA) size (>5 mm)
Autosomal dominant polycystic kidney disease
Symptoms of Subarachnoid Hemorrhage
Classic
Sudden, severe headache, worse in the back of the head (occiput).
* “Worse headache of my life!” *
Other
N/V
Dizziness
Orbital (eye socket) pain
Diplopia
Visual loss (occiput)
Meningeal
Positive Brudzinski’s
Specific to meningeal irritation.
Possibly Kernig’s due to spread of blood down the 4th ventricle.
Blood gets into CSF
Indicates disc disease.
Management of Subarachnoid Hemorrhage
Control blood pressure
Administer anti-hypertensive medications to keep MAP <130mmHg.
Osmotic Diuretics and/or Hypertonic Solutions
These medicines reduce cerebral edema.
Treatment for Subarachnoid Hematoma
Surgical treatment to prevent rebleeding.
Clipping
Coiling
The choice between coiling and clipping usually depends on:
The location of the lesion.
The neck of the aneurysm.
The availability and experience of hospital staff.
Complications of Subarachnoid Hematoma
Hydrocephalus
Brain Herniation
Vasospasm
Receptors are off
Repeated Vasodilation/Vasoconstriction
Seizures
Hyponatremia
Loss of Na+ through urine.
Exacerbates cerebral edema.
Pulmonary & Cardiac
Issues of control w/ brain and heart.
MAP Calculation
MAP = [(2 x diastolic)+systolic] / 3.
Intracerebral Hematomas
Bleeding in the brain tissue itself.
Causes
Contusion or shearing injuries.
Hypertension
Hypertensive Crises
Cerebral/Vascular Accidents (CVAs)
Strokes
Aneurysms
Often congenital
Arterio-venous malformations (AVMs)
An abnormal/malformed connection between arteries and veins.
Causes weakness in connection, can burst.
Management of Intracerebral Hematomas
Depends on the cause and the severity.
Prevent/Reduce cerebral edema.
Control blood pressure.
Surgical for space occupying bleeds.
Conservative treatment for small bleeds.
Complications of Intracerebral Hematomas
Hydrocephalus
Seizures
Rebleeding
Vasospasm
Brain herniation
Transient Ischemic Attack (TIA)
Warning signs of stroke.
Transient and focal (localized) neurologic dysfunction.
Most commonly occurs in the face.
Causes
Brief interruption in cerebral blood flow
Resulting from cerebral vasospasm or systemic arterial hypertension.
T/F: A patient with reversible ischemic neurologic deficit has signs and symptoms that look just like a stroke (paralysis, weakness, numbness, loss of speech) except that these symptoms will go away within a week.
False; These symptoms go away within 24 hours.
Stroke (Cerebrovascular Accident (CVA))
A change in the normal blood supply to the brain.
Two Types
Ischemic
Hemorrhagic
Treatment of CVA depends on which type it is.
Why is a CVA (Stroke) life-threatening?
The brain is unable to store oxygen or glucose and must receive a constant flow of blood to function.
Strokes restrict adequate blood flow throughout the brain through blockage of blood flow or intense cerebral bleeding.
Ischemic Stroke
Stroke caused by a blockage:
Thrombotic = Stationary blood clot.
Embolic = Blood clot that travels.
Both types of blockages block blood flow to an area of the brain.
Hemorrhagic Stroke
A CVA that occurs due to immense bleeding.
Causes
Ruptured cerebral aneurysm.
Arteriovenous malformation (AVM) bleeding
When a clot is “thrombotic,” what does this mean?
The clot is stationary.
When a clot is “embolic,” what does this mean?
The clot is traveling throughout the body.
Risk Factors for CVAs
Populations
African Americans
Those living in the Southeast.
Lifestyle
Hypertension
Smoking
Inactivity
Obesity
High Cholesterol
Diabetes
Atherosclerosis
Oral Contraceptive use
Increases risk of blood clots.
Alcohol abuse
Illicit drug use
Arterial Fibrillation
Irregular and very rapid heart rhythm.
Can lead to blood clot formation → become emboli → cause embolic CVA.
Symptoms of an Aneurysm Rupture
A sudden severe headache
Increased ICP
FAST Stroke (Signs and Symptoms of a Stroke)
Face
Ask pt. to smile.
Facial drooping on one side = pos. finding for CVA
Arms
Ask pt. to raise both arms.
Weakness or paralysis in one arm = pos. finding for CVA
Speech
Ask the pt. to repeat a simple phrase.
Difficulty speaking = pos. finding for CVA
Time
Call 911
Clock starts ticking from the FIRST clinical manifestation.
Only 3 hours available to receive treatment to reverse neurological deficits.
After 3 hrs, permanent damage occurs.
Complications Immediately After the Stroke
Cerebral edema
Increased intracranial pressure
Dysphagia
Seizures
Stroke Complications Related to Immobility
Hydrocephalus
Vasospasms
Rebleeding or rupture
Bed sores
Meningitis
Inflammation of the meninges (usually infectious).
What causes Meningitis?
The following causes trigger the inflammatory process, leading to swelling of the meninges and increased ICP.
Bacteria (Can be Quickly Fatal)
Neisseria meningitidis
Streptococcus pneumoniae
Haemophilus influenza
Viruses
Enterovirus
Measles
Influenza
Herpes
Other (Rare)
Tumors
Allergens
Meningitis Risk Factors
Age
<25 y.o (frequent community settings)
Infants (immature immune system)
Community Settings
Schools
Institutions
Certain Medical Conditions
Immunosuppressed individuals.
Travel to Endemic Regions
Sub-Saharan Africa
Meningitis Signs and Symptoms
S/S
May present with sudden onset of fever, headache, and stiff neck.
Stiff neck = Positive Brudzinki
Nausea
Vomiting
Photophobia
Altered mental status-confusion
Development of S/S
Typically develops 3-7 days after exposure
Can appear suddenly or over several days.
Diagnosing Meningitis
History
Physical examination
Test Brudzinski’s
Throat cultures
Strep
Lumbar puncture with CSF analysis
If CSF cloudy = high WBC count = definitive for infection
PCR test
Polymerase chain reaction test
Tests DNA of infecting agent
Head CT
Treating Meningitis
Treatment
Antibiotics (if bacterial)*
Antiviral (if viral)*
Hydration
Fever management
Prevention
Vaccination (MCV4 series)
Meningococcal Conjugate Vaccine
Consists of 4 injections spread out through childhood and adolescence.
*Medications must be able to cross the blood-brain barrier.
Encephalitis
Inflammation of the brain and spinal cord.
Usually results from an infection.
What are the causes of Encephalitis?
Viral
Arthropod-borne viruses
Most common
Ex) Eastern Equine Encephalitis, West Nile Virus
Herpes simplex
Bacterial
Lyme disease
TB
Syphilis
Pathology of Encephalitis
Infection triggers inflammatory response.
Vasodilatation
Increased capillary permeability (“leaky”)
Leukocyte infiltration.
The inflammatory process can cause nerve cell degeneration and diffuse brain destruction
Cerebral edema possible from inflammation.
Nerve cell degeneration → Liquid necrosis