Upper GI Pathologies
1/31
Earn XP
Description and Tags
Esophagus, stomach, neoplasia
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
32 Terms
where is the esophagus in relation to the trachea
posterior
what is Esophageal Atresia with Tracheoesophageal Fistula?
a condition where the fetus’ wall between the trachea and esophagus is incorrectly developed leading to…
a) a blind pouch —> esophageal atresia
b) remain somewhat attached to the trachea forming a tracheoesophageal fistula (TEF).
what is the classification and etiology for Esophageal Atresia with Tracheoesophageal Fistula?
C: congenital
E: may be a link to gene malformations, usually a fistula is associated between the trachea and esophagus
what is the pathogenesis for Esophageal Atresia with Tracheoesophageal Fistula?
when the esophagus and trachea wall fail to form, the organs don’t separate, therefore a fistula occurs @T4 level
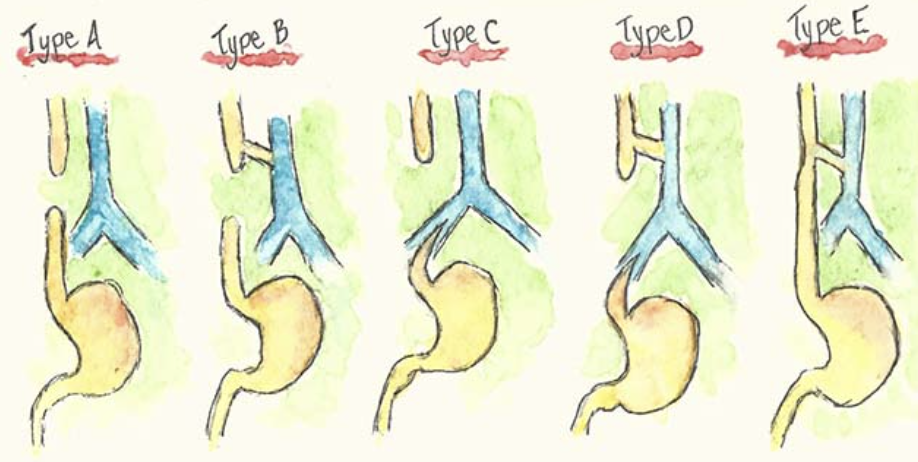
what are the five different types of atresia with and w/o TEF?
Type A: esophageal atresia only. no connection to stomach —> upper esophagus ends in a blind pouch and lower esophagus is sealed. (esophagus not connected).
Type B: upper esophagus connected to trachea, lower esophagus sealed. food and liquid will end up in the lungs
Type C: upper esophagus ends in a blind pouch, lower esophagus connected to trachea. air from trachea can go to stomach.
Type D: upper and lower esophagus connected to trachea. food and liquid will travel to lungs and bowel gas present.
Type E/H: esophagus complete but fistula is formed between esophagus and trachea so food and liquid could still enter into lungs and normal bowel gas patterns as food will enter stomach.
which types of atresia have bowel gas and which types do not have bowel gas?
No bowel gas: Type A, B
Bowel gas present: Type C, D, E/H
which type of atresia is the most common?
type C
what are the S&S of esophageal atresia w/ TEF?
cyanosis, choking, excessive salivation, dyspnea and gagging. Continual suction may be required to prevent aspiration pneumonia. There may be an inability to pass an NG tube into the stomach.
why is extra saliva a sign of esophageal atresia?
because saliva is usually swallowed and with no connection to the stomach, there is no way for the saliva to drain
what is the treatment for esophageal atresia w/ TEF?
aspiration is a major concern, surgical correction is needed. A thoracotomy is usually performed to attach the proximal to the distal esophagus.

RA of esophageal atresia w/ TEF
U/S and MRI can be used to detect this pathology in utero
water soluble contrast must be used for contrast studies
plain x-ray will show bowel gas or not
what is acquired tracheoesophageal fistula?
a TEF that occurs for causes other than congenital development abnormalities.
what is the classification and etiology of acquired TEF?
C: degenerative but also traumatic if an injury was the cause
E: result of malignancy in the mediastinum (majority of cases), trauma, infectious process
what is the pathogenesis of acquired TEF?
In terms of mediastinal malignancy, a tumor may grow large enough to encompass both the trachea and esophagus creating a tunnel between the two structures.
In terms of injury, if the injured area of the trachea or esophagus does not heal properly, it may ulcerate causing a fistula to develop between the two structures.
what are the S&S for acquired TEF?
Hemorrhaging of the fistula may occur causing blood in the sputum, aspiration pneumonia may occur as a result of food and liquid entering the lungs.

RA of acquired TEF
A plain CXR may show air within the mediastinum, if the TEF is a result of malignancy.
Fluoroscopy with water soluble contrast can be used to identify the actual fistula.
treatment of acquired TEF
surgical: treatment plans vary greatly depending on the ability to remove the mass. If so, repairs are done to the existing structures
non-surgical: a stent can be placed in the esophagus to maintain its patency and block off the fistula
what is Zenker’s Diverticulum?
A Zenker's Diverticulum is an outpouching on the posterior wall of the upper esophagus, specifically the hypopharynx, where the mucosa layer has herniated through the muscular layer
what is the classification and etiology for Zenker’s Diverticulum?
C: degenerative (usually occurs ages 40+), inflammatory if food gets lodged causing irritation
E: The mucosal layer of the esophagus herniates through the muscular layer at the bottom of the hypopharynx as a result of of the failure of the cricopharyngeal muscles to contract properly to aid in the swallowing of esophageal contents.
what is the pathogenesis for Zenker’s Diverticulum?
the cricopharyngeal muscles become weak which causes the area above these muscles (the pharyngoesophageal junction) to herniate posteriorly.
contents can get stuck and will not be able to pass through the esophagus
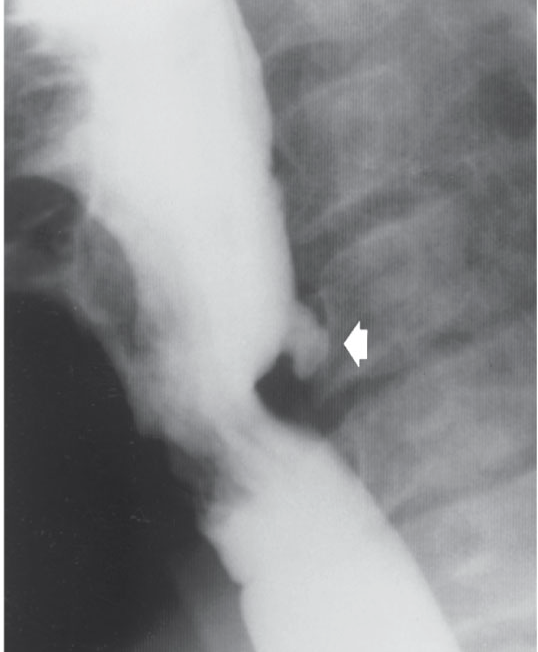
RA for Zenker’s Diverticulitis
barium swallow is the most common modality used
S&S of Zenker’s
urge to clear throat
risk of aspiration (aspiration pneumonia)
treatment for Zenker’s
no treatment unless they cause issues with swallowing
change diet to softer foods, eat slowly
excision of divericula
what is achlasia?
aka cardiospasm or megaesophagus, esophageal achalasia is a condition where the cardiac sphincter (lower end of the esophagus) fails to relax.
Classification and Etiology
C: degenerative neuromuscular
E: obstruction of the distal esophagus caused by degeneration of the nerves controlling the cardiac sphincter. This leads to incomplete relaxation of the cardiac sphincter resulting in incomplete clearing of esophageal contents into the stomach.
pathogenesis of achlasia
gradual degeneration to the nerves
reduced peristalsis in distal esophagus
distal esophagus dilates

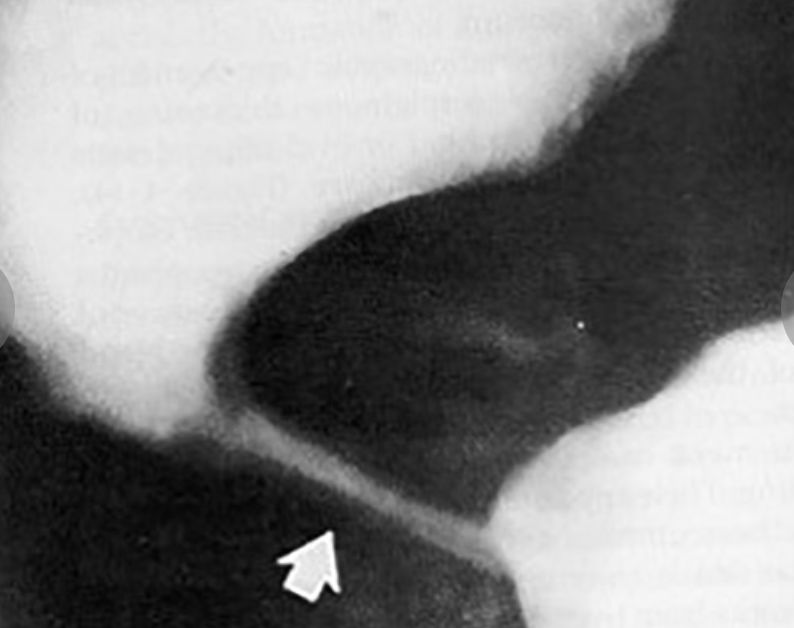
RA of achlasia
xray shows widened mediastinum with an air fluid level
radiographic signs include bird’s beak, string sign or corkscrew esophagus
bird’s beak sign of achalsia
S&S
difficulty swallowing (dysphagia)
substernal pain
regurgitation
some weight loss due to insufficient nutrients
treatment
lifestyle
botox
meds
balloon dilation
myotomy