Lecture 13: Bandaging and Techniques
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
advantages of bandaging
protects wounds
speed wound healing
disadvantages/complications with bandaging
result in limb amputation
kill your patient!
bandage injury
can happen even when bandage is placed properly!

what can happen with the owners with a bandage injury??

they may blame you!
owner education is imperative!
good things that bandages do:
provide wound cleanliness
control wound environment
reduce edema and hemorrhage
eliminate dead space
immobilize injured tissue
minimize scar tissue
make patient more comfortable
complications with bandages:
patient discomfort
patient mutilation of bandage and wound
bacterial colonization of wound
ischemic injury
damage to healing tissues
become GI foregign body obstruction
Indications for bandages:
typically used below elbow and stifle
treating injuries
bandages reduce pain, swelling, local tissue damage
protecting wounds or devices
for transport
soft padded bandage (modified robert jones)
immobilizes limb
decreases/limits soft tissue swelling
absorbs wound exudate
add splint material
premade, thermoplastics, fiberglass, aluminum rods
fracture MUST be below the elbow/stifle
the basic layers of a bandage:
1) primary (contact layer)
2) secondary (intermediate layer)
3) tertiary (outer layer)
functions of primary layer
debrides tissue
delivers medication
transfers wound exudate
forms occlusive seal
minimizes pain
prevents excessive loss of body fluids

primary layer
Functions of a secondary layer
absorbs and stores deleterious agents
retards bacterial growth
pads wound from trauma
splints wound to prevent movement
holds primary bandage layer in place
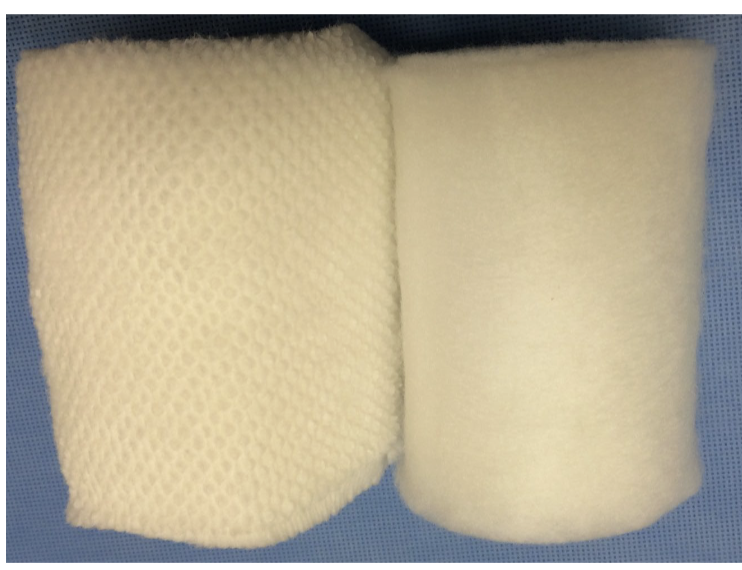
secondary layer
secondary layer
functions of tertiary layer
holds other bandage layers in place
protects against external bacterial colonization
cosmesis

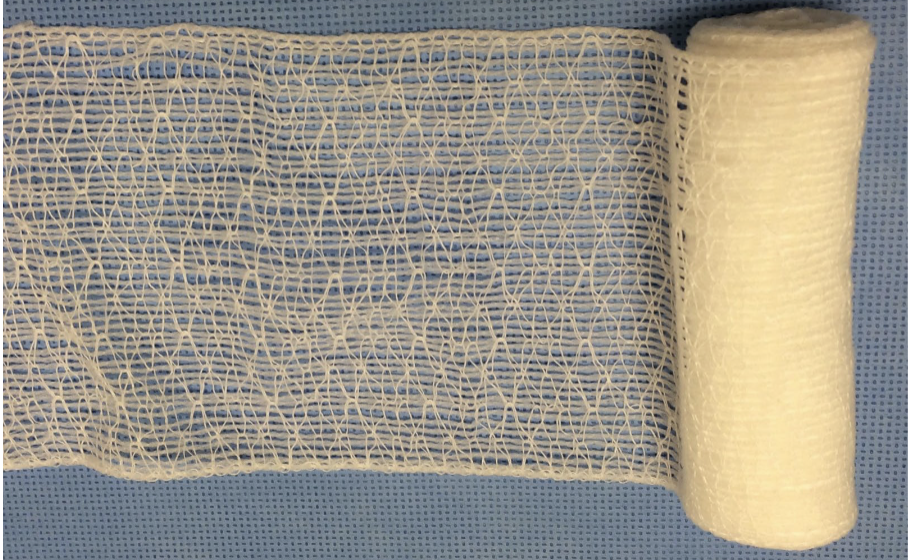
tertiary layer
types of primary layers
adherent
nonadherent
occlusive
semi-occlusive
primary/contact layer selection
based on:
phase of wound healing
amount of exudate
wound location and depth
presence of absence of eschar
amount of necrosis or infection
types of primary layers:
adherent vs. nonadherent
adherent primary layer
used when wound debridement required
may be wet or dry
nonadherent primary layer
during repair phase or if no necrotic debris
retains moisture to promote epitheliazation and prevent dehydration
drains excess fluid and prevents maceration
occlusive primary layer
impermeable to air
use on nonexudative wounds to keep moist
speeds rate and quality of healing compared to dressings allowing desiccation
use in partial thickness wounds w/o necrosis or infection
semi-occlusive primary layer
allows air to penetrate
allows exudate to escape
what is the most commonly used primary layer?
semi-occlusive!
applying soft padded bandage
1) tape stirrups
2) primary layers
3) secondary layer
4) tertiary layer
5) labeling
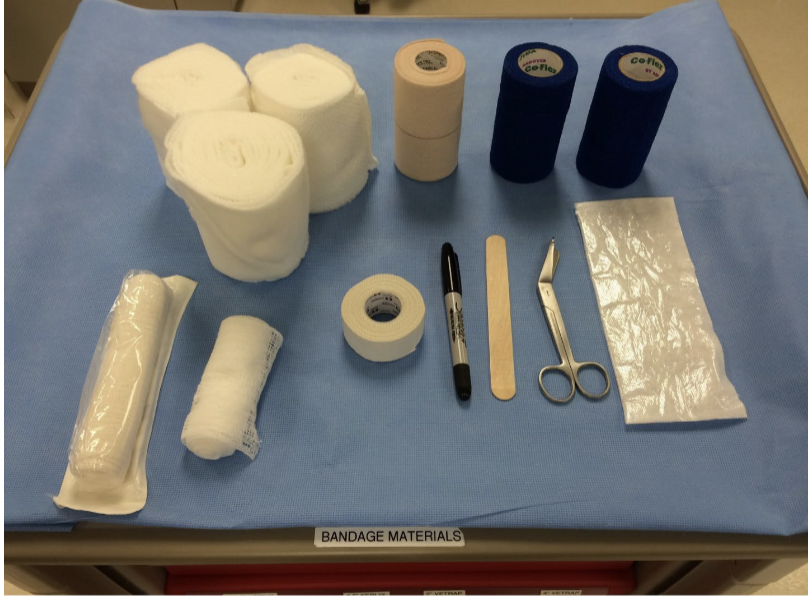
bandage material and supplies
applying tape stirrups
tape stirrups:
distal 1/3 of limb
medial and lateral or dorsal and palmar/plantar
tabbed ends or tongue depressor to help separation
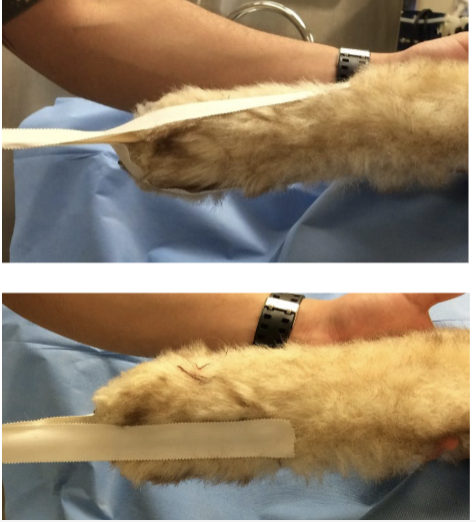
tape stirrups
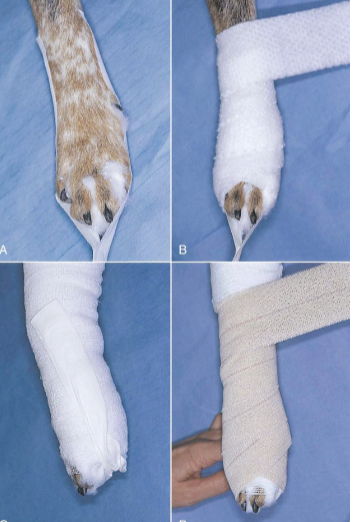
modified rovert jones/soft padded bandage
tip for modified robert jones/soft padded bandage
place cotton between toes!
decreases moisture build-up
increases patient comfort
don’t forget dewclaw
applying primary layer
contact layer
nonadherent
± medication
usaully sterile
wicking

contact layer - primary layer
applying secondary layer
intermediate layer
absorbent
supportive
± rigid support
applied
distal to proximal
overlapping
firm, even pressure

secondary layer
steps for applying secondary layer
separate tape stirrups
rotate stirrups proximally while twisting 180 degrees
secure sirrups to underlying wrap
prevents distal slipping

applying tertiary later
outer layer
applied
distal to proximal
overlapping
firm, even pressure
this is what the client sees!
tertiary layer

applying a walking pad
Elastikon or durable material
very adhesive
water resistant
applied w/o pressure
elastic properties may lead to swelling
doozies!

walking pad
applying labels to bandages
date
initials
reminders
warnings

applying labels to bandages
general types of bandages:
absorbant
adherent
wet-to-dry (most common adherent)
no longer recommended
wet-to-wet (contact layer expected to stay wet)
dry-to-dry
no longer recommended
nonadherent
now recommended for all stages of wound healing
occlusive
semi occlusive
bandages most often used in vet med
tie-over
wound in area inaccessible by standard bandaging techniques
stabilizing
post-operative or closed wound
over closed incision or drain
which two types of bandages are no longer recommended
adherent wet-to-dry
and adherent dry-to-dry
which type of bandage is most often used in vet med?
semi occlusive
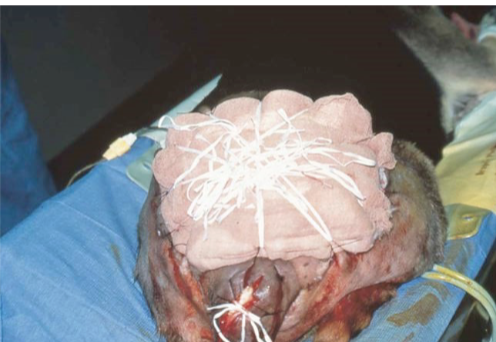
tie-over bandage
wound in area inaccessible to standard bandaging techniques (e.g. hip, shoulder, axilla, or perineum)
contact and absorbent layers held in place with tie-over bandage

tie-over bandage would be good for this wound

tie-over bandage used to manage large open wound on lateral thigh of 6 yo greyhound
how to apply tie-over bandage
apply sutures or skin staples w loose loops around edges of wound
apply primary and secondary bandage layers
hold tertiary layer in place
lacing umbilical tape or heavy suture through loose skin sutures or staples
pressure relief bandage
usually over bony prominence
to treat/prevent pressure sores
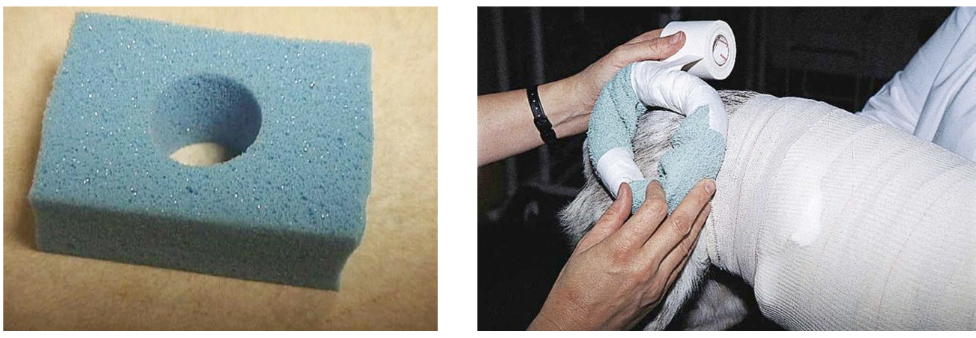
pressure relief bandage
what are pressure bandages good for?
control minor hemorrhage, edema, and excess granulation tissue
direct application of corticosteroid ointment to wound helps control excess granulation tissue
the more convex the surface, the greater pressure exerted by dressing on tissue
when to use wet adherent bandages
wound surface has necrotic tissue, foreign matter, or viscous exudate
sterile wide mesh gauze soaked in:
sterile saline solution
1:40 (0.05%) Chlorohexadine diacetate
necrotic tissue and foreign material adhere to gauze and removed with bandage
when to use dry adherent bandages
when wound surface has loose necrotic tissue and foreign material
when wound has large quantity of low-viscosity exudate that does not aggregate
robert jones is used for: (REMEMBER THIS)
temporarily immobilization of fractures
decreases/limits soft tissue swelling
absorbs wound exudate
soft padded (modified robert jones) uses
similar benefit as with robert jones
add splint material
premade, thermoplastics, fiberglass, aluminum rods
*FRACTURE MUST BE BELOW ELBOW/STIFLE
Robert Jones vs Soft Padded (Modified Robert Jones)
Robert Jones:
very large/thick bandage
uses rolled/sheet cotton
wrapped with more compression
Soft Padded (Modified Robert Jones)
similar benefits as Robert Jones
add splint material
premade, thermoplastics, fiberglass, aluminum rods
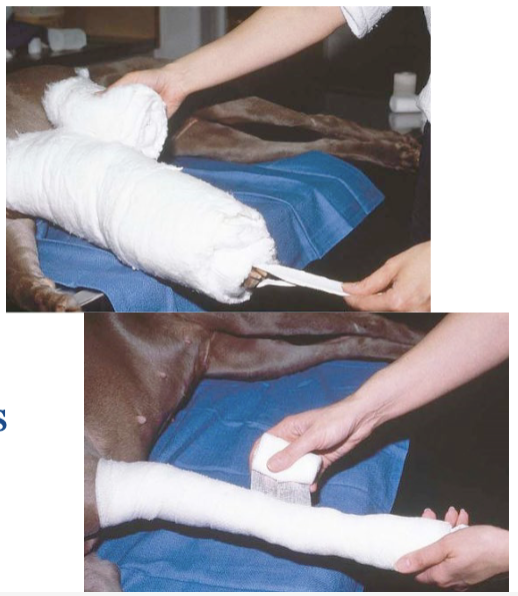
Robert Jones vs. Modified Robert Jones
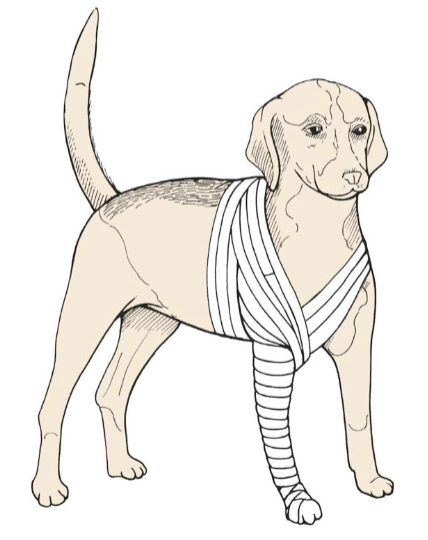
Proximal Extremity Lesions
continue bandage up leg, around chest or abdomen and between legs to create spica type bandage
Paw bandage
placed like leg bandage except digits are covered
after placing stirrups and contact layer
reflect cast padding over digits from dorsal to ventral - then ventral to dorsal
wrap padding around distal limb
conform bandage to limb with elastic gauze
secure bandage with elastic tape in similar fashion

Schroeder-Thomas Splint
traction splint
labor intensive
soft tissue complications
lacks predictability

which type of splint has “historical significance”
Schroeder-Thomas Splint
Spica splint

for immobilization of shoulder
Ehmer Sling

what is the Ehmer Sling for?
prevents pelvic limb wt-bearing
post hip reduction or acetabular fractures
“Ehmer Femur”
Velpeau Sling
prevents forelimb wt-bearing
after shoulder/forelimb procedures
“Velpeau Elbow”
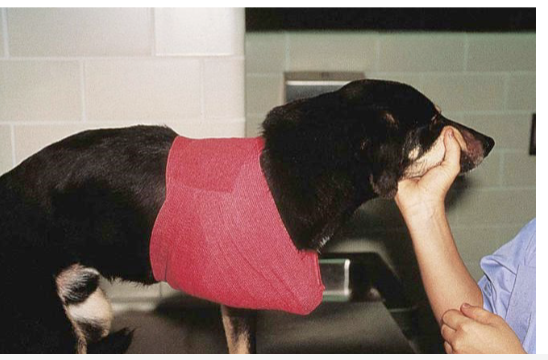
Velpeau Sling
Casts for fractures
stable minimally displaced fractures
young rapidly healing animals
unable to repair with surgical techniques
expense: discuss with owner
potential issue?
only injuries distal to elbow/stifle!!!
should you cast open fractures?
NO!!!
always radiograph after casting
must have > 50 % overlap of fracture ends
in each of 2 radiograph views
what must you ensure happens before casting?
swelling reduces
greenstick fractures may not need what?
sedation
displaced fractures require
general anesthesia
when to check casts?
at least q2 weeks (weekly initially if possible)
how to place cast
with limb in standing position
encourages use when walking
limits muscle atrophy and joint stiffness
shortens recovery period after removal
tendon repair protection
support an arthrodesis!
common complications with bandaging
slipping/loosening
water or urine-soaked
joint stiffness and muscle atrophy
pressure sores
hard materials or constricting bands
prominences
checking and changing bandages
bandages require high degree of client compliance!
discharge should include verbal, written, and visual instructions for clients
check frequently!!
check frequency for bandages:
age
activity
cleanliness
associated wounds
swelling
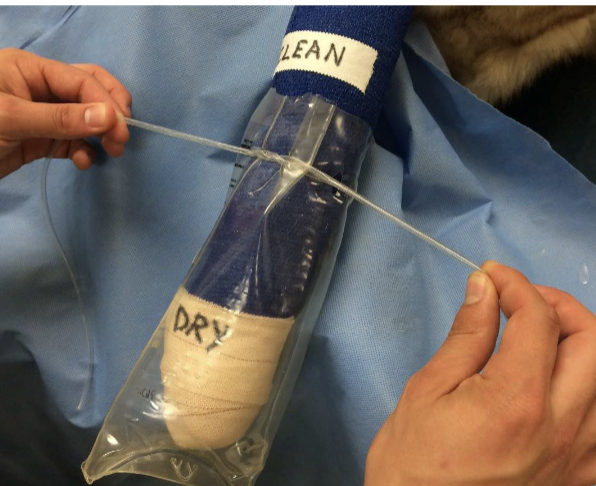
assessing bandage
clean
dry
protect during post-op recovery, hospital blue pads
plastic bag when going outsidea
assessing bandage - comfort:
chewing at bandage
lameness increase after discharge
when to remove bandage?
with these signs:
odor - swelling
toe temperature - compare to other foot!
nail bed cyanosis
if any doubt… REMOVE IT!!!

Rules to remember:
sedation or anesthesia may be required
leave middle 2 toes (claws) exposed when possible!!
bandages start at toes and go up limb to avoid swelling!

keep toes how when bandaging
in physiologic position
typocally standing
do NOT apply with limb in full extension (straight)
how much should you overlap your bandage material?
1/3 to ½ the width of your wrap
apply firm even pressure during application of bandages, tension should be proportional to:
amount of padding and size of patient
owner compliance with bandaging is the:
key to success!
no single dressing has optimum microenvironment for all wounds or all stages of what?
wound healing of single wound
when bandaging, identify underlying structures, examples:
mark the ear!
prevents iatrogenic injury