Physical Diagnosis of the Respiratory System
1/187
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
188 Terms
Symptom
Complaints as reported by the patient
Subjective
Something that comes form the patient and it is up to us to believe it or not
the amount of experience will help us determine whether patient is telling the truth or not
Sign
Findings by the medical professional
Objective
Established by using a standardized test
Ex. fever - inc temp
Tidal Volume
amount of air a person is able to inhale and exhale at rest
500 ml
Inspiratory Reserve Volume
Amount of air a person can maximally inspire at the end of a normal inspiration
1,900 mL to 3,300 mL
Expiratory Reserve Volume
Amount of air a person exhale some more maximally at the end of anormal expiration
700 mL and 1,200 mL
Vital Capacity
IRV + TV + ERV
Amount of air that can come in and could get out of a person’s lungs
3-5L
Residual Volume
Air that always stays in the lungs at the end of the expiratory reserve volume
1-1.5L
Total Lung Capacity
VC + RV
~6L
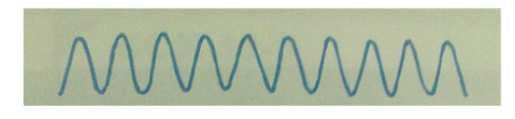
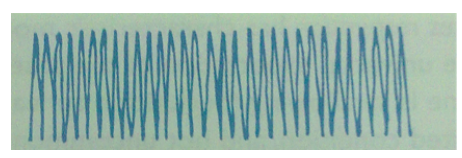
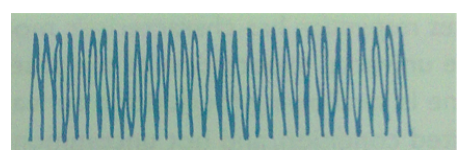
Pattern of Breathing - Eupnea
Normal, regular and comfortable at a rate of 12-20 cpm
The younger the patient is, the faster the respiratory rate they would have
Babies will be breathing faster than an adult
Older people will be breathing slower
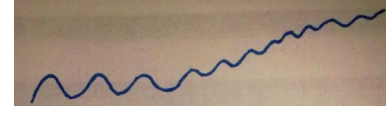
Pattern of Breathing - Tachypnea
>20 cpm
Can range from normal conditions to abnormal conditions
Causes:
Infection
Acidosis
Hypoxemia
Heart Failure
Tachypnea - Infection
Infection causes faster metabolism → need to burn more/ need energy in the face of infection → so pulmonary system also compensates because body needs more oxygen → thus ↑ respiratory rate
Tachypnea - Acidosis
High levels of acid present in the blood
Acidosis → produces a lot of carbonic acid (one major form of acid) and if not removed will cause injury to the body → so respiratory system works hard by eliminating a lot of CO2 which is a by product of metabolizing carbonic acid and is blown off as CO2
Tachypnea - Hypoxemia
Low levels of O2 in the blood
Tachypnea - Heart Failure
Heart can’t pump blood well and floods the pulmonary system
Left side of the heart fails to pump → damming of blood in left ventricle → damming in left atrium → blood and fluid will go back upstream to pulmonary bed causing it to be flooded → low oxygenation → compromised O2 and CO2 exchange (in the capillary beds) → hypoxemia → difficulty breathing → ↑ respiratory rate (tachypnea)
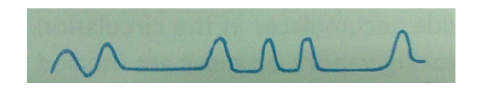
Breathing Pattern - Bradypnea
<12 cpm, slow
Causes: hypothyroidism, electrolyte imbalances (sodium, potassium), drugs, obesity
Thyroid gland releases thyroid hormones which interact with many body processes including respiration,
Low levels = slow metabolism which can also affect breathing pattern
Drugs such as anesthetic drugs/ pain reliever slow down the heart
Sign of poor prognosis
Breathing Pattern - Hyperpnea
Hyperventilation, deep breathing
Form of tachypnea
>20 cpm
Causes: neurologic, psychiatric, metabolic, infection, stroke, tumor
Psychiatric - some patients overexaggerate (TIA)
Deeper than tachypnea; may observe labor breathing
Breathing Pattern - Sighing
Frequently interspersed
Deeper breath
Can happen in between normal breaths
Frequent sighs may suggest hyperventilation syndrome - (common cause of dyspnea & dizziness)
Occasional sighs are normal
Breathing Pattern - Air Tapping
increasing difficulty in getting breath out
Causes: asthma, chronic obstructive pulmonary disease (COPD)
Asthma: no problem in air entry, problem is found in expiration of air; asthmatic patients have bigger lungs than normal people
Chronic Asthma - you can observe that their chest is bigger than normal individuals d/t air trapping
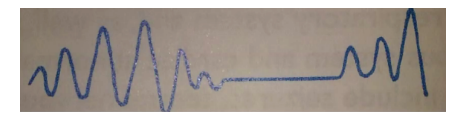
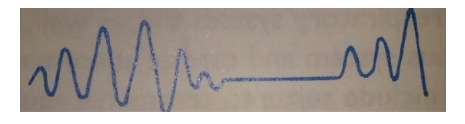
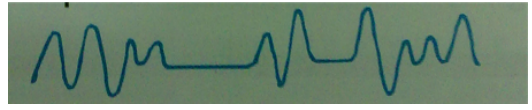
Breahting Pattern - Cheynes-Stokes
Varying periods of increasing depth interspersed w/ apnea (not breathing)
Apnea in between of increasing depths of breathing
“Parang naghihingalo”
More abnormal breathing; more serious pattern of breathing
Commonly seen in ICU & in pts who are dying
Causes: Obesity, Heart failure, Stroke, Brain tumor, TBI
Medical emergency. Call MD immediately.
Normal in children & older adults during sleep
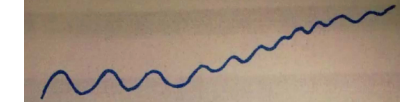
Breahting Pattern - Kussmaul
Rapid (tachypnic), deep, labored
Can also present with intercostal retractions (from video of pt c diabetic ketoacidosis)
Ketoacidosis - specific smell of ketones; d/t too much rigor in the body → poor sourcing of fuel leads to the body sourcing from ketones, with acid becoming a byproduct
Patients with poorly controlled rigor can go into ketoacidosis ● Causes: acidosis, renal failure
An effort to blow off a lot of acids (CO2) in the body
Breahting Pattern - Biot
Irregularly interspersed periods of apnea in a disorganized sequence of breaths
Causes: trauma, stroke, damage or pressure to medulla oblongata
Medulla oblongata: where the control of respiration is located
Similarity with Cheyne-stokes: there’s an apnea in between
Has equal depths in the breathing pattern compared to Cheyne-stokes; depth is not increasing
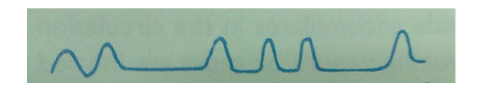
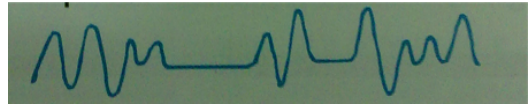
Breathing Pattern - Ataxic
Significant disorganization w/ irregular & varying depths of respiration
Indicates poor prognosis
Occasionally interchanged w/ biot; difference is there is more irregularity & depth is varying, and has no apnea
Worse than biot
Causes: damage to medulla oblongata (center for respiration; brain infection)
Influences on the Rate and Depth of Breathing: Increases
Acidosis
CNS Lesions (pons)
Anxiety
Aspirin poisoning
Hypoxemia
Pain
Influences on the Rate and Depth of Breathing: Decreases
Alkalosis
CNS Lesions (cerebrum-volitional breathing)
Myasthenia Gravis
Narcotic overdose (sedatives)
Obesity
Questions to ask pt (in order to come up with the right diagnosis or to be able to assess at what intensity the exercise should be given)
Is it present even when the patient is resting?
How much walking? On a level surface? Up stairs?
Is it necessary to stop and rest when climbing stairs?
What other activities precipitate it? What level of physical demand?
Orthopnea
SOB that begins or increases when the pt lies down; gets the feeling of being drowned
Quantified by the number of pillows needed to lie down comfortably (more venous return)
4-pillow orthopnea: need 4 pillows for comfort
In upright position, there is less venous return to the heart as compared to a lying position wherein gravity is eliminated thus more blood return to the heart.
Lying position will require the heart to work more. Thus, the heart of pts with congestive heart failure will have more difficulty in pumping the blood
Heart failure: pulmonary edema, congestive heart failure ● Pts will be more comfortable in the upright position
The blood that cannot be pumped by the system will just upstream to the pulmonary bed resulting into orthopnea.
How is Orthopnea quantified?
Quantified by the number of pillows needed to lie down comfortably (more venous return)
True/False: Orthopnea is worse compared to paroxysmal nocturnal dyspnea
True
Paroxysmal Nocturnal Dyspnea
A sudden onset of shortness of breath after a period of recumbency ■ Sitting upright is helpful
Does NOT happen immediately after assuming the supine position. Happens 3-4 hrs (sometimes 5 hrs) after assuming the recumbent position. The heart eventually gets tired from the ↑ venous return when the pt assumes a supine position.
Paroxysmal Nocturnal Dyspnea: Mechanism & Sx
When the heart gets tired, it would rest/ “fail” resulting in an upstream of blood on the left ventricle to the lungs.
Implies the heart is kind of weak but not as weak as overt heart failure.
Pt would wake up in the middle of the night and describes experiencing a “feeling of drowning”
Assuming the upright position helps in alleviating the sx and pt can go back to sleep afterward
Usually occurs once or twice a night
Platypnea
SOB that begins or increases when the pt is upright
Platypnea - Cardiac Defects
Cardiac defects, ie: ASD (atrial septal defect) with right-to-left shunt
In utero, there's an opening between the two atria, but would close when the baby is born d/t the pressure outside prompting the closure of the foramen ovale.
When the foramen ovale does not close, it results in atrial septal defect. Since the pressure on the left atrium is greater than the right atrium, the flow of blood will be from the left atrium to the right atrium. Overtime, because there is an ↑ of blood flowing from left to right, the pressure on the right side would exceed the left making it abnormal (process is called eisenmengerization).
Normal Shunt: Left-to-right
The right-to-left shunt would cause the SOB in the upright position
Platypnea - Worsening VQ Mismatch
Mismatch between ventilation and perfusion
Trepopnea
SOB that is pronounced on side lying
Due to a unilateral diseased lung
E.g. Dyspnea occurs more when lying on the side of the normal lung since these structures are being compressed.
Collapsed L lung and R sidelying = trepopnea
10 Ps of Dyspnea of Rapid Onset
Pneumonia
Pericardial Tamponade
Pneumothorax
Pump Failure
Pulmonary Constriction
Peak Seekers
Peanut
Psychogenic
Poisons
Pulmonary Embolus
10 Ps of Dyspnea - Pericardial Tamponade
Excessive fluid in the pericardial sac 50mL fluid accumulated in the pericardial space suffocates heart & prevents it from pumping well
10 Ps of Dyspnea - Pneumothorax
hole in air sac, air stays in the pleural cavity compressing on the lung parenchyma resulting to dyspnea, can lead to death in an instant
10 Ps of Dyspnea - Pump Failure
blood / fluid will get dammed up in the pulmonary bed
*In patients with CAV, post-bypass, post-angioplasty, ischemic cardiomyopathy, they might go into rapid onset dyspnea bc of excessive exercise/having another heart attac
10 Ps of Dyspnea - Peak seekers
(High altitudes) diff in breathing because body is not accustomed to high altitudes (thinner air / levels of O2
10 Ps of Dyspnea - Peanuts
Foreign body e.g. small objects lodged / stuck in the airway
Cough
Common symptom of a respiratory problem
Causes may be related to localized or more general insults at any point of the respiratory tract.
is a reflex response to stimuli that irritate receptors in the larynx, trachea, or large bronchi.
May be voluntary or reflexive response to an irritant
Cough can signal ____ sided heart failure
left
Cough - Sequence of events
Usually preceded by a deep inspiration closure of glottis
It is important to close the glottis for the air to be maintained inside below the level of the glottis down to the pulmonary/airway/air sacs
Contraction of chest, abdominal and pelvic muscles sudden spasmodic expiration (forces open the closed glottis; coughing out all the things that have been irritating the airway)
In the elderly or in patients who have difficulty in controlling or weak pelvic muscles, they involuntarily urinate when they cough.
Can do Kegel exercises to strengthen pelvic muscles
Air and secretion are exhaled
Sputum
Generally associated with cough
In more than small amounts and with any degree of consistency always suggests the presence of disease
Sputum characteristics may give a clue to some causes of sputum
The phlegm by itself or the sputum that sticks along the walls of the airway will cause irritation thereby initiating the cough reflex.
Cannot expel sputum without coughing.
Ask in a discreet way as this may be a social stigma
Hemoptysis
can arise from anywhere in the respiratory tract; from the glottis to the alveolus.
commonly results from infection, malignancy, or vascular disease; however, the differential for bleeding from the respiratory tree is varied and broad
Sputum - Bacterial infection
Yellow, green, rust (blood mixed w/ yellow sputum), clear, or transparent; purulent (pus); blood streaked; mucoid (thick), viscid (thicker)
clear/transparent - not yet prescribed with antibiotics in a patient with respiratory tract infection caused by bacteria, defer therapy as it will aggravate the pt’s condition. Wait for doctor’s clearance before continuing PT rehab.
Sputum - Viral Infection
mucoid, viscid; blood streaked (not common; possible that airways are wounded d/t continuous coughing); not too much hue
Sputum - Chronic Infectious Disease
Could be yellow or any color. All of the above; particularly abundant in the early morning; slight, intermittent, blood streaking; occasionally, large amounts of blood
Sputum - Carcinoma
slight, persistent blood streaking
Sputum - Infarction
Blood clotted; When large amounts of blood, pt should be brought to the ER already, as pt may die anytime d/t blood loss or obstruction in the airways
Sputum - Tuberculous Cavity
Large amount of blood
Breath Smells - Sweet, fruity
Diabetic ketoacidosis (c loss of sensorium; ketones - sweet smelling; loss of consciousness/ consciousness is waning); starvation ketosis
Breath Smells - Fishy, stale
Uremia (acute/chronic renal failure, too much toxic in blood, urea nitrogen, creatinine in the blood)
Breath Smell - Ammonia-like
Uremia
If noticed before PT session, defer therapy because the patient might not carry on with the exercises
Breath Smells - Musty fish
Fetor hepaticus: hepatic failure, portal vein thrombosis, portocaval shunts
Breath Smells - Foul, feculent
Intestinal obstruction, diverticulum (feces reroutes towards mouth)
Breath Smell - Foul, prutrid
Nasal/sinus pathology: infection, foreign body (common in pedia), cancer; respiratory infections: emphysema, lung abscess, bronchiectasis
Breath Smell - Halitosis (type of ulcer caused by bacteria
Tonsillitis, gingivitis, respiratory infections, vincent angina, gastroesophageal reflux, PUD (peptic ulcer disease, H. Pylori
Breath Smell - Cinnamon
Pulmonary tuberculosis
Physical Examination - Position
In the tripod position, there is an exchange of O2 and CO2 in the pulmonary bed
This alone can tell you that the patient is in respiratory distress
Physical Examination - Color
Cyanotic, bluish discoloration, pale
Hypoxemia
Physical Examination - Mental Status
Is the patient awake?
Alert, enthusiastic
Level of oxygen can always affect the level of mentation
Ex: If Pt is hypoxemic, the brain goes hungry so the sensorium can actually deteriorate
Physical Examination - Ability to speak
Can Pt speak in phrases? Full sentence?
Can belt out into songs
Physical Examination - Respiratory Effort
Is Pt speaking c so much effort?
Is it just a breeze? (To speak)
Physical Examination - Thoracic Contour
Chest will not be absolutely symmetric
Normally wider than it is deep
AP < transverse diameter ○ Should NOT be > 0.70 - 0.75
AP diameter increases c age
Up to 0.9
Upon checking the thoracic cage, you can assess whether Pt is a:
Barrel Chest (malapad)
Sign of air trapping
Chronic asthma
Emphysema
Cystic fibrosis
Pectus Excavatum
Now, if it’s not too deep it won’t render anything abnormal OR make Pt symptomatic it if doesn’t really compress the lungs or the heart
Compression of the heart & great vessels may cause murmurs
Pectus Carinatum
Doesn’t really impact negatively on the heart or the lungs UNLESS associated with some inborn metabolic derangement or any bony abnormalities
Sign that this may be part of some syndrome, but not necessarily compromises the heart and lungs
Kyphosis
Definitely compromises heart & lungs
Compresses and limits the airways
Unequal chest expansion and respiratory compromise caused by:
A collapsed lung & limitation of expansion
d/t fibrosis, muscular contracture, jt. mob problems, etc.
If there is UNEQUAL expansion, you want to observe the breasts (do not oggle if female)
Observe the collar or movement of the dress or shirt; collapsed lung on the lagging side
Etiology of unequal chest expansion
Extrapleural air: air is now in the pleural cavity compressing normal lungs
Fluid: also limits expansion
Mass (or Tumor)
Retractions suggest an?
obstruction to inspiration at any point in the respiratory tract
Retractions
Intrapleural pressure becomes increasingly negative degree and level of retraction depend on the extent and level of obstruction
Mechanism: Acts like a vacuum effect on the thorax
Ex: You bought a cup of sago’t gulaman. As you sip from a straw, you can’t sip further as it gets blocked
Your cheeks become the vacuum
Medical emergency. Bring pt immediately to the ER
Signs of Upper Airway Obstruction
Inspiratory Stridor
Hoarse cough or cry or barking cough
Alar flaring
Retraction at the suprasternal notch
Cyanosis
Signs of Upper Airway Obstruction - Inspiratory Strider
Expiratory is severe; audible even without steth
Signs of Upper Airway Obstruction - Hoarse cough or cry or barking cough
“Umiiyak na hindi basa”
Like a dog barking
Signs of Upper Airway Obstruction - Alar flaring
Sign of air hunger
Signs of Upper Airway Obstruction - Retraction at the suprasternal notch
Could tell level of obstruction
Signs of Upper Airway Obstruction - Cyanosis
signs of low levels of oxygen
Signs of Supraglottic Obstruction
Stridor tends to be quieter
Because the obstruction is not full
Muffling voice (“hot potato in mouth”)
Dysphagia
No cough
Because you’re not irritating the most irritating part of the airways
Awkward position of head and neck to preserve the airway
Looking for that position to establish a good airway (air can come in better)
Signs of Infraglottic Obstruction
Stridor tends to be louder, rasping
Hoarse voice
Swallowing not affected
Cough is harsh, barking
Head positioning is not a factor
Because no matter the position of the head, pt will still have difficulty breathing since the obstruction is infraglottic, which is more difficult to attend to
Peripheral Signs of Airway Obstruction
Cyanosis
Pursing
Clubbing
Alar flaring
Peripheral Signs of Airway Obstruction - Cyanosis
lips, nails
Depending on the severity, when a pt becomes cyanotic, cyanosis of the lips and nails may simultaneously occur
Not really evident on the onset
Peripheral Signs of Airway Obstruction - Pursing
Pursed lip breathing = something hot between mentis and lower lip and it seems like you are blowing that area
Peripheral Signs of Airway Obstruction - Clubbing
finger nails
Almost always indicates chronic hypoxemia
Peripheral Signs of Airway Obstruction - Alar flaring
air hunger, esp. alveolar involvement
Suggest cardiac or pulmonary difficulty
Chronic pulmonary or cardiac problem
In neonates: congenital cardiac or pulmonary defect
Auscultation - Breath sounds characteristics
Intensity
Pitch
Quality
Duration
Auscultation - Reminders
As PTs, it’s okay if you’re listening for normal breath sounds but once you hear abnormal breath sounds, refer to a doctor
Start from top to bottom
Always compare both sides
It’s not checking all on one side first, but has to be contralateral side
Listen to the chest anteriorly and laterally as the patient breathes with mouth open, and somewhat more deeply than normal.
Listen to the breath sounds, noting their intensity and identifying any variations from normal vesicular breathing.
Breath sounds are usually louder in the ________ lung fields
upper anterior lung fields
________ breath sounds may be heard over the large airways, especially on the right
Bronchovesicular breath sounds
Normal Breath Sounds - Vesicular
Heard over most of the lungs
Most commonly auscultated breath sounds
Low pitch
Rustling quality
Soft and short expiration
Sounds become even softer during expiration
More prominent in thin individuals or children
Diminished in the overweight or muscular individuals
Inspiratory time (I) is longer than Expiratory time (E)
Approx. I:E of 3:1
Can be best heard in most areas of the lungs but are most prominently heard at the lung bases and periphery
Normal Breath Sounds - Bronchovesicular
Heard over the main bronchus area and over upper right posterior lung field
Breath sounds that you listened to over the bronchioles would be different if you listen to the breath sounds over the air sacs
When you place the stethoscopes over the lung parenchyma, over the air sacs → ______
Vesicular
There would be parts in the lungs that would be covered by the bronchioles and air sacs → ______ sound
Bronchovesicular
Bronchovesicular sounds characteristics
Medium (mid-range) pitch and intensity
Expiration equals inspiration
Normal breath sounds
Inspiratory time (I) is often equal to Expiratory time (E)
I:E of 1:1
Intermediate/ mixture of:
Higher-pitched bronchial sounds
Low-pitched vesicular sounds
Bronchovesicular sounds can be heard hroughout the lung fields, but can be commonly heard in the __________
upper third of the chest
Bronchial / Tracheal (Tubular) sounds are heard only over _____
trachea
Bronchial / Tracheal (Tubular) sound characteristics
High pitch
Hollow or tubular sounds
Imagine blowing through a pipe
Loud and long expirations, sometimes a bit longer than inspirations
True/False: Tubular sounds are quieter than vesicular sounds
False
Tubular sounds - If heard in the peripheral of the lungs, this could be a finding which is _______________________
abnormal and suspicious for pneumonia, pleural effusions or atelectasis
Vesicular - Duration, Intensity, Pitch, Locations
Duration | Inspiratory sounds > Expiratory sounds |
Intensity of Expiration | Soft |
Pitch of Expiration | Relatively low |
Locations where heard normally | Over most of the lung |