BME 365S Exam 1
1/27
Earn XP
Description and Tags
BME 365S Physio II Exam 1
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
4 functions of the respiratory system
1) Gas exchange
2) regulation of pH: done by retaining or excreting CO2
3) Protect against inhaled pathogens/irritating substances: respiratory epithelium
4) Vocalization: air moving across vocal cords creates vibrations
External vs internal respiration
External resp is breathing: inspiration & expiration
—>Pulmonary circulation has 500 mL of blood (50% total amt)
Internal resp is exchange of gases between blood & cells
3 functions of the upper resp system (airways)
1) Warm air to body temp
2) Add water vapor —> 100% humidity
—>Prevent exchange epithelium from drying out
3) Filter foreign material: bacteria, viruses, inorganic particles
Explain the airway epithelium (mucus/saline). What cells?
Goblet cells secrete mucus w/ immunoglobulins (Ig aka antibodies)
Underlying cilia push mucus toward pharynx where it’s swallowed
Fluid layer beneath mucus to prevent cilia-mucus sticking
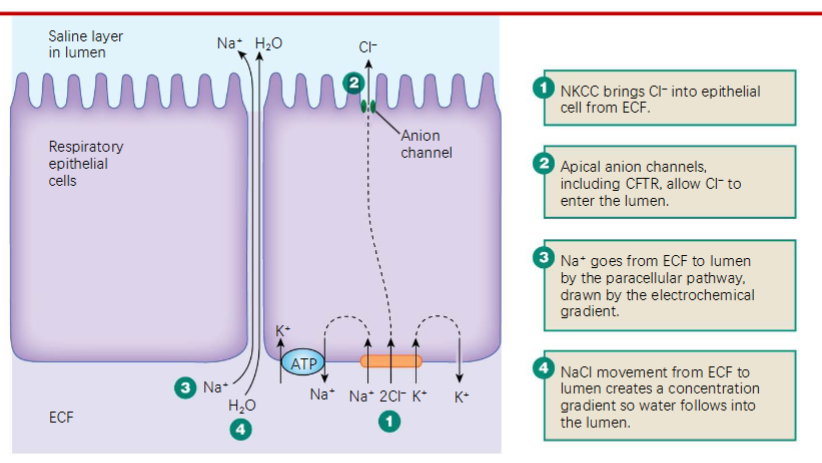
Model of saline secretion
1) NKCC symporter brings Cl- from ECF → inside epithelial cell
2) Apical anion channels allow Cl- epithelial cell → lumen (airway)
3) Na+ goes from ECF→ lumen via paracellular pathway (due to electrochem gradient)
4) NaCl mvmt from ECF→ lumen makes cxn gradient, so water follows into the lumen
Air flow equation (Poiseuille’s law)
Airflow Q = ΔP/R
Poiseuille: R is func of Lμ/r4 where L is length of tube
3 types of alveolar cells (and function)
Type I alveolar epithelium: rapid gas exhange, 95% of alveolar surface, thin squamous cell
Type II alveolar epithelium: produce surfactant to dec surface tension & help expansion of lungs
Alveolar macrophage (dust cell); ingest foreign material
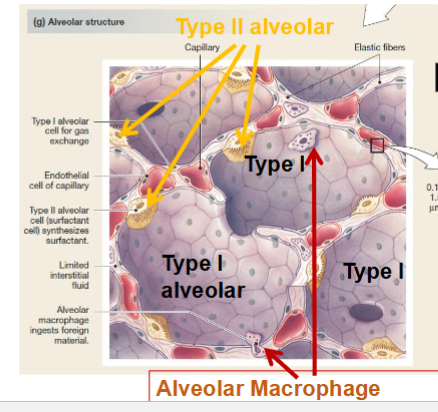
What’s between alveoli cells?
Blood vessels fill 80-90% of the space, also connective tissues w/ elastin & collagen fibers to give elastic properties
NO muscle — it would block gas exchange
Explain pleural sac & pleural fluid. Interpleural pressure?
Double MB around lung w/ fluid in between. Creates moist slippery surface so lungs can move within thorax, holds lungs tight against thoracic wall
Interpleural pressure is sub-atmospheric, -3 mmHg.
Ideal gas law & boyle’s law & dalton’s law
Ideal: PV=nRT
Since n & T are constant for humans we get Boyle’s law: P1V1 = P2V2
Dalton’s law: Ptotal = Pa + Pb + Pc
Pgas = Patm* % of the gas in the atmosphere
What happens in inspiration?
Active process: Diaphragm contracts, external intercostals & scalene contract
Scalenes lift sternum & upper ribs
Thoracic cavity expands (inc volume, dec pressure to 759 mmHg)
Air flows inwards into low pressure space
What happens in expiration? Quiet breathing?
Passive process: diaphragm relaxes
Forced: internal intercostals & abdominal muscs contract
Dec volume, pressure increases (to 761 mmHg), air pushed out (return to 760 mmHg)
In quiet breathing, diaphragm causes 60-75% volume change, rib cage mvmt causes remaining 25-40%
Quiet breathing: PO2 & PCO2 barely change bc amt O2 entering alveoli = amt O2 entering blood. Also amt fresh air entering lungs is only 10% total lung volume
Ventilation diseases (3)
Neuromuscular diseases that affect motor control of ventilation:
1) Myasthenia Gravis: ACh receps of motor end plates of skeletal musc destroyed
2) Polio: virus that damages MNs @ spinal cord, paralyzes skeletal muscs
Pneomothorax: sealed pleural cavity is opened to atmosphere, lung collapses
→Treated w/ tube thoracostomy (insertion of chest tube)
Resp volumes & capacities
Tidal Volume (TV): normal breathing
Inspiratory reserve volume (IRV): max additional inspiration
Expiratory reserve volume (ERV): max additional expiration
Vital Capacity (VC): TV + IRV + ERV
Can’t be measured w/ spirometer:
Residual volume (RV): air left after complete expiration
Total lung capacity (TLC): VC + RV
Total pulmonary ventilation vs alveolar ventilation?
Total pulmonary ventilation (aka respiratory minute volume): ventilation rate (breaths/min) * tidal volume (mL/breath)
Alveolar ventilation: amt fresh air reaching alveoli per minute: ventilation rate * (tidal vol - dead space vol)
Anatomical dead space: air remaining in airways
Compliance v elastance
Compliance: expansibility, how easily it stretches
Compliance = ΔV/ΔP, aka slope of P-V curve
Elastance: elastic recoil, ability to return to original shape
ex: Emphysema: alveoli enlarge & lose elasticity →difficulty exhaling bc less recoil
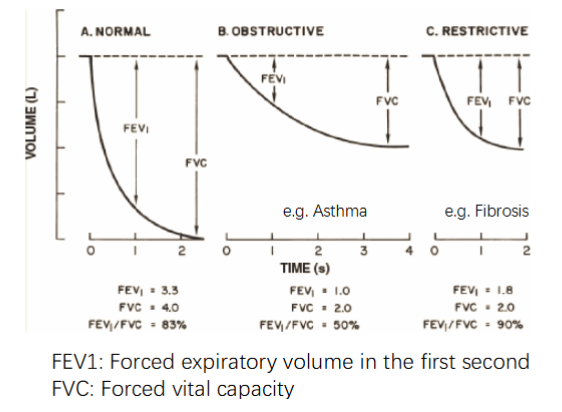
Obstructive vs Restrictive lung diseases.
Restrictive: dec in lung compliance→resp musc must work harder to stretch stiff lung
→Caused by scar tissue or inadequate surfactant
Obstructive: dec air flow bc inc airway resistance from physical obstructions: mucus, asthma, bronchoconstriction
How does bronchoconstriction & dilation happen?
Bronchoconstriction
By histamine: allergic rxn or tissue damage → release histamine → bronchoconstriction
By nervous system: inhaling irritants → parasym neurons signal → bronchoconstriction (defense mechanism)
Bronchodilation
By CO2: during expiration, CO2 inc, relaxed bronchiolar smooth musc → bronchodilation
By nervous system: epinephrine activates B2 adrenergic receptor → symp nervous system activates → relaxation of bronchial smooth musc → bronchodilation
Role of surfactants. Pathophysiology?
Dec surface tension of alveoli → dec R of lung to stretch so easier to expand → inc lung compliance
Surfactant more concentrated in smaller alveoli
Newborn Respiratory Distress Syndrome: babies born prematurely w/out adequate surfactant, thus expend huge amt energy to breathe. Must treat via aerosol administration of artificial surfactant
Controlling bronchioles & alveolar blood flow. Cause of low alveolar PO2
Arteriole diameter regulated by O2 content of surrounding interstitial fluid: if ventilation decreases, PO2 dec so blood near alveoli doesn’t get oxygenated. Thus, constriction around under-ventilated alveoli so that blood flows to better ventilated alveoli
→Cause of low alveolar PO2: high altitude so air has low O2; inadequate ventilation from inc airway resistance or dec lung compliance or CNS depression from drugs/alcohol
Bronchiolar diameter mediated by CO2 contents
Capillaries & bronchioles are collapsible as function of blood pressure
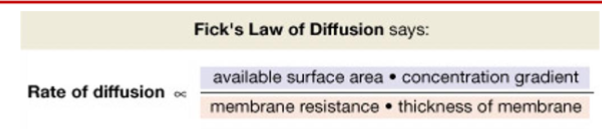
Diffusion rate across membrane
Fick’s Law: rate of diffusion = (surface area * cxn gradient) / (MB resistance * MB thickness)
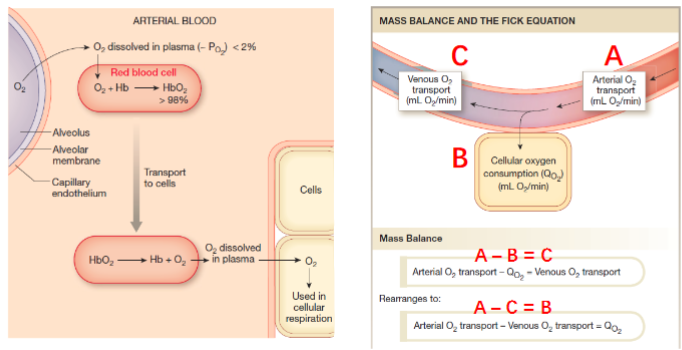
Oxygen transport?
Only dissolved O2 can be utilized by body:
98% of oxygen transported in RBCs via hemoglobin (Hb)
2% dissolved in plasma (increases w/ temp)
270 million Hb per RBC
Mass balance: Arterial O2 transport - venous O2 transport = cellular oxygen consumption
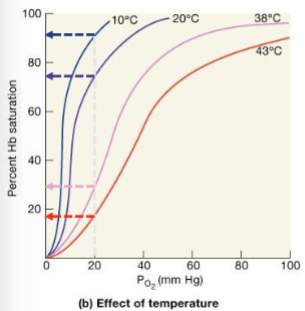
O2-Hb Binding saturation curve. How to shift curve? Fetal Hb?
Binding affinity inversely related to acidity & cxn CO2: inc CO2 or lower pH (inc H+) → dec affinity of Hb to O2, SHIFT RIGHT
Inc temp (ex: exercise): shift right so Hb releases more O2. Lactic acid from exercising → lower pH → additional O2 released
Fetal Hb: stronger affinity to O2 (SHIFT LEFT). 2 gamma protein chains allow binding O2 even in the low O2 enviro of placenta
At alveoli PO2 = 100 mmHg, in resting cells Hb is 75% saturated
In exercising muscle PO2=20mmHg, Hb is 35% saturated
Carbon dioxide transport?
CO2 20x more soluble in fluids than oxygen: 7% dissolved in blood, 93% diffused into RBCs where 70% converted to bicarbonate ion & 23% binds Hb
High PCO2 depresses CNS function → confusion, coma, death
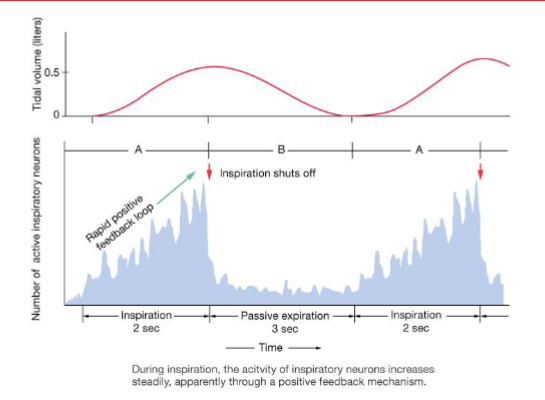
Control of ventilation in brain? Respiratory neurons?
Resp neurons in medulla oblongata control inspiration & expiration
→Dorsal Respiratory Group (DRG): insp neurons, control musc of thorax & diaphragm
→Ventral Respiratory group (VRG): neurons control musc for active expiration & forced inspiration
Neurons in pons modulate ventilation
→ Pontine respiratory groups (PRG): provide tonic input to medullary network
Ventilation modulated by CO2, O2, H+
Chemoreceptors in ventilation. Location & function?
Nucleus Tractus Solitarius (NTS, medulla): receive sensory info from central & peripheral chemoreceps
→Central chemoreceps: in medulla, monitor cerebrospinal fluid (CSF) composition & respond changes in CO2
→Peripheral chemoreceps: in aortic wall & carotid artery, sense changes in O2, pH, PCO2
What are some protective reflexes? What does regulation of respiratory rate depend on?
Reflexes: in response to inhaled particles or noxious gases: bronchoconstriction, coughing, sneezing
Regulation of resp rate: depends on conscious & unconscious thought, emotional state, anticipation
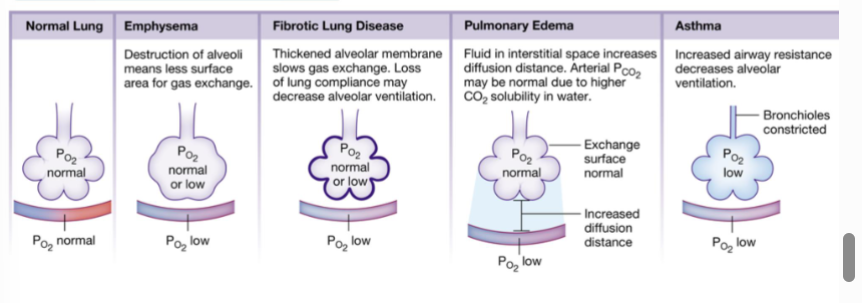
Pathologies causing hypoxia? (4)
Emphysema: destruction of alveoli → less SA for gas exchange
Fibrotic lung disease: thickened alveolar MB & dec lung compliance → slows gas exchange & dec alveolar ventilation
Pulmonary edema: fluid in interstitial space → inc diffusion distance, higher PCO2 bc higher CO2 solubility in water.
Asthma: inc airway resistance → dec alveolar ventilation