Fetal Heart Tones and Monitoring MC Exam 2 Blueprint
1/25
Earn XP
Description and Tags
MC Exam 2
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
Fetal Reserves
a healthy maternal-fetal placental unit, there is oxygen and nutrients available to the fetus beyond baseline needs of the fetus.
When O2 is decreased, blood flow is deferred to fetal vital organs, then adaptation to labor may begin to be affected
Prolonged or repeated fetal hypoxemia leads to decompensation
Non-Hypoxic fetal reflex
FHR accelerations
Compensatory response to hypoxemia
variable decelerations
Impending decompensation responses
late decelerations
Normal FHR
(110-160) with moderate variability and uterine contractions
Baseline is recorded over a 10-minute period
Absent FHR variability Definition
abnormal finding
No detectable amplitude range to unaided ey
Undetectable variations (0-2 (3) bpm)
Absent FHR Variability Causes
Fetal sleep cycles
Fetal tachycardia
Extreme prematurity
CNS depressing medications
Congenital anomalies
Neurologic injury
Interruption of fetal oxygenation
Minimal FHR Variability
Abnormal Finding
Amplitude range ≤ 5 beats/minute
Visible to unaided eye
similar causes to absent
Moderate FHR variability
Normal Finding - indicates normal FHR regulation and no significant oxygen issues
Peak to trough amplitude is 6-25 bpms
Marked FHR Variability
Greater amplitude range
Often represents normal variant
Clinical significance not fully known
Abnormal Variability Nursing Interventions
Change maternal position to side-lying
Reduce vena cava and aortic compression
Increase supplemental oxygen
Increase IV fluid administration
Monitor response to interventions
Sinusoidal Pattern
Regular, smooth, undulating wavelike pattern
Must persist ≥ 20 minutes
Associated with:
Severe fetal anemia
Chorioamnionitis
Fetal sepsis
Opioid medication effects
Placental Abruption
FHR Acceleration
Increase in FHR over baseline for greater or equal to 15 seconds (15x15), but equal to or less than 2 minutes.
Before 32 weeks gestation, FHR acceleration definition is equal or greater than 10 bpm over baseline for equal or greater than 10 seconds (10x10).
Indicates adequate fetal oxygenation
Highly predictive of normal fetal acid-base balance
Reassuring sign of fetal well-being
Prolonged Acceleration
acceleration greater than or equal to 2 minutes but less than 10 minutes
Early Decelerations
decrease of FHR below baseline in relation to UC’s: not a bad sign
Nadir (lowest point) of deceleration occurs at the same time as the peak of the UC.
They are a mirror image of one another.
Recovery of FHR baseline is immediate when UC is done.
Early Deceleration Causes
Fetal head compression during UC
Can be sign of baby dropping
Variable decelerations
abrupt decrease of FHR below baseline greater or equal to 15 bpm, lasting equal or more than 15 seconds, but less than 2 minutes
variable shapes and sizes - may be shaped as V’s or U’s
occurs before, during or after UC’s,
Late Decelerations
Nadir (lowest point of FHR) occurs after peak of UC
slow return to baseline when UC is already done
Late Deceleration Causes
Uteroplacental insufficiency
Late Deceleration Interventions
Reposition mom, give mom fluid bolus, figure out contraction frequency, if on petocin slow or stop, give oxygen later if needed
Prolonged Deceleration
abrupt decrease in FHR baseline that is greater or equal to 15 bpm, lasting more than 2 minutes, but less than 10 minutes
Extended interruption of fetal oxygen supply
Mechanisms similar to late/variable decelerations but longer duration
Can lead to fetal metabolic acidemia if sustained
Normal Contraction Frequency
No more than 5 contractions in a 10 minute period
Category 1 FHR
baseline is 110-160, variability moderate, early decels absent or present, accelerations absent or present
Category 2 FHR
= equivocal—not 1 or 3—yet… they include any of the following: bradycardia, with absent variability, minimal baseline variability, absent baseline variability not accompanied by recurrent decelerations, marked baseline variability, absence of induced accelerations after fetal stimulation, recurrent variables with minimal or moderate variability, prolonged decelerations greater than 2 minutes, but less than 10 minutes, recurrent late decelerations with moderate variability, variable decelerations with slow return to baseline or overshoots (shoulders)
Category 3 FHR
absent variability with any of the following: recurrent late or variable decelerations, bradycardia, or sinusoidal pattern
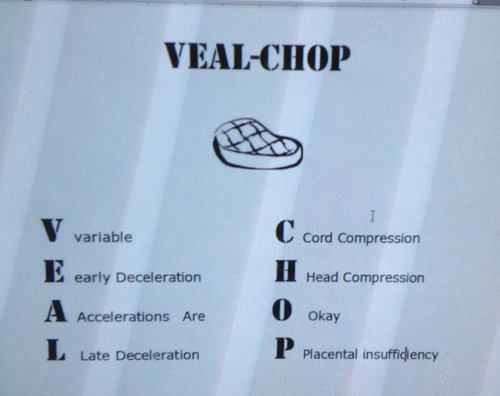
VEAL CHOP