Diagnostic approach to LRT disease in horses
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
What presenting signs indicate LRT disease?
Cough
Bilateral nasal discharge
Tachypnoea/Dyspnoea
What are the causes of a cough in LRT?
Stimulation of irritant receptors
Forced expiration against closed glottis
high velocity expiration
Possible causes:
Physical stimulus (Foreign material, turbulent air, mucus)
Chemical stimulus (Osmolarity, irritant)
Increase response to stimulus in inflammation
How does airway inflammation cause bilateral nasal discharge?
Increased mucus production
Altered mucus composition
(result in bilateral mucopurulent discharge)
What is the significance of bilateral/unilateral discharge?
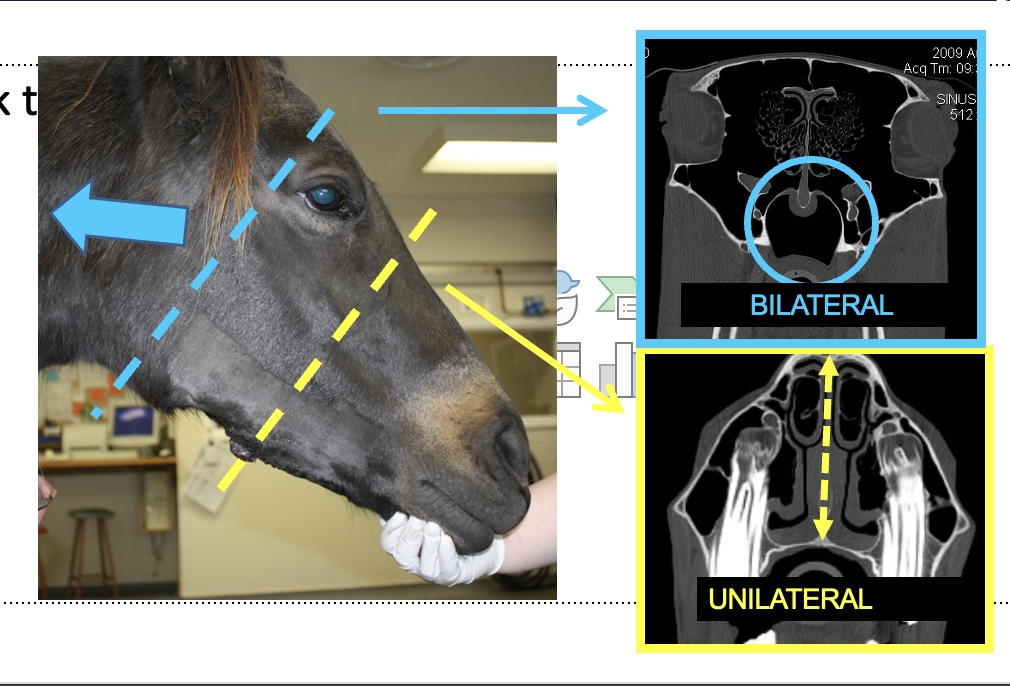
Helps determine location of origin
bilateral = behind nasal septum
unilateral = either side of nasal septum
if guttural pouch can begin unilateral + become bilateral
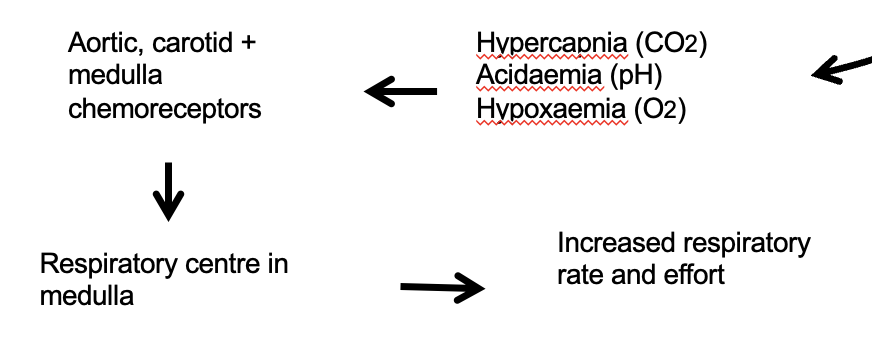
How does LRT disease cause tachypnoea/dyspnoea?
Hypoventilation
V/Q mismatch
Impaired gas diffusion in alveolus
What is VO2 max? and the significance of this in horses?
Maximal oxygen consumption
A fit thoroughbred only uses 4% VO2 at rest so signs of resp disease not always apparent at rest
What history and signalment factors can determine likelihood of resp disease presentation?
Disease time course and features
Herd or individual problem
Age and use of horse
Management and environment
Coexisting problems
What should be observed from a distance before physical exam?
Posture (extended head and neck = severe respiratory distress, tail lifted)
Abdominal effort
Respiratory Rate
Respiratory Depth –
Pattern – biphasic?
Hypertrophy of Ext. ab. oblique
‘Heave line’
Why is collapse more likely in URT during inspiration?
Relatively negative pressure in trachea cf to atmorsphere whereas relatively positive in lungs compared to body so collapse more likely in trachea
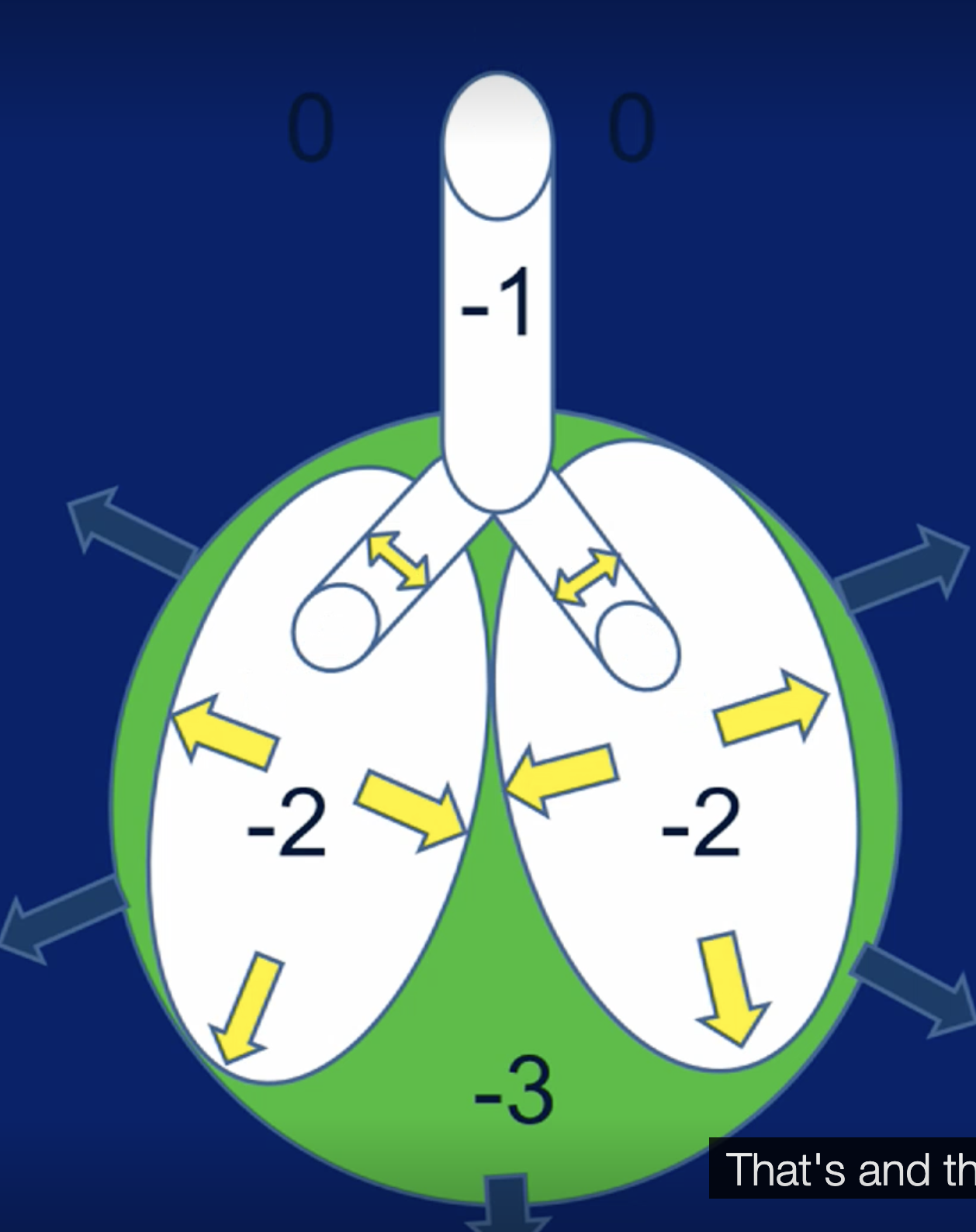
Inverse true in expiration
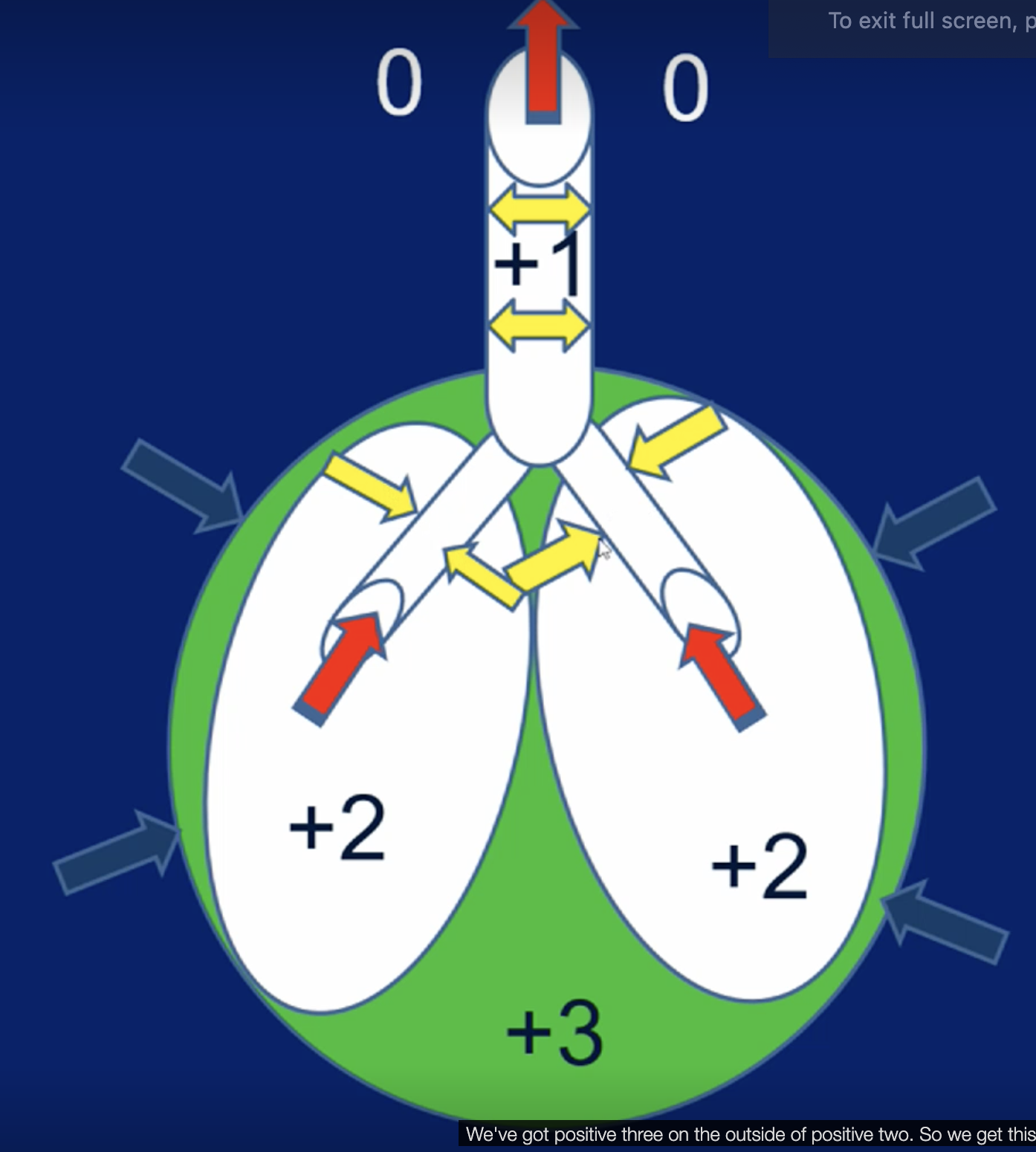
Where is collapse most likely to occur on inspiration and expiration?
Inspiration- URT
Expiration - LRT
What would you look at on clinical examination of suspected LRT disease?
All systems
Temp / Heart rate
Ventral oedema? (more likely cardiogenic cause)
Guttural Pouches & Lymph nodes (submandibular)
enlargement, discharges
Nares and Nasal Passages
airflow obstruction
discharges
Where should you auscultate the resp tract in horses?
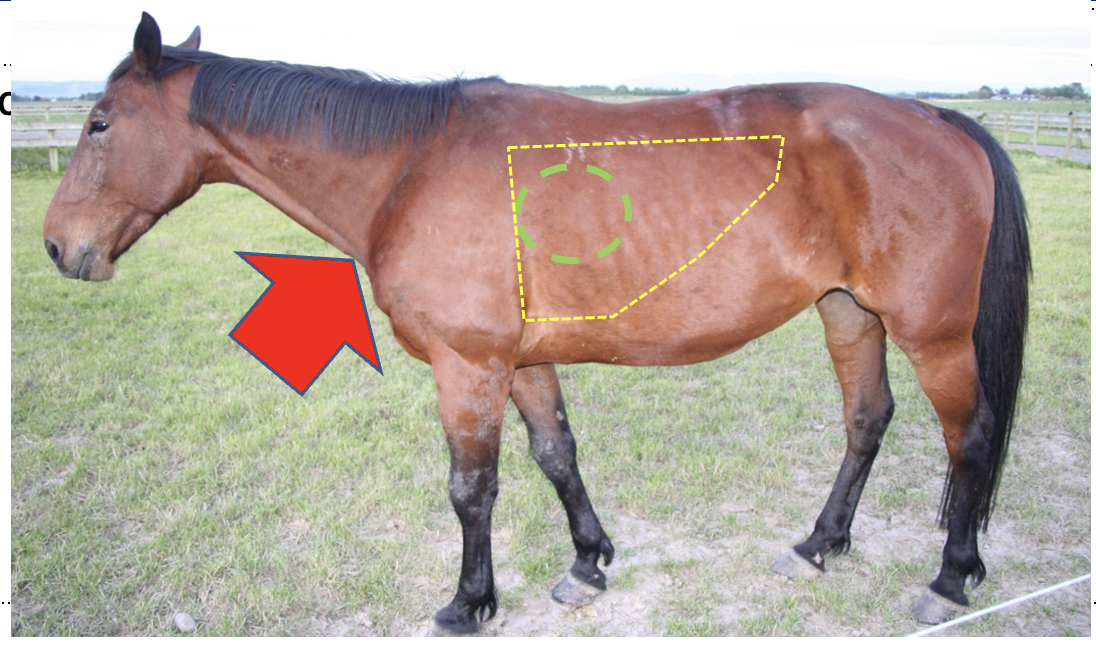
Base of the trachea
Then the green circle- where normal lung sound is going to be loudest, bifurcation of trachea
And then whole lung
What do normal breath sounds sound like?
turbulent air in large (>2mm) airways
Soft blowing sound
Inspiration > expiration
Faster air = louder
Low frequency sounds travel best through normal lung
What are the main adventitiouos (abnormal) sounds?
Wheezes
Crackles
Pleural rubs
Cough
Expiratory Grunts/groans
What does a wheeze sound like?
'Musical note, whistling sound'
What causing wheezing?
Airway narrowing and vibration which can be caused by:
Thickened wall
Intraluminal obstruction (mucus/foreign body)
Bronchospasm
Extra luminal compression
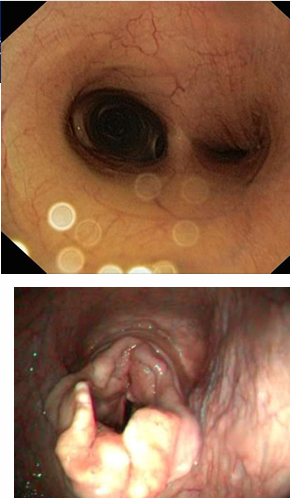
What is being shown here
Mucus accumulation
What are the types of wheezes?
Polyphonic wheeze
Monophonic wheeze- single sound (in image)
What is the bernoulli effect?
High velocity air causing lower pressure
Further narrowing of airway
Can cause wheeze
When are the lower airways smallest and most likely to collapse (Insp/exp, early/end)?
Inspiration
Expiration, particularly at end
When does wheezing occur most commonly in the LRT and URT?
LRT – most common end expiratory
URT – most common inspiratory
(often insp. + exp.)
What are the two types of crackles?
Coarse crackles
Bubbling mucus
Insp or expiration
Radiate widely
Fine crackles
Popping open of collapsed small airways
Most common: early insp
What are pleural friction rubs?
Inflamed parietal and visceral pleural membrane (ex- if they have fibrin on)
Variable- fine crackles to sandpaper rubbing together
Usually insp and exp at same point in resp cycle
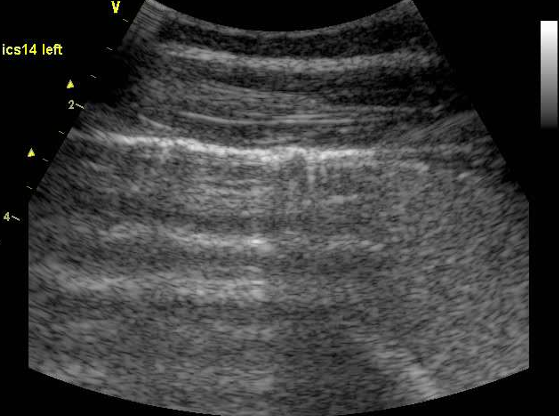
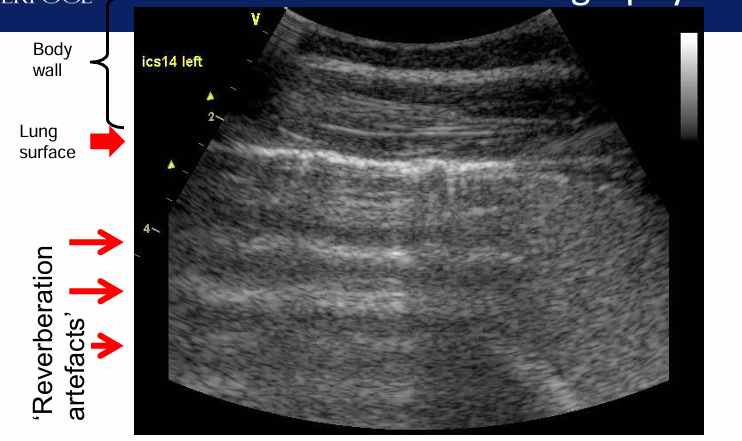
How can you do equine thoracic auscultation (using rebreathing)?
Increases PaCO2
Increases Respiratory Rate and Tidal volume + resp effort
Increases normal and abnormal resp. sounds
Cough = abnormal (sign of inflam)
To exacerbate adventitious sounds

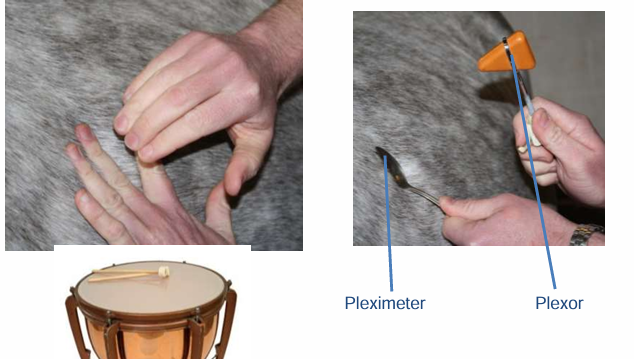
How can you use thoracic percussion?
If you have airfilled lungs will get resonant percussion
Dull sound with fluid (ex- pleural effusion)
What further diagnostic tests can you do for LRT disease?
Laboratory and Clinical Pathology
Nasopharyngeal swab
Endoscopy and transendoscopic tracheal aspirate
Percutaneous tracheal aspirate
Bronchoalveolar lavage
Thoracocentesis
Imaging
Radiography
Ultrasonography
Lung biopsy
What blood samples can you take for LRT disease?
Inflammatory profile:
WBC / proteins / Fibrinogen /Serum Amyloid A —> all increase in inflam
fibrinogen = acute but remain longer than SAA
serum amyloid A (SAA) = acute + decrease over 24hrs
Lactate
Tissue hypoxia (if marked resp. disease)
Blood gas profile
Arterial Blood gas (will indicate cause of hypoxia)
Hypoxaemia
Hypercapnia
What tests can you do for specific viruses/bacteria in the LRT?
Polymerase Chain Reaction (PCR) to identify RNA/DNA of specific viruses / bacteria
Paired serology
Virus isolation from:
buffy coat
nasopharyngeal swabs (insert to level of lateral canthus)
Bacterial Culture / identification
What can an endoscope be used for?
Imaging
Sample
(URT, trachea, carina —> 1st point bifarcation)
What LRT samples can be taken?
Tracheal aspirate (TA) Transendscopic or transtracheal
Bronchoalveolar Lavage (BAL)
Thoracocentesis
How is a transendoscopic tracheal aspirate performed?
add saline
collect fluid from tracheal sump
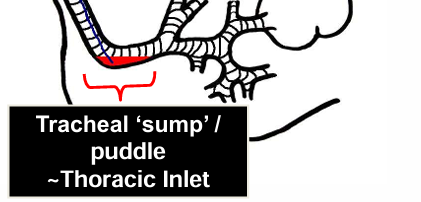
What are the advantages and disadvantages of transendoscopic tracheal aspirate?
+ve
easy
non-invasive
sample representative of whole lung
-ve
sample contaminated by nasopharyngeal flora and equipment (not best for bacteriology)
specialist equipment required
How is a transtracheal aspirate performed?
puncture through skin (between cartilage rings)
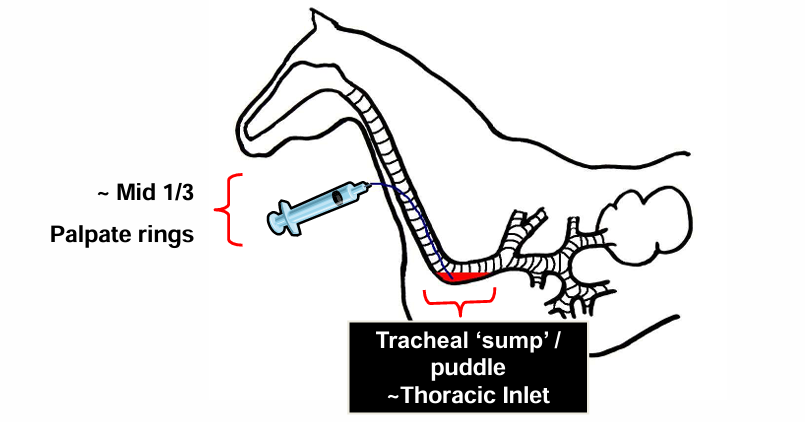
What are the advantages and disadvantages of transtracheal aspirate
+ve
no pharyngeal contamination
no specialised equipment
useful in young foals when endoscopes too large
-ve
Horse may cough catheter into pharynx and contaminate sample (can cause invert)
invasive
cellulitis
subcutaneous emphysema
How can you analyse a tracheal aspirate sample?
Differential cell counts
macrophages should be predominant cell type in normal
Abnormal = >20% neutrophils
Abnormal = Presence of mast cells, eosinophils (inflam)
Presence of mucus, amount, Curschmann’s spirals
Gram stain
Especially for intracellular organisms
Bacterial culture / sensitivity
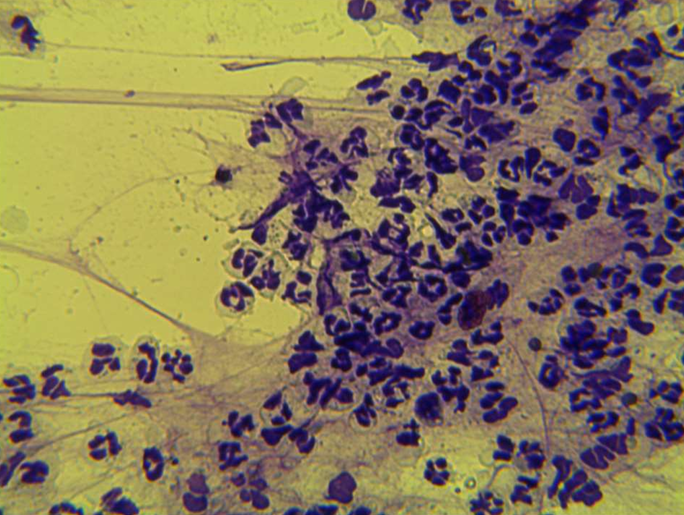
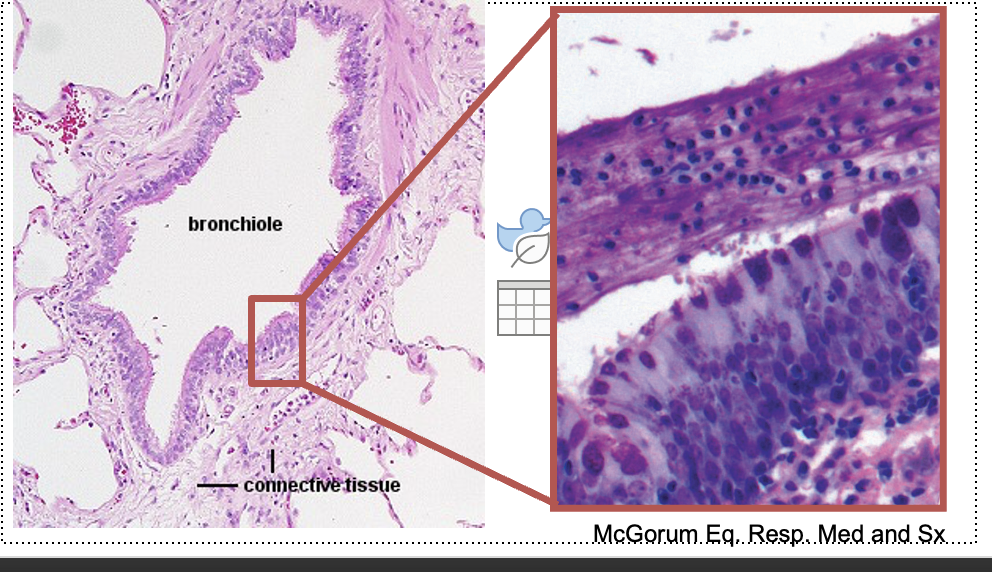
What does this show?
non septic
LRT inflam
neutrophils (not degenerate)
How is a bronchoalveolar larvage carried out? What is it suitable/unsuitable for?
Specific BAL tube or >2m endocope
Small area of distal airway lavaged with saline
Best for diffuse lung disease
Good for cytology
Unsuitable for bacteriology
What should a BAL sample look like?
Surfactant so must get foam on your sample
(surfactant = line bronchioles/alveoli + increase compliance of lungs)

What are the advantages and disadvantages of BAL?
+ve
sample obtained from DISTAL airways = most commonly affected
Best correlation with pulmonary function and histopathology
equipment cheap and accessible (unless endoscopically obtained)
-ve
Site may not be appropriate in animals with
localised pulmonary abscesses or pneumonias (cranioventral lobes)
Pharyngeal contamination
Culture not useful
Invasive
What characteristics of LRT disease might be seen when performing BAL?
Mostly severe / chronic / treatment failures
e.g. neutrophilic vs mast cell inflammation
mature vs degenerate neutrophils
identify pathogens
When should BAL used vs TA?
BAL: better correlation with:
Airway obstruction (pulmonary function testing)
Exercise induced hypoxaemia
Lung histopathology
TA is most useful for
Bacteriology
Focal lung lesions e.g. Abscess/neoplasia
Tracheal inflammation
What can be seen on this radiograph? Is it normal?
normal
What can be seen on this radiograph? Is it normal?
show pleural effusion
can see pleural surface + lung anatomy due to fluid
can see diaphragm
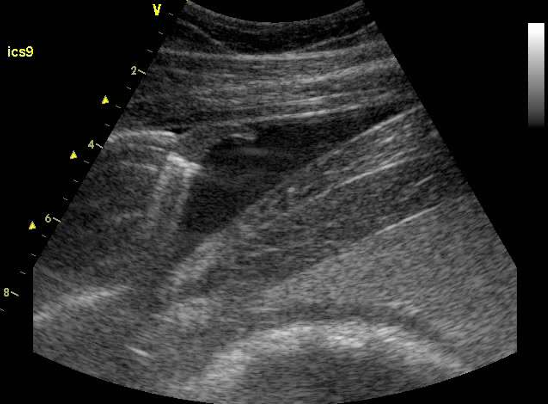
When is thoracocentesis indicated?
Whenever there is a pleural effusion
What are the clinical signs of pleural effusion?
Increased resp. rate
Dull thoracic percussion ventrally
Pleurodynia
Ultrasound