Unit 3 Lecture Objectives
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
Describe the functions of different layers of connective tissue that surround and are associated with the skeletal muscles
Epimysium
Surrounds entire muscle
Perimysium
Surrounds fascicles (bundles of muscle fibers)
Contains blood vessels and nerves
Endomysium
Surrounds individual muscle cell
Contains capillaries
Describe the unique features of the skeletal muscle compared to a typical cell
multinucleated
Develop through embryonic cells called myoblasts
Contains myofibrils
Smooth ER is sarcoplasmic reticulum
T-tubules
Describe the structural and functional unit of the muscle
sarcomere
Between Z lines
Has thick filaments (myosin) and thin filaments (actin)
Dark band is called the A band
Light banned is the I band
Explain how the proteins in the thick and thin filaments regulate muscle contraction and relaxation
thin (actin)
Tropomyosin (Tm)
Troponin (Tn)
TnI
C-terminus
Helps anchor the troponin complex to actin and tropomyosin, holding filament in a blocked state and preventing muscle contraction
Switch region
Binds the hydrophobic pocket in TnC
TnC
N-terminus
contains calcium-binding sites; key calcium sensor
TnT
N-terminus
Helps regulate function of troponin complex
Compare and contract the three functional states of the thin filaments with the three states in which the myosin heads can exist
thin
Blocked state
Unbound/detached myosin crossbridge
Closed state
weakly bound XB
Open state
Strongly bound XB
Distinguish between the calcium-mediated activation of the thin filaments and crossbridge-mediated activation of the thin filament
calcium-mediated activation
Electrical signal (like an action potential) causes release of calcium ions
Calcium ions bind to troponin, causes tropomyosin to move
Movement of tropomyosin exposes myosin-binding site
Blocked state to closed state
Crossbridge-mediated activation
Closed state to open state
Crossbridge forms, holds tropomyosin in “on” position
Initiates power stroke, where myosin head pulls actin filament and muscle contraction occurs
Describe the various steps involved in excitation-contraction coupling and relaxation of the skeletal muscles
excitation-contraction coupling
Action potential arrives, ACh released into synaptic cleft. Binds to receptors on sarcolemma
action potential travels along T-tubules
Action potential activates dihydropyridine (DHP) receptors
Triggers opening of ryanodine receptors (RyRs), causes rapid release of Ca2+
Ca2+ binds to troponin, causing movement of tropomyosin and exposure of myosin-binding sites
Crossbridges form, hydrolysis of ATP fuels power stroke, shortening the sarcomere and causing muscle contraction
Relaxation
Nerve stimulation stops, RyRs close
Ca2+ pumped back into SE by SR Ca2+ pumps (SERCA)
Troponin returns to original shape, tropomyosin moves back to block myosin-binding sites
Cross-bridges detach, muscle relaxes
Why does rigor mortis occur
SERCA can’t function ‘
Describe some of the structural and functional differences between skeletal vs cardiac muscles, skeletal vs smooth muscles, and between cardiac vs smooth muscles
Smooth
Involuntary control
Spindle-shaped
Single, central nucleus
No tendons, T-tubules, myofibrils, or sarcomeres
NOT striated
Scattered thick filaments with many myosin heads
Thin filaments attached to dense bodies
Function
No neuromuscular junction. Instead, neurotransmitters are released into synaptic cleft from varicosities in axons that course through muscle
Ca2+ ions trigger contraction when released from SR and enter through voltage-gated calcium channels
Calcium binds to calmodulin (not troponin like in skeletal muscle), activates myosin light-chain kinase (MLCK)
Control of contractions
Multi-unit smooth muscle cells are innervated by a motor neuron
Visceral smooth muscle cells are interconnected
Mechanical stretch controls activity
Cardiac muscle
Ordered myofibrils like smooth muscle
Structural differences
smaller
Branched
Intercalated discs
Desmosomes
Gap-junctions
Conduction system and gap junctions rapidly propagate action potentials across entire myocardium, enabling heart to contract and relax as a single unit
Describe the various fuels used by muscles depending on the intensity and duration of physical activities
aerobic activity - carbs, fats, protein if on short supply of other fuels
Anaerobic - carbs
Rest - carbs and fat
Predict the type of activity and the substrate used to make ATP based on the RQ values (0.7, 0.8, 1)
0.7
Fats
RQ of 0.8
Either rest or protein
1
Carbs
Compare and contrast between the physiological relevance of fast, slow, and intermediate muscle fibers
Fast
Anaerobic
Easily fatigued
Large diameter
Slow
Darker color due to myoglobin (stores oxygen in muscles)
Fatigue resistant
Aerobic
Smaller diameter
Intermediate
3 mechanisms proposed to explain DOMS (also what’s DOMS)
DOMS - delayed-onset muscle soreness
Tears in the muscle tissue permits the loss of enzymes; myoglobin may stimulate nearby pain receptors
Muscle spasms
Connective tissue and tendon tears
Explain how muscle contractions are classified based on muscle length and the load
isotonic contraction
Concentric - muscle shortens
Eccentric - muscle lengthens
Isometric contraction - length doesn’t change
Speed of shortening is inversely proportional to the load
Describe the three ways in which the force generated by skeletal muscle can be regulated/fine-tuned
Recruitment of motor units
More force = more motor units recruited
Twitch summation
More action potentials in quick succession is more force (does eventually plateau - called tetanic contraction)
Force-length relationship
Describe action potentials in cardiac muscles
Stimulus
Rapid depolarization due to opening of Na+ channels and Na+ influx
Plateau due to slow Ca2+ influx balanced by K+ efflux
This is the refractory period
Repolarization due to rapid K+ efflux and closure of Ca2+ channels
Compare and contrast between the physiological relevance of force-length relationship in cardiac and skeletal muscles
cardiac muscle on ascending limb (change in sarcomere length causes greater change in force percentage)
Allows it to adjust force output to volume of blood in ventricle (Frank-Starling law)
Skeletal muscle on plateau region
Describe the blood flow through the various chambers of the heart, the cardiac valves, and cardiac blood vessels to the systemic and pulmonary circuit.
Right atrium
Coronary sinus receives deoxygenated blood from superior and inferior vena cava, empties into right atrium
Blood goes through tricuspid valve to right ventricle
Right ventricle
Discharges deoxygenated blood
Blood goes through pulmonary trunk to lungs
^ pulmonary circuit
\/ Systemic circuit
Left atrium
Receives oxygenated blood from pulmonary veins (one exception - veins usually carry deoxygenated blood)
Blood goes through bicuspid valve to left ventricle
Left ventricle
Discharges oxygenated blood
Oxygenated blood leaves through aorta to rest of the body
What happens when ventricles relax vs contract
relax
Right and left atrioventricular (AV) valves open but aortic and pulmonary valves close
Contract
Right and left AV valves close, aortic and pulmonary valves open
Describe the various components and the functioning of the cardiac conduction system
autorhythmic cells
Found in the nodes and in the internodal pathways
Produce action potential spontaneously
Smaller
Few contractile fibers
No organized sarcomeres
Hyperpolarization and Cyclic Nucleotide (HCN) channels
Generate “funny” pacemaker current (I sub f)
Activated by hyperpolarization and cAMP binding
Unstable resting potential; slow inflow of Na+ without compensating outflow of K+
Process
I sub f/HCN channels spontaneously depolarize cell to threshold
Voltage-gated Ca2+ channels open, Ca2+ flows into the cell
At peak, K+ channels open, K+ flows out to hyperpolarize the cell
Nodes
Sinoatrial (SA) node
Fired 75-100 action potentials/min
Atrioventricular (AV) node
50 impulses/min - delayed about 100 ms to allow for full contraction of atria
Right and left bundle branch
Fires 20-40 times/min
Explain how the various layers of the heart aid in its function
pericardium - membrane enclosing the heart, consisting of an outer fibrous layer and an inner double layer of serous membrane
Endocardium
Endothelium
Areolar tissue
Myocardium
Cardiac muscle cells
Connective tissues
Pericardial cavity
Visceral layer of serous pericardium
Mesothelium
Areolar tissue
parietal layer of serous pericardium
Dense fibrous layer
Areolar tissue
Mesothelium
Compare and contrast between the physiological relevance of autorhythmic and contractile cells in the heart
autorhythmic
Produce action potential spontaneously
Smaller
Few contractile fibers
No organized sarcomeres
HCN channels depolarize to threshold, then rapid depolarization occurs bc of voltage gated Ca2+ channels
Contractile
Na+ channels depolarize to threshold
Plateau phase due to Ca2+ influx balanced by K+ efflux
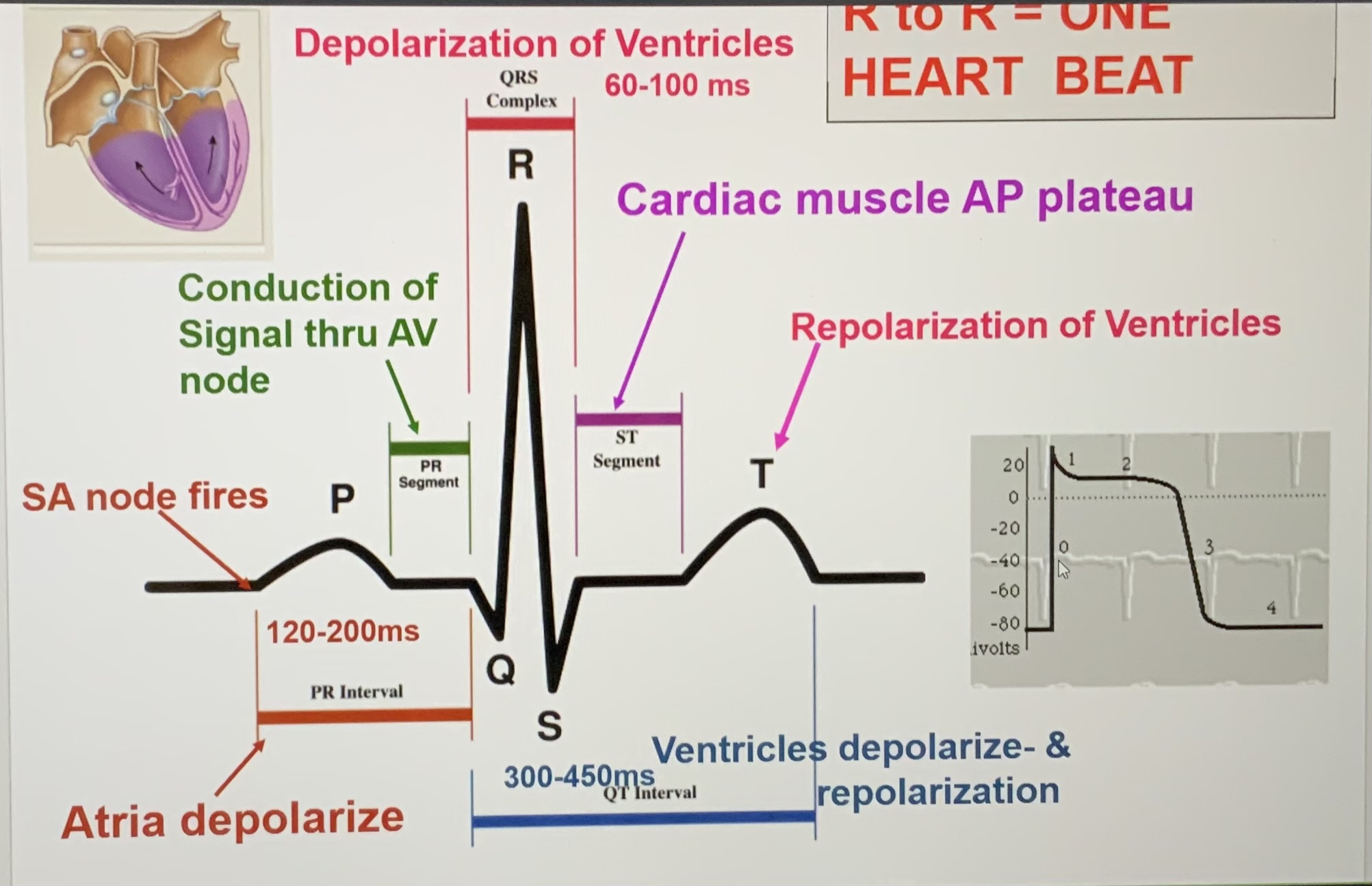
Explain how the various parts of the electrocardiogram (ECG/EKG) relate to the cardiac cycle
SA node fires
P wave
Atria depolarize/atrial contraction (atrial systole begins)
PR segment
Conduction of signal through AV node
QRS complex
Depolarization of ventricles
Q - isovolumetric contraction
R - ventricular contraction/first phase of ventricular systole
S - ventricular ejection/second phase of ventricular systole
ST segment
Cardiac muscle AP plateau
T wave
Repolarization of ventricles
Isovolumetric relaxation/early ventricular diastole
Right after T wave
Ventricular filling/late ventricular diastole
R to R is one heartbeat
Explain with examples how the electrocardiogram readings can indicate various pathologies of the heart
Bradychardia - slow heart rhythm
Tachycardia - fast heart rhythm
Heart block - interruption in the normal conduction pathway
First-degree AV block
Delay in conduction between SA and AV nodes
Second-degree
Only some impulses from SA node reach AV node (only P wave present occasionally)
Third-degree
No correlation between atrial and ventricular activity (P waves and QRS complex)
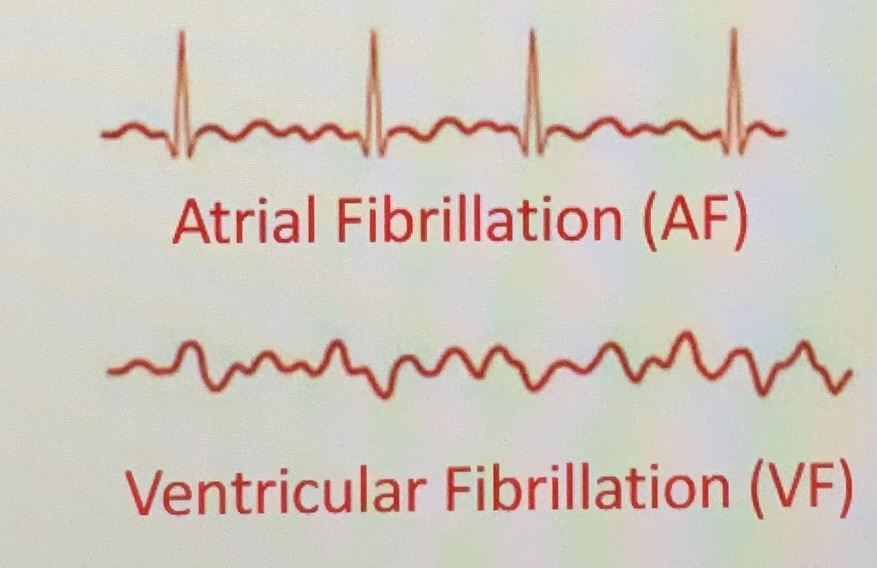
Fibrillation- rapid, irregular out-of-phase contractions; useless for pumping blood
Difference between a heart attack and cardiac arrest
heart attack
Clogged artery disrupts blood flow to your heart
Common cause of cardiac arrest
Cardiac arrest
Rapid, abnormal impulses override heart’s natural rhythm
Describe how the blood pressure and blood volume changes in the ventricles and atria during the cardiac cycle
ventricle diastole/atrial systole (P wave)
Atrial pressure slightly greater than ventricular
Ventricular volume rising until end-diastolic volume
After QRS complex
Aortic valve opens, left AV valve closes
Ventricular pressure much greater than atrial pressure but slightly less than aortic
Ventricular blood volume drops significantly, then stays the same for a period bc pressure lower than aortic pressure but higher than atrial
After T wave
Aortic valve closes, then left AV valve opens
Ventricular pressure drops. After left AV valve opens, pressure is less than atrial
Blood volume steadily rises
Explain how the cardiac cycle is represented using a pressure-volume loop
preload - stretch of myocardium or end-diastolic volume of the ventricles
After load - force or load against which the heart has to contract to eject the blood
Contractility - relative ability of the heart to eject a stroke volume (SV) at a given prevailing afterload (arterial pressure) and preload (end-diastolic volume; EDV)
Ejection fraction - percentage of EDV represented by stroke volume
Stroke volume (SV) = EDV - ESV
Slope constructed using the end systolic volume in the PV loop indicates contractility/inotropy
Predict how changes in heart rate and stroke volume can affect the cardiac output
CO = HR x SV
CO = HR x (EDV - ESV)
Explain how the autonomic nervous system regulates the increase and decrease of heart rate by impacting the action potentials of autorhythmic cells
To decrease HR, parasympathetic neurons release ACh which opens K+ channels. K+ leaves the cell, cell hyperpolarizes, thus slowing the rate of depolarization (slowing the heart rate)
To increase HR, sympathetic neurons release norepinephrine, which opens HCN channels, causes Na+ influx → rapid repolarization, which accelerates reaching threshold, thus increasing HR
Explain the relationship between pressure, flow, and resistance
Resistance has a direct relationship with blood viscosity
Resistance has a direct relationship with total blood vessel length
Resistance has an inverse relationship with vessel radius and cross-sectional area
Site of greatest resistance is arterioles
Describe the role of smooth muscles in blood vessels
regulate blood flow and maintain blood pressure by contracting and relaxing to change the vessel’s diameter
Explain how the progressive branching of blood vessels between the aorta and capillary beds influences the cross-sectional area of the vessels, rate of blood flow, resistance to blood flow, and the blood pressure in the vessels
Cross-sectional area least at elastic arteries and venae cavae
Vessel diameter greatest at elastic arteries and venae cavae, least at capillaries
Describe the various components of blood and their proportions
plasma (55%)
Water (92%)
Plasma proteins (7%)
Other solutes (1%)
Formed elements (45%)
Buffy coat
white blood cells and platelets (<0.1%)
Red blood cells (RBC)/erythrocytes (99.9%)
Describe the structural features and functions of red blood cells (RBCs), white blood cells (WBCs), and platelets
red blood cells (RBCs)
Biconcave discs
Large surface-area-to-volume ratio to quickly absorb and release oxygen
Small, highly specialized disks
Lack organelles
Short lifespan bc can’t synthesize proteins or repair damage
Form stacks called rouleaux that allow for smooth blood flow
White blood cells (WBCs)
Also called leukocytes
Have nuclei and other organelles
Lack hemoglobin
Most are in connective tissue proper and organs of lymphatic system
Small fraction circulates in the blood
Functions
Defend against pathogens
Attracted to specific chemical stimuli (positive chemotaxis)
Some phagocytic
Remove toxins and wastes
Attack abnormal or damaged cells
Different kinds of WBCs
Neutrophils
50-70% circulating WBCs
Multilobed nucleus
Pale cytoplasmic granules containing lysosomal enzymes and bactericidal compounds
Mobile, active, phagocytic
Eosinophils
2-4% circulating WBCs
Bi-lobed nucleus
Involved in allergic reactions and parasitic infections
Basophils
Less than 1% circulating WBCs
Enhance local inflammation by releasing
Histamine - dilates blood vessels
Heparin - prevents blood clotting
Monocytes
Spherical and large cells
2-8% circulating WBCs
Aggressive phagocytes - enter peripheral tissues to become macrophages
Lymphocytes
Thin cytoplasm around nucleus
20-40% circulating WBCs
Continuously migrate in and out of blood stream (found in lymphatic organs and connective tissues)
Part of body’s specific defense system
B cells complete development in bone marrow
T cells develop and mature in the thymus
Describe the steps involved in heme recycling, breakdown, and synthesis of red blood cells
synthesis
Macrophage secretes IL-3, which influences differentiation of a hematopoietic stem cell into a proerythrocyte
Pericytes (cells on blood vessels) release erythropoietin (EPO)
EPO binds to receptor on proerythrocyte
Proerythrocyte becomes a normoblast
Normoblast loses nucleus and organelles, becomes a reticulocyte
In bone marrow capillaries, reticulocyte matured into an erythrocyte (RBC)
breakdown
Red pulp of spleen has macrophages that inspect the glycoproteins on erythrocytes for oxidation
If oxidized, death by phagocytosis
Recycling
Old and damaged RBCs broken down into amino acids and heme
Heme converted into biliverdin then bilirubin
Bilirubin binds to albumin in bloodstream, taken to liver, excreted in bile
Hemoglobin that’s not phagocytized after hemolysis (rupture of RBCs in bloodstream) breaks down. Alpha and beta chains eliminated in urine
Predict how exogenous administration erythropoietin (EPO) can impact athletic performance
increases VO2 max
Increases time to exhaustion
Describe the structure and functions of hemoglobin
Hemoglobin
Protein that transports O2 and CO2
Heme - iron-containing pigment in each hemoglobin
O2 binds Fe
CO2 binds alpha and beta chains
Distinguish between the regulation of red blood cell and white blood cell production
RBC production largely regulated by hormone erythropoietin (EPO)
WBC production regulated by colony-stimulating factors (CSFs)
Multi-CSF
Granulocytes, monocytes, platelets, RBCs
GM-CSF
granulocytes and monocytes
M-CSF
Monocytes
G-CSF
Granulocytes
Describe the major functions of blood
transports dissolved gases, nutrients, hormones, and metabolic wastes
Regulated pH and ion composition of interstitial fluids
Restricts fluid losses at injury sites
Stabilizes body temp by redistributing heat generated by muscles
Defends against toxins and pathogens
Describe the functions of cytokines, CDs, PAMPs, and DAMPs with examples
cytokines
Secreted proteins that function as signaling molecules in an autocrine, paracrine, or endocrine fashion
Growth factors, interleukins, chemokines (induce chemotaxis)
Can cause cell motility (chemotaxis), differentiation, cell division, altered gene expression, etc.
CDs
Cluster of differentiation molecules
Surface molecules/markers expressed on blood cells which are used for cell-cell signaling and identifying cells
CD4 and CD8
PAMPs
Pathogen associated molecular patterns
Signal presence of pathogens to immune system
DAMPs
Damage associated with molecular patterns
Damage signaled by unusual molecules in the extracellular spaces
Describe the function of primary and secondary lymphoid tissues with a few examples
primary - sites where lymphocytes are formed and mature in the
Red bone marrow
Thymus
Primary lymphoid organ that atrophies after puberty
Regulates T cell lymphocyte development and maturation
T cells divide in the cortex, maturing migrate into medulla, matured leave by medullary blood vessels
Selection is done at thymi’s epithelial cells for:
Efficacy - ability to recognize proteins (positive selection)
Specificity - should not recognize self proteins (negative selection)
Secondary - where lymphocytes are activated
Tonsils
Mucosa associated lymphatic tissue (MALT)
Lymph nodes
Cortex contains follicles (collections of lymphocytes)
Naive B cells
Germinal centers - activated B cells are generating daughter cells (plasma cells, which release antibodies)
Medulla contains macrophages
Paracortex contains dendritic cells
Spleen
Red pulp - contains many red blood cells
White pulp - resembles lymph nodes
Functions
Filter blood to remove abnormal blood cells and other blood components by phagocytosis
Storage of iron recycled from RBCs
Initiate immune responses to antigens in blood by macrophages, B cells, T cells
Compare and contrast between innate and adaptive immunity by listing the various types of cells responsible for them
innate
Neutrophil
Eosinophil
Mast cell
Adaptive
T lymphocyte
Memory B cells
B lymphocyte
Plasma cell
What cells are most directly responsible for humoral branch of immunity
Plasma cells
Describe the various steps involved in innate immune response to a bacterial vs viral infections
bacterial
Bacteria damages dermis
PAMPs and DAMPs presented, activate mast cells
Mast cells degranutes to release histamines
Damaged cells secrete cytokines and chemokines
Cytokines dilate capillaries, heparin is anticoagulant
chemokines induce chemotaxis of neutrophils to damaged tissue
Chemotaxis of neutrophils triggers expression of selectin receptors on endothelial cells
Neutrophils bind to selectin receptors to enter damaged tissue via diapedesis
Neutrophils phagocytose bacterial and damaged cells until it explodes - contains free radicals, hydrogen peroxide, killing both healthy cells and bacteria
Chemokines recruit monocytes from bone marrow
Viral
Cell becomes infected with H1N1
Viral fragment displayed on MHC I, triggering death by cytotoxic/killer T cells
Interferons released, bind with receptors on nearby cells, trigger decrease in endocytosis, exocytosis, transcription, translation (triggers closing up) until viral infection no longer a threat
Steps of adaptive immune response for bacterial vs viral infections
bacterial
Macrophage presents antigen on MHC II
CD4 of naive T cell binds MHC
Antigen recognition - T cell receptor interacts with antigen
Co-stimulation - B7 from macrophage interacts with CD28 from T cell,
Proliferation/colonial expansion - IL2 released by T cell engages in autocrine signaling, becomes activated helper T cell that can recognize the antigen. Many copies form
B cell activation
Naive B cell presents antigen on MHC II
CD4 of naive T cell binds MHC
Antigen recognition
Co-stimulation - CD40 from B cell interacts with CD40L from T cell
Paracrine stimulation - T cell releases IL4, binds on B cell. Naive B cell becomes plasma B cell that produce antibodies that bind to pathogens and target them for phagocytosis
Viral
Macrophage presents antigen on MHC I
CD8 of naive T cell binds MHC I
Antigen recognition
Co-stimulation - B7 from macrophage interacts with CD28 from T cell
Proliferation/clinal expansion - IL2 released, autocrine signaling, becomes activated killer T cell that will kill cells that are infected
Explain the purpose of an interferon response to the viral infection of a cell
Alerts cells in the nearby vicinity to close up until virus is no longer a threat
List the four cardinal signs of inflammation and explain the factors that cause them
pain - nociceptors
Redness - histamine
Swelling - histamine
Heat - histamine
Explain how the innate inflammatory response leads to an adaptive immune response
Immune recruits monocytes, which become macrophages
Describe the various steps involved in activation of a T cell vs a B cell
both CD4, MHC II
B7 of macrophage is like CD40 on B cell
CD28 for macrophage from T cell is CD40L for B cell
T cell releases IL2 for autocrine signaling for activating T cell, releases IL4 for activating B cell
Explain how antibodies perform their function based on their structure
variable segments of light and heavy chains form antigen-binding sites
Heavy chain is site of binding to macrophages
Describe where T-cells mature and how they are activated
Thymus
Compare and contrast how CD4 and CD8 cells are related to MHCI and MHCII receptors, respectively
CD4 and MCHII interact to activate helper T cells
CD8 and MCHI interact to activate killer T cells