SECTION 04: LUNG VOLUMES
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
By the end of Section 04, you should be able to:
Describe the different lung volumes and why they are important.
Describe how lung volumes are affected in obstructive and restrictive lung diseases.
Using the formula for minute ventilation, make an argument as to whether it is better to increase frequency of breathing or tidal volume in order to increase ventilation.
Describe what is meant by the “work” of breathing
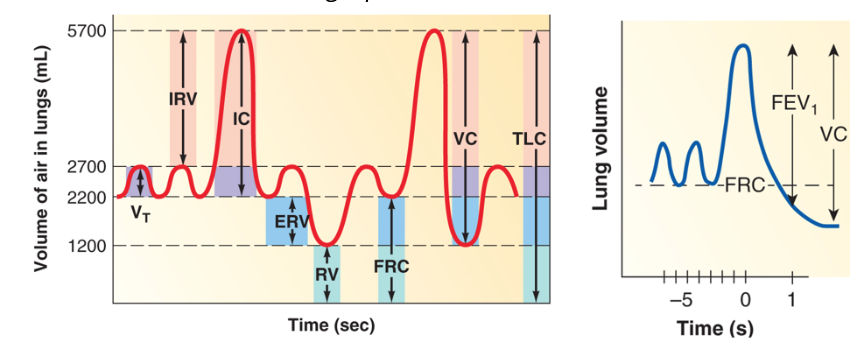
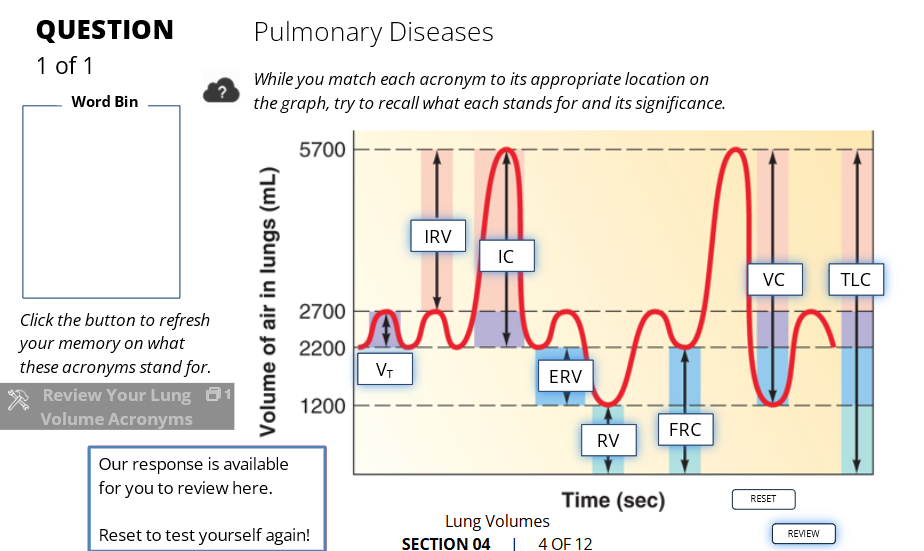
🫁 LUNG VOLUMES & CAPACITIES (Spirometry)
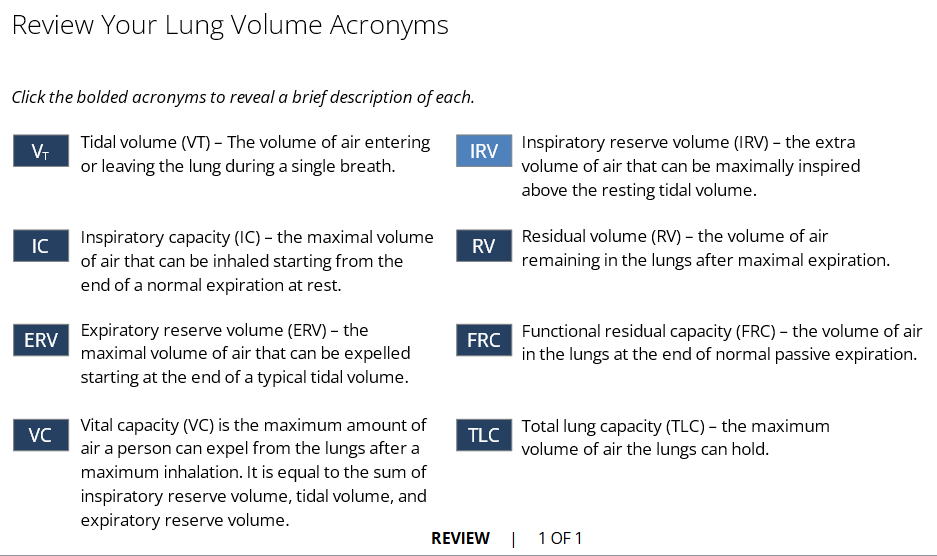
🔹 VT – Tidal Volume
💨 Normal breath in/out
~500 mL at rest
🟢 Everyday breathing
🔹 IRV – Inspiratory Reserve Volume
⬆ Extra air you can inhale after a normal breath in
~3000 mL
🟢 "Big inhale" on top of a normal breath
🔹 IC – Inspiratory Capacity
Total air you can inhale from a normal breath out
IC = VT + IRV = ~3500 mL
🟢 Breath in as much as possible after a normal exhale
🔹 ERV – Expiratory Reserve Volume
Extra air you can breathe out after a normal breath out
~1000 mL
🟠 Push out as much as you can after a normal exhale
🔹 RV – Residual Volume
Air that’s left in lungs after full exhale
~1200 mL
🔴 Can’t be measured by spirometry
🛑 Keeps lungs from collapsing
🔹 FRC – Functional Residual Capacity
Air left in lungs after normal breath out
FRC = ERV + RV = ~2200 mL
🟣 “Resting” air in lungs
🔹 VC – Vital Capacity
Max amount you can breathe out after a full breath in
VC = IRV + VT + ERV = ~4500 mL
🔵 Big breath in → big breath out
🔹 TLC – Total Lung Capacity
All the air lungs can hold
TLC = VC + RV = ~5700 mL
⚫ Total capacity
🔹 FEV₁ – Forced Expiratory Volume in 1 Second
How much air you can forcefully exhale in 1 second
Used to test lung function (esp. in asthma/COPD)
✅ Normally ~80% of VC
Graph summarizing the above
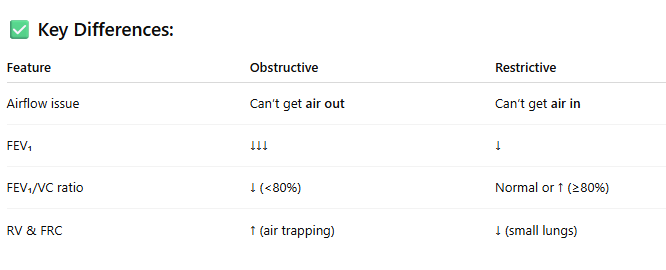
🫁 Obstructive vs. Restrictive Lung Disease
🟥 Obstructive Lung Disease
Examples: Asthma, COPD (Chronic Bronchitis, Emphysema)
🫁 Obstructive vs. Restrictive Lung Disease - 🔹 What’s Happening?
📉 Spirometry Results:
↓ FEV₁ (can't blow out much air in 1 sec)
↓ VC (Vital Capacity)
↑ RV & FRC (air gets trapped → hyperinflation)
↓ FEV₁ / VC ratio (< 80%)
❗ Common Symptoms:
Shortness of breath
Wheezing
Breath stacking
🟦 Restrictive Lung Disease
Examples: Pulmonary fibrosis, obesity-related lung restriction, scoliosis
🔹 What’s Happening?
Lungs are stiff or small
Hard to get air in
📉 Spirometry Results:
↓ FEV₁ (less air overall)
↓ VC
↓ RV & FRC (lungs hold less air overall)
**FEV₁ / VC ratio is normal or high (≥ 80%)
❗ Common Symptoms:
Shallow breathing
Feeling like you can’t take a deep breath
✅ Key Differences:
Master and understand this labelling
Review terms
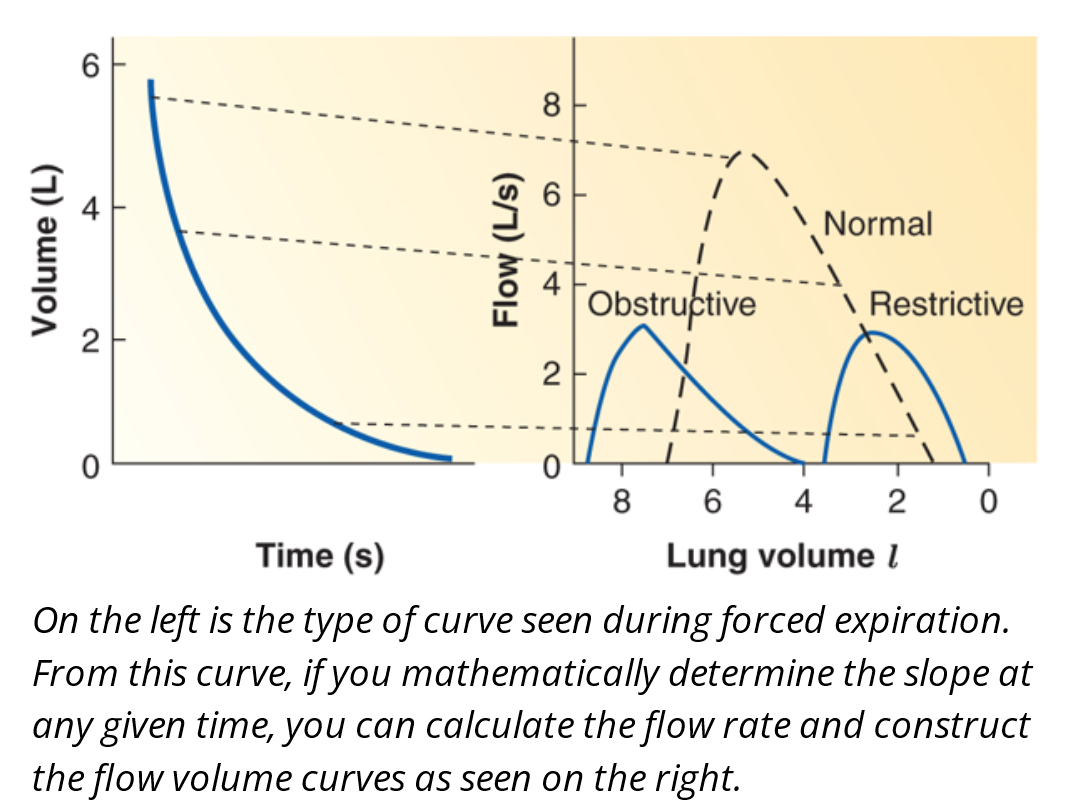
🫁 Using Expiratory Flow to Assess Lung Function
📈 What’s Measured?
We analyze forced expiration — breathing out as fast and fully as possible — to see how the lungs perform.
🔹 Why Use Expiration (Not Inhalation)?
🧪 Try this:
Inhale fast: Takes <0.5 sec
Exhale fully: Takes ~5 sec
➡ Expiration is harder → better reveals lung limitations
📉 How It’s Measured:
Patient exhales forcefully
Curve on left shows volume over time
Slope = flow rate
This data builds flow-volume curves (right graph)
🟢 Normal Curve
Starts at full lung (TLC)
High peak flow (~7 L/s)
Linear drop in flow with decreasing volume
Ends at residual volume
🔴 Obstructive Disease Curve
Starts at higher lung volume (due to air trapping)
Lower peak flow
Scooped or "caved-in" shape
Ends at higher residual volume
➡ Example: Asthma, COPD
🔵 Restrictive Disease Curve
Starts at lower lung volume
Lower peak flow (but sharp curve)
Ends at lower residual volume
➡ Example: Pulmonary fibrosis
💡 Key Takeaway:
Forced expiration reveals more about lung function than inspiration
➡ It’s where limitations appear most clearly
🌬 VENTILATION & DEAD SPACE
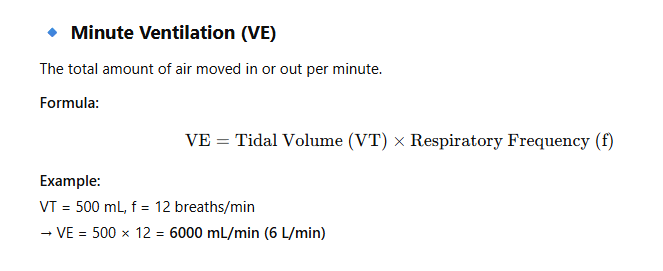
🔹 Minute Ventilation (VE)
🧠 But Not All Air is Useful for Gas Exchange!
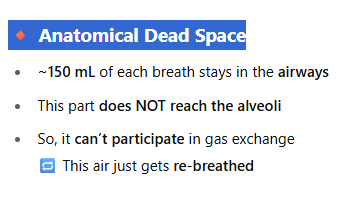
🔸 Anatomical Dead Space
📊 Gas Exchange Breakdown (Per Breath):
500 mL total inhaled (VT)
150 mL → stays in airways = dead space
350 mL → reaches alveoli = effective for gas exchange
🔁 Exhalation Works the Same:
First 150 mL of air you breathe out = from the airways (not alveoli)
So, 150 mL of fresh oxygen-rich air from the last breath never reached the alveoli at all
💡 Key Takeaway:
Even if your minute ventilation is normal, the actual gas exchange is lower
→ You need to account for anatomical dead space (150 mL)
🫁 VENTILATION: What Improves Gas Exchange?
🔹 Key Question:
Is it better to breathe faster or deeper to get more oxygen into your blood?
📊 Minute Ventilation Formula:
🛑 The Problem: Dead Space (150 mL)
Every breath: first 150 mL of air = wasted (just fills airways, doesn’t reach alveoli)
If VT = 150 mL, then alveolar ventilation = 0
🔁 Compare the Two Options:
➤ Breathing Faster (↑ f):
Many small breaths
More total air moved — BUT most of it gets trapped in dead space
→ Poor alveolar ventilation
➤ Breathing Deeper (↑ VT):
Fewer, larger breaths
More air goes beyond dead space
→ Better gas exchange
✅ Best Strategy:
✅ Best Strategy:
Slow, deep breathing
→ Maximizes alveolar ventilation
→ More oxygen in, more CO₂ out
🧠 Takeaway:
To improve gas exchange, it's better to increase tidal volume, not just breathing rate.
🫁 Alveolar Ventilation (V̇A)
📘 Key Concept:
Dead space (VD) = ~0.15 L (150 mL) → doesn’t participate in gas exchange
Effective breathing = VT > VD
Alveolar Ventilation (V̇A) = the air actually reaching alveoli per minute
📊 Formula Review:
Minute Ventilation (V̇E) = VT × f
Alveolar Ventilation (V̇A) = (VT - VD) × f
V̇A/V̇E = % of total ventilation used for gas exchange
→ Higher = more efficient breathing
🛌 At Rest Examples (All V̇E = 6 L/min)
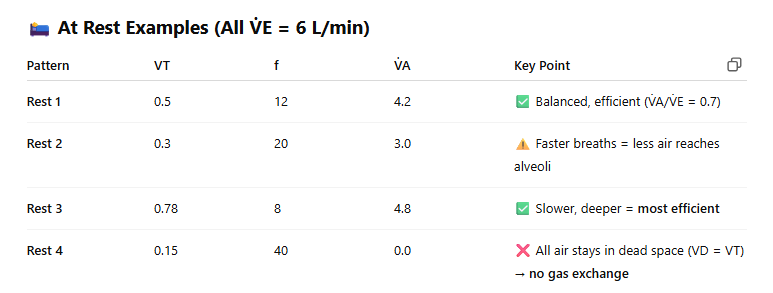
🏃♂ During Exercise
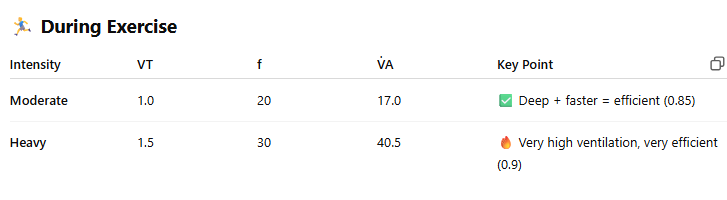
✅ Main Takeaways
Deep > Fast for gas exchange
Best efficiency = when VD/VT is low
Breathing too shallow and fast → wastes air in dead space
Exercise increases both depth and rate → improves gas exchange
💨 Work of Breathing
🧠 Definition:
Work of Breathing = Energy your body uses to move air in and out of your lungs
🛑 Normal breathing uses < 3% of total body energy at rest
📈 Two Types of Work:
Elastic Work
Effort to stretch the lung and chest wall
⬆ When tidal volume is high (deep breaths)
Flow-Resistive Work
Effort to overcome airway resistance
⬆ When breathing frequency is high (fast breaths)
📊 Graph Breakdown:
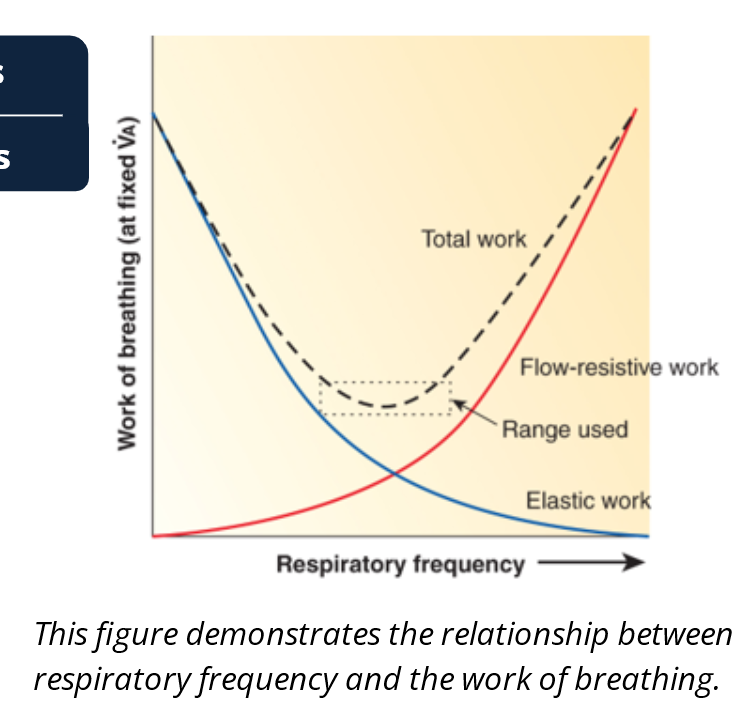
X-axis = Respiratory Frequency (breaths/min)
Y-axis = Work of Breathing
🔵 Elastic work = Higher at low frequencies
🔴 Flow-resistive work = Higher at high frequencies
⚫ Total work = U-shaped curve
✅ Minimum total work occurs at moderate frequency
→ That’s the optimal breathing rate your body naturally uses at rest
⚖ What Happens at Extremes?
Low frequency → deep breaths = ↑ elastic work
High frequency → shallow, fast breaths = ↑ flow resistance
🟢 Best strategy = balance both for efficient breathing
🫁 Work of Breathing: COPD vs. Exercise
🔴 COPD (Chronic Obstructive Pulmonary Disease)
🚫 What Happens:
Airways are narrowed → ↑ flow-resistive work
Breathing out becomes hard and slow
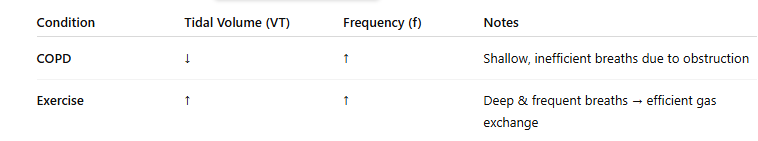
📉 Tidal Volume (VT): ↓ (lower, because lungs are already full—air trapping) 📈 Respiratory Frequency (f): ↑ (faster, shallow breaths)
⚠ Problem: More shallow breaths = more dead space = less gas exchange efficiency
🏃♂ During Exercise
💪 What Happens:
Body needs more oxygen and must remove more CO₂
📈 Tidal Volume (VT): ↑ (deeper breaths) 📈 Respiratory Frequency (f): ↑ (more breaths per minute)
✅ Strategy: Take deep and faster breaths → improves alveolar ventilation
→ Flow-resistive + elastic work both increase, but this is tolerated short-term
🧠 Summary Chart:
🫁 Factors That Increase the Work of Breathing (
🔹 2. ↑ Airway Resistance
Airways are narrowed or blocked
Example: COPD, asthma
❗ Effect:
↑ Flow-resistive work
↓ Breathing Rate (f)
VT stays roughly the same
➡ Takes longer to breathe out
🔹 3. ↓ Elastic Recoil
Lungs don’t spring back easily
Example: Emphysema (damaged alveoli)
❗ Effect:
Expiration needs muscle effort
↓ Breathing Rate (f)
VT stays the same
➡ Air gets trapped → harder to exhale
🔹 4. ↑ Demand for Ventilation
Body needs more oxygen
Example: Exercise
❗ Effect:
↑ Tidal Volume (VT)
↑ Breathing Rate (f)
➡ More work but beneficial
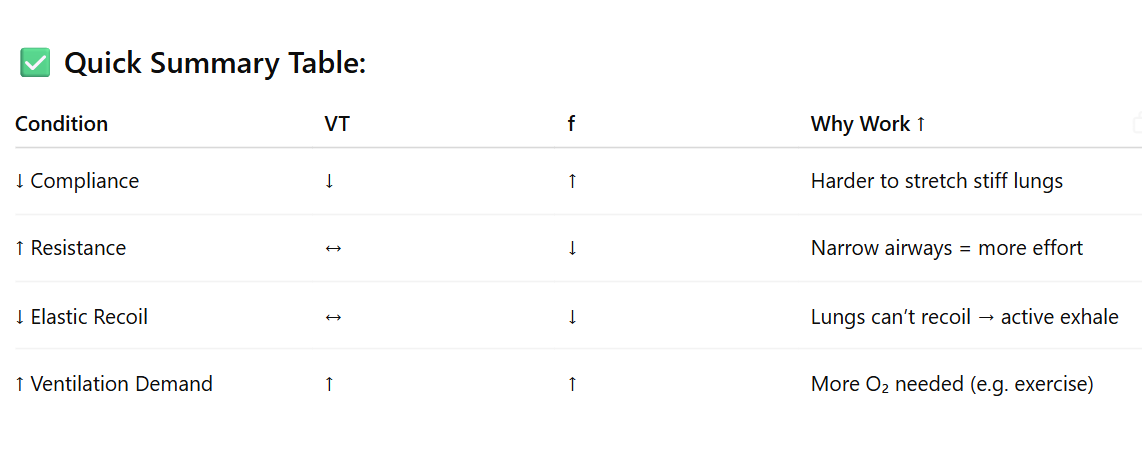
✅ Quick Summary Table: