L2 Haemoglobin, related disorders
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
characteristics of erythrocyte
simple - no nucleus, ribosomes, mitochondria
unattractive to infecting organisms
no protection
no capacity for mRNA or new protein translation
limited reducing power or capacity to generate ATP so vulnerable to damage
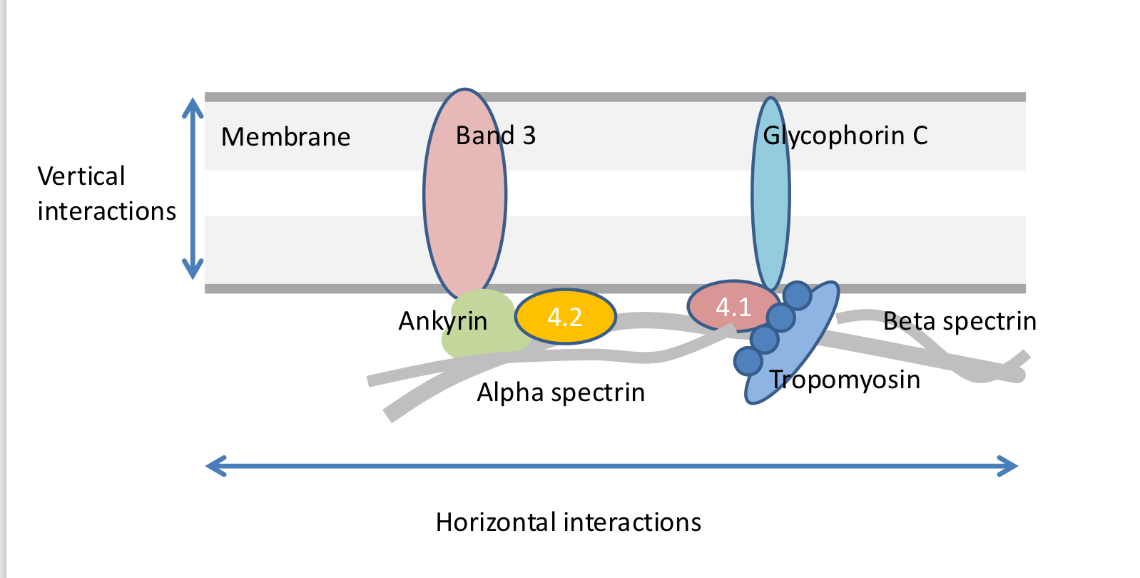
what forms the membrane skeleton and the horizontal lattice of the cytoskeleton
spectrin
ankyrin
protein 4.2
actin
what is the most abundant protein found within the erythrocyte membrane
spectrin
local damage
fibrin strands in circulation caused by local clotting activation
slicing damage
vacuole pops but red cell is sealed
cytoskeleton structure allows self repair
diffuse damage
inherited abnormal cytoskeleton or heat, toxins, antibodies may cause diffuse membrane loss
small sealed blebs of membrane are lost
cell shrinks becoming rigid sphere
spherocyte formed and removed by spleen
inherited abnormal cytoskeleton
loss of anchoring proteins in membrane
hereditary spherocytosis - defect of red cell membran edprotein such as ankyrin or band 3
what leads to spleen enlargement
red cell membrane is unstable, lost
spherocytes formed (diffuse damage)
rapid breakdown of RBC cause anaemia (<30 days turnover)
breakdown products of RBC leads to mild jaundice and gall stones, inc bile
inc rbc destruction leads to spleen being enlarged
seen in sickle cell, thalassaemia, leukaemia, lymphoma
haemoglobin in circulation
through diffuse damage
highly toxic
cytoskeleton repair helps to prevent this leakage
porphyrin structure
holds iron in flat 2D structure
2 interaction sites above and below the plane
one fix molecule to globin
one for oxygen
interconnection of chains of haemoglobin
after release of first oxygen structure becomes tighter
more likely to release another oxygen as tight formation has less room
what else influences tight or loose conformation of haemoglobin
pH
CO2
metabolic products
why does foetal haemoglobin have higher affinity for oxyegn
doe snot bind to 2,3 DPG
G6PD glucose 6-phosphate dehydrogenase
red cell enzyme that generates reducing power NADPH that protects haemoglobin from oxidative damage
G6PD deficiency
oxidative stress is high, Hb is damaged, RBC destroyed
oxidative lysis
prevalent gene in Africa, Arab states
cause death after some medicines which inc oxidation and cause chronic anaemia
how does G6PD deficiency lead to anaemia
pentose phosphate cannot function
reducing power NADPH is not generated
H is damaged
shrinks to one cell in denatured form
anaemia
how is G6PD deficiency an advantage
cells infected by malaria are inhospitable
less available for the parasite to be consumed