SEHS A.1.3: Transport
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
cardiorespiratory system
-cardiovascular system+respiratory system (known as circulatory system)
-system working in highly coordinated manner to increase oxygen delivery during exercise
- part of body continuously trying to maintain constant internal environment (homeostasis)
main components of cardiovascular system
-heart
-blood
-vessels: arteries, veins, capillaries
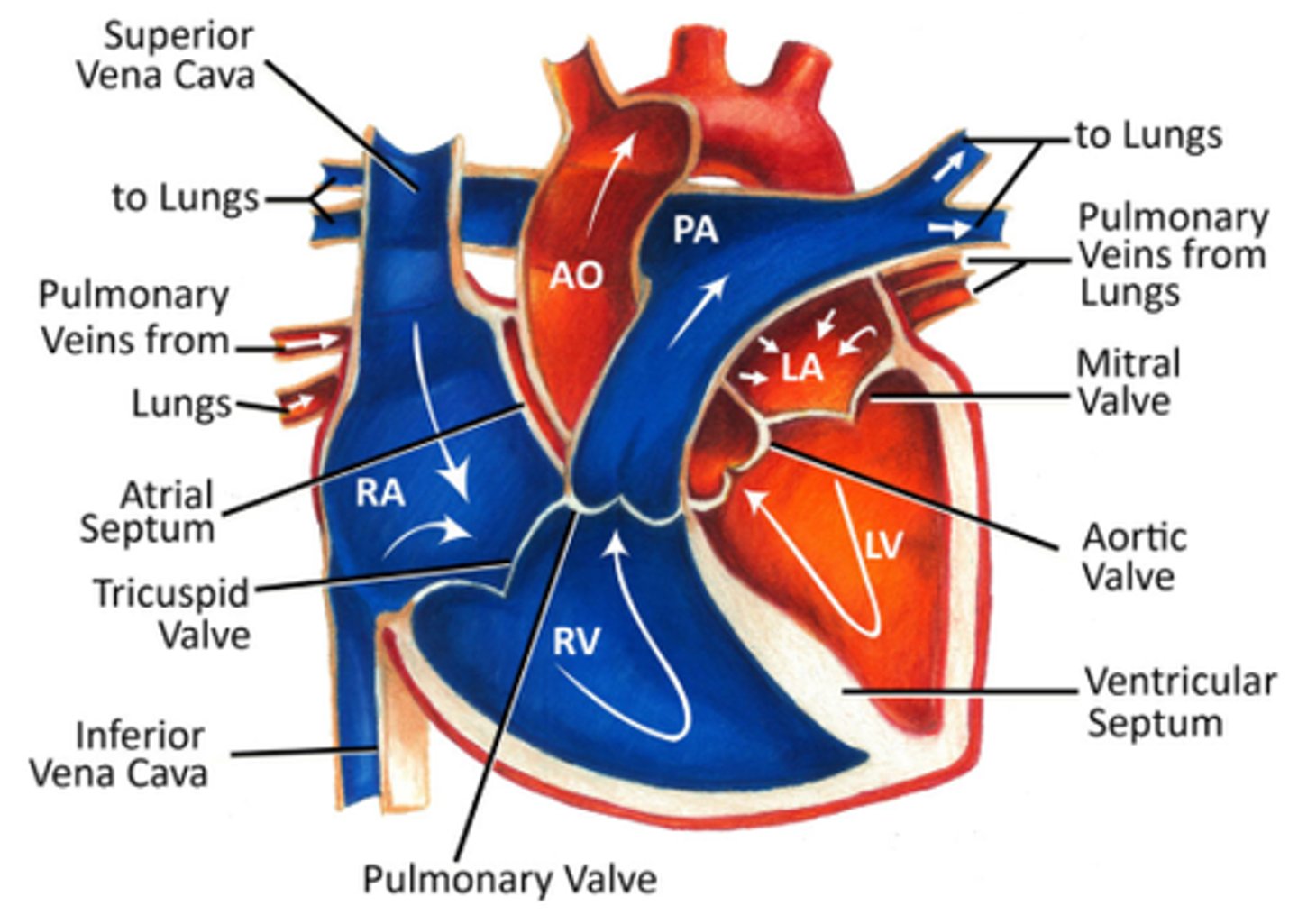
blood pathway to get oxygenated
inferior vena cava
right atrium
tricuspid valve
right ventricle
pulmonary valve
pulmonary artery
lungs
blood pathway (After being oxygenated)
lungs
pulmonary vein
left atrium
mitral valve (bicuspid valve)
left ventricle
aortic valve
aorta
what are the composition of bloods and their functions
- plasma: takes nutrients, hormones, and proteins to the parts of the body that needs it, removes cell wastes (transportation)
- platelets (thrombocytes): blood clotting (coagulation: repair function)
- leukocytes (WBC): defends against pathogens (immune function)
- erythrocytes (RBC): transports oxygen and CO2 ( gas transport)
arteries
- relatively large in diameter, thick muscular wall, transports high-pressure oxygenated blood away from heart to tissue, branch into narrower arterioles
capillaries
- narrow vessels (thin walls), forms extensive branching network, siles of exchange between blood and tissue
veins
-branche into venules, flexible than arteries, contains valves to prevent back flow, transport from body TO heart
what is the cardiac cycle process
events occurs during a complete heartbeat
- atriole systole begins ( atrial contract forces blood to ventricles)
- ventricular systole (1st phase): ventricular contraction pushes AV valves closed
- ventricular systole (2nd): semilunar valves open and blood is ejected
- ventricular diastole (early): semilunar valves closed and blood flows into atria
- ventricular diastole (late): chambers relax & blood fills ventricles passively
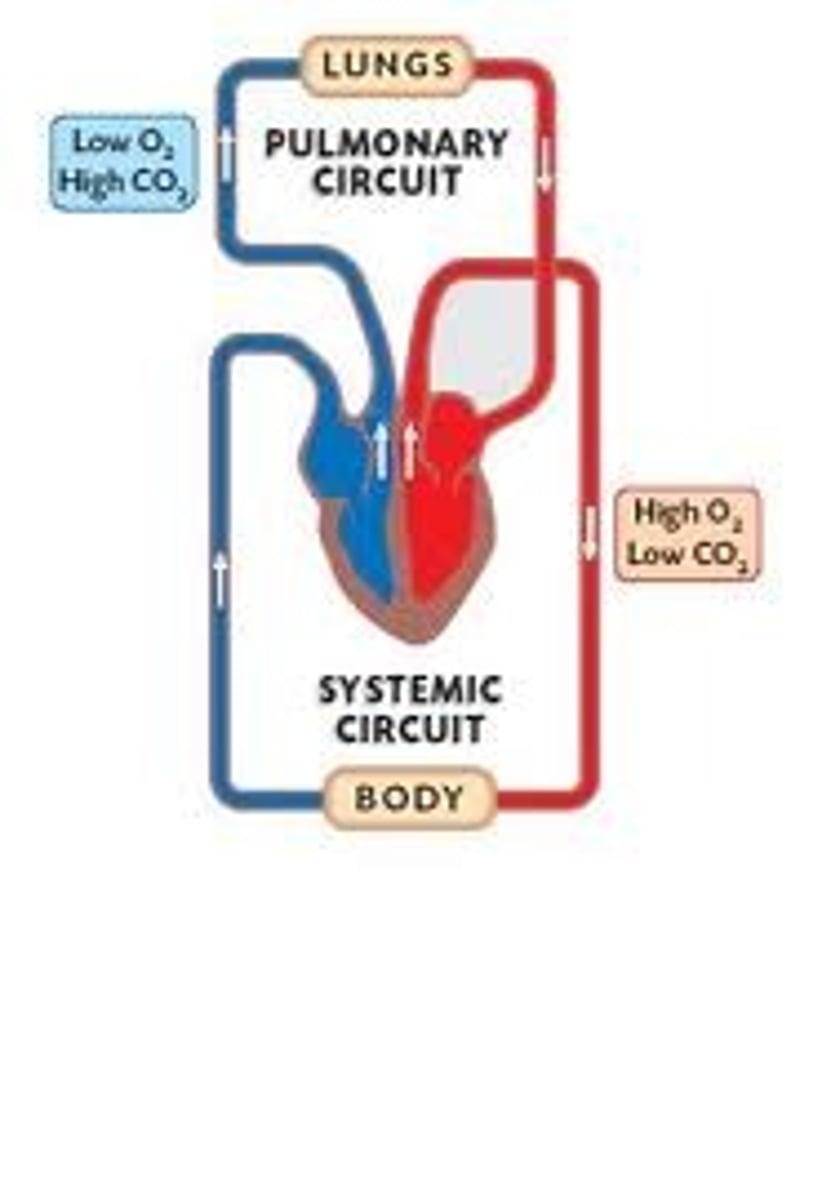
what is the pulmonary circulation and its process
heart and lungs
- blood flows to lungs (from heart)
- from right ventricle to lungs
- from lungs to left atrium
- blood leaving heart is low in oxygen (deoxygenated)
-blood that returns to heart is high in oxygen
what is the systemic circulation and its process
heart and body
- blood flows to body (from heart)
- from left ventricle (through aorta) to organs of body
- from body to right atrium
- blood leaves heart is high in oxygen (oxygenated)
- blood that returns to heart is low in oxygen
diastolic blood pressure
force exerted by blood on arterial walls during ventricular relaxation
- pressure blood exerts within arteries between heartbeats
- normal dias. is 80mmHg or below
- fills with blood
systolic blood pressure
- force exerted by blood on arterial walls during ventricular contraction
- pressure exerted when blood is injected into arteries (squeezing and pushing blood throughout body)
- normal sys is 120 mmHg or below
- indicator of heart attacks/strokes
-high sys. indicates increased risk for cardiovascualr
what is blood pressure
measurement of force of blood against artery walls as heart pumps it throughout the body
- categorized into several stages (low BP to hypertensive crisis w/ specific systolic and diastolic ranges defining each category
- expressed as systolic and diastolic
- High BP can weaken heart and blood vessels (increase risk of heart attack/stroke)
is systolic and diastolic blood pressure higher in dynamic or static exercises?
- sbp increases significantly during dynamic exercises bc heart pumps harder to deliver more oxygenated blood to working muscles
- diastolic pressure usually stays the same or slightly drops
- sbp increases more during static holds due to intense muscle tension and restricted blood flow in static efforts, therefore static exercises imposes greater pressure load
difference between dynamic and static exercise
dynamic: continuous movement thru range of motion to warm muscles for activitiy (ex: bicep curls, lunges), improves power + blood flow
static: holding fixed position to build strength, stability, used for recovery (ex: plank)
responsibility of cardiovascular system
deliver continuous supply of oxygen and nutrients to active muscles, maintaining high level of energy transfer while removing metaboiltes (chemical reactions break own food, drugs to remove waste)
cardiac output
volume of blood pumped by heart in one minute
CO= stroke volume x heart rate
stroke volume
volume of blood pumped from left vent5ricle per beat
- expands and HR increases during exercise
cardiovascular drift
upward drift of HR over time + progressive decline in SV + continued maintenance of CO
- Occurs while exercise intensity remains constant
- characterized by increase in HR and decrease in arterial pressure and st5roke volume
- connected to an increase in core temperature and body water losses
- body responds by increasing skin blood flow to control temperature, creates competition for blood between muscles and skin (thermoregulation)
- proper hydration and pacing strategies can help minimize its impact on performance
blood flow during rest
- blood distributed to working internal organs
- blood distributed to peripherals decreases bc of vasoconstriction
- blood redirected to organs
flows quite evenly to brain, liver & gut, kidneys, skeletal muscle
blood flow during exercise
- blood distributed to working muscles
- blood moves to working muscles bc:
of vasodilation
need of oxygen + nutrients increases
need for waste and heat removal increases
flows to skeletal muscles the most
respiratory system
- enables transport and exchange of oxygen for use in cellular respiration
- basis of movement by breathing: substance flows from an area of higher pressure to an area of lower pressure
- action of breathing is involuntary process, but can be controlled by choice to an extent
principle structures of respiratory system (smooth muscle tissues)
- nose
- mouth
- pharynx
- larynx (voice box)
- trache (windpipe)
- lungs
- bronchi
- bronchioles
- alveoli
ventilation
process of breathing
inhalation and exhalation
inhalation: process of air moving into lungs (inspiration)
exhalation: process of air moving out of lungs (expiration)
air pressure in ventilation
- movement of air in and out of lungs is result in change of pressure
- for air to enter lungs, pressure inside lungs must be lower than in atmosphere
- change of pressure caused by change in thorax volume
process of inhalation
- external intercostal muscles contract, forces rib cage up and out
- diaphragm contracts, moving itself down (flatter)
- increase in thorax volume, results in drop in pressure inside thorax
- lungs have space to expand
- air moves from place with more partial pressure (outside) to place with less partial pressure (inside lungs)
- air flows into lungs from outside the body through conducting airways
- air continues to enter lungs until pressure inside lungs rises to atmospheric pressure
exhalation process
- internal intercostal muscles contract, forces rib cage down and in
- diaphragm relaxes and abdominal muscle contract, moves diaphragm up
- decrease in thorax volume, results in rise in pressure inside thorax
- lungs compressed
- air move from place with more partial pressure ( inside lungs) to place with less pp (outside)
- air flows out of lungs to outside of body thru nose/mouth
- air continues to flow out of lungs until pressure in lungs fall back to atmospheric pressure
pulmonary ventilation
inflow & outflow of air between atmosphere and lungs (breathing)
total lung capacity (TLC)
volume of air in lungs after maximum inhalation
- sum of vital capacity and residual volume
vital capacity (VC)
maximum volume of air that can be exhaled after maximum inhalation
tidal volume
volume of air breathed in and out in one breath
expiratory reserve volume
volume of air in excess of tidal volume that can be exhaled forcefully
inspiratory reserve volume
additional inspired air over and above tidal volume
residual volume
volume of air still contained in lungs after maximal exhalation
influential factors to ventilatory
- age
- fitness
- activity
- gender
- body size
what is the function of blood
- transports electrolytes, proteins, gases, nutrients, waste products & hormones
- protects from disease, prevents bleeding, helps regulate temperature, water content and pH
what is blood
- 8% of our body weight
- healthy males: 5-6 litres, females: 4-5 litres
- color of blood depends on amount of oxygen it's carrying
- oxygen-poor : dark red color
- oxygen rich: scarlet red
- consists of plasma (55%) and other elements (45%): RBC, WBC and platelets
- density of blood crucial for its function in transporting nutrients, gases and waste products
- circulates thru complex network of vessels driven by heart & regulated by valves and capillaries (ensure oxygen delivery& waste removal= essential for healthy body function)
valves
the 4 one way gates in heart
- valves in veins ensure blood flows in correct direction, prevent backflow and maintain efficient circulation
- open/close by force in response to coordinated sequences of muscle contractions
- papillary muscle and interventricular septum are crucial for valve function and chamber separation
what is erythrocytes and its function
- RBC
- carries oxygen + contains haemoglobin (gives blood red color)
- lives for 120 days, replaced at rate of 2 million per second
- essential for transporting oxygen from lungs to tissues and removes CO2
- biconcave shape increases surface area for gas exchange
what is leukocytes and its function
- WBC
- combat infection and inflammation ( by ingesting foreign microbes thru process called phagocytosis)
- critical role in immune system response to pathogens
- ex: neutrophils, lynphocytes, monocytes w/ own specialized functions
what is platelets and its functions
- thrombocytes
- clot and help repair slightly damaged blood vessels
- contains proteins and antibodies produced by immune system to fight diseases
- aggregate at vessel injury to form plugs and prevent blood loss
- release chemical signals which promote healing and tissue repair
what is the upper chambers and its function
- atria
- receives incoming blood
what is the lower chambers and its functions
- ventricles
- pumps blood out of heart
- heart valves act as gates at chamber openings to ensure one-way blood flow
what are the 4 types of valves and its functions
1. tricuspid valve
- closes off upper right chamber (atrium) that holds blood coming in from body
- opens to allow blood to flow from top right chamber to lower right chamber (right atrium to right ventricle)
2. pulmonary valve
- closes off lower right chamber (right ventricle)
- opens to allow blood to be pumped from heart to lungs (via pulmonary artery) to receive oxygen
3. bicuspid (mitral) valve
- closes off upper left chamber (left atrium) to collect oxygen-rich blood from lungs
- opens to allow blood to pass from upper left side to lower left side (left atrium to left ventricle)
4. aortic valve
- closes off lower left chamber that holds oxygen-rich blood before pumped out to body
- opens to allow blood to leave heart (from left ventricle to aorta to body)
what are 3 muscle layers form the 3 main layers of the heart wall
- epicardium
- myocardium
- endocardium
atrioventricular valves
- dense connective structures to prevent backflow of blood into chambers
- 2 types: tricuspid (right) bicuspid (left)
- open and shut as heart contracts and relaxes
- proper functioning ensures blood flows in 1 direction (atria to ventricles)
semilunuar valves and coronary arteries
- both arteries from heart have semilunar valve (prevent backflow)
-pulmonary and aortic semilunar valve are key
- heart has own blood supply via coronary arteries
- ensures blood exits heart efficiently and doesn't return to ventricles
heart regulation and excitation sequence
- doesn't require nerve stimulation to contract
- contract on own via pacemakers (specialized cells): sinotrial node (SA node) and atrioventricular node (AV node)
what is the SA node (full name + function)
sinoatrial node
- found on wall of right atrium
- coordinates heart contractions and acts as primary pacemaker
- generates nerve impulses causing atria to contract, regulated by autonomic nerves to speed up/slow down HR
what is the AV node (full name + function)
atrioventricular node
- located in middle of 2 ventricles and 2 atria
- sends impulses down atrioventricular bundle to ventricles
- signal delay and safety
- delays impulses for about 0.1 seconds (allows atria to empty before ventricles contract), prevent rapid and irregular atrial beats
parasympathetic regulation
- innervation originates in centers in medulla, passe to heart thru way of vague nerves
- Vague nerve fibers innervate SA and AV nodes
- when stimulated: release acetylcholine, shlows heart
- slow of heart: bradycardia (>60 bpm), supports rest and digest
sympathetic regulation
- sympathetic nerves stimulate release of norepinephrine and adrenaline
- increases HR and strength of ventricular contraction
- speeding of HR: tachycardia (<100 bpm), supports fight or flight
resting cardiovascular function
- cardiac output at rest (5 liters per minute)
- SV and HR lower at rest
- resting HR (60-80 bpm)
- well trained athletes have lower resting HR (bc greater cardiac efficiency)
- differences in resting values influenced by genetics, age and fitness level
cardiovascular changes during maximal exercise
- Cardiac output can increase 20-30 liters per min during maximal exercise
- SV and HR rise during exercise to meet increased oxygen demand
- Hr can reach <200 bpm at maximal effort
- maximal cardiac output due to differences in body size and endurance training
- endurance training can enhance maximal SV and CO
what is pulse pressure
numeric difference between systolic and diastolic bp
ex: resting bp is 120/80 mmHg, pulse pressure = 40mmHg
- <60 good indicator of heart attacks and cardiovascular diseases (especially for men)
what does a low and high pulse pressure mean
- low= poor heart function
- high= leaky heart valves or arterial stiffness (usually in older adults)
fill in the blank
stiffness of aorta is most important cause of...
elevated pulse pressure
additionaly: or fatty deposits (atherosclerosis), leaves arteries less elastic
what does bp response depend on?
- type of exercise
- muscle mass used
- static vs dynamic exercise
- individual health
- greater intensity of exercise, greater rise in HR and SBP
dynamic exercise (isotonic) response of bp to various exercise modalities and recovery
- increases systolic pressure in first few mins then levels off
- diastolic pressure remains relatively unchanged
static exercise (isometric) response of bp to various exercise modalities and recovery
- can increase bp dramatically
- muscular force/contraction compresses peripheral arteries (increase resistance to blood flow)
upper body exercise response of bp to various exercise modalities and recovery
- exercise at given % of VO2 max increases bp substantially more w/ upper body than lower body
recovery response of bp to various exercise modalities and recovery
after a period of light to moderate exercise, SBP decreases below pre exercise levels for up to 12 hours in normal and hypertensive subjects
effects of incremental exercise on bp and blood flow distribution
- as exercise start and cardiac output increases, blood flow shifted from organs of body (ex: liver and kidneys) to working muscles
- person w/ normal sbp of 120 can see SBP increase to <180 or higher during instense aerobic activity
- may take 10-20 mins for SBP to return to resting levels after exercise
- diastolic bp remains relatively unchanged (indicates efficient vascular adaptation)
bp response to aerobic resistance exercise
- raises bp but response is less dramatic than with heavy resistance training
bp response to heavy resistance exercise
- strength and hypertrophy training with heavy loads are among few training types that dramatically raise bp
- heavy load increase strain on skeletal muscles (makes heart work harder to push blood into contracted muscles)
- recovery takes 20-40 mins
lifestyle changes for lower BP
1. regular physical activity
2. focus on nutrition
- cut salt
- take meds
- check bp regularly
- lose weight
- cut alcohol/dont smoke
- de-stress and sleep well
effects of prolonged standing
cause significant health risks (loss of blood volume from circulation and increased long term circulatory issues)
- pressure increases in capillaries (veins aren't accepting blood from them bc they are dammed up w/ their own)
- some plasma lost to interstitial fluid
- after short time around 20% of blood volume lost from circulation this way
- arterial bp falls and blood supply to brain diminished= fainting
- increases risk of carotid atheroscierosis (due to additional load on circulatory system)
- increase risk for varicose veins
blood distribution at rest vs during exercise
rest:
- distributed more evenly throughout body to support all organs and tissues
exercise:
- nervous system prepares body by secreting hormones to signal dilation of blood vessels in heart and working muscles
- more blood directed to working muscles
- more training= systems act faster and more efficiently to redistribute blood during workout
- stopping/starting abruptly= slow effects and cause blood to pool in working muscles from sudden reduction of muscle contractions (pooling makes u dizzy since blood takes time to return to heart)
- no. of capillaries in muscles increase w/ training, improve blood flow distribution
- blood becomes thinner bc increase plasma volume and dissolved proteins= flow better
RBC slightly ..... with training
increases
cardiovascular adaptations reulted from endurance exercise training
- during prolonged exercise cardiac output maintained at same level for trained and untrained at fixed intensity
- lower hr in trained is bc of increased stroke volume and heart efficiency
- capillarization increases w/ training= greater oxygen delivery and efficient removal of CO2
- increased capillary density and mitochondrial work capacity improves ocygen utilization in muscles
- decrease in exercising hr is due to aerobic trraining and increase in stroke volume
physiological adaptations to endurance training
cardiac adaptations
- increased left ventricle dilation and chamber volume
- increase cardiac muscle mass & stroke volume
muscular changes
- increase mitochondria, oxidative enzyme efficiency and slow twitch msucle fibers expression
metabolic efficiency
- greater carbohydrate sparing
- increased disposal of metabolic waste & fat oxidation
oxygen utilization
-faster diffusion rates of oxygen & fuel to muscles
- improve cell regulation of metabolism
what is VO2 max and what is it based on
maximal oxygen consumption, key measure of aerobic endurance and cardiovascular fitness
- based on factors like: training status, sex (males tend to have higher), age, atheltic background and exercise mode