Week 10: Medication Administration
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
What is the point of Med Admin rules?
patient safety
Medication administration is:
knowing, understanding of the why and what for as well as the manual dexterity to administer it while caring for the patient
Client safety is ________________
Client safety is doing what’s necessary to reduce harm including human and system errors
Medical administration encompasses:
caring, compassion, critical thinking and strict attention to patient safety
What are the top 4 standards of medication guidelines from CRNA?
Safety
Authority
knowledge
Ethics
What is standard 1 of the CRNA guidelines for medication administration?
safety: responsible and accountable to provide safe medication management
What is standard 2 of the CRNA guidelines for medication administration?
Authority: regulated members must follow current regulations such as who can we give what to
What is standard 3 of the CRNA guidelines for medication administration?
Knowledge: regulated members must be knowledgeable about what they’re giving including NHP’s
When can students perform activities that include med admin and other procedures?
•Which they have received formal theory and lab instruction and are deemed competent by the clinical instructor to perform the skills
when it comes down to two policies, the most restrictive policy prevails (i.e. FON, or clinical agency)
What are the main 10 rights of medication administration?
right drug
right dose
right patient
right route
right time
right documentation
right reason
right frequency
right education/ to know
right to refuse
what are the other 5 mundane rights of med admin?
right assessment
right site
right technique
right approach
right route
What should we always do when giving medications?
introduce ourselves
communicate with patient, 3 checks (arm band)
vitals before medication
explain medication and what each one does
what are the 3 checks of drug admin?
compare medication label to the MAR (record) as we remove it from storage
compare medication label to the MAR (record) as we prepare the drug (remove from container)
compare medication label to the MAR (record) as we return the drug to storage area
Prior to administering any and all medications, we must?
do the 3 checks and 10 rights must be completed
What is the AHS patient identification policy?
Patient identifiers shall be used to confirm the patient’s identity prior to a health service being provided, to confirm that the correct patient receives the intended health service
How do we identify a patient according to the AHS identification policy?
both the patients first and last name
full date of birth (day, month and year)
ULI (unique identifier)
Medical record number (MRN)
patient ID barcode ==> we scan it?
Photograph
How does co-signing medications work?
some medications require a co-signature from regulated health care professionals
student is one signature
regulated health care professional is the second signature
Medications requiring a co signature, direct observation of preparation, and initial direct observation of medication administration include:
aka. what meds need co-signatures and direct supervision?
Narcotics —> morphine, alcohol, cannabis
all IV medications
High alert medications
paediatric dosages?
other medications depending on policy of place
What are common medications we co-sign in 2nd year?
Diabetic medications
thrombolytics medications
opioids
paediatric fractional doses
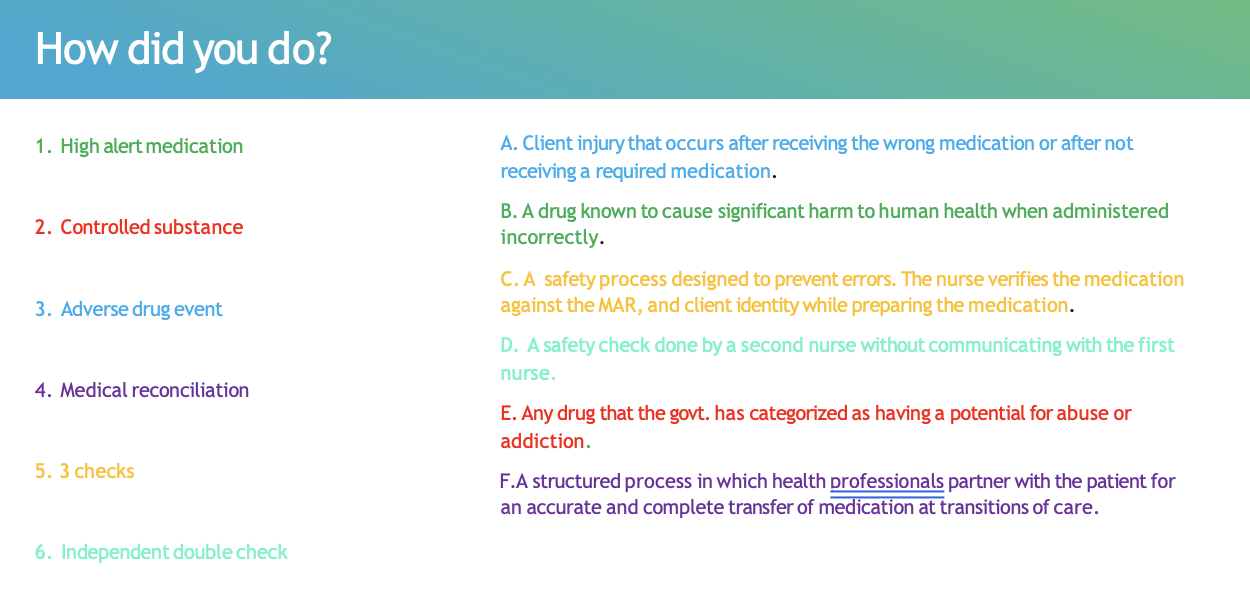
What is an indepedant double check?
consistent process prior to medication administration
Two (2) health professionals (student would be a 3rd) shall independently verify the medication prior to administration
The first health care professional shall not communicate to the second until the second has finished verification, each will then share results.
**This is done for high alert medications ==> they also do the 10 rights and 3 checks
Co-signing vs. Indepedant double check
Co-signing = shared responsibility
Independent double check (IDC) = two separate verifications, one decision
Co: Two regulated health professionals review and approve the same medication order together, and both are legally accountable.
IDC: Two qualified clinicians separately verify a high-risk medication without influencing each other, then proceed.
Independent double check = separate verification.
What are high-alert medications?
‘a drug known to cause significant harm to human health when administered incorrectly’
***high alert medications are drugs that bear a heightened risk of causing significant patient harm when they are used in error”
What is an adverse drug event?
clinical injury occurs after receiving the wrong medication or not recieving required medication
What is the MAR?
Medication administration record
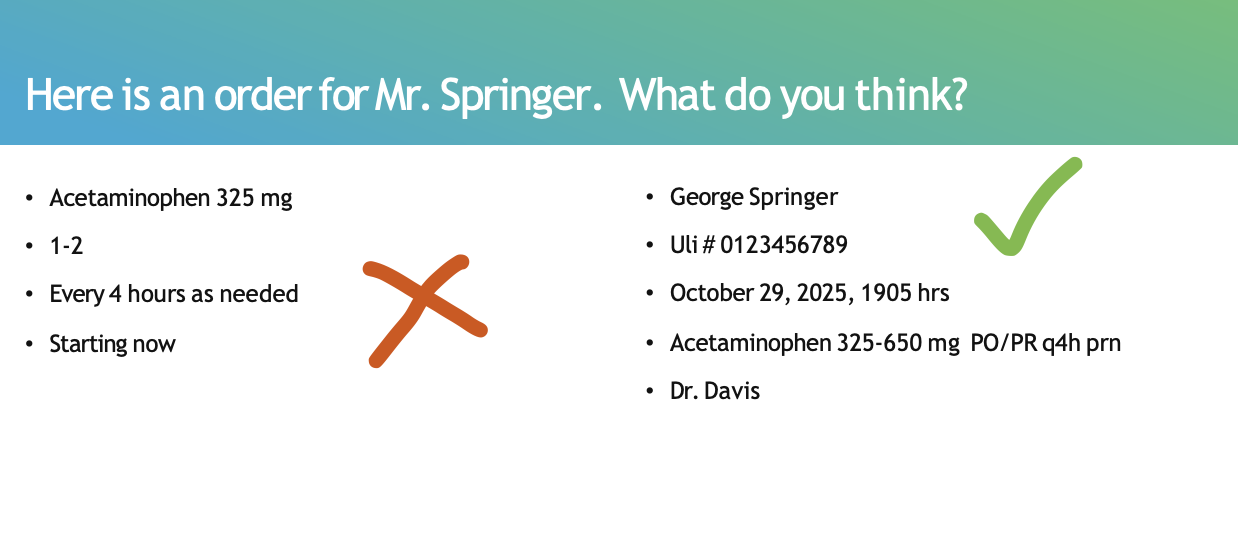
What does the MAR contain?
the patients full name and ULI
date and time the order is written
Medication name, dose and route
time and frequency of administration
signature of prescriber
***We CANNOT give medication without the full complete medication order
We can use abbreviations, true or false?
False
What does instillation route of admin mean?
Instillation is a medication administration route where a drug is placed drop-by-drop into a body cavity or opening, rather than swallowed or injected.
aka. nasal, eye, ear, vaginal, rectal
what are characteristics of the oral route?
Easiest and most desirable way to administer
Comes in many forms i.e. liquid, tablets, capsules, sustained release, buccal, sub lingual
Patient must be able to swallow well (prevent aspiration)
have no contraindications (NPO)
and no GI alterations that would prohibit intake (such as being on NG suction).
what are characteristics of the topical route?
•Medications applied to intact skin or mucous membranes
•Come in many forms such as pastes, lotions, ointments, or patches
•Can be local or systemic in effect, and maybe timed release
Do we wear gloves during topical administration, yes or no?
yes
We must wear gloves during topical administration so that we don’t absorb the medication
**Document where we applied the patch and document taking off the old patch
What are characteristics of the inhalation route?
•Medications that are inhaled and penetrate the lung airways
•Rapid absorption
What should we include in the documentation of Medication Administration?
date and time
medication administered
route administered
Patient response
medication effects
observations of any sort
**Don’t forget to sign off
what medication we gave, time it was given, what dose and route was give, reaction patient had.
-We HAVE to make sure we indicate what route/order we gave it
What is medication reconciliation?
“…a structured process in which health care professionals partner with the patient, family, and caregiver for an accurate and complete transfer of medication information at transitions of care.
Generic vs. Trade names?
Trade name:
used for a medication that is designed, researched and manufactured by a trademark pharmaceutical company
Generic name:
an affordable drug reproduced with the same active pharmacological ingredients
What are the different ways to distribute meds?
Unit dose —> individually with patient’s name
Ward stock —> common place to just go and get meds
Automatic dispensing —> PIC
what should we review before giving the medications even after 3 checks and 10 rights?
review medication order
review patient allergies
considering the reason for administering medication
check any lab results (blood glucose before insulin)
Extra info:
•Communication —> patient education, right to refuse,
•Patient teaching
•Cultural considerations —>dietary habits that might affect medications, privacy when exposing body parts (r they allowed to see opposite sex see them exposed, spiritual belief etc.)
When is medication reconciliation done?
Medication reconciliation is done any time care is being transferred or changed — not just once.
Medication reconciliation is the process of creating a complete and accurate list of a patient's current medications and comparing it to their new medication orders to prevent errors, omissions, or overdoses
Medication reconciliation is done in which situations (name all)?
Medication reconciliation happens whenever the patient’s care setting changes.
Reconciliation = ATD
Admission
Transfer
Discharge
Controlled substance:
The government categorizes it as having potential for abuse or addiction