SAM Exam 2: Urinary
1/41
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Proteinuria
Marked proteinuria w/ inactive sediment is the hallmark of glomerular disease!!
Et: hallmark of glomerular dz
Lower UT > upper urinary tract
Limited by filtration barrier, fixed negative charges, tubular reabsorption/catabolism
Dt: location of kidney dz, UPC if inactive sediment
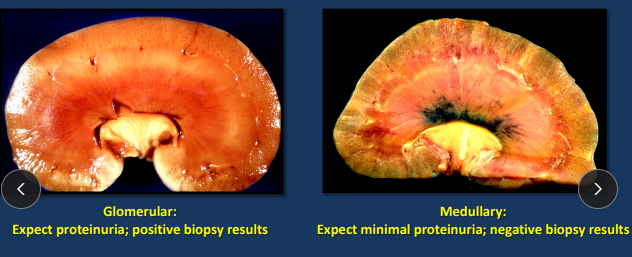
Glomerular: proteinuria, ↑ cholesterol, ↓ albumin
Endothelium
Visceral epithelial cells (podocytes)
Medullary: isosthenuria, no proteinuria
Tx: ACE inhibitors, ARBs, Diet
Rules for Diagnosing Proteinuria
Indicates glomerular dz vs medullary dz
UPC is unreliable in presence of pyuria or hematuria
Needs inactive sediment
Urine Protein/Creatinine Ratio “UPC”
↓ Upr/Ucr + azotemic + ↓ GFR ≠ improvement
Diet protein + ↓ albumin worsens urinary protein loss
Nephrotic syndrome
What: Poor GN prognostic indicator
Et/Cs:
Proteinuria
↓ hypoalbuminemia and ↑ hypercholesterolemia
Plasma [cholesterol + triglyceride] inversely correlated w/ serum [albumin]
Edema/ascites
Hypercoagulable state
Thromboembolism (15-25%)
Loss of anti-thrombin III in urine → inhibit factors II, IX, X, XI, XII
Hypertension (50-80% dogs)
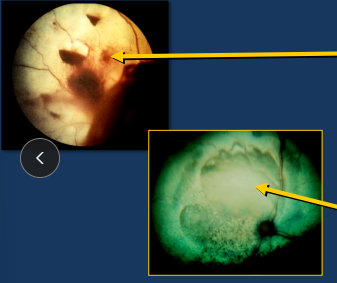
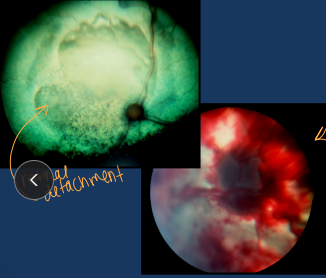
Retinal hemorrhage/detachment
Always check BP
Tx: amlodipine, enalapril
Glomerular Anatomy
Endothelium
Neg charges in endothelium, GBM, podocytes
Glomerular basement membrane (GBM)
neg charges in endothelium, GBM, podocytes
Type IV collagen for size selectivity
Podocytes (visceral epithelial cells)
neg charges in endothelium, GBM, podocytes
Mesangial cells
Produce matrix, phagocytic, contractile, modulate injury
Microfilaments: Respond to vasoactive substances and alter surface area (angiotensive 2)
Glomerular Nephritis
Immunologic injury underlies most cases of glomerulonephritis
Et: infections, neoplasia, genetics, idiopathic
Sig: old male
Membranoproliferative GN: Wheaten terrier, Bernese, Brittany Spaniel
BM disorders: English Cocker, Samoyed, Doberman & Bull terrier
Cs: CKD, liver rupture, hemoabdomen, poor coat, weight loss, small irregular kidneys, nephrotic syndrome, thromboembolism, retinal hemorrhage/detachment, hypercoagulability
Dt: BP, variable proteinuria/UPC, ↑ cholesterol, ↓ albumin, Azotemia, ↑ P, microalbuminuria (unclear Px factor, vascular dz - increases risk for renal dz), biopsy definitive (Renal cortical tissue, IH, EM, IF)
Macroalbuminuria - UPC >0.5
Tx: ACE inhibitors, Angiotensive receptor blocker, ↓ Na Diet, low dose Aspirin, Clopidogrel!, Mycophenolate, decrease glomerular hydrostatic pressure
Prognosis: variable, treat the proteinuria
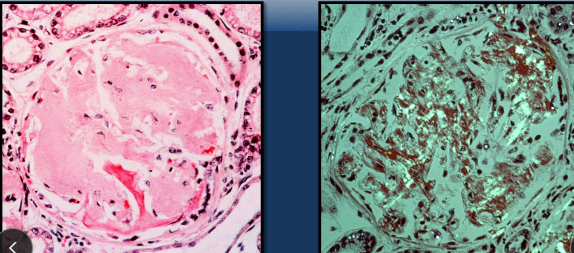
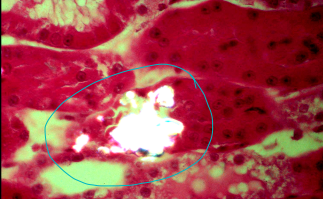
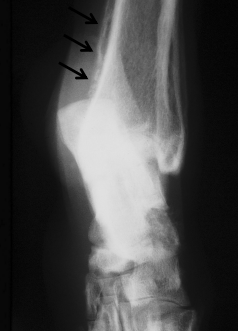
Amyloidosis
Path: β-pleated sheet deposits
Distribution: systemic (most common) > localized (pancreatic islet cells of cats)
Cat are 100% medullary, 75% glomerular
Protein: AA, AL, ATTR, Aβ2M, AIAPP
Et: Reactive systemic dz, idiopathic, familial (dogs, cats)
chronic infectious and non-infectious inflammatory, neoplasia
Sig: Mid age, Shar Pei (M), Beagle (G), FoxHound (G), Abyssinian (M), Siamese (M), Oriental (M)
Glomerular > Medullary - dogs except shar pei
Medullary > Glomerular - cats including Abyssinian
Lugol’s iodine can be used to presumptively identify
Cs: CKD, recurrent fever, tibotarsal swollen joints(shar pei), liver rupture, hemoabdomen, poor coat, small odd kidneys, nephrotic syndrome, thromboembolism, retinal hemorrhage/detachment - sudden blindness (Ab. cats)
Cs from kidney involvement + CKD: except shar pei and cats which is liver rupture, hemoabdomen
Dt: proteinuria/high UPC >10, ↑ cholesterol, ↓ albumin, Azotemia, ↑ P, microalbuminuria (unclear Px factor, vascular dz), biopsy definitive (Renal cortical tissue, IH, EM, IF, Lugos iodine)
Tx: none to be benifical, relentless Px is the rule

Pathophysiology of Acute Renal Failure
Types:
Pre-renal: hypoperfusion, Physiologic oliguria, Reversible
Intrinsic: nephrotoxic nephrosis, nephritis, ischemia
Post-renal: obstruction
MOA: obstruction, tubular backleak, intraluminal crystal deposition
Ischemic nephrosis: tubular degeneration, acute tubular necrosis, afferent arteriole constriction, vasomotor nephropathy, Systemic Arterial Hypotension = NOT REQUIRED
dehydration, shock, anesthesia, sepsis, hemorrhage, trauma, ACE inhibitors, myoglobinuria, NSAIDs.
NSAIDs: impair renal vasodilation, worsen ischemic injury
No direct renal damage; GI bleeding and impaired renal autoreg
Nephrotoxins: direct tubular cell injury rather than ischemia, low ATP, cell death, renal vasoconstriction
Ethylene glycol, aminoglycosides, cisplatin, NSAIDs, Easter lily (C), heavy metals(arsenic, lead), grapes/raisins (D), hypercalcemia (rodentaside)
** Simultaneous exposure: nephrotoxins & ischemia increases risk of renal injury
Nephritis: lepto (D)

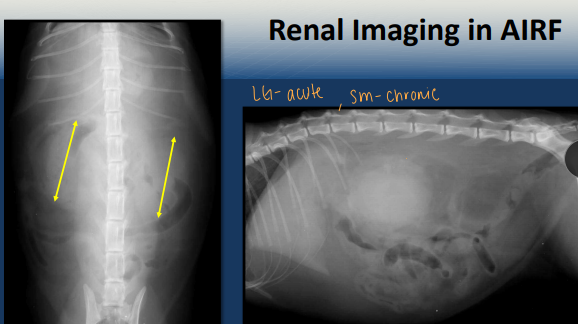
Diagnosis of AIRF
History: Absence of longstanding PU/PD, potential for renal ischemia or nephrotoxin exposure, oliguria, polyuria, non specific signs
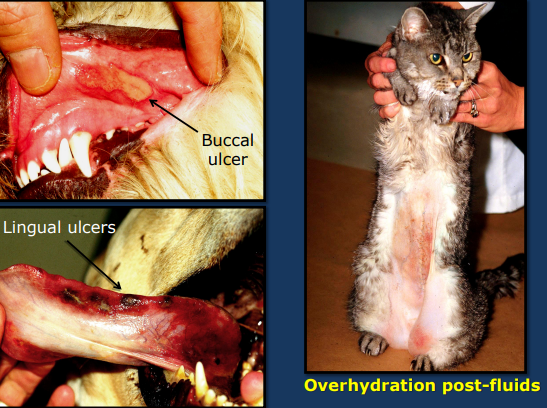
PE: normal BCS, uremic breath, oral ulcers, hypothermia(nephrosis) or hyperthermia (nephritis), back pain(renal pain)
Absence of pallor MM
No evidence of lower urinary tract obstruction
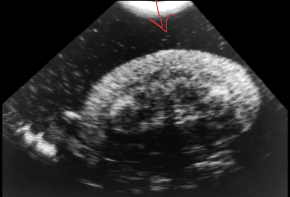
Labs: chemistry/cbc/UA/renal size(normal to large)/renal biopsy
labs BEFORE treatment = helpful
uremia usually are more severe than in pre-renal azotemia
CBC: increased BUN, creatinine, phosphorus (severe)
hyperkalemia severely impaired renal excretory function and oliguria
Hemogram: Anemia = NOT early on (more common with CKD)
TP = normal to elevated (hydration)
+/- thrombocytopenia (Lepto)
Inflammatory / stress leukogram
UA: DILUTE very early on 1.007-1.017
Does NOT differentiate AIRF from CKD (both have low USG)
Proteinuria, Hematuria, May see glucosuria w/ normal blood glucose
Increased WBC, RBC, tubular epithelial cells = Non-specific reaction to renal injury
Blood gases: Moderate / severe metabolic acidosis during
maintenance phase of AIRF
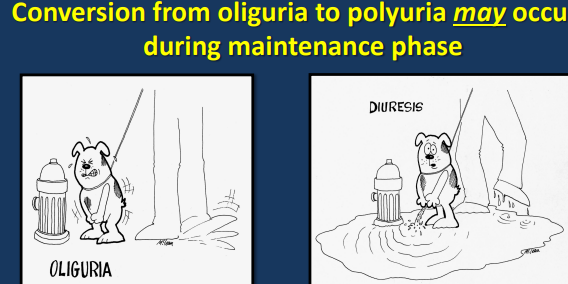
Maintenance Phase of AIRF
severe decrease in RBF and GFR
RBF returns to normal → GFR remains low
Urine output
Oliguria
Normal urine output
Polyuria
Patient experiences a 1-3 week course before restoration of renal function can occur
Removal of the inciting cause at this point will NOT result in immediate return of renal function
severe baseline azotemia during the maintenance phase often are NOT successfully managed without dialysis
Recovery Phase of AIRF
Return of normal BUN & Creatinine = POSSIBLE
decreased GFR may persist → sometimes
Partial improvement = CKD
Urinary concentrating defect may persist
Death / euth:
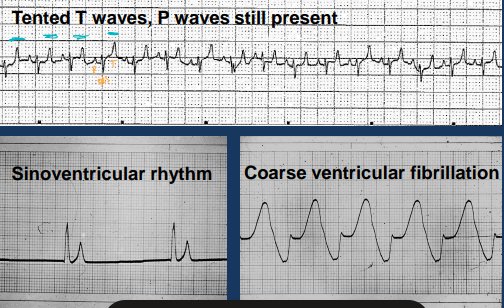
Hyperkalemia → fluids, insulin, calcium gluconate, sodium bicarb
dialysis if persistent
Metabolic acidosis
Severe azotemia
Tx: Meticulous attention to fluid therapy
Potassium affects RESTING potential
Calcium affects THRESHOLD potential
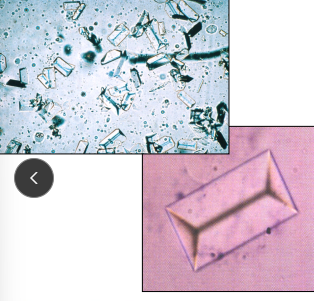
Ethylene Glycol
Alcohol dehydrogenase → the problem (1st-2nd metabolism) then moves to Lactate dehydrogenase (after glycolate) **
Et: AKI; glycolate/glyoxylate → Ca oxalate crystals : causes obstruction intraluminal or intracellular
Cs:
Neuro (<12h) → intervene here
Cardio(12-24h) → intervene here
Renal (24-72h) → when the problem occurs
profound oligo-anuric AIRF (almost always fatal once established)
oligo-anuric AIRF (fatal)
Dt: dilute urine, oxalate crystalluria, ↑ Anion Gap/OG, ↓ Ca, progressive azotemia
False + : Propylene glycol, glycerol, metaldehyde
False - : <30mins after ingestion, >12h after
Tx: TIME! w/in 4 hours of ingestion Decontaminate/GI lavage, ethanol, fomepizole(4-methylpyrazole)!!, dialysis(furosemide)
within 2-4h is best Prognosis
ethanol → within 4h ingestion
fomepizole 4-methylpyrazole → within 8h ingestion
Cats: within 3h of ingestion

Leptospirosis
Et: L. cterohaemorrhagiae + L. canicola
filamentous, motile, spirochete bacteria
urine, wildlife(rodents), zoonotic

Path: leptospiremia (2-12d) → ARF, hepatitis, DIC
Affect kidney and liver
Cs: fever, vomiting, dehydration, pain, ARF (oliguria, PU/PD), icterus, vasculitis, DIC, jaundice, AHF, hepatic fibrosis
#1 cause of ARF/nephritis → infects renal tubule
Dt: serology (MA titers ≥1:800) → antibody, PCR → antigen
Antibody titer - most common
Tx: Doxycycline, penicillin (↓ trans), hemodialysis, multivalent vax
Good Px if Tx early
Chronic kidney Disease
Et: Chronic tubulointerstitial nephritis(idiopathic), genetics
No longer able to maintain: excretory, regulatory, endocrine functions
Nitrogen, fluid, lyte, acid-base, hormome imbalance
Cs: Anorexia/weight loss, PU/PD, vomiting, oral lesions, pale MM, dehydration, osteodystrophy(2ndary), edema, hypertension, retinal detachment, murmurs, mineralization, cachexia, Proteinuria & hypertension = Poor Prognosis
Dt/Labs: Small/ odd kidneys, nonregen-anemia/lymphopenia, isosthenuria, azotemia, ↑ P, odd PT gland, biopsy (diffinitive)
Serum EPO: low to normal
30% – 65% of cats with CRF have associated anemia
Don’t judge pre multi day fluid tx for those w/ decompensated CRF
Tx: MAKE patient feel better #1, ↓ Diet P!!/Na, ↑ diet protein/ omega 3/ K, P binders(diet fails), ACE inhibitors, Calcitriol, erythropoietin, appetite stim, ACE inhibition: amlodipine/enalapril
Chronic progressive: Dogs live less (<1y) than cats
Progression of CRF
Intraglomerular hypertension (SNGFR)
Increases in phosphorus, PTH, BP
Systemic hypertension → treat: BP consistently > 160 mm Hg
Ocular, cardiovascular
Renal 2nd hyper-PTH
Renal mineralization (Ca x P product)
UTI
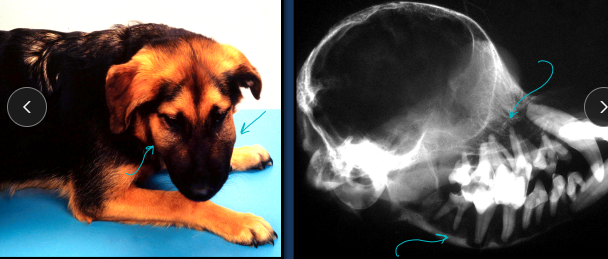
Renal Secondary Hyperparathyroidism
A genetic condition affecting young, growing dogs, primarily in Terrier breeds
bony overgrowth in the jaw, and Fibrous Osteodystrophy
metabolic disorder, often due to kidney failure and secondary hyperparathyroidism, which causes the jawbone to soften and expand

Staging Chronic Kidney Disease
Staged @ stable and hydrated
IRIS Staging: Creatinine-based / SDMA
I: <1.4 (D) <1.6
no azotemia, normal creatinine
II: 1.4-2.8 (D), 1.6-2.8(C)
mild azotemia
III: 2.9-5 (both)
mod. azotemia
IV: >5 (both)
severe azotemia
Substaging: proteinuria (degree) → UPC & systemic hypertension (magnitude)
Cats progress slower then dogs!!
Cats hang out in stage 1-2
Dogs hang out in stage 3-4
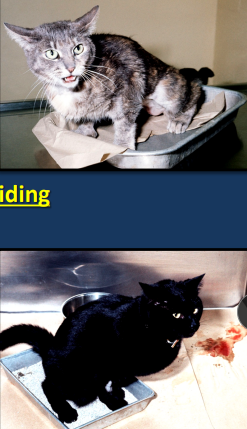
Feline Idiopathic Cystitis
Stress, genetics —> “get better” in 5-10 days regardless of tx
Et: Bladder/urethra hemorrhagic inflam, idiopathic!!
Leaky urothelium, MCl infiltration, overactive PSN
NOT associated w/ bacteria!! or narrow urethra (males)
Sig: fixed, 2-6y, Persians, dry food, stress, indoors
Cs: Inappropriate urination, stranguria, ± hematuria, pain bladder/small, Pollakiuria
“FISHY” signs wax + wane
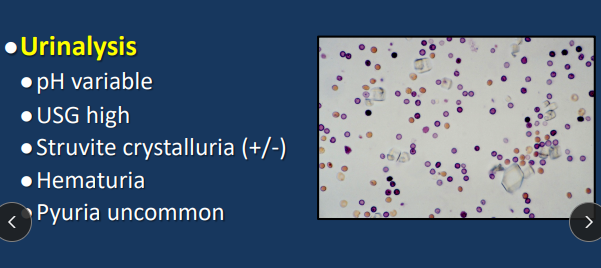
Dt: US of Sm thick bladder, ↑ USG, non septic UA
Crystals normal in cats, always check for them
Tx: ↑ drinking, anti-stress envrio, Feliway, analgesia, ace, phenoxybenzamine, amitriptyline, buspirone, wet food
Spontaneous recovery (5-10d), common reoccurrence, no cure
Acidifying or ↓ Mg does NOT work
FIC is NOT caused by bacteria!!!
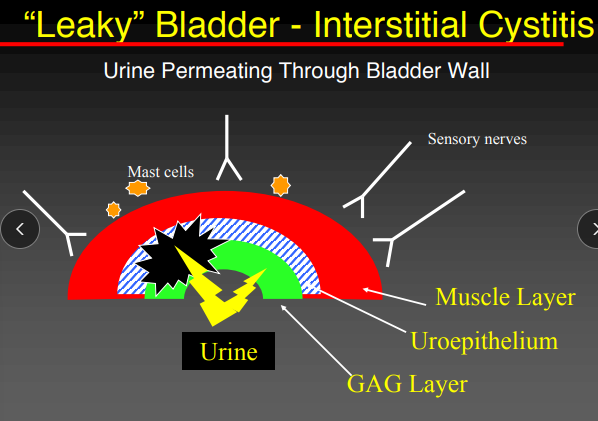
Feline Idiopathic Cystitis: Pathophysiology
Abnormal bladder permeability
Altered glycosaminoglycan layer (GAG)
Mast cell infiltration
Upregulated sympathetic outflow
Increased sensory nerve terminals and substance P
Urethral Obstruction in Cats
Et: Urethral plug, struvite, Ca oxalate, neoplasia, idiopathic
↑ Intratubular pressure, ↓ GFR, ↓ Renal perfusion
Cs: early/partial: stranguria, pollakiuria, hematuria, late/complete: vomiting, anorexia, Lg painful bladder- difficult to express, resistance to catheterization, arrythmias
Acute reversible oliguric renal failure
Dt: ↕ Azotemia, ↑ P, ↑ K (Tented T), met. acidosis, ↓ Na, Ca
Normal P range = 2.5-5.5 mg/dl
Tx: Fix ↑ K, BES fluids, decompressive cystocentesis, hydropulpulsion, analgesia, catheter + pain meds, perineal urethrostomy (>3 reoccurances)
Med emerg: complete obst. → Uremia + death 3-5d w/o tx, self limiting diuresis 2-7d post
Treat while running tests
Sx does not prevent reoccurance or FIC
Balanced electrolyte solutions (e.g. lactated Ringers solution, Normosol-R) but can use NaCl if you have to
Post-obstructive diuresis
Self-limiting
Lasts 2 to 7 days
kidneys produce an excessive, inappropriate volume of urine after a urinary tract obstruction is relieved
What causes azotemia in cats with urethral obstruction?
increased Intratubular pressure
Low GFR
Low Renal perfusion
Cathaterization
Remove if:
Relatively easy
Urine is clear after flushing
Minimally sick cat
Place if:
Difficult to do
Urine still very bloody or cloudy after flushing
Very sick cat
Rx: use analgesia, avoid antimicrobials while catheter is in place
Dt: watch urine output and monitor for hypokalemia→ add KCl
Watch for: post obx diuresis, urethral spasm (give ace)
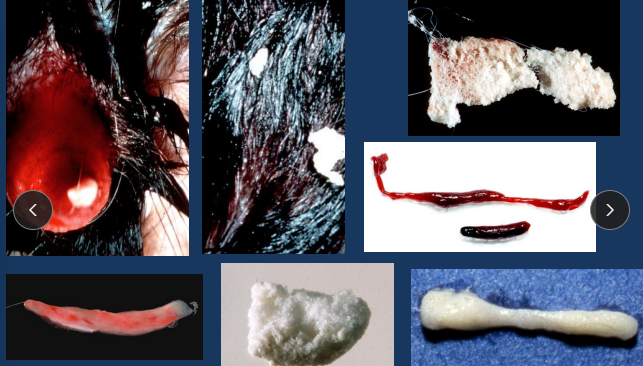
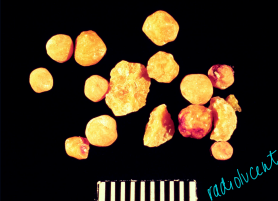
Urinary Stones in Small Animals
Types
Dogs: Struvite > Oxalate > Urate > Cystine
Cats: Oxalate > Struvite > Urate > Cystine
Cs: location, duration, UTI dependent
Kidney: none, flank pain, hematuria, infection, renal failure
Ureter: silent or acute obx/post-renal azotemia
Bladder: dysuria, pollakiuria, hematuria
Urethra: obx, post-renal azotemia, dysuria
Sx discouraged for urethral stones
Radio-opque: struvite, oxalate
Tx: Dissolution for struvite, urate, cystine
Unlikely to cause obx = do not remove
Likely to cause an obx = remove w/ lithotripsy and basket retrieval
Urethral sx is discouraged

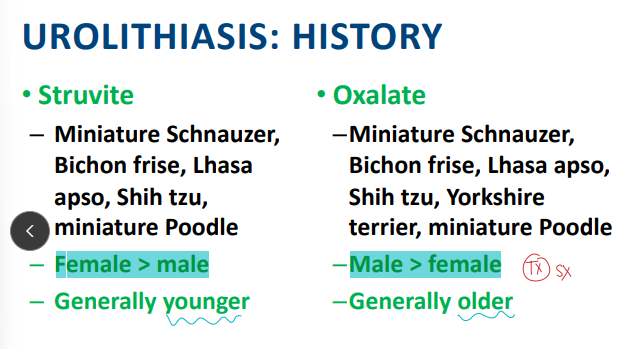
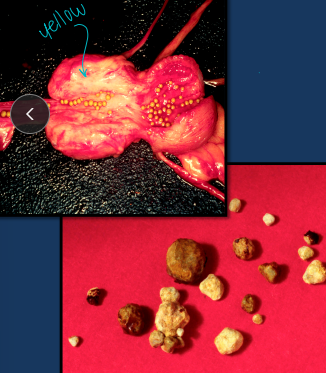
Struvite Uroliths
Due to infection
Et: + Urease bacti UTI (D), Alkaline urine
staph, proteus, pseudomonas, klebsiella infection
Sig: Dogs → bladder
Cs: location, duration, UTI dependent
Dt: radiopaque, culture, UA
Tx: Dissolution diet + antibiotics, catheter, urohydropropulsion, Sx
eradicate UTI, recurrence >20%
Urine pH <6.8
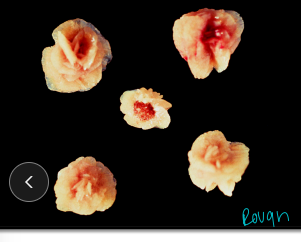
Calcium Oxalate Uroliths
Et: bladder (D), kidney/ureter/bladder (C), ↑ calciuria
Cushing’s, idiopathic ↑ Ca (cats)
Increasing incidence
Sig: Old, fixed, male, cats, sm dog, Persian, Himalayan, acidifying diet, indoor
Cs: location, duration, UTI dependent
Dt: radiopaque, UA
Tx: catheter, urohydropropulsion, Sx, hydrate, citrate supp, thiazides, Rx diet
dissolution NOT possible, ↑ reoccurance, avoid acidifying/excess protein diets
Altered calcium metabolism can result in increased urinary excretion of calcium (hypercalciuria)
Urate Uroliths
Et: ammonium acid urate, Bladder/urethra
Hepatic urate transport dz in Dalmatians
Radiolucent
Sig: Dalmatians, Bulldogs, Portosystemic shunts, males, mid age
Defective” uric acid metabolism
Converted to allantoin by dogs other than Dalmatians
Cs: location, duration, UTI dependent
Tx: ↓ purine/protein diet, allopurinol, alkalinization, catheter, urohydropropulsion, Sx
↑ reoccurance
Cystine Uroliths
Et: Bladder/urethra
UTI complicates, not predisposes
Radiolucent
Sig: 4-6y, male Bulldogs, Dachshunds, Irish Terriers, Newfie, Bassets
↓ w/ age, least common
Cs: location, duration, UTI dependent
Tx: ↓ protein diet, alkalinization, neutering, catheter, Sx↑ recurrence, neuter
Voiding hydropulsion
Stones must be small
< 4 mm in female dog
< 2 mm in male dog
Renal Tumors
Et: rare - primary, malignant, (common)metastatic carcinomas/adenocarcinomas, lymphoma
Sig: Older, GSD
Cs: anorexia, weight loss, abdominal mass, hematuria → painless
Polycythemia (↑ EPO), leukemoid rxn, ↓ glucose, hypertrophic osteopathy → Transitional cell carcinoma
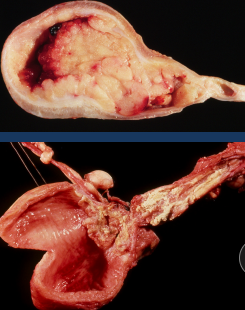
Bladder Tumors
Et: Transitional Cell Carcinoma
Trigone > Fundus
Locally invasive and metastasize (lungs) → prone to seeding
Sig: Dogs, old, Scottish Terrier, recurrent UTI
Cats are low risk
Cs: Dysuria, stranguria, pollakiuria, hematuria, incontinenc
Most dogs = T2/T3 at presentation
RECAL EXAM! esp. females w/ dysuria
Dt: hematuria, pyuria, malignant epithelial cells, urine culture, Cytology/biopsy, BRAF test (cells w/ mutation, high specificity/sensitivity), imaging
can cause obstruction and hydronephrosis
Risk of seeding during Sx, biopsy, cysto
Tx: Partial cystectomy (<80%), piroxicam, chemo, radiation
Palliative: Tube cystostomy (chronic UTI risk), Urethral stenting
Piroxicam is a non-COX-specific NSAID - Not directly cytolytic
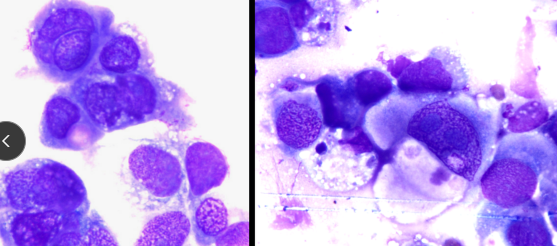
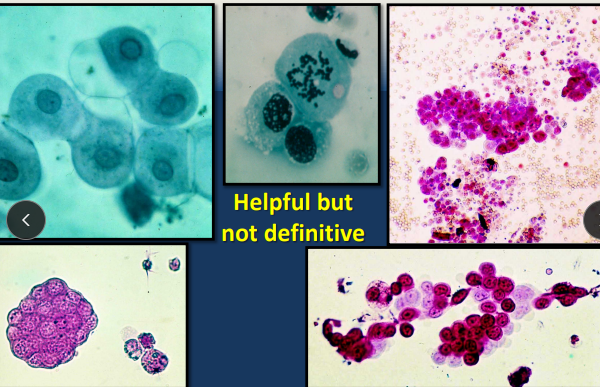
Urethral Tumors
Rare
Et: TCC > SCC
Sig: old dogs, females
Cs: LN metastasis, urethral obstruction, UTI
Dt: Rectal examination is KEY part of physical
examination!
Metastasis to regional lymph nodes
Tx: Tube cystostomy, Piroxicam
Urinary Tract Infection (Cystitis)
Et: single ascending G- organism, e-coli (most common)
Bowel flora
Cs: hematuria, pollakiuria, dysuria, stranguria, urge incontinence, inappropriate small volume urination
Dt: PE, History, prostate exam (M), peri-vulvar conformation (F), UA, alkaline pH (+ urease bacti), cysto + culture
Tx: Antibiotics, hydrate
First: Amoxicillin, Sulfa(kcs), Cephalexin, Cefadroxil
Second: Amoxicillin/clavulanate, FQ(resistant)
Third: cephalosporins(simplicef), Aminoglycosides(kidney/ear toxic), convenia
Urine concentration may be 10-100 times higher than blood concentration
Urine Cultures
Why: UTI
Baci suggestive not diagnostic
Not done if subclinical
How:
Cysto: >1,000 CFU/ml = infection
Gold standard
Catheter: >10,000–30,000 CFU/ml = infection
ISCAID UTI Guidelines
Sporadic Cystitis: uncomplicated, isolated UTI w/ lower UT signs
Sig: RARE in cats and intact males
Dt: LUT signs + UA + culture
Tx: Amoxicillin (#1), amoxi-clav, TMS
No benefit from nutraceuticals (cranberry, D-mannose)
3-5d duration
Recurrent Cystitis: ≥3 in 12m or ≥2 in 6m
Et: Recessed vulva, ectopic ureters, PU sx, Cushing’s, DM, neoplasia, catheterization
Dt: culture, imaging, cystoscopy
Tx: targeted antibiotics for 14d duration
Pyelonephritis: upper UTI
Bacterial Prostatitis: infection of prostate
Subclinical bacteriuria:
Et: + culture but no CS (diagnostic culture not req)
Tx: None (unless pre-op or spinal cord injury)
NOT associated w/ cystitis dev or poor survival
Canine Urinary Incontinence
Et:
Neuro: UMN/LMN bladder, Detrusor-urethral dyssynergia, Dysautonomia - large bladder
Non-Neuro: Ectopic ureters, pelvic bladder, Obx, UTI, idiopathic, PSMI - small bladder
Sig: Lg female dogs, spayed
Dt: CBC, Chem, UA, Urine culture, BP, imaging
Cs:
Lg bladder: UMN, LMN, paradoxical
Sm bladder: PSMI, urge incontinence, ectopic ureters
Tx: Phenylpropanolamine(proin), Estrogens(incurin), Testosterone, Collagen, Suburethral sling / TVT-O tape, Hydraulic occluder, Artificial urethral sphincter

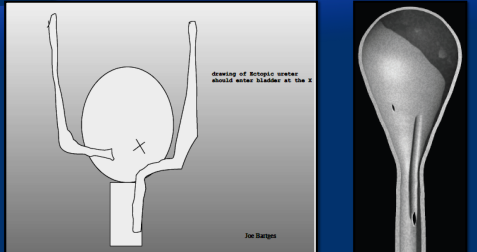
Ectopic ureters
Sig: young(born with it), females, Labs, Goldens, Huskies
Cs: constant or intermittent dribbling, recurrent UTIs
Dt: cystoscopy, contrast CT
Tx: cystoscopic laser ablation, neoureterostomy, ureteroneocystotomy, hydraulic occluder
Drugs for Cardiovascular function
ACE inhibitors (enalapril, benazepril)
Why: Hypertension, proteinuria, CKD, GN, kidney dz, FIC
How: ↓ glomerular capillary hydrostatic pressure by ↓ post-glomerular arteriolar resistance
ARBs (telmisartan)
Why: Hypertension, proteinuria, kidney dz, GN
Amlodipine: hypertension, kidney dz
Aspirin
Why: Thromboembolism, GN
How: Inhibits platelet aggregation
Clopidogrel
Why: Thromboembolism, GN
Diuretics (Furosemide, Mannitol, Dopamine)
Erythropoietin / Darbepoetin
Why: anemia of CKD when PCV <20%
Risk: antibody formation
Drugs for Electrolyte Balance
Hyperkalemia Tx (Na bicarb, Insulin + dextrose, Ca gluconate, Polystyrene sulfonate)
Phosphate binders (Aluminum salts, Lanthanum carbonate, Sevelamer HCl,
Ca carbonate, Epakitin, Renalzin)
Why: CKD
How: Given with food
Aluminum: toxic but common
Dialysis: Ethylene glycol toxicity, lepto, AKI
Neuromuscular Agents
Pain management (buprenorphine, butorphanol, fentanyl patch)
Why: FIC, Urethral obx
Appetite Stimulation (Cerenia, Mirtazapine, Capromorelin)
Why: CKD
NSAID (Piroxicam, rimidyl)
How: NSAID, not cytolytic, sm tx window
Why: bladder/urethral tumors
Risk: ulcers, never use w/ steroids
Urethral relaxants (acepromazine, phenoxybenzamine)
Why: FIC
Tricyclic antidepressant (amitriptyline)
Why: FIC
Anxiolytic (buspirone)
Why: FIC
How: Stabilizes MC in bladder, ↓ sensory nerve fiber activity
Phenylpropanolamine (PPA)
How: α-adrenergic agonist, ↑ urethral tone
Why: Effective in 75–90% incontinence cases
Risk: ↑ BP, anxiety
Drugs altering the Immune System
Chemotherapy
Cisplatin: nephrotoxic, NOT in cats
Carboplatin: safer alternative
Mitoxantrone
Doxorubicin
Mycophenolate
Why: Immunosuppression, GN
NSAID (Piroxicam, rimidyl)
How: NSAID, not cytolytic, sm tx window
Why: bladder/urethral tumors
Risk: ulcers, never use w/ steroids
Antimicrobials
Fluoroquinolones (-floxacin)
Why: excellent penetration, second line UTI
Risk: Articular cartilage damage (young dogs), retinal toxicity / blindness in cats
Aminoglycosides (amikacin, gentamicin)
Why: resistant cases, third line UTI
Risk: Nephrotoxic & ototoxic
Penicillins (penicilin, amoxicillin)
Why: first line UTI, AKI form lepto
Cephalosporins (Cephalexin, Cefadroxil)
Why: first line UTI
Hormonal Therapy's
Estrogens (DES, Estriol) incurin
Why: incontinence
How: use ↓ effective dose
Risk: alopecia, estrus signs, BM suppression
Testosterone
Why: incontinence, limited success
Calcitriol
Why: ↓ PTH secretion in CKD
How: ↓ serum [PTH]
Use only after ↑P is controlled
Felaway:
Why: FIC