MCN Exam 3
1/155
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
156 Terms
What is the main characteristic of cardiac obstructive disorders?
Involve "stenosis" or narrowing in a vessel
What is considered the perinatal period? Neonatal period? Neonatology?
Perinatal period = 28th week of gestation to 7th day after birth
Neonatal period = Birth to 28 days after birth, "neonate" = baby > 28 days old
Neonatology - subspecialty that deals with mostly sick or premies, neonatologist work in the NICU, high morbidity, goal is to increase survival rate
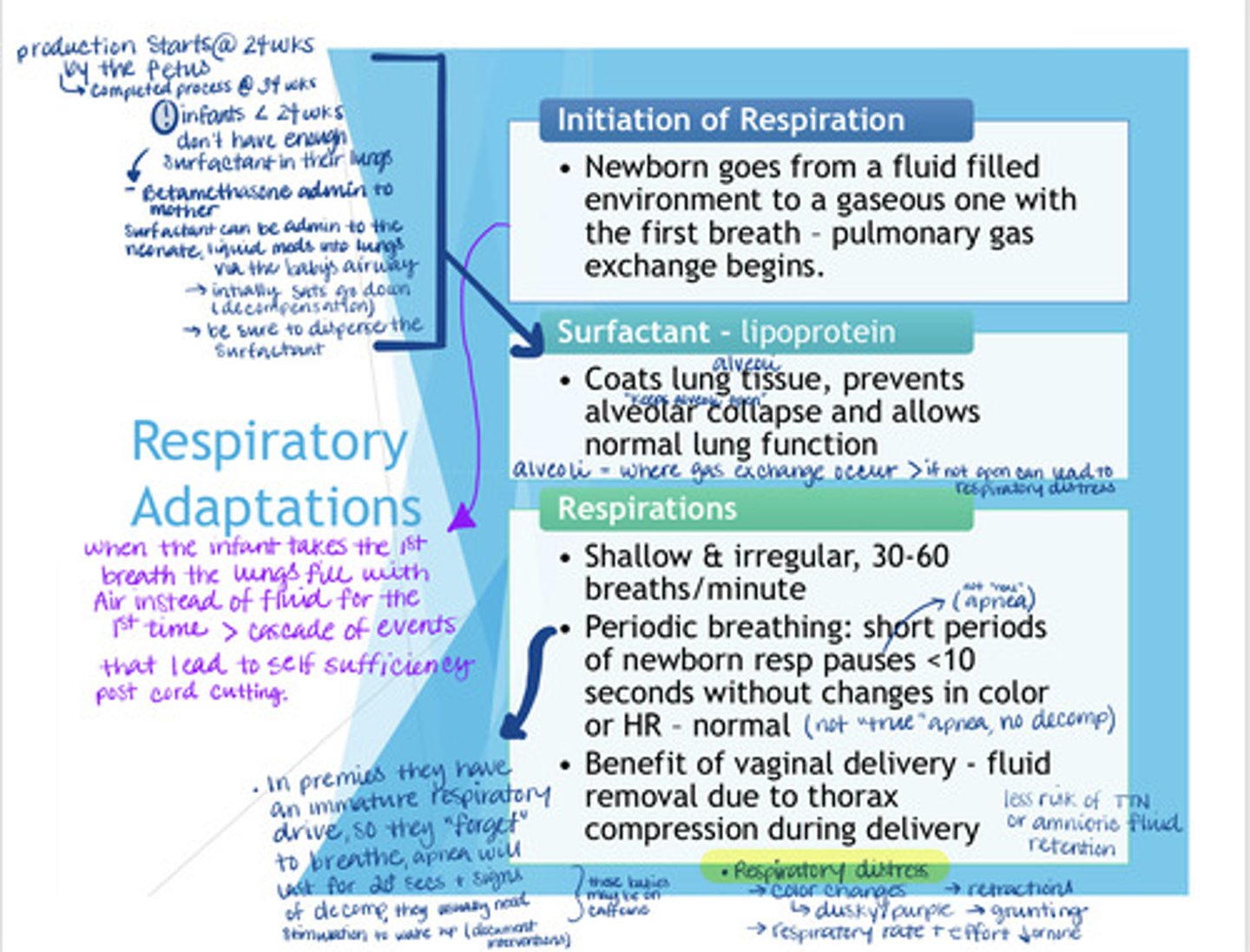
How are respirations initiated in newborns? What is surfactant? How would you describe newborn respirations?
- Respirations are initiated when the infant's lungs fill with air for the first time instead of fluid. Once the cord is clamped it becomes necessary for the infant to become self-sufficient because the mother is not supplying oxygen and nutrients anymore.
___________________________________________
- Surfactant is a lipoprotein that starts to be produced at 24 weeks of gestation and completes production at 34 weeks. This is why HCP are especially concerned about premies who are less than 24 weeks because their lungs are not fully developed & they don't have enough surfactant to keep their alveoli (where gas exchange occurs) open outside of the uterus.
_____________________________________
- It is thought that vaginal delivery is better than c-section because the extra "squeeze" infants get coming out of the birth canal allows for more of the amniotic fluid to come out of the lungs leading to a ⬇ risk for TTN in newborns.
________________________________________
- NV RR = 30 - 60, shallow & irregular w/ periods of apnea. These periods of apnea can be described as "pauses" because they last <10 secs & don't have HR changes or color changes
- Real apnea which is mostly seen with premies is accompanied by HR changes and color changes and last for 20+ secs with signs of decomp
___________________________________________
- During premature labor mothers can receive betamethasone to help speed up the dvlpmt of the lungs if <34 wks
______________________________________________
- Outside of the uterus premies can also receive surfactant directly into their lungs in a liquid form, you should make sure the med is dispersed, intially you will see sats go down and s/s of decomp
_______________________________________________
Respiratory distress = color changes (dusky/purple), grunting, retractions, ⬇ RR/effort or no RR at all
What are some newborn cardiovascular adaptions? (fetal to neonatal circulation)
There are 3 vessels that the fetus uses to circulate their blood
Ductus arteriosus which shunts blood from the pulmonary artery to the aorta
Foramen ovale shunts blood from the right to left atrium this bypasses the lungs since the lungs are not fxing intrauterine
Ductus venosus shunts blood by bypassing the hepatic vessels to vena cava this becomes a ligament once the placenta is clamped
_______________________
Transition from fetal to neonatal circulation happens in steps
Inutero - the O2 and nutrients is provided to the fetus via the umbilical veins and the waste is removed via the umbilical arteries
1. ⬆ O2 in lungs (lungs inflate)
2. All blood vessels open up
3. ⬇ pulmonary vascular resistance, the pressure to get into the lungs ⬇
4. blood flows into the lungs
5. right atrial pressure ⬇
6. ⬆ pressure in the left atrium
7. Foreman ovale closes
8. Ductus venosus becomes a ligament/occluded
9. ⬆ aortic pressure
10. Ductus arteriosus becomes a ligament/occluded
How would describe normal newborn heart rate, blood volume, and blood components?
- NV HR = 110 - 160, * sensitive indicator
- You may hear a benign or fxnal murmur because it can take some time for the fetal vessels to close
-> get a 2nd set of ears to make sure the murmur is not indicative of anything more serious
* neonates are HR dependent bc the ❤ muscle is stiff & can't expand ∴ in order to ⬆ CO the HR must ⬆
- Neonatal BV NV 80 - 85 ml/kg in term NBs
- Fetal RBCs live for about 80 - 100 days due to ⬆ hemolysis, but premie RBCs last 35 - 50 days
- Increased HR (tachy❤) can be caused by:
> fever
> crying
> pain
> drug w/drawal
> volume depletion
> ❤/RR dz
- Decreased HR (brady❤) can be caused by:
> hypothermia
> hypoxia, ⬇ O2 (they don't have stroke volume or ❤ compliance to compensate, their ❤ tired out, it happens after tachy❤)
> hypoglycemia
> sedation probs
> apnea
____________________________
- Fetal RBCs are immature until about 1 y/o
_____________________________
- Leukocytosis, not r/t infection, r/t birth trauma
What is the benefit of delayed cord clamping?
* only delayed for a few minutes
- ⬆ blood volume
- ⬆❤ status
- ⬆ BP
- ⬆ O2
- ⬇ anemia
What is physiologic fetal anemia?
- Starts at 6 - 8 wks of age
> can be caused by:
--> hemodilution due to rapid ⬆ blood volume expansion
--> ⬇ bone marrow activity
--> ⬆ rate of hemolysis
How do newborn's regulate their body temperature? Why is it important
- They can't shiver
- They rely on the nurse to maintain their environment because they can't modify their environment on their own
- They have limited muscle movement
- Their body goes through a chemical process of breaking down brown fat/ breaking down the glycogen stores in brown fat tp produce heat, this is called THERMOGENESIS
- Brown fat is found:
> around the kidneys & adrenal glands
> mediastinum
> scapula
> axilla
> nape of neck
NV temp = 97.7 - 99.5
* ⬆ temp = ⬆ O2 use
* ⬆ temp = ⬆ metabolic rate = ⬆ O2 demand
* ⬇ temp = ⬆ glucose use, energy use
- NBs are unable to balance heat loss & production
- Thin skin but increased body surface area & lack fat
What is NTE?
- Neutral Thermal Environment
- maitain the NB's temp w/out energy i.e. glucose or O2 use
- NO cold stress or overheating
What are 4 ways NBs can lose heat?
1. Evaporation - liquid to vapor, insensible heat loss, when are bron we immediately dry them and remove the wet towel
2. Conduction - heat lost through touch, e.g. cold hands, cold stethoscope, cold weighing table, pv heat los we warm our hands/stethoscope
3. Convection - losing heat loss due to a fan or air conditioner
4. Radiation - when heat is loss by being near an area that has a lower temp
What is the function of the liver?
* all of the fx(s) of liver aren't fully mature until about 3 mos of age
- Blood coagulation
- conjugation of bilirubin
- storage of fat soluble vitamins i.e. A, D, E, K
- Carb metabolism
- Iron storage
- Detox
What are some important notes about the liver's fx (blood coagulation + bilirubin conjugation) in NBs?
- There are 2 types of bilirubin: Unconjugated (fat soluble) + Conjugated (water soluble, ready for excretion), the fx of the liver is to breakdown the unconjugated bili so that it can be excretted in bile, urine, or stool
- When RBCs hemolyze (remember neonatal RBCs only last 80 - 100 days) the broken down heme becomes bilirubin
- Jaundice which is the yellow discoloration of the sclera (the whites of the eyes), skin, and mucous membranes can put NBs @ an ⬆ risk of mild to severe encephalopathy
Why do we admin vitamin K to NBs?
- We gives NBs vitamin K w/in 1 hour of them being born bc they are no longer getting Vitamin K from their mother and they don't have any stored in their liver which can make them @ risk of bleeding
> Concern: premies @ risk of bleeding in the brain due to superficial capillaries in head & brain + r/f intrventricular hemorrhage
- Vitamin K is synthesized int he intestine by our normal flora, neonates don't have this until about 1 week of age
What are some causes of Jaundice?
- overproduction of billirubin
- ⬆ RBC hemolysis
> delayed cord cutting
- impairment in bile excretion
> billiary obstruction
> ⬇ output - not feeding well, not voiding, delayed meconium removal
- liver malfx
What are some important notes about the liver's fx (carbohydrate metabolism + iron storage) in NBs?
- Their energy needs increase postbirth
- @ risk for hypoglycemia
*hypothermia > hypoglycemia
- NV glucose levels - 40+ mg/dl, <40 may require intervention bc the glucose is needed for brain dvlpmt
- They will mainly get energy from the release of glycogen from the liver for the 1st 24hrs (janky feeding schedule), it may take some time to get up to full feedings
- If they are full term they will have enough iron stores for 4 - 6 mos from mother since the last trimester is when the mother shares the most iron w/ fetus, how much the fetus gets is dependent on how much the mother consumes
- Premies are @ ⬆ risk of anemia
- If exclusively breatfed the infant will require iron supplements via diet after 4 - 6 mos, ~ 1 mg/kg/day, ⬆ r/f deficiency
What are some GI adaptions in newborns?
- gut is sterile until the first feeding
- sterile means the gut has not been colonized and is susceptible to infection
- colonizes in 24 hrs
- the stomach is rigid (1st 48 hrs) & can only hold 30 -90 ml, in the first 24 hours it can only hold 10 - 20 ml
- immature gastroesophageal sphincter > "spit up"
- after the 1st feeding when the gut is no longer sterile vitamin K begins synthesis
- maternal breastmilk
> provides protection against bacterial infections of the gut
> contains WBCs & antibodies
> protects the gut flora
- term babies lose 5-10% of their birth weight and gain it back w/in 10 - 14 days
-Meconium is greenish black tarry stool = tissue+blood+intestinal secretions, babies eliminate w/in 24hrs of birth
> if it's delayed, r/f cystic fibrosis/ hirschsprung dz, associated w/ delayed BM
> concerning if they pass meconium inutero
- transitional stool (greenish- brown/yellow, seedy) >> Milk stool (yellow)
*early feeding = ⬆ stools + elimination of bilirubin
What are some renal changes that occur in newborns?
- decreased GFR therefore they can't excrete fluid fast so we have to be careful when we are feeding them or admin fluids or meds
- low specific gravity
- they can go into fluid overload easily
- their 1st voids will have pink uric acid crystals educate the parents about this
- ⬇ ability to reabsorb Na+, fluid loss high
- intolerant to fluid imbalance
- NV urine output: 1 ml/kg/hr = 6 -8 wet diapers/ day in the 1st few days
Why would fluid loss be high in neonates?
- ⬆ insensible loss due to ⬆ metabolism
- ⬆ water loss due to RR
What are some immune system adaptions in newborns?
- 80% of their circulating antibodies = IgG
- IgG can cross the placenta, G = GO as in "GO across the placenta"
- IgA and IgM can't cross the placenta
- IgA antibodies that responds first in GI and respiratory infections
- IgA = high in breastmilk "Breastmilk is A1" immunity boost from mom
- IgM responds in infections in general
- 9 mos - 1 year antibodies reach adult levels
What are three types of immunity and how are they related to neonates?
Natural - skin, mucous membrane, gastric acids, enzymes
Acquired -
> active - absent until you get exposed to a foreign organism
> Passive - antibodies from mom
What are some newborn integumentary adaptions?
- Skin makes up 13% of their bodyweight as compared w/ adults at 8% of bodyweight
- protective barrier against pathogens
- dry, thin, peeling, can easily tare, be careful not to use adhesive/tape on their skin bc it's sensitive
- bc the skin is thin & they have little to no body fat the capillaries are closer to the surface making topical meds easily absorbed through the skin
- starts to dvlp mid gestation and is fully formed by 32 wks
- thremoregulation
- physical trauma protection
- limits water loss but ⬆⬆ heat loss
in what pattern do infants typically grow?
cephalocaudal = head to toe
proximal-distal = center to periphery
What are some newborn neurologic adaptions to consider?
- reflexes - the absence, persistence, or reappearance of reflexes can indicate brain pathology
*early detection
- sensory capabilities include:
> hearing - fully dvlped at birth
> taste - sweet & sour @ 72 hrs
> smell - distinguishes mom breastmilk
> touch - pain, responds to tactile stimuli
> vision - incomplete @ birth, focuses @ 8-15 in, ☑ black & white toys, color vision is at 4 mos., they like human faces, nearsighted, distance&tracking @ ~ 7 mos.
What are some behavioral patterns to take note of in newborns?
4 periods
1. reactivity - 1/2 hrs to 2 hrs, alert, moving, ⬆HR/RR, bonding, eye contact w/ parent, start breastfeeding
2. ⬇ responsiveness - 1 - 2 hrs, sleepy, ⬇ activity, no no interest in sucking, difficult to arouse NB
3. 2nd reactive period - 2 -8 hrs, awake, interest in surroundings, ⬆HR/RR, meconium, voiding, bonding, pt. ed can start
4. Stability - sleep & wake cycle stable after 24hrs
What are some neurobehavioral responses of newborn to take note of?
- orientation - aka alertness, response to stimuli
- habituation - responding and blocking stimuli
- motor maturity - controls & coordinates movement, limited but they can kick their feet and bring their hand to their face
- consolability - self soothing, 5Ss, start to swaddling (make them feel secure & warm), sucking, swinging, shushing (white noise)
- social behaviors - pos response to interaction e.g. cuddling
What is the RAPP assessment?
RA - respiratory activity (breathing/color)
P - perfusion
P - position (are they limp? moving extremities? flexed?)
less formal than APGAR
can be done as the baby is coming out
What is the APGAR score?
A - activity (muscle tone)
P - pulse (HR)
G - grimace (reflex irritability, "big cry")
A - appearance (color)
R - respiratory effort
0 - 2 points for each category
max score = 10
usually 9 because they get marked off for their color (cyanotic appearance, hands & feet)
ax NB transition to extrauterine life
done @ 1 & 5 min after birth
score 5 >> 10 min score
minimum score is 7
4 -7 moderate difficulty
0 - 3 severe distress >> respiratory interventions
How long can it take for a newborn to transition to extrauterine life?
12 hours
What are some immediate interventions for newborns? (airway)
- Suctions, use bulb syringe, mouth first then nose
- dry off w/ towel
- Sometimes just drying them with no suction is fine as long as they are able to breathe well, crying + good respiratory effort
* airway patency
What are some immediate interventions for newborns? (ID)
Make sure they have all of their ID bands, including the security band (alarm) to prevent anyone from leaving certain areas with the child
the NB + mom + S/O get ID bracelets
NB gets 2
Same ID numbers on all of them
What are typical newborn vital signs?
RR - 30 - 60 rpm
HR - 110 - 160 bpm
T - 97.7 - 99.5
Count vitals for a full minute
> infants are intermittent breathers
BP is typically y only done when there's a clinical indication for it
> in the output setting the BP is not typically taken unless they have a jaundice post discharge then there may be concern
VS are taken q30mins until stable for 2hrs
What are some immediate interventions for newborns? (Thermoregulation)
1. dry them off
2. skin to skin with mom ***
- use radiant warmer
- warmed blankets
Maintain Neutral Thermal Environment (NTE)
> warm room temp
> eliminate drafts or ceiling fans
- use a cap
- warm stethoscope
- delay bath until stable
What are some immediate interventions for newborns? (Meds admin)
Erythromycin for the eyes to pv blindness from chlamydia and gonorrhea, pv opthalmia neonatorum conjunctivitis, admin even w/ c-section babies, admin 1 - 2 hrs after birth
> 0.5% 1cm ribbon applied bilaterally to conjunctival sacs w/out touching the applicator to the eyes
Hep B within 12 hours
If mom was positive Hep B, the baby receives Hep B AND immunoglobulin within 12 hours
If mom negative then the Hep B vaccine can be delayed for 1 - 2 months or at first pediatrician visit
Vitamin K is administered to help pv bleeding since the gut is sterile and is not synthesizing clotting factors, admin to vastus lateralis
What is the gestational age assessment?
Dubowitz/Ballard Score
2 categories Physical maturity + Neuromuscluar maturity
Physical maturity = "Please Beg" = PLS BEG:
Plantar creases (hands/feet, ⬆ creases = ⬆ level of maturity)
Lanugo (soft downy hair, fine hair usually on shoulders & back)
Skin texture (color, opacity, vernix)
Breast tissue (⬇ in premies)
Eyes & ears (eyes fused closed until 26 - 28 wks, if born before then eyes will still be fused, look for recoil to sound, how much cartilage is there? << indicates maturity)
Genitals (males, @ 36 wks testes are in scrotal sac females, labia menora prominent as ⬆ age labia majora will cover menora)
Neuromuscular maturity
floppy baby
⬆⬆ flexibility = premie
flexing = term baby
What's included in the newborn H2T ax?
Skin - color, jaundice, cyanosis
Head - size & shape, circumference, skull deformity? Vag birth?
Muscle tone & activity
Chest, abdomen - respiratory effort, HR, bowel sounds
Reflexes
Safety - managing temp, ID pt, stable, transition to extrauterine life
Parental interaction & teaching - new parents? older kids, need refresher? breastfeeding education
What are some skin variations you may find in an H2T ax?
Mongolian spots - may be mistaken for bruising, document them well, bluish spots on lower back, buttock, upper outer thigh, common in dark skin/AA babies, may or may not go away
Vernix caseosa - thick white substance that protects skin when in the uterus, dealy bath bc it acts as a moisturizer
Stork bites - aka salmon patches, superficial vascular areas on nape of neck, eyelids or b/t eyes goes away in a year
Nevus flammeus aka Port-wine stain (permanent), will not fade with time, usually on face or head area, more to childhood CAs, best to treat (lighten w/ laser) before the age of 1
Acrocyanosis (⬇ APGAR score) - doesn't indicate cold temp, baby is getting adjusted to self-circulation
> cyanosis becomes an issue when it is central cyanosis, cyanosis of the head/around the mouth
Milia - unopened sebaceous glands on the nose, goes away in 2 - 4 wks
Epstein pearls -milia formed in the mouth, goes away in few moths
Erythema toxicum - benign papular-pustular rash, chest or back
Harlequin sign aka Clown suit - dilation of blood vessels on one side of the body, not common usually resolves itself
Nevus vasculosus aka strawberry mark/hemangioma - may darken, disappear by age 3
What are some head variations you may find in an H2T ax?
Overlapping sutures plates/molding/"conehead" - elongated head shape to accommodate birth canal
Cephalhematoma - Localized effusion of blood beneath the periosteum of the skull (does not cross suture lines)
- no tx, but ax it
- can contribute to jaundice bc there's more RBCs to breakdown
- caused by difficult birth
- may take weeks to months to resolve
- fills w/in the 1st few hrs of birth
- blood takes longer to be reabsorbed
Caput succedaneum -
Localized serous, soft tissue swelling
(crosses suture lines)
- like edema w/ pitting
- not associated w/ jaundice
- easier to absorb, take 3- 5 days to resolve w/ no tx
- not generalized to one side
- commonly observed after prolonged/ dificult birth/ labor
- may see petechiae, bruising
What are fontanels? sutures?
Fontanels - soft membranous
gaps between skull bones - should not be bulging or sunken may indicate hydrocephalus or dehydration respectively
Sutures - fibrous joints occurring
only in the skull
the anterior fontanel takes longer to close (12 mos.) than the posterior (2 mos.)
What reflexes do you assess during an H2T ax?
Sucking
Rooting
Moro aka starle reflex
Grasp (palmer + plantar)
Stepping
Babinski
Tonic neck (fencing reflex) "after you drink tonic you want to fight"
Truncal incurvation (Galant reflex) - disappears with 4wks, ventral suspension/prone, firm pressure down spine stroking will cause pelvis to flex towards stimulated side T2 to S1 innervation, lack of response indicates neuro or spinal cord problem
Gag & cough reflex - ax especially in head injuries
What are some newborn screening tests we perform in preparation for discharge?
FL state-required 53 disorder test screening via heel stick that includes galactosemia, SCD, thalassemia, PKU, congenital hypothyroidism
done 24 hours after the first feeding
hearing testing - most common disorder of NBs, all NBs are screened, parents may refuse
Critical Congenital Heart Defects (7 Complex
Congenital Heart Defects) - CCHD
> Pulse-ox readings of right hand & either foot
> Completed after 24 hours
What is included in discharge planning - education after birth?
- Car seat & crib - sizing, they should tolerate it w/out desaturating
- Never leave unattended on bed or sofa (may fall) - no loose sheets
- Choking hazards, toys from other siblings
- Hot bath water - r/f burning
- Co-sleeping - r/f asphixiation
- Sleep up to 15-20 hrs/day
- Sleep on back, no pillows or fluffy animals, pv SIDS
- No bottles in crib
- Cord care & bathing
- Diaper changes
- Feeding (breast or bottle)
- How and when to introduce solid
foods
- Elimination patterns
- Frequency & schedule of
pediatric visits
- Immunization schedule
- Recognize signs of illness
- How to take temperatures
- When to call the Healthcare
Provider (fever >100.4°F or 38°C) - high or low can indicate sepsis
What are some factors that can affect fetal development?
multifactorial
Fetal -
•Sex (males larger)
•Multiple gestations
•Anomalies/chromosomal defects - intrauterine growth retardation or spontaneous abortions
•Fetal infection (TORCH)
Placental - impacts supply of nutrients
•Calcification (aging) of the placenta, size/insufficiency, previa/abruption
Maternal -
•HTN, smoking, diabetes, weight gain, drug use
How can nurses identify newborns that may be at risks using variations in birthweight & gestational age?
Gestational age is inversely correlated w/ the r/f physical, neuro, dvlpmtal challenges, ⬆ maturity = ⬇ challenges
- Variations in BW or GA ⬆ neonatal risk factors
- Know how to ID NBs @ risk
- Classification methods:
- Birthweight
- Birthweight & gestational age
- Gestational age
___________________________
BW & Gestational age:
- AGA = appropriate for gestational age
- SGA = small for gestational age
- LGA = large for gestational age
BW (associated w/ premies:
- Low BW
- Very low BW
- Extremely low BW
What is considered an SGA, AGA, LGA baby?
AGA
•Weight is 10% - 90% for gestational age
•Lower morbidity and mortality rates
- generally, term NBs (38 - 42 wks gestation, 6- 8 lbs.)
SGA
<2500 g (5lbs 8oz) at term
•Weight is <10% for gestational age (growth charts)
LGA
>4000 g (8lbs 13oz) @ term
•Weight is >90% for gestational age (growth charts)
How would a small for gestational age (SGA) baby look upon assessment?
- Disproportionately large head
- Thin extremities and trunk
- Reduced subcutaneous fat stores
- Thin umbilical cord (less blood flow, less nutrients)
- Loose, dry skin
How would a nurse manage an SGA baby?
- Weight is generally 5 lbs, 8 oz or less
> Hypothermia - fewer glucose stores to provide thermogenesis, cold stress, they have even less fat
> Hypoglycemia - thin umbilical cord > less glucose from mom to fetus
> Polycythemia /Hyperbilirubinemia - ⬆ blood viscosity "sludge-like" leads to poor perfusion, compensation for low O2 & perfusion, trying to make more RBCs to ⬆ O2 *lab work, very red skin, respiratory distress, more RBCs breaking down > ⬆ r/f jaundice > may need their blood diluted w/ IV fluids or partial exchange transfusion
>>(hematocrit >65%, hemoglobin > 20 gm)
> Provide parental education
> On-going growth follow-up
What are some risk factors associated w/ an SGA baby?
Risk factors:
- Maternal smoking/drug use
- Genetics
- Multiple gestations
- HTN (mom's blood volume is mostly going to be used for mom & less going to baby)
- Maternal illness
What is Fetal Growth Restriction (FGR)?
- Pathologic counterpart of SGA
- @ risk for lifelong dvlpmtal deficits
- Failure to thrive in fetus
How would a large for gestational age (LGA) baby look upon assessment? Concerns? Risk factors?
- Weight is generally > 9 lbs
Risk factors
- Maternal diabetes mellitus, prolonged pregnancy, previous LGA baby, maternal obesity
Assessment findings
- Large body, appears plump, full-faced
- Head circumference/body length at upper limits
Nursing Concerns
- Traumatic birth injuries - shoulder dystocia, clavicle fractures, look for uneven moro response & one arm not being used, look crepitus over their clavicles may indicate fractures
- Hypoglycemia - due to ⬆ insulin > somatic growth, look for lethargy tachypnea, irritability, weak cry, jittery
-> usually born to diabetic mom
-Polycythemia/hyperbilirubinemia - may be caused by cord compression & ⬇ blood flow to the fetus > ⬇ O2 > ⬆ RBC production
How would a hypoglycemic neonate manifest?
- Blood glucose level <40 mg/dL
- 40+ = good
* hypoglycemia + hypothermia = married
Risk factors: maternal DM, prematurity, inadequate calorie intake, sepsis, asphyxia, hypothermia
Assessment:
-Listlessness/lethargy
- Weak cry, poor feeding
- Tremors, irritability
- Apnea
- Cyanosis
- HYPOTHERMIA!
Sometimes the way we notice the HR dipping > ⬇ temp
How would neonatal hypoglycemia be treated or prevented?
Treatment:
- Early recognition & intervention
- Immediate & frequent feedings w/in 1st hr
- Frequent glucose monitoring
- IV glucose for severe condition - bolus + D10W
Prevention:
- Early initiation of feedings
- Frequent ax of high-risk newborns
- NTE - thermoregulation
What are some general characteristics of hyperbilirubinemia (jaundice)?
2 types - mild & severe
- Most common reason for hospital readmission
- Results from imbalance in rate of bilirubin production & elimination (immature NB hepatic system)
- Essential data: age of NB (in hours) to determine rate of progression of condition, cause & tx
What is bilirubin & a neonates high r/f jaundice?
- Bilirubin is a byproduct of RBC hemolysis
- Bilirubin has 2 forms:
> unconjugated & conjugated
Unconjugated:
fat soluble, toxic to body tissues, unable to be excreted - ⬆ eating+drinking = ⬆ excretion
Conjugated: transformed by liver, water soluble, non-toxic, excreted in urine & stool
NB is @ high r/f jaundice:
> Immature liver unable to keep up with bilirubin production
> Fetal RBCs - shorter lifespan → faster break-down
> Delay in meconium excretion through bowel
⬆ prematurity = shorter RBC lifespan + ⬆ liver immaturity
What is a trancutaneous bilirubinometer?
- Like a thermometer, but it measure bilirubin levels through the skin
- Jaundice usually appears H2T & disappears in the same way
Jaundice spreads from skin > forhead > sclera
Blanch the skin (will blanch yellow)
What would an ax in a pt w/ potential physiologic jaundice include & how would you treat it?
Assessment:
-> Ax skin, sclera, body fluids for yellow color
-> Labs: polycythemia, Rh incompatibility (or ABO w/ pathologic jaundice), bilirubin, Coombs test (RBC antibody screening)
Treatment:
-> Promote early and frequent breastfeeding
-> Monitor serial bilirubin levels
-> Phototherapy (aka bili lights) care (can tx w/ indirect sunlight vitamin D):
- Eyeshield
-> NTE - frequent temperature monitoring
-> Strict I&O - daily weight - hydration ax
-> Monitor stool frequency & appearance
-> Positioning to maximize skin exposure
-> Meticulous skin care - no lotions
-> Parental support & education
take off lights for feedings
What's the difference between physiologic and pathologic jaundice?
PHYSIOLOGIC
-> Occurs in 60% of term & 80% preterm newborns
-> Occurs 1-7 days after birth
->Caused by shortened RBC life & immature liver
-> Levels usually peak at 10mg/dL then decline rapidly
PATHOLOGIC 5+ mg/hr Alarming!
-> Occurs in first 24 hours
-> Caused by severe polycythemia, blood incompatibilities (Rh-), or systemic acidosis
-> May reach toxic bilirubin level > 17mg/dL
-> Kernicterus → Encephalopathy
What is pathologic jaundice - hemolytic disease of the newborn (HDN)?
- First 24 hours
Rh incompatibility (Isoimmunization):
-> Mother is Rh - & baby is Rh +
-> Mother's anti-Rh antibodies (initially IgM) do not cross placenta - repeat encounter will produce IgG antibodies that do cross
-> Effects subsequent pregnancies
ABO incompatibility:
-> Mother is type O & baby is A, B, or AB
-> Mother's anti-A & anti-B antibodies (IgG) attack baby's RBCs by crossing placenta
-> Less serious rxn
-> Can happen in 1st baby
-> Doesn't get more severe in subsequent pregnancies
How would hyperbilirubinemia be managed by the nurse?
- Phototherapy
- Parental education
- Exchange transfusion
- Counseling for future pregnancies
What would a nurse find upon assesment if the newborn had an infection?
- Hypothermia, inability to regulate temp - can't mount fever response to infection
- Pallor or duskiness
- Hypotonia
- Poor weight gain
- Respiratory distress
- Irritability
- Hypoglycemia (late sign)
- Seizures (late sign)
"SHHH I P Pd Rd"
More lines, more site for infection
Signs of sepsis are subtle
What is neonatal sepsis and how does it present?
Neonatal Sepsis
- Presence of bacterial, fungal, or viral microorganisms (or toxins) in blood or other tissues - most common Group B Strep - early onset sepsis, onset birth to 1 wk, infection from birth canal
- Presents as: septicemia, pneumonia, meningitis
- Congenital infection - present @ birth, infection directly from the mother, TORCH, contracted in utero
- Late-onset sepsis - onset beyond 1 week, maternal or external source of infection
- 50% mortality rate in untx
What are TORCH infections?
TORCH infections- group of infections acquired perinatally
- Toxoplasmosis - infected cat feces
- Other (Gonorrhea[erythromycin], Syphilis[if infected antibiotics, if tx before birth they will not likely stay there], HIV, Chlamydia) STIs via birth canal, tx mom, r/f blindness
- Rubella (leads to miscarriages)
- Cytomegalovirus (miscarriages, FGA, hydrocephaly stillbirth)
- Herpes Simplex Virus (c-section if active, otherwise if there's no lesions > vaginal birth is ok)
How are newborn infections managed by the nurse?
Early recognition & tx treatment
- Antibiotic tx - monitor response
-> 7 - 21 days for positive cultures (blood, urine, spinal tap bc it may be meningitis)
-> 72 hours until neg cultures
- Supportive care: oxygen PRN, pain control
- Promote hydration - po/IV fluids, inotropes
- Prevention: handwashing, aseptic wound care, frequent monitoring of invasive catheter sites, identifying risk factors, family education
What is Transient Tachypnea of the Newborn (TTN)? What are the risk factors for it?
- gradual onset
- risk factor is c-section bc they don't get the thoracic squeeze
- Self-limiting respiratory disorder
- Mild respiratory distress
- Cause: retention of fluid in lungs or transient pulmonary edema
- Fluid in fetal lung eliminated slowly or incompletely
- Occurs within a few hours of birth, resolves by 72 hours
- Risk factors: cesarean birth, prolonged labor, male, maternal asthma, fetal macrosomia, maternal meds
What would a nurse find upon assessment of a newborn w/ TTN? How would a nurse treat it?
CXR - will see hyperairation
Assessment: retractions, expiratory grunting, cyanosis
"REC", usually normal pH, mild hypoxemia
Treatment: supportive
- Supplemental oxygen
- Frequent assessment
- Thermal regulation and NTE
- IV fluids or gavage feedings until stable respiratory status
Airway before feeding in terms of priority
usually NPO until ⬆ respiratory status
What is considered a preterm newborn?
- born before completion of 37 weeks (<38 weeks)
Prematurity is the 2nd leading cause of NB death
-> 2nd only to congenital defects
What are the effects of prematurity on a newborn?
Respiratory → Chronic Lung disease; O2 use can cause retinopathy of prematurity
-> infants chest wall is unstable. doesn't have the musculature
-> respiratory control center not dvlpd leading to apnea
-> they can outgrow some of their respiratory issues, depends on severity
-> retinopathy can lead to blindness
-> surfactant deficiency can lead to respiratory distress syndrome = RDS is a syndrome specific to premies w/ ⬇ surfactant, starts production @ 24 wks and completes it @ 34 wks
-> generally respiratory distress simply means the baby is not breathing well
Cardiovascular → persistent fetal circulation; anemia
-> hypoxia
-> happens bc areas in the ❤ that need to close do not
-> impaired BP regulation > ⬆ r/f intracranial pressure
Gastrointestinal - Uncoordinated suck, swallow
-> Shunting of blood to vital organs; NEC - due to ⬇ blood flow to intestines > bacterial infection in the intestines
-> require enteral/parenteral feedings until they coordinate breathing & swallowing
Renal → decreased GFR
-> fluid retention
-> caution! fluid overload
-> electrolyte imbalance > ⬆ r/f toxicity
Immune → IgG deficiency; infection, septicemia
Central Nervous System
-> Mental/motor/developmental delays
-> Intraventricular hemorrhage (IVH)
-> trouble w/ thermoregulation
-> issues w/ hypoglycemia > dvlpmtal delays
What is the foucs of a preterm NB ax?
Ballard Scale -
- Physical characteristics: (assessed w/ in 1st 2 hrs of life)
-> Skin - transparent, minimal subcutaneous fat; plentiful vernix caseosa
-> Lanugo - sparse
-> Plantar creases-absent to few on soles & palms
-> Breast tissue - not developed
-> Eyelids fused, poorly formed ear pinna
-> Genitals - undescended testes/clitoris prominent
- Neuromuscular characteristics - poor muscle tone and flexion, increased flexibility - minimal resistance when performing neuromuscular assessments
- General - scrawny appearance, head disproportionately larger than chest
-> flexed = term neonates
-> assessed w/in 1st 24 hrs as long as neonates is stable
What is included as routine NICU care?
- Continuous cardiac and respiratory monitoring
- Neutral thermal environment (NTE) - isolettes
- Low stimulation - cluster care "feed & grow", q6hours for care
- Fluid management, I&O, daily weights
- Nutritional support; glucose level maintenance
- Infection prevention
- Handwashing
- Screening visitors
- Prone position (increases resp, decreases stress)
- Parental education and participation in care
How are preterm NBs managed by the nurse?
Promote oxygenation
-> Identify asphyxia - prepare for resuscitation
-->> ask when is your date in order in order to ID r/f respiratory issues
-->> risk determined @ birth
-> Administer oxygen (judiciously) to maintain p/ox from high-80s to mid-90s
-->> high O2 can cause retinopathy
-> Monitor respiratory status and airway patency
-> Administer medication (surfactant)
Maintain thermoregulation
-> Radiant warmer, isolette, kangaroo care, if stable
-> Promote nutrition and fluid balance
-> Monitor daily weight, strict I&O/calorie count
-> Encourage breastfeeding/use of maternal breast milk
--> mom is encouraged to pump
Prevent infection (low temp, temp instability = 1st sign of infection)
-> Monitor changes in vital signs and pulse-ox
-> Protect skin (skin is fragile)
-> Screen visitors (limit them)
Provide appropriate stimulation
-> Rocking, swaddling, sucking, massage, holding
-> Promote growth and development
-> Alter NICU environment; cluster care
Manage pain (sedation)
Promote parental coping
-> Validate feelings
-> Encourage frequent visits
-> Identify family and community resources
After 34 weeks, when they can coordinate suck & breathing/swallow then we can address potential dvlpmtal delays
What are the benefits of kangaroo care?
How are preterm newborns prepared for discharged?
Prepare for discharge
-> Provide parental education
-> Teach infant CPR and emergency care (sx to look for)
-> Develop appropriate home care environment (social work)
-> Establish a medical home and referrals
-> Initiate primary care routine
-> Celebrate progress and milestones! (expect the neonate/NB to reach late milestones anticipatory guidance)
How can a nurse help parents deal with perinatal loss?
Assisting parents to cope
-> Convey concern and acknowledge parental loss
-> Use active listening
-> Give parents a sense of control
-> Provide privacy as needed
-> Assist parents to make memories (hand/footprints)
-> Respect and incorporate cultural interventions
-> Help family with grieving process
Supporting the family afterwards
give them all the time they need
death during pregnancy - up to 1 month after birth
What is respiratory distress syndrome (RDS)? Risk factors? Assessment?Treatment?
Disorder from lung immaturity and lack of surfactant
Risk factors: preterm, maternal Diabetes Mellitus
Assessment: Grunting, nasal flaring, retractions, increasing atelectasis and cyanosis
Treatment: supportive
-> PEEP ventilation (weened of vent)
-> Administration of exogenous surfactant therapy
-> Mechanical ventilation if needed
-> Prevention: single dose betamethasone
-->> ID due date in order to admin betamethasone to mom. be proactive
What are the effects of mechanical ventilation on preemies?
Bronchopulmonary Dysplasia (BPD)
•"Chronic Lung Disease" - neonates treated with mechanical ventilation and oxygen > 28 days
-> lung damage, gets better as they grow
•Results in fibrosis, atelectasis, increased pulmonary resistance, decreased lung compliance, pulmonary hypertension & edema
•Medications: bronchodilators, corticosteroids, diuretics
Retinopathy of prematurity (ROP)
•Separation/fibrosis of retina, can lead to blindness (caused by high O2 levels)
•Damage to immature retinal blood vessels thought to be caused by high oxygen levels or low birth weight (low 90s)
•Prevention: vitamin E, avoid high concentrations of oxygen
•Cryosurgery may reduce long-term complications
ween O2 asap
What are some characteristics of term NBs?
- 38-42 weeks
- Less morbidity and mortality
- Best outcomes
- Best ability to deal with stressors
- Still require much education
- Adaptation of family
What are some characteristics of postterm NBs?
- At or beyond 42 weeks
- Risk factor: prior post-term infant
- Placental issues occur:
- Decreased oxygen and nutrient supply
- Wasting of fetus due to using stored nutrients
placenta starts to calcify over time
What is the focus of postterm NB ax?
Ballard Scale -common physical characteristics
- Skin - dry, cracked, peeling, wrinkled
- Lanugo - absent, minimal vernix caseosa
- Plantar creases - cover the entire soles of feet
- Breast tissue - measureable
- Eyes - fully developed, ears firm and stand away from head
- Genitals - creases on scrotum, descended testis, labia majora covers labia minora
- Neuromuscular characteristics: increased flexion and resistance to range of motion; less flexibility
- General - abundant hair on scalp, thin umbilical cord, meconium-stained skin/nails; longer nails
How are postterm NBs managed by the nurse?
- Anticipate newborn resuscitation - check respirations, ABGs
- Monitor blood glucose levels
- Prevent hypothermia
- Screen for polycythemia & hyperbilirubinemia (physiologic jaundice over time, ⬇ O2 > RBC production)
What is meconium aspiration syndrome? RFs? Ax? Tx?
Inhalation of meconium-filled amniotic fluid (thick tarry stool)
Risk Factors: post-term pregnancy, maternal DM, prolonged labor; breech presentation, forceps or vacuum-assisted births,, maternal smoking or drug abuse
Assessment: tachypnea, respiratory distress, grunting, cyanosis, uneven pulmonary ventilation
Treatment: (if mom comes in w/ ROM, what color is?)
-> Assess for green-stained amniotic fluid
-> Hyperoxygenation or oscillatory ventilation (dilation pulmonary vasculature)
-> Pulmonary vasodilators and surfactant PRN
-->> Aggressive suction > intubation
-->> CXR shows infilitrate + hyperairation
-->> atelectasis
-> Acidosis, pH changes, acidotic
- diluted meconium may not be as big of an issue
- in severe cases may need to be can nitrous oxide or ECHMO/life support
What is perinatal asphyxia? RFs? Tx? Complications?
- Respiratory distress
- hypoxemia
- acidosis
- bradycardia
Inability to successfully transition to extrauterine life
-> Perinatal acidosis
-> Most common clinical insult in perinatal period
Risk factors:
-> Birth trauma
-> Intrauterine asphyxia (cord compression, maternal HTN) -->> come out blue/ not breathing
-> Meconium aspiration
-> Sepsis
-> Malformation (congenital anomalies)
-> Hypovolemic shock (from abruptio, cord rupture)
- Early ID of risk, early recognition of symptoms, early intervention = improved perinatal outcomes
- 10% require active resuscitation attempts:
-> Dry newborn quickly, place under radiant heater
-> Suction nose/mouth
-> Begin resuscitation procedure
-> Continue until newborn has pulse >100 with good respiratory effort and pink tongue
Complications:
-> Cerebral palsy (was the cord around the neck?), mental retardation, speech disorders, hearing and/or visual impairment, and learning disabilities
What is macrosomia (LGA)? What are the concerns associated with IDM - LGA?
Macrosomia (LGA) - due to maternal hyperglycemia and fetal response of hyperinsulinemia which leads to somatic growth
Nursing Concerns:
Hypoglycemia
Birth Trauma - injury occurring during birth (shoulder dystocia/clavicle fractures)
Respiratory Distress Syndrome (RDS) - ⬆ insulin levels inteferes w/ surfactant production
Polycythemia & hyperbilirubinemia
Hypocalcemia (tremors, hypotonia, apnea, high-pitched cry, seizures) - cord compression, hypocalcemia
What are characteristics of IDM?
Characteristics of IDM:
•Distended abdomen
•Wide shoulders
•Rosy cheeks
•Excessive subcutaneous fat on extremities
•Short neck
What is Fetal Alcohol Syndrome?
FETAL ALCOHOL SYNDROME (FAS)
-> there's no screening for this
-> severe end of spectrum
•Effects: growth restriction, craniofacial structure malformations, CNS dysfunction
•Clinical features: delayed motor development, dysmorphic facial features, cognitive/developmental dysfunction, growth restrictions, kidney defects
What is FASDs?
•Fetal Alcohol Spectrum Disorders (FASDs)
-> "don't drink at all"
-> pattern of fetal anomalies r/t alcohol abuse
•Prenatal alcohol use
•Effects: developmental/cognitive/behavioral disabilities
•Birth defects - commonly heart, kidneys, bones
•No safe level, life long, affects 40,000 newborns/yr
What are some characteristics of FAS?
Clinical findings:
*Microcephaly (small head > small brain)
*Low nasal bridge
*Small eyes
*Fetal Growth Restriction
Thin upper lip Delayed motor skills
Missing philtrum Mental retardation
Narrow forehead Cardiac defects
*Micrognathia (small chin/jaw)
*Poor eye-hand coordination
dx criteria:
- must have @ least 3 of facial abnormalities
- < 10% percentile for growth
- CNS abnormality - microcephaly OR documented dvlpmtal delay
What are the effects of opioids on newborns?
- Opioid receptors are concentrated in CNS and GI tract
- Signs and symptoms of withdrawal:
-> CNS irritability - may last for 7-8 months
-> Autonomic over-reactivity
-> Gastrointestinal tract dysfunction
How is a newborn with Neonatal Abstinence Syndrome (NAS) assessed? What are the types of s/s found?
Assessment:
-> Review maternal history and risky behaviors
-> Obtain urine, blood, meconium toxicology screens
-> Assessment tools
-->> Finnegan NAS scoring system
- S/S withdrawal disturbances in the:
-->> Central Nervous System
-->> Metabolic vasomotor/respiratory, systems
-->> Gastrointestinal system
What is the NAS scoring system?
- most commonly used; should be done after feedings when the infant is awake
-->> The higher the score, the greater the opioid effects/withdrawal effects
How is an NB w/ NAS managed by the nurse?
- Promote comfort
- Low stimulation, low lighting (quiet, calm, no loud noises)
- Swaddle, pacifier, calm approach
- Meet nutritional needs
- Frequent small feedings
- Benefits of breastfeeding for the baby are good, even with Mom in treatment/i.e. methadone
-Strict I&O, daily weight
- Prevent skin breakdown, weight loss, dehydration
- Administer meds based on NAS scores (>8)
-->> Opioid (morphine, buprenorphine or methadone)
-->> 50-80% of infants get pharmacological management
-->> Phenobarbital to control breakthrough symptoms
- Promote parent-newborn interactions, educate & refer
What are the long-term outcomes of NAS?
- Poor cognitive, perceptual and memory skills
- Hyperactivity and impulsivity
- Short attention span
- Poor verbal and performance skills
- Vision and hearing problems
- At higher risk for child abuse and neglect
- Risk for future substance abuse
- Sleep disturbances
* r/f abuse due to the high pitch cry
What are some GI variation in pediatric children?
GI tract is immature until about 2 years old
GI tract includes all structures from mouth to anus
- Primary functions are digestion and absorption of nutrients and water
- Elimination of waste products
Mouth - common portal of entry for infections
- Bc of their behaviors, everything they find/pick up will go in their mouths
Esophagus
- Bottom of esophagus is the lower esophageal sphincter (prevents backflow of stomach content into esophagus)
- In children there's an ↑ incidence of reflux and can last until about 1, bc the sphincters muscle tone is underdeveloped
Stomach - small at birth and will continue to grow
- At birth can only hold about 1 ounce of fluid
- By 2 months, can hold about 2 ounces
- Hydrochloric acid levels don't mature until about 6 months of age
- Pyloric sphincter (allows partially digested food into small intestine)
Intestines - smaller and still growing
- Less than half of what it will be as an adult
- Removal of part of the intestine can accuse lifelong problems with absorption
Liver and pancreas are not apart of the GI tract but contribute to the breakdown of nutrients
- Liver is a little larger at birth - may be able to palpate - functionally immature
- Pancreas - pancreatic enzymes which help break down food don't reach adult level until about 2 years of age
What is included in a GI nursing assessment? (health hx, dx testing)
Health history
- Growth patterns - what percentile for weight height?
- Dietary concerns - feeding issues?
- Toilet training and bowel patterns
- Patient history - medical/surgical issues r/t GI tract
- Family history
Diagnostic testing:
- Esophageal pH probe - to determine if they have gastroesophageal reflux
--->>> Probe down nose, placing at the bottom of the esophagus, not quite into the stomach (above esophageal sphincter)
--->>> Xray to ensure correct placement and will be left in for 24 hours
--->>> Will go from basic to acidic every time there's stomach reflux up into esophagus - then looks at 24 hour data to see how many times it occurred
- Ultrasound (abdominal) - if there's issues of pain/mass
- KUB
- Barium studies - only for imaging test for GI tract
--->>> Barium swallow: to see how esophagus is doing, if there's any aspiration
--->>> Upper GI with small bowel follow through or barium enema if you need to see large intestinal structures
--->>> After use of barium, important to encourage a lot of water because if caught in system it can cause more constipation
- Stool studies
--->>> Hemoccult - blood in stool
--->>> Cultures: O&P - test for ova and parasites
What is included in a GI assessment? (physical exam)
Physical Exam:
Inspection & Observation
- Abdominal size and shape - should be soft, non tense
- Look at abdominal musculature
- Paleness? Could indicate GI bleed or jaundice indicating liver issues
- Protuberance could mean gaseous distention occuring
- Depressed abdomen could mean an obstruction/dehydration
- May observe umbilical hernia - not uncommon because musculature is still weak so intestines may poke out some. Should be able to be pushed back in
Auscultation - always listen before palpate/percuss
- Listen in all 4 quadrants - hypo/hyper/normal sounds?
Percussion
- Usually tympany over most of abdomen
- May be dull sounds over organ or colon full of stool
Palpation
- Lightly first, assess for tenderness (would be abnormal)
They do need to be as relaxed as possible, it's invasive for them to have someone lift up their shirt
They also could be ticklish/tense which can make their abdomen seem more firm
Could have issues with dehydration - should note general appearance like mental status, are they lethargic?, recent weight gain/loss, needs to be addressed first
What is cleft lip and cleft palate?
Cleft Lip and Palate - common congenital craniofacial anomalies
Pathophysiology
- Develops early on in gestation - form around 5-9 weeks of life
- Could have unilateral (more common) or bilateral
Complications
- Potential for aspiration, feeding difficulties
- Altered dentition
- Greater risk for ear infections
- Could have long term issues which speech and language development
Medical Management - multidisciplinary approach
- Surgeons/nurses/ENT specialists
- Language/speech pathologists
- Orthodontist
- Geneticist is associated with another syndrome
- Social worker to help family navigate what they will have to go through
Cleft lip is repaired first and earlier at around 3-6 months of age
Palette not usually done until 6-12 months of age - ideally before they are learning to talk
What is included in the nursing ax of cleft lip/palate?
Risk factors
- More common in males
Health history
Physical exam
- Can often be seen in US but if not, upon delivery
- If not cleft lip deformity, the palette will be checked upon examination in 1st assessment - they'd be able to palpate the defect
- Another sign is baby choking, gagging, aspirating during first feed
Family education
- Kids will go home with assist devices for feeding
- Family should know CPR in case of aspiration
What is included in the post-op nursing care of a cleft lip patient?
C - Calming techniques - prevent crying to avoid suture pulling
L - Lie on back - so they can't rub lip on something
E - Evaluate airway
F - Feeding - special feeders, still have cleft palate
T - Teaching
L - Lip protection (Logan bow) - tape and metal bar (added protection)
I - Infection - clean site daily (don't want crust to form) apply vaseline
P - Parent bonding
- Arm restraints used continually for the first 10 days, can take off a little bit every few hours (maybe one side at a time) if you are there for direct supervision
- Around the clock pain management
For cleft palate:
- Most of the same interventions, but will be more painful
- Since we are working in mouth, we worry about swelling at back of throat
- For the first 3 weeks after cleft palate repair, goal is to protect the suture line at top of mouth. These pts will be on liquids for 1st 2-3 weeks, use spoon to feed
-> Can introduce soft things baby 2nd week, nothing too hot or hard (applesauce, pudding, baby food, etc) and water after to clean palate
- Arm restraints to avoid them touching or getting hands in mouth
What is acute hypertrophic pyloric stenosis?
Disease in which babies stomach is blocked or abnormally narrow
Pylorus becomes hypertrophied - muscle grows to large
Stenosis of the pyloric sphincter - none of the food/milk from stomach can't get to small intestine - this causes them to forcefully vomit it up (can cause dehydration)
- Dehydration symptoms
--->>> Sunken eyes
--->>> No tears while crying
--->>> Sunken soft spot
--->>> Less urine (or brown/dark yellow)
Leads to obstruction
Will need pyloromyotomy a month or two after birth, once discovered
What is included in the nursing ax & management of a hypertrophic pyloric stenosis pt?
Risk Factors
- More often males than females
- Family hx common (usually dads)
Health history and symptoms:
- Non-bilious emesis 30-60 minutes after feeding
-> Because with the sphincter preventing the food from getting to intestine, it will only be the food coming back up
- Hungry and crying despite having been fed - they are throwing it all up
- Progressive weight loss
Physical Exam:
- "Olive shaped" mass in upper abdomen - the thickening muscle
- Progressive dehydration
Fluid and electrolyte management
Parental education
Pre & Post-op care
Resume feedings
What is intussusception?
Bowel telescopes into a distal segment
- Folds in on itself, could be edema or imparied circulation
-> Edema and impaired blood circulation
-> Partial or total bowel obstruction
Occurs in children < 2, they can't really tell you what's happening/how they feel
If there is lack of circulation to the intestine before parents realize what's going on, that portion of the bowel may die and need to be removed
In order to diagnose it, air emena is usually done - which can also allow the telescoped bowel to pull itself out. If not, surgery will be needed
What is included in the nursing ax of a pt with intussusception?
Sudden onset intermittent pain
- Babies will often pull up legs when in pain
- Bilious emesis - will have bile in the emesis
- "Currant jelly" stools - mucus and blood mixed
Physical exam
- Lethargy
- "Sausage"-shaped mass
Emotional support