Chapter #10 Muscle Tissue (copy)
1/81
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
82 Terms
Skeletal Muscle
This tissue is packaged into skeletal muscles, organs that are attached to bones and skin.
Skeletal muscle fibers are the longest of all muscles and have striations (stripes)
Also called voluntary muscle: can be consciously controlled
Contract rapidly; tire easily; powerful
Keywords for skeletal muscle: skeletal, striated, and voluntary

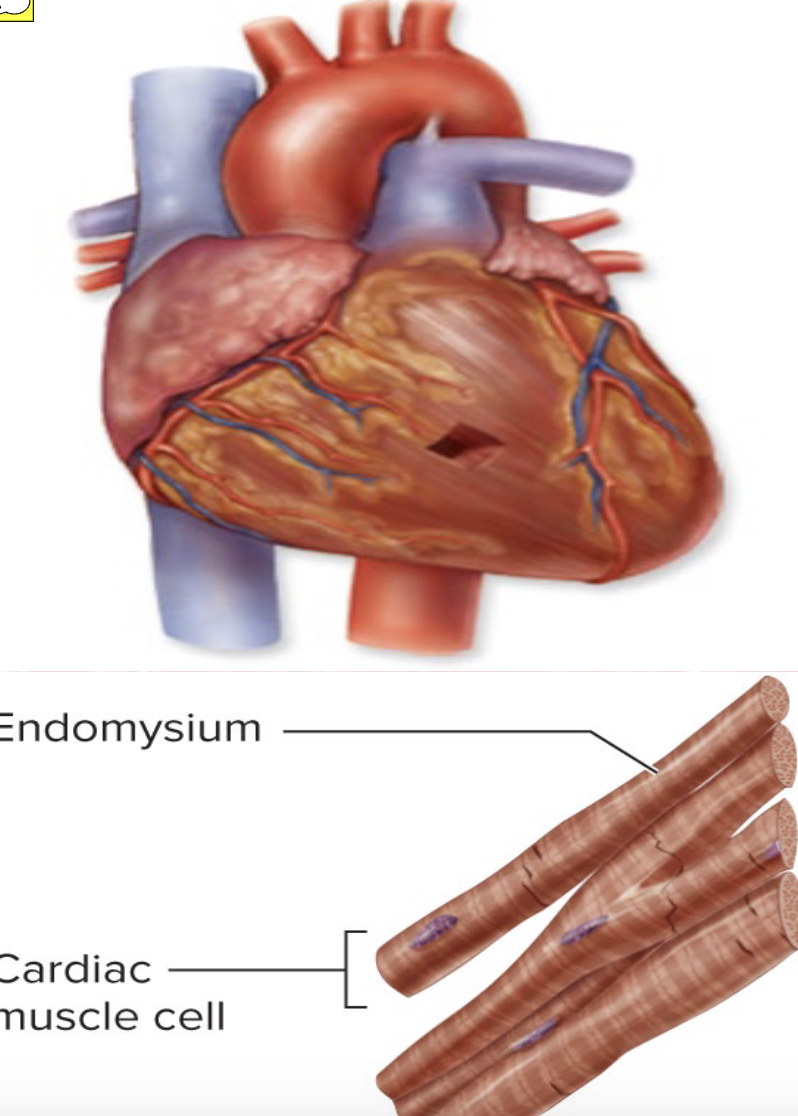
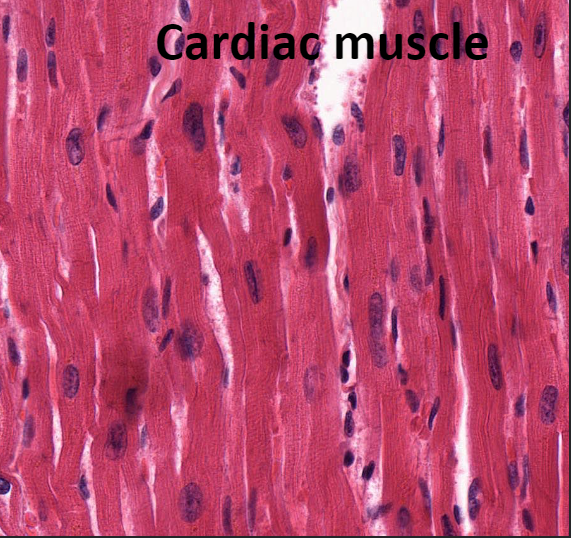
Cardiac Muscle
This tissue is found only in heart
Makes up bulk of heart walls
Striated
Involuntary: cannot be controlled consciously
Contracts at steady rate due to heart’s own pacemaker, but nervous system can increase rate
Key words for cardiac muscle: cardiac, striated, and involuntary

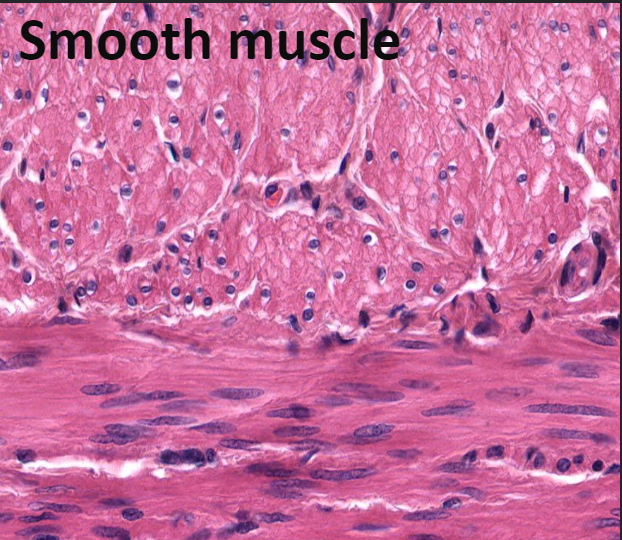
Smooth Muscle
This tissue is found in walls of hollow organs
Examples: stomach, urinary bladder, and airways
Not striated
Involuntary: cannot be controlled consciously
Key words for smooth muscle: visceral, nonstriated and involuntary
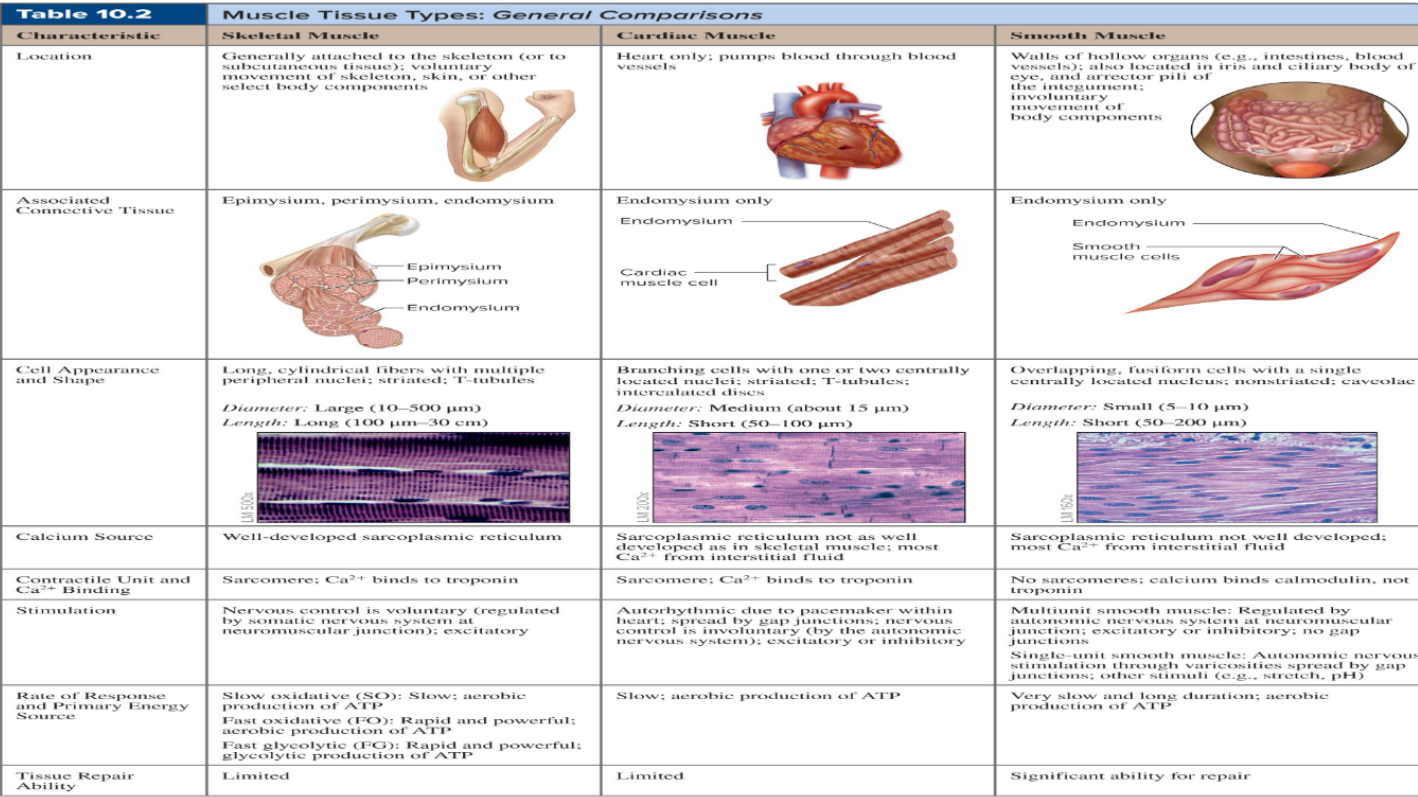
Muscle Tissue Comparisons
Skeletal Muscle ( Explained)
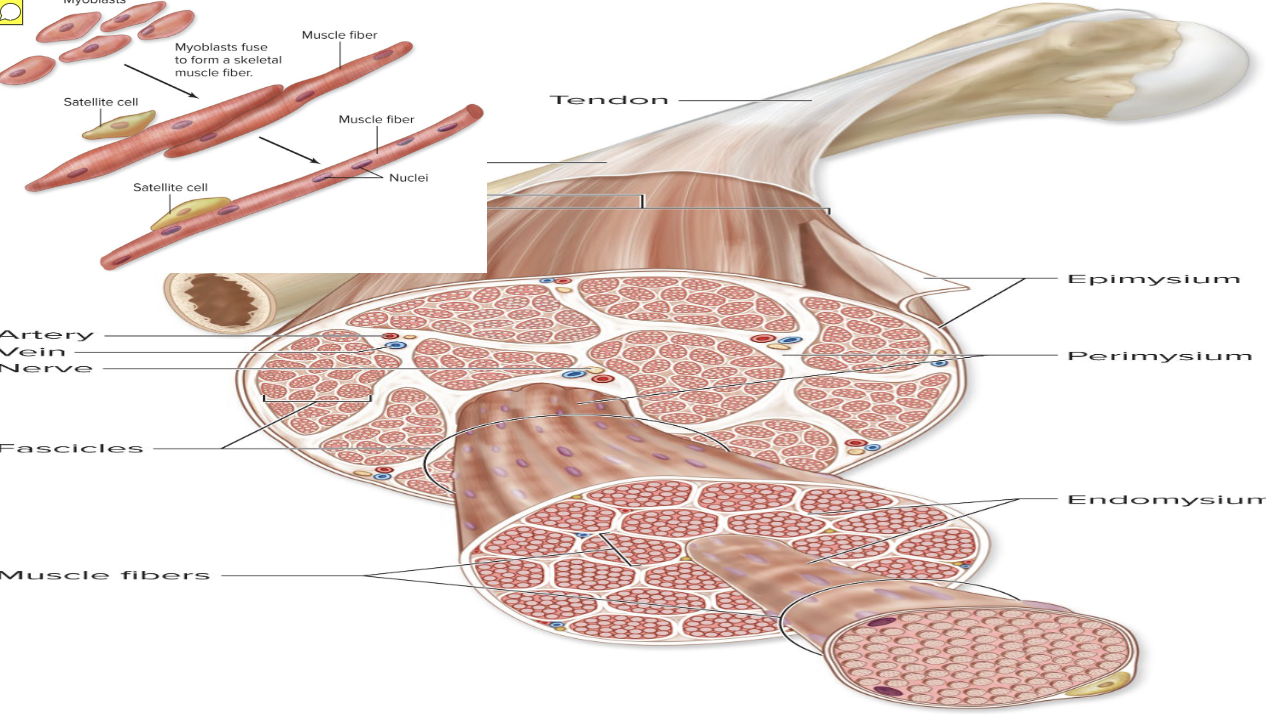
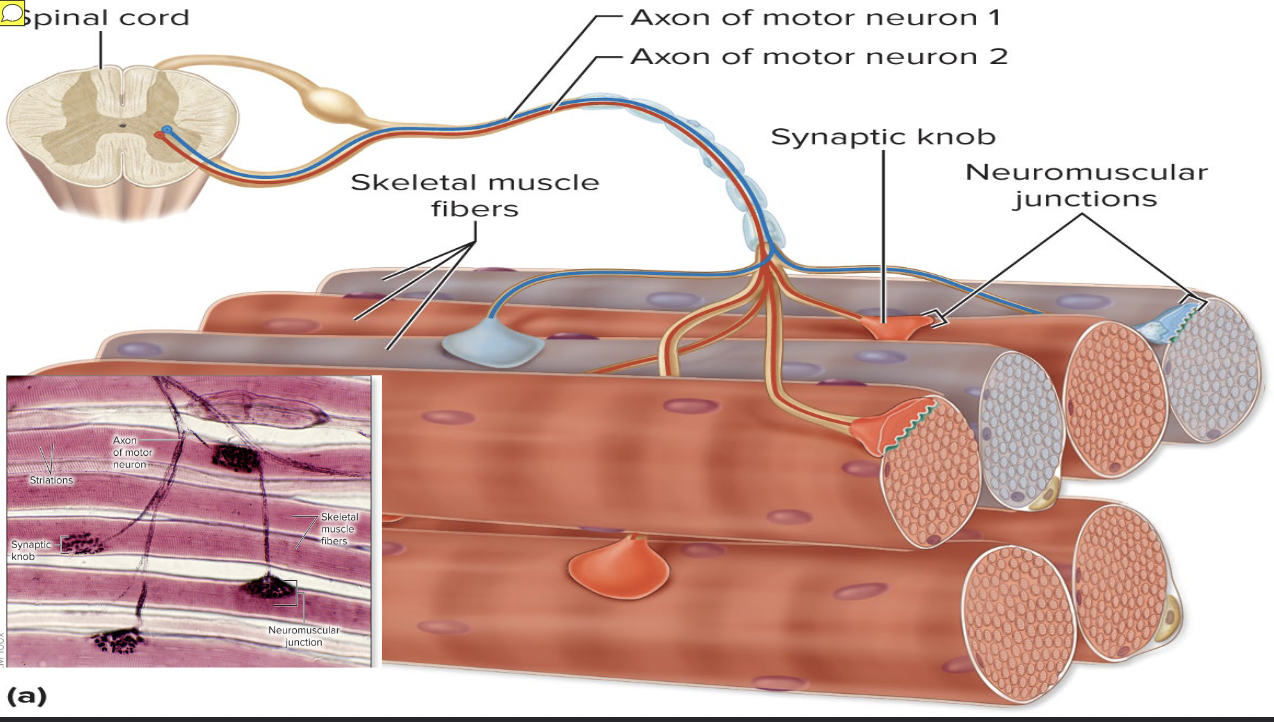
Skeletal muscle is an organ made up of different tissues with three features: nerve and blood supply, connective tissue sheaths, and attachments
Each muscle receives a nerve, artery, and veins
Consciously controlled skeletal muscle has nerves supplying every fiber to control activity
Contracting muscle fibers require huge amounts of oxygen and nutrients
Also need waste products removed quickly
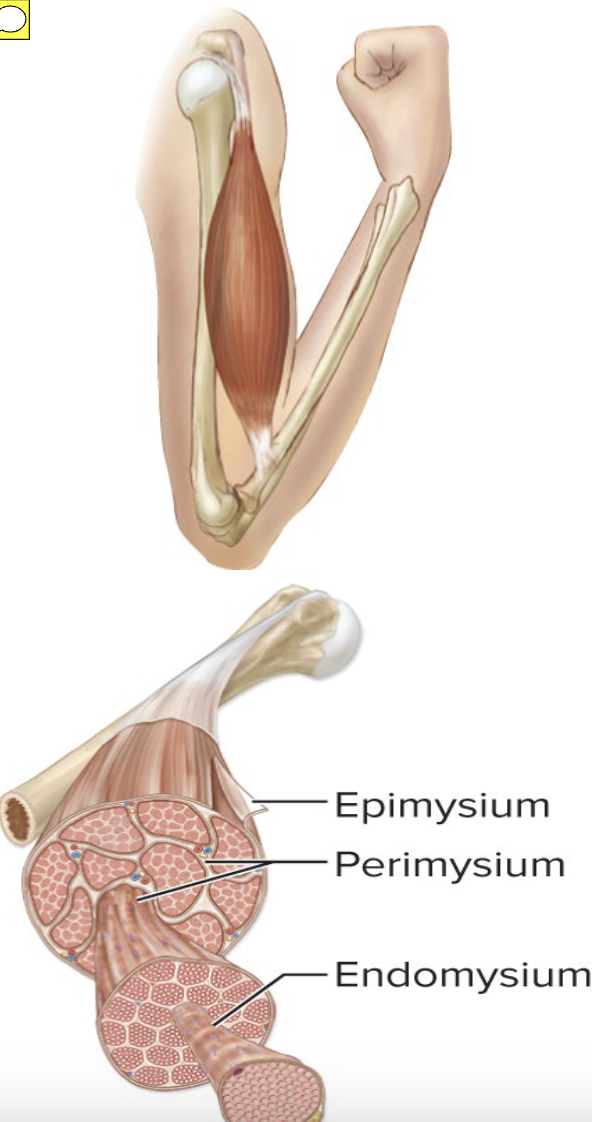
Each skeletal muscle, as well as each muscle fiber, is covered in connective tissue
Support cells and reinforce whole muscle
Sheaths from external to internal:
Epimysium »Perimysium»Endomysium

Epimysium (skeletal muscle)
dense irregular connective tissue surrounding the entire muscle; may blend with fascia
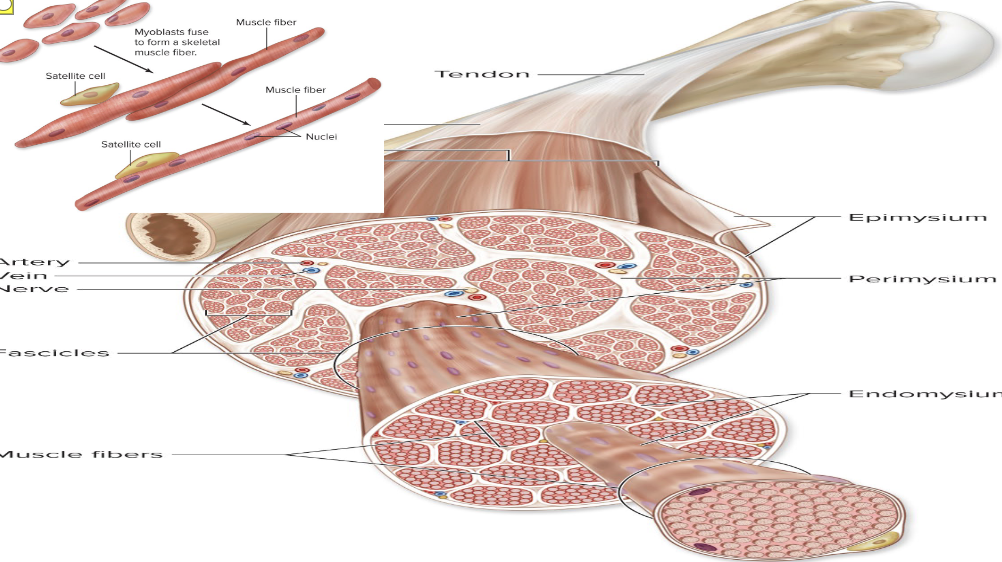
Perimysium (skeletal muscle)
fibrous connective tissue surrounding fascicles (groups of muscle fibers)
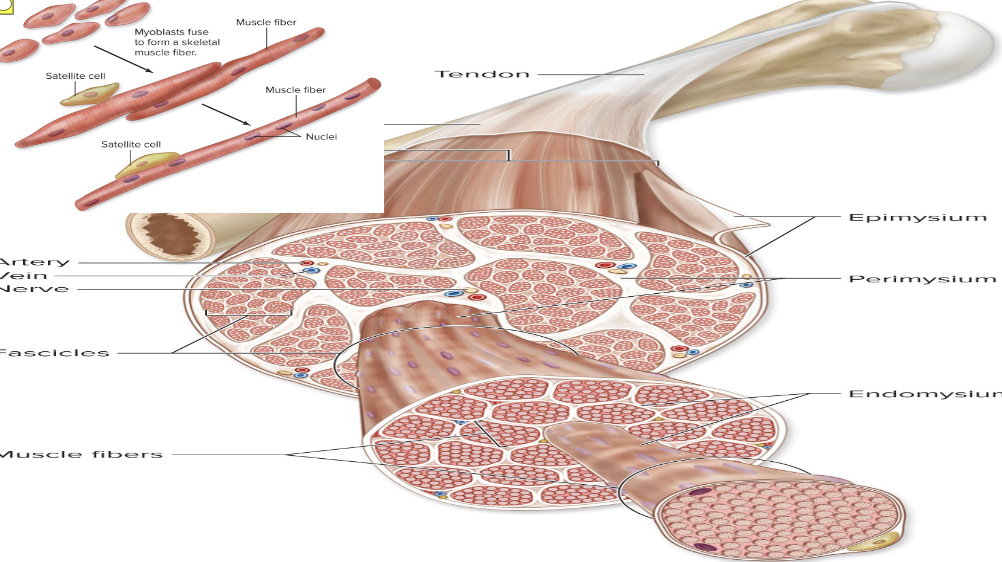
Endomysium (skeletal muscle)
fine areolar connective tissue surrounding each muscle fiber
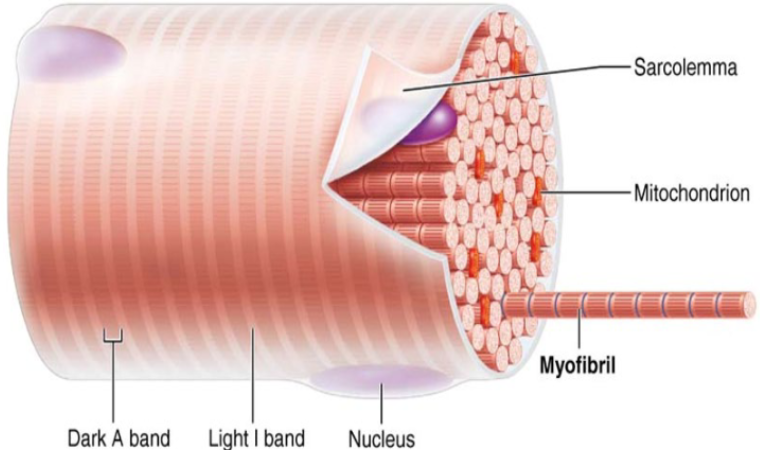
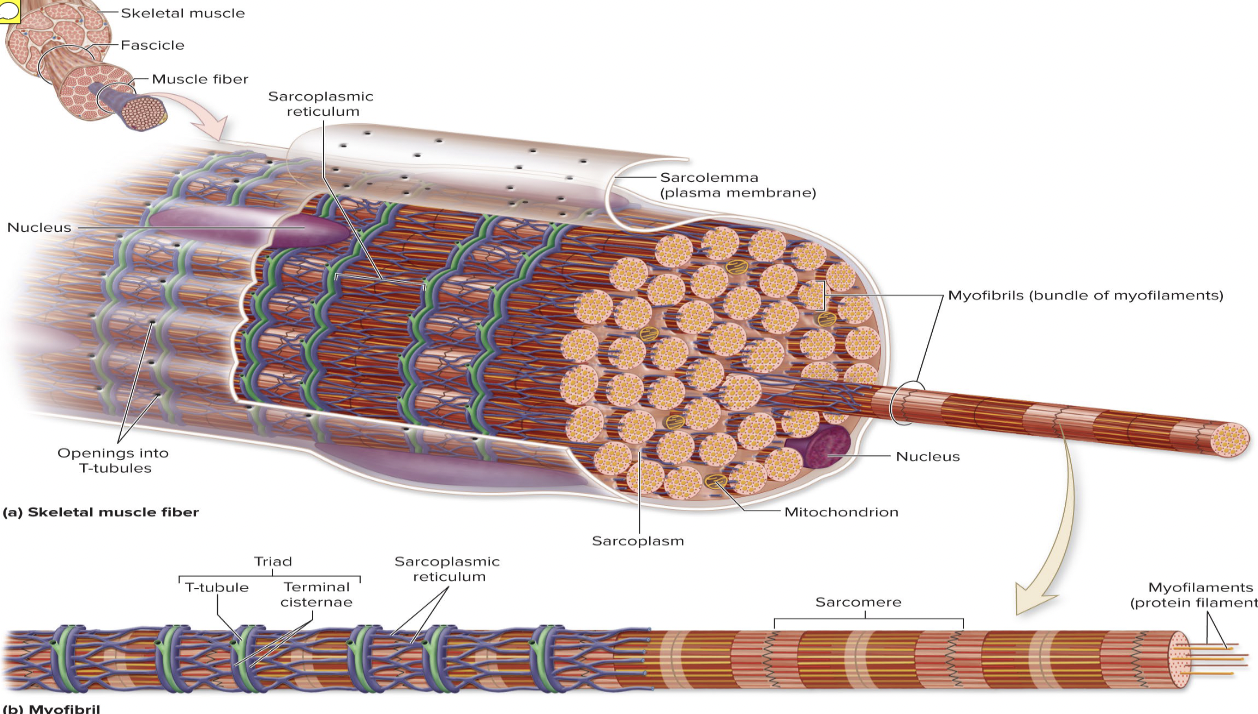
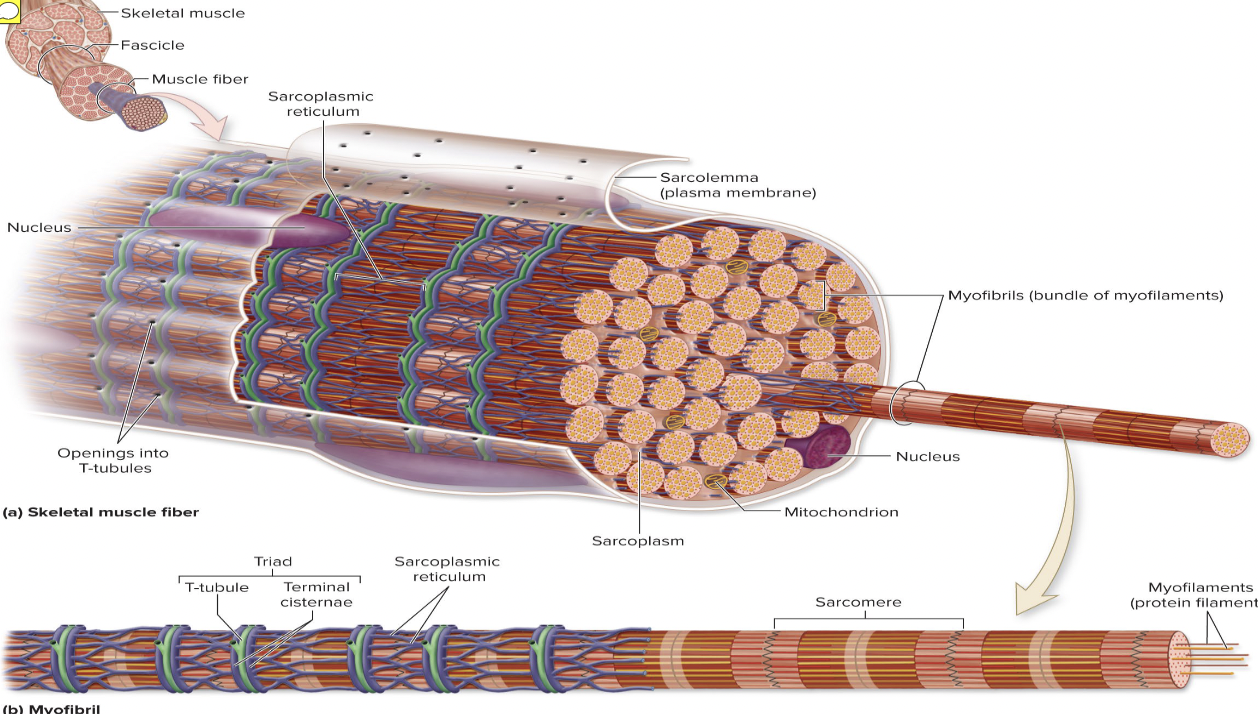
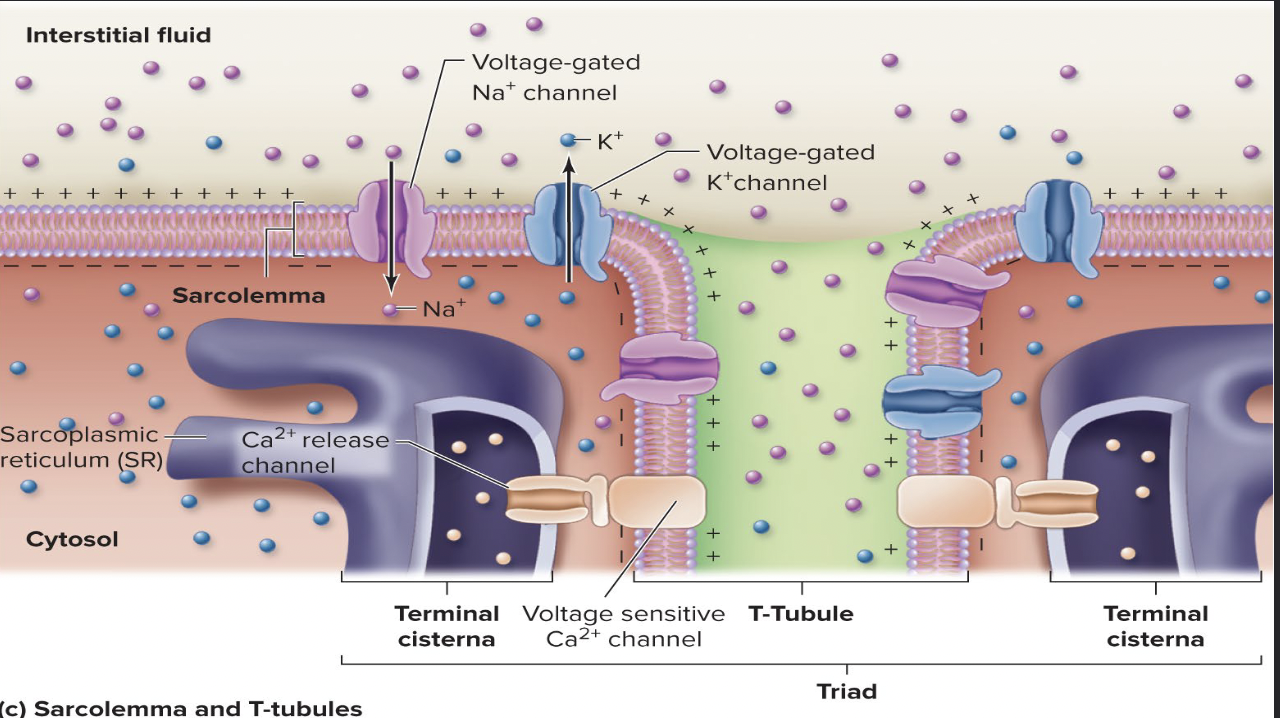
Sarcolemma (Skeletal Muscle Fiber Microanatomy)
muscle fiber plasma membrane
Sarcoplasm (Skeletal Muscle Fiber Microanatomy)
: muscle fiber cytoplasm
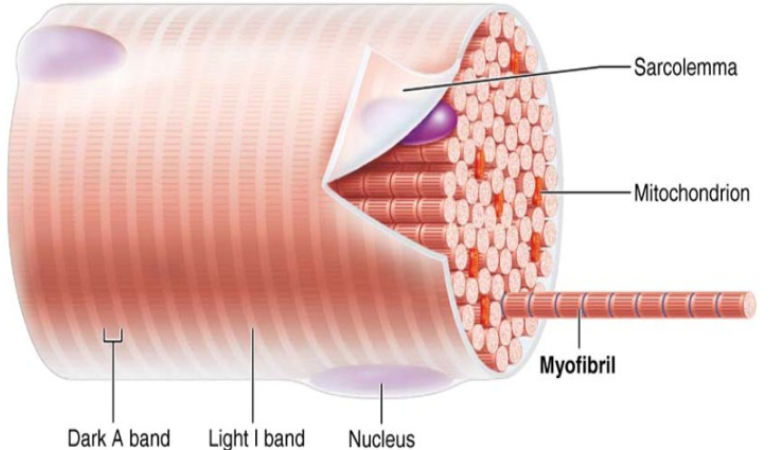
Myofibrils (Skeletal Muscle Fiber Microanatomy)
Myofibrils are densely packed, rodlike elements
Single muscle fiber can contain 1000s
Accounts for ~80% of muscle cell volume
Myofibril features Striations, Sarcomeres, Myofilaments, Molecular composition of myofilaments
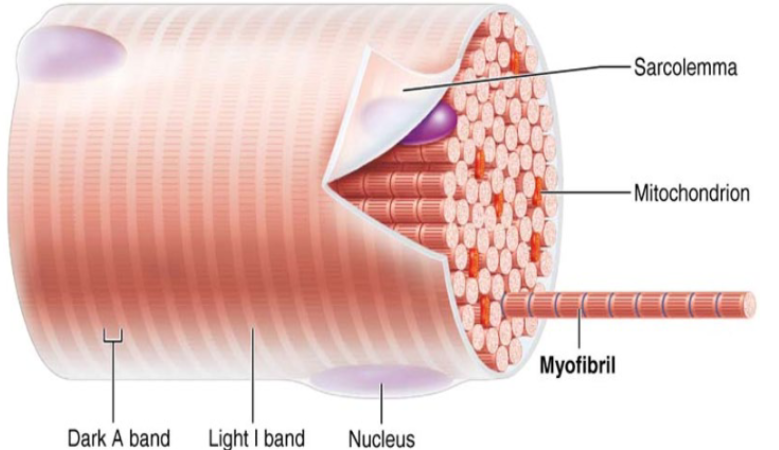
Sacromere
Smallest contractile unit (functional unit) of muscle fiber
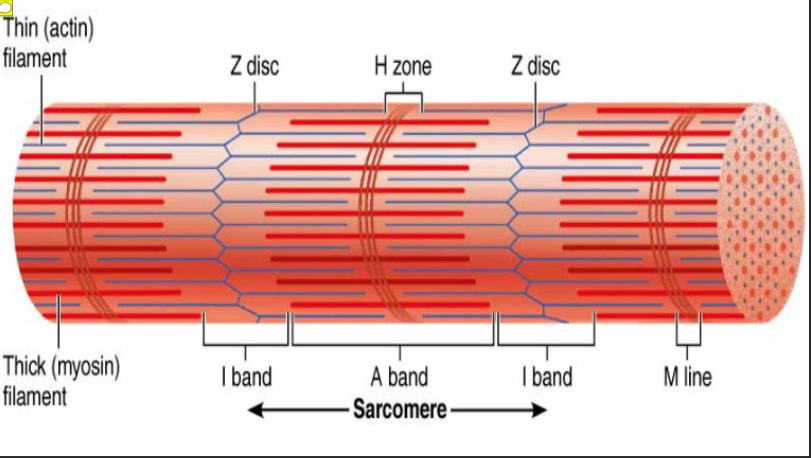
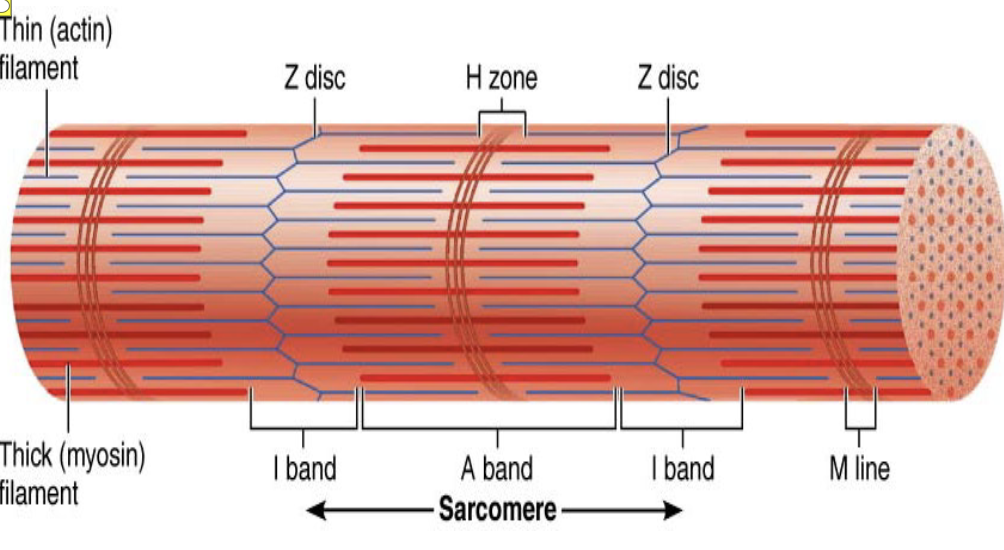
A bands (Sacromere)
dark regions
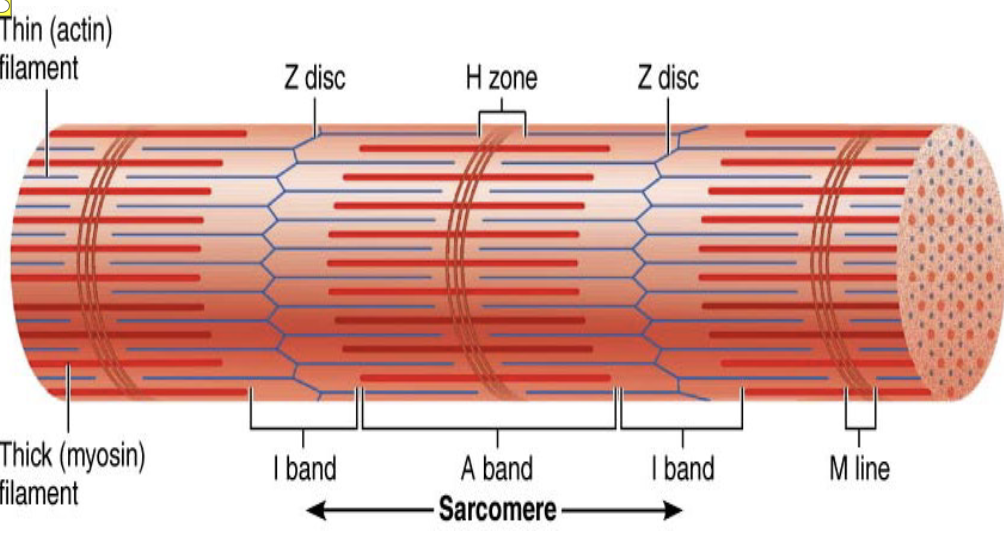
I bands (Sacromere)
lighter regions

Z disc/line (Sacromere)
coin-shaped sheet of proteins on midline of light I band

M line (Sacromere)
line of protein (myomesin) that bisects H zone vertically

H zone (Sacromere)
lighter region in middle of dark A band
All muscles share four main characteristics:
Excitability (responsiveness): ability to receive and respond to stimuli
Contractility: ability to shorten forcibly when stimulated
Extensibility: ability to be stretched
Elasticity: ability to recoil to resting length
Four important functions of muscle
Produce movement: responsible for all locomotion and manipulation
Example: walking, digesting, pumping blood
Maintain posture and body position
Stabilize joints
Generate heat as they contract
ONLY skeletal and smooth muscle cells are elongated and referred to as…
muscle fibers

Striations
stripes formed from repeating series of dark and light bands along length of each myofibril
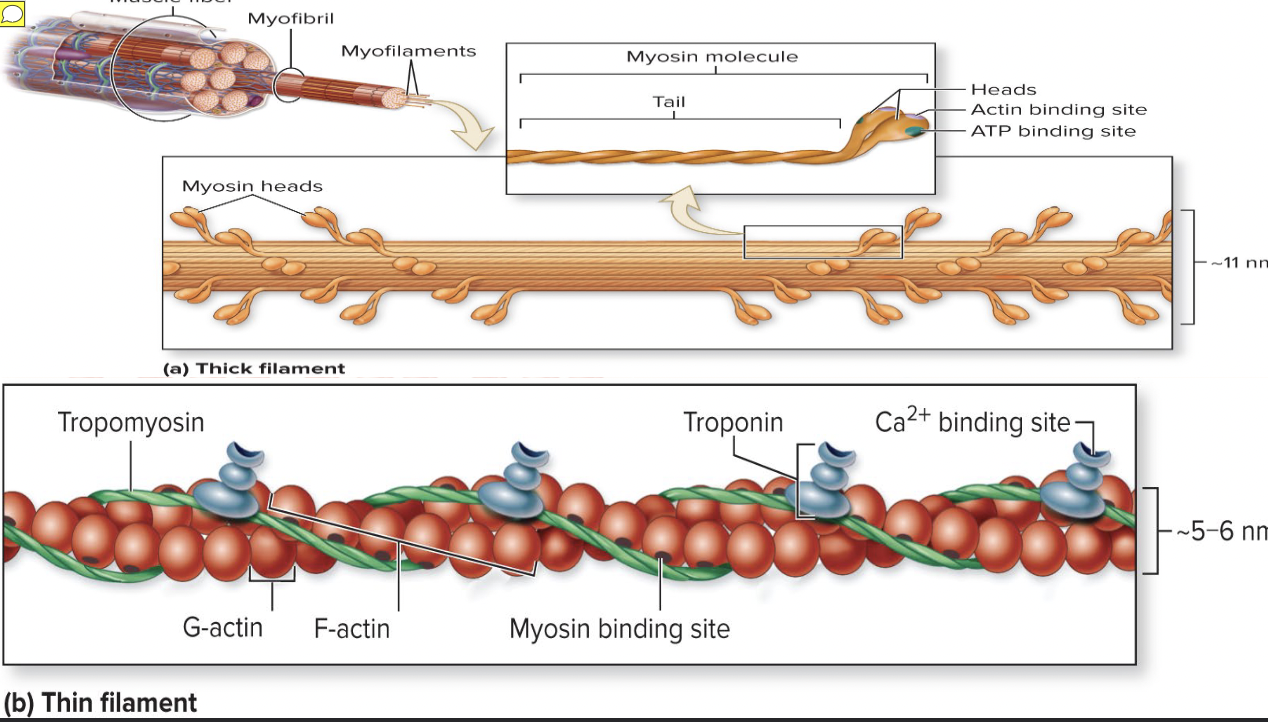
Myofilaments
Orderly arrangement of actin and myosin myofilaments within sarcomere
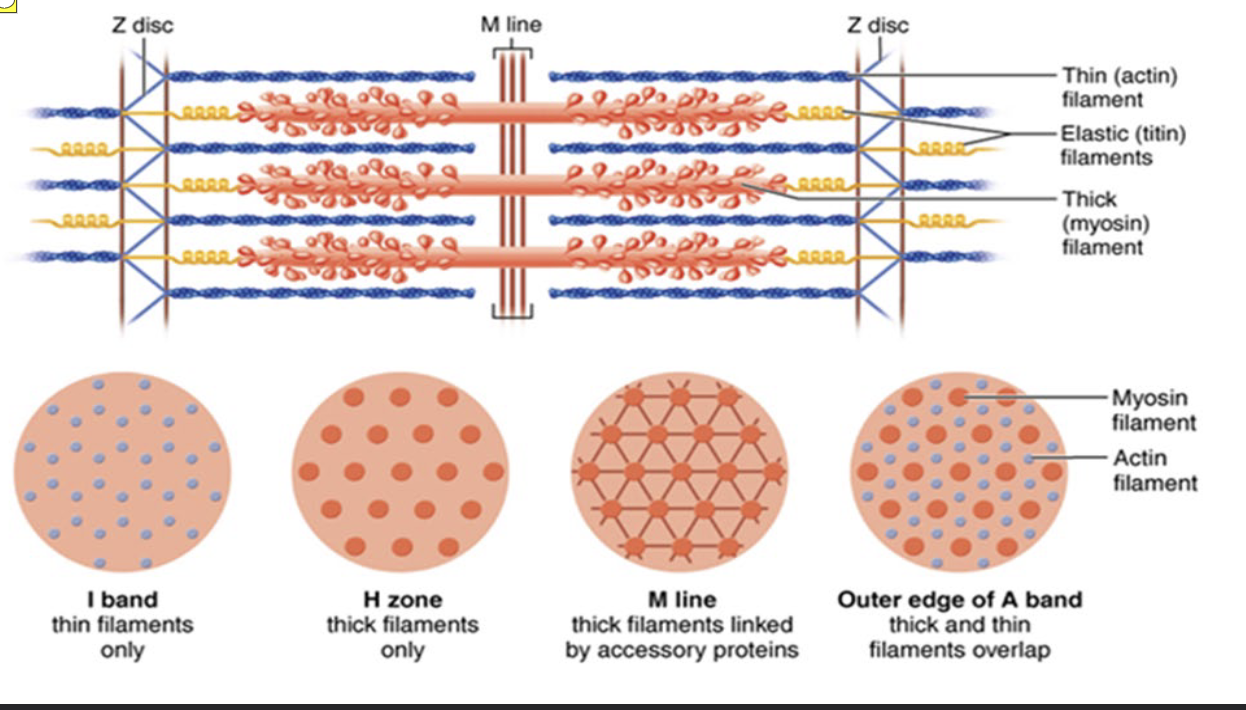
Actin myofilaments
thin filaments Extend across I band and partway in A band and Anchored to Z discs
Myosin myofilaments
thick filaments Extend length of A band Connected at M line
Sarcomere cross section shows hexagonal arrangement of one thick filament surrounded by six thin filaments
Sarcomere cross section shows hexagonal arrangement of one thick filament surrounded by six thin filaments
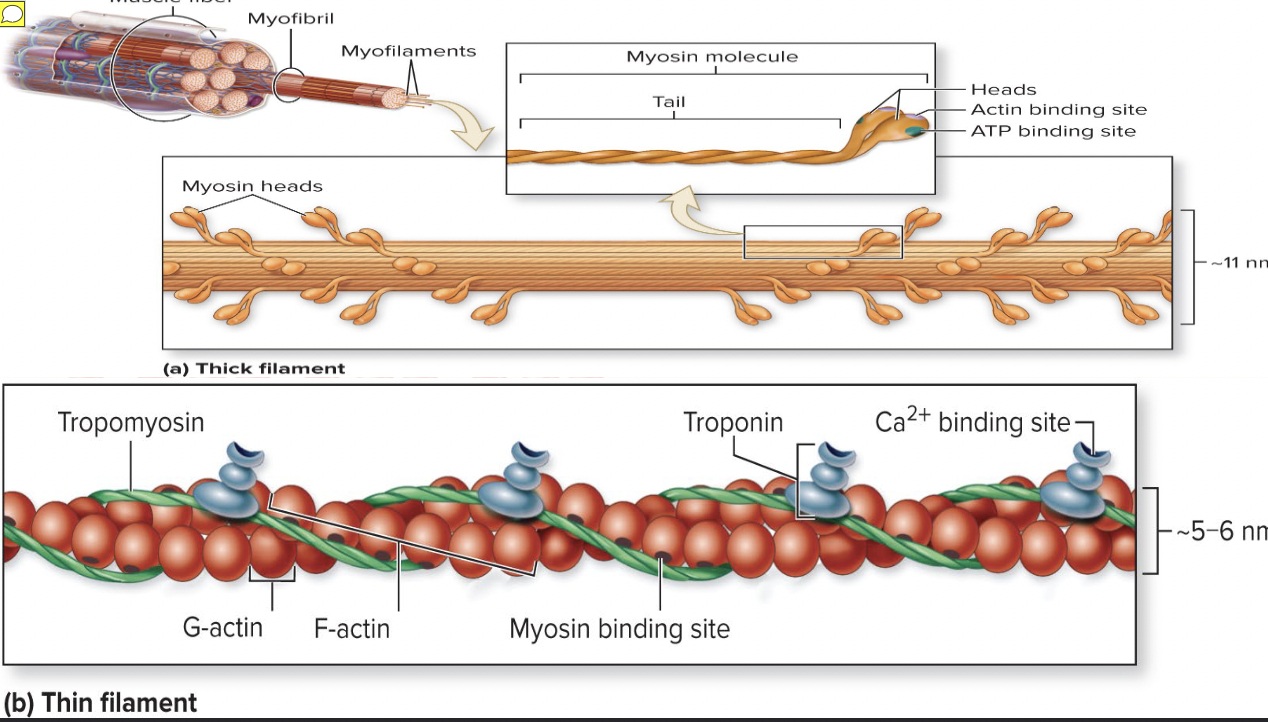
Thick filaments (myofilaments)
composed of protein myosin that contains two heavy and four light polypeptide chains
Heavy chains intertwine to form myosin tail
Light chains form myosin globular head
During contraction, heads link thick and thin filaments together, forming cross bridges
Myosins are offset from each other, resulting in staggered array of heads at different points along thick filament
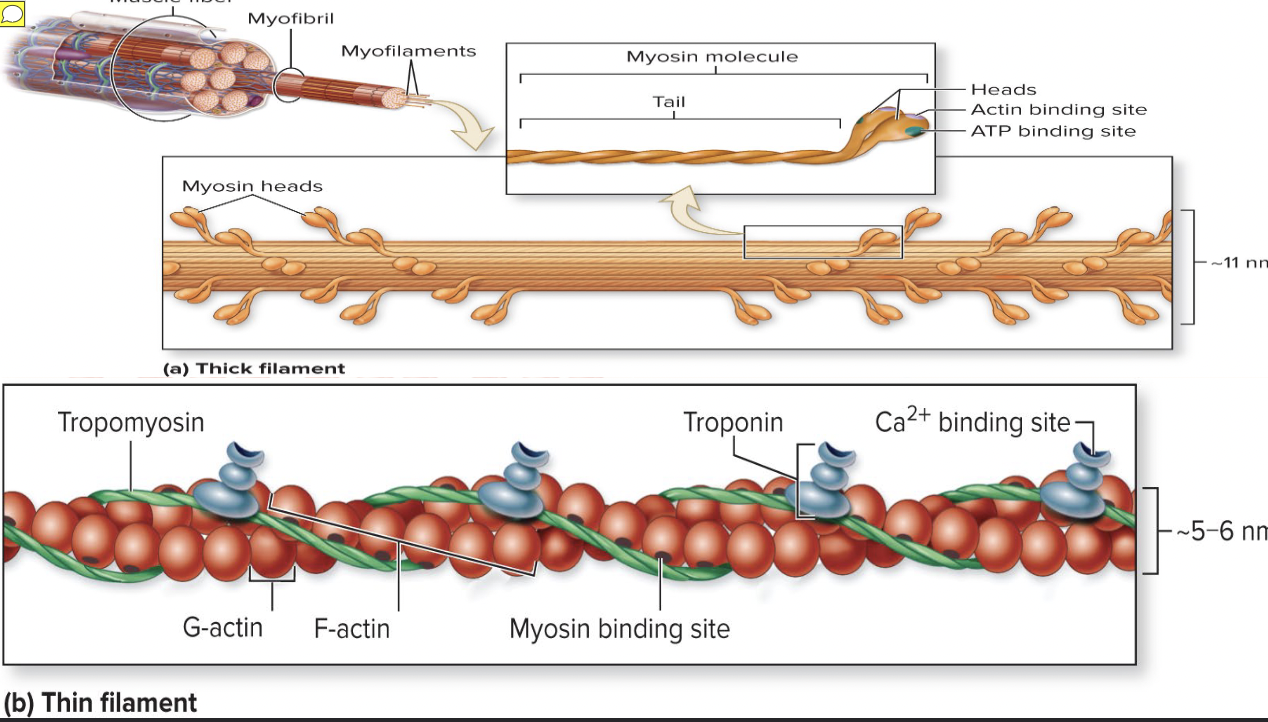
Thin filaments (myofilaments)
composed of fibrous protein actin
Actin is polypeptide made up of kidney-shaped G actin (globular) subunits
G actin subunits bears active sites for myosin head attachment during contraction
G actin subunits link together to form long, fibrous F actin (filamentous)
Two F actin strands twist together to form a thin filament
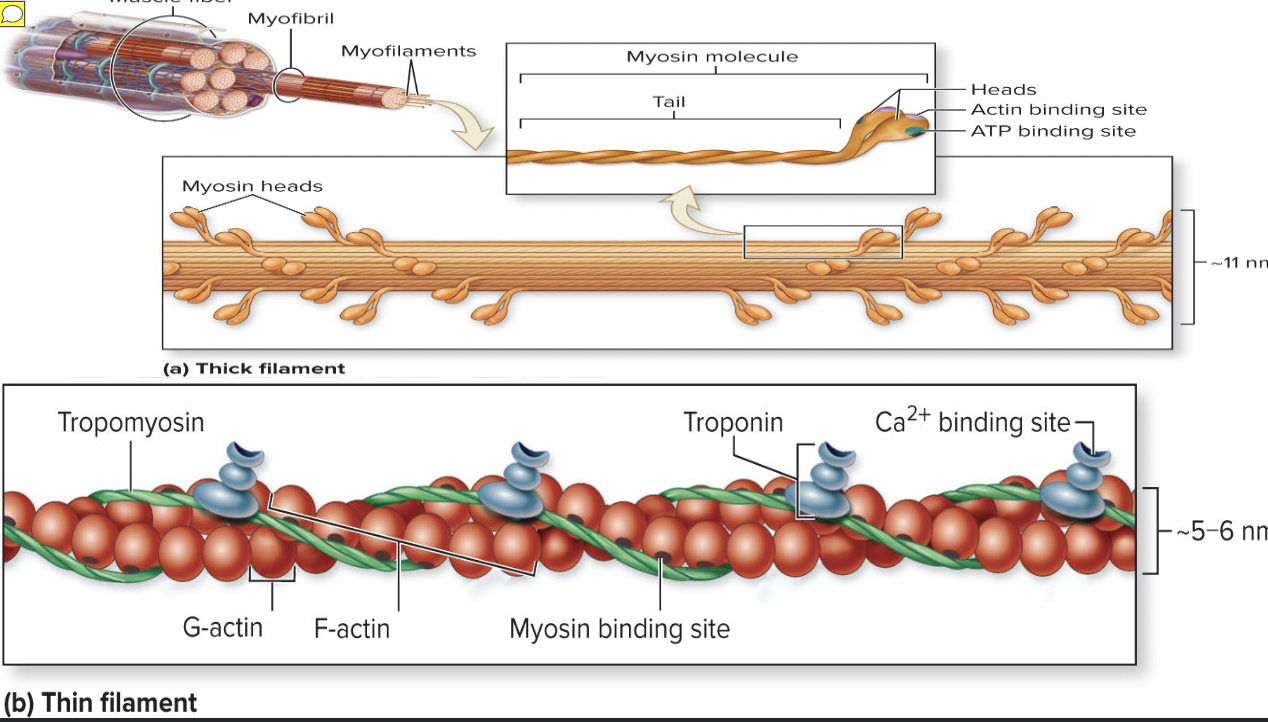
Tropomyosin and troponin (myofilaments)
regulatory proteins bound to actin
Elastic filament (myofilaments)
composed of protein titin
Holds thick filaments in place; helps recoil after stretch; resists excessive stretching
Dystrophin
Links thin filaments to proteins of sarcolemma
Nebulin, myomesin, C proteins bind filaments or sarcomeres together
Maintain alignment of sarcomere
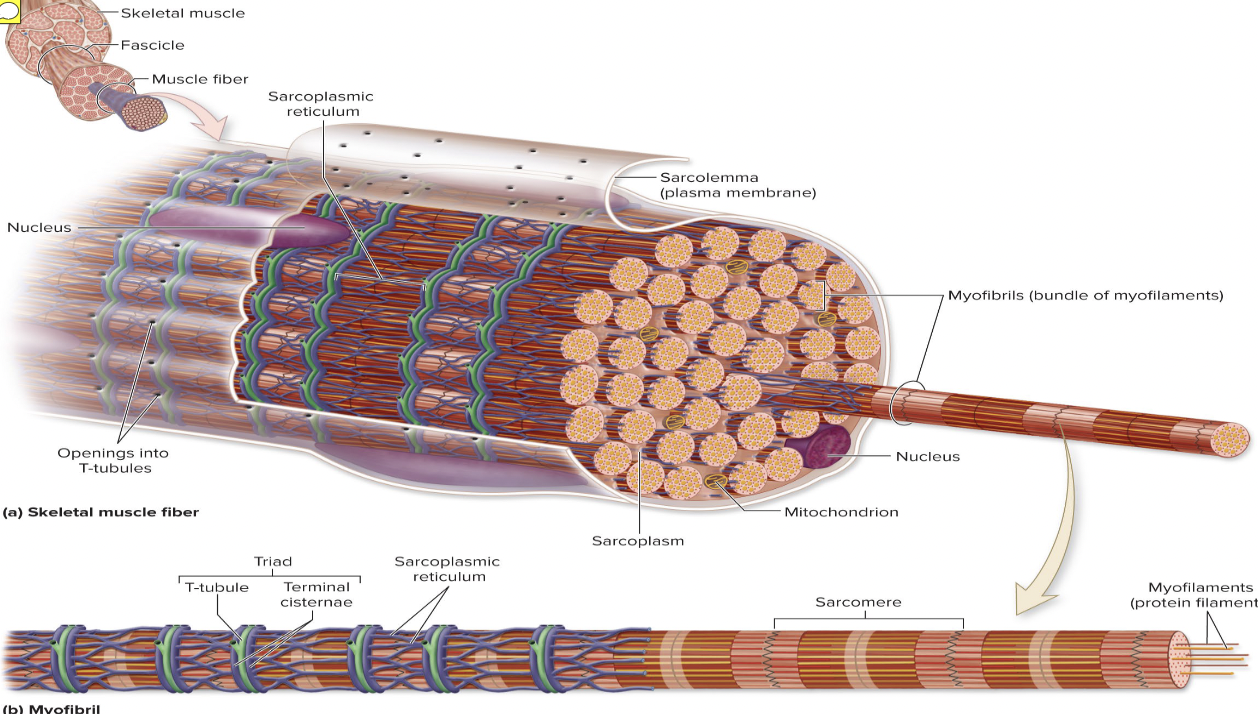
Sarcoplasmic reticulum
network of smooth endoplasmic reticulum tubules surrounding each myofibril and Most run longitudinally
Terminal cisterns form perpendicular cross channels at the A–I band junction
SR functions in regulation of intracellular Ca2+ levels and Stores and releases Ca2+
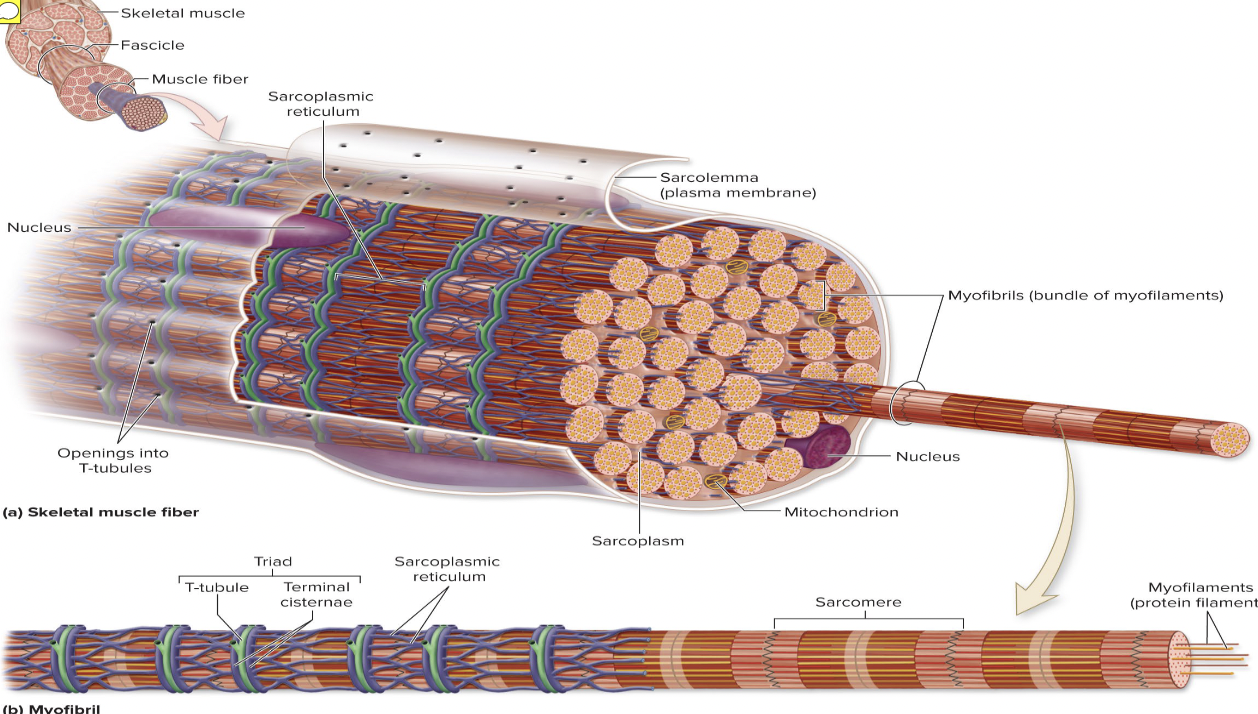
T tubules Tube
formed by protrusion of sarcolemma deep into cell interior
Increase muscle fiber’s surface area greatly
Lumen continuous with extracellular space
Allow electrical nerve transmissions to reach deep into interior of each muscle fiber
Tubules penetrate cell’s interior at each A–I band junction between terminal cisterns
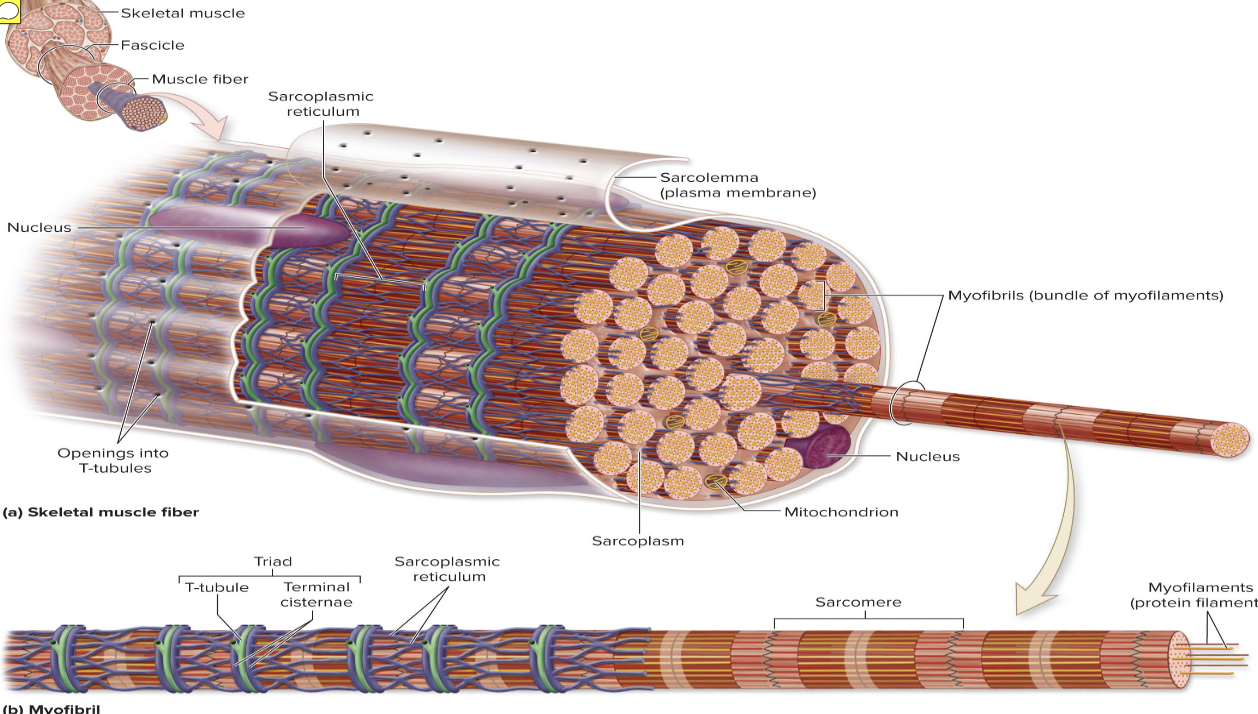
Triad
area formed from terminal cistern of one sarcomere, T tubule, and terminal cistern of neighboring sarcomere
Triad relationships
T tubule contains integral membrane proteins that protrude into intermembrane space (space between tubule and muscle fiber sarcolemma)
Tubule proteins
act as voltage sensors that change shape in response to an electrical current
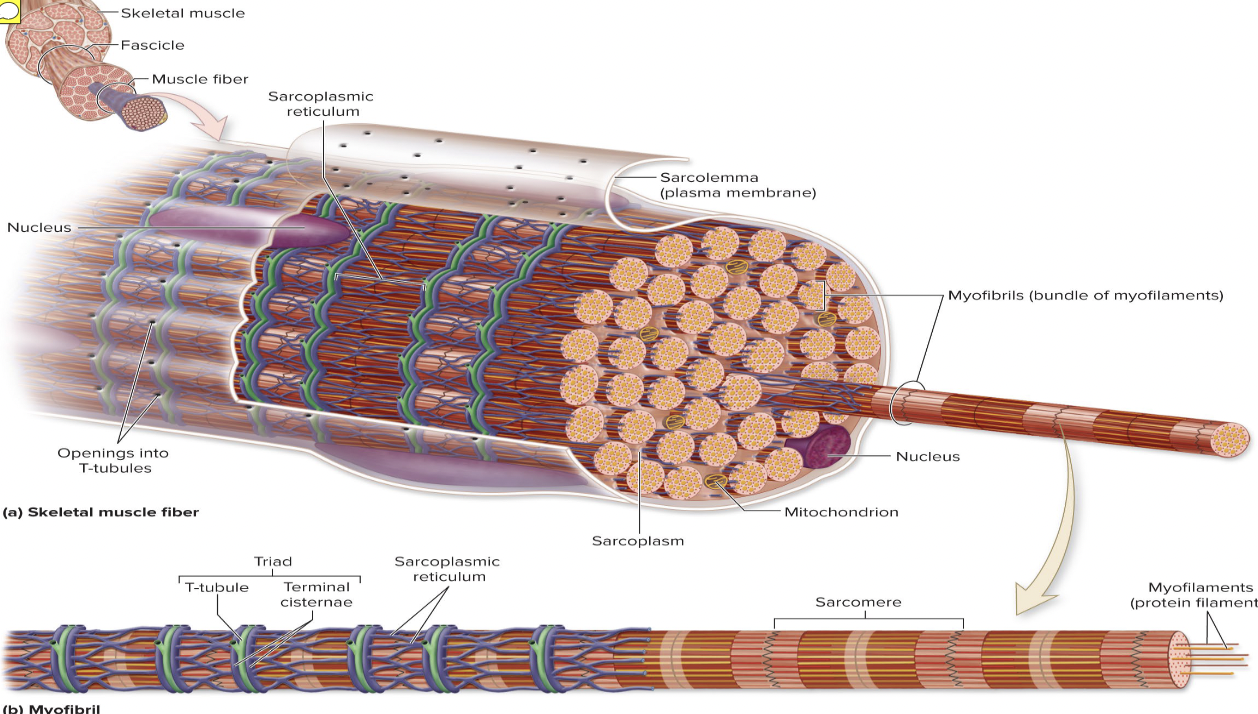
SR cistern membranes
have integral membrane proteins that protrude into intermembrane space
SR integral proteins control opening of calcium channels in SR cisterns
When an electrical impulse passes by, T tubule proteins change shape, causing SR proteins to change shape, causing release of calcium into cytoplasm
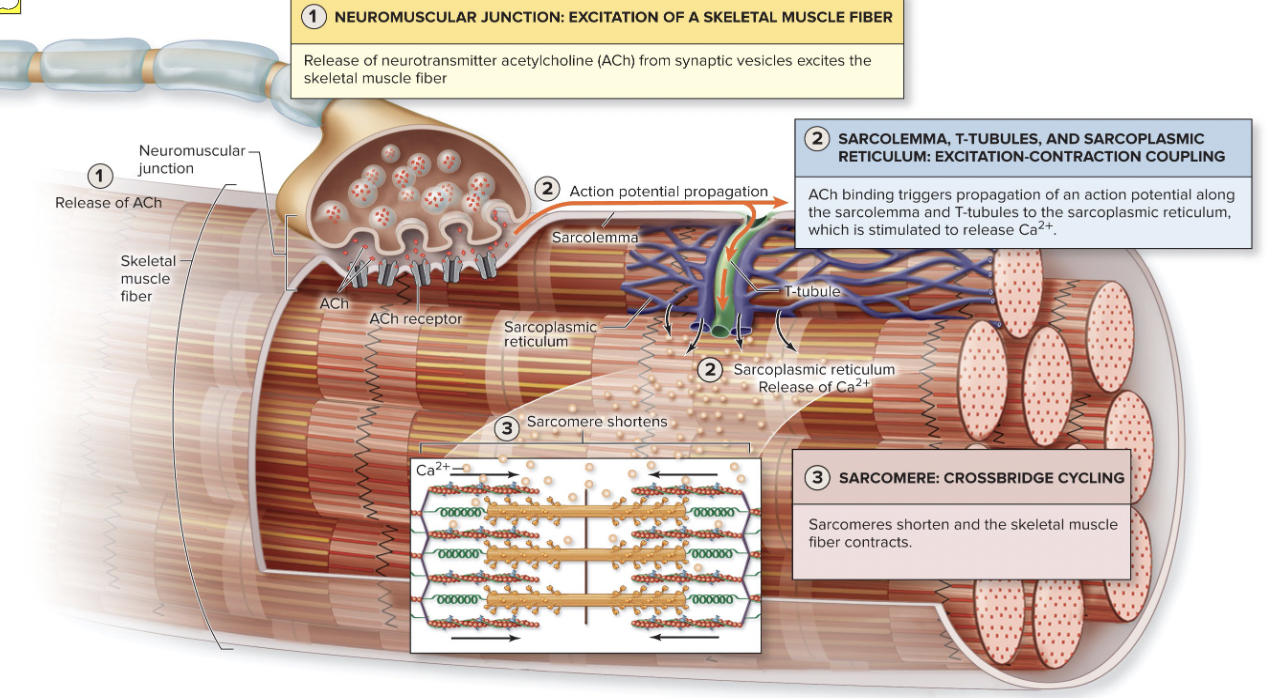
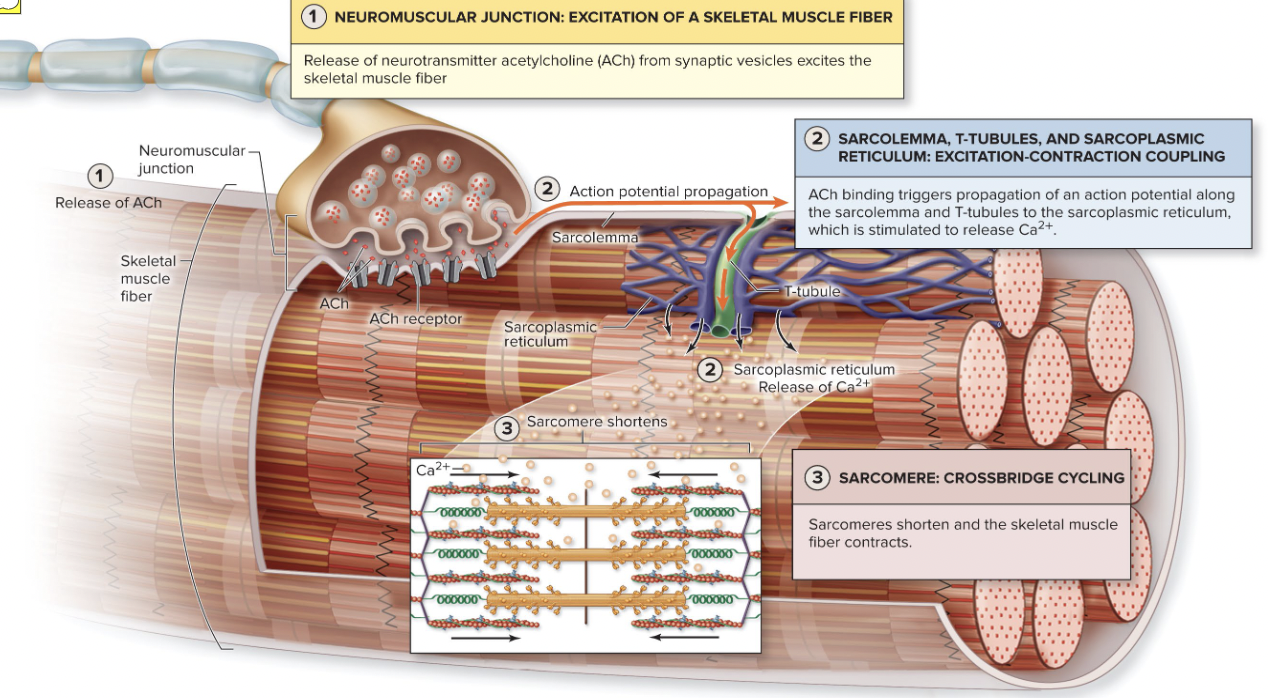
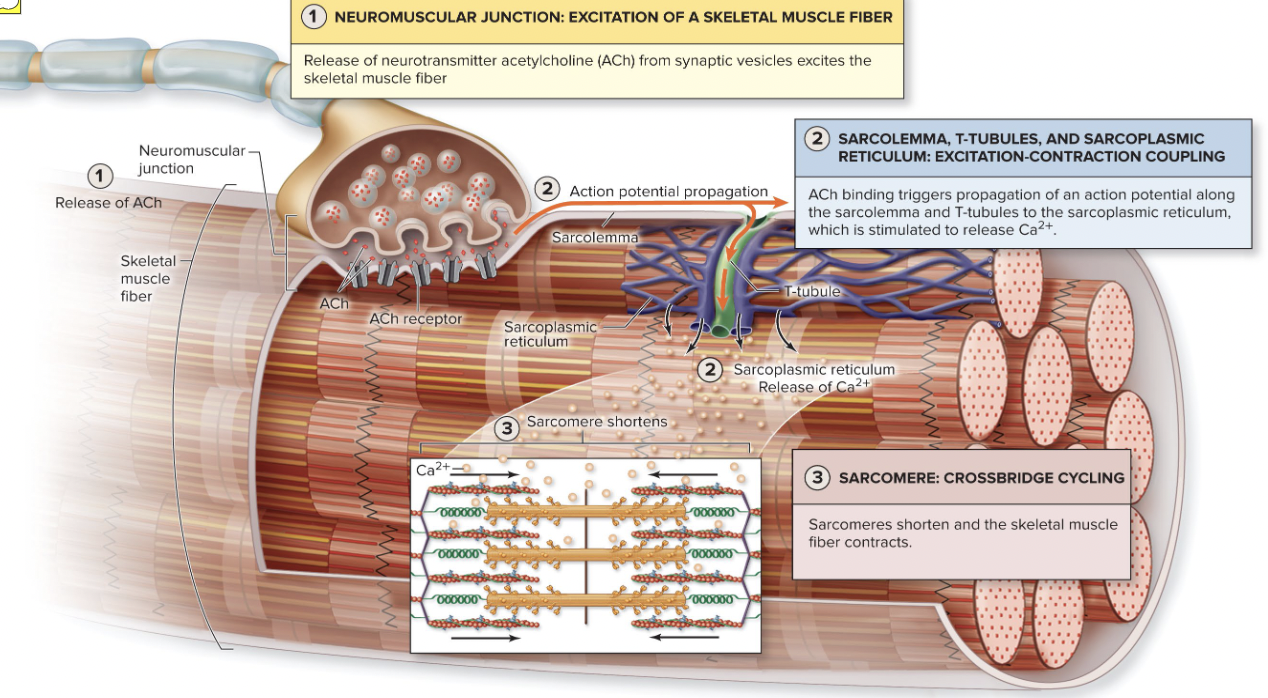
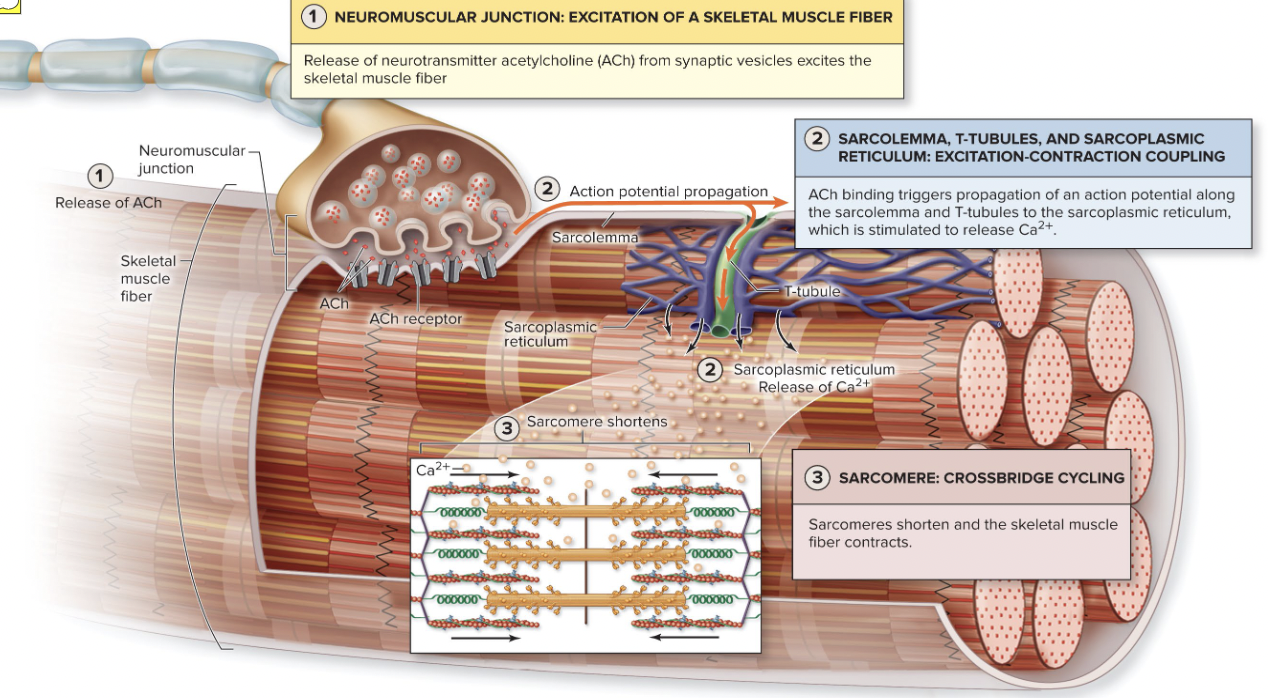
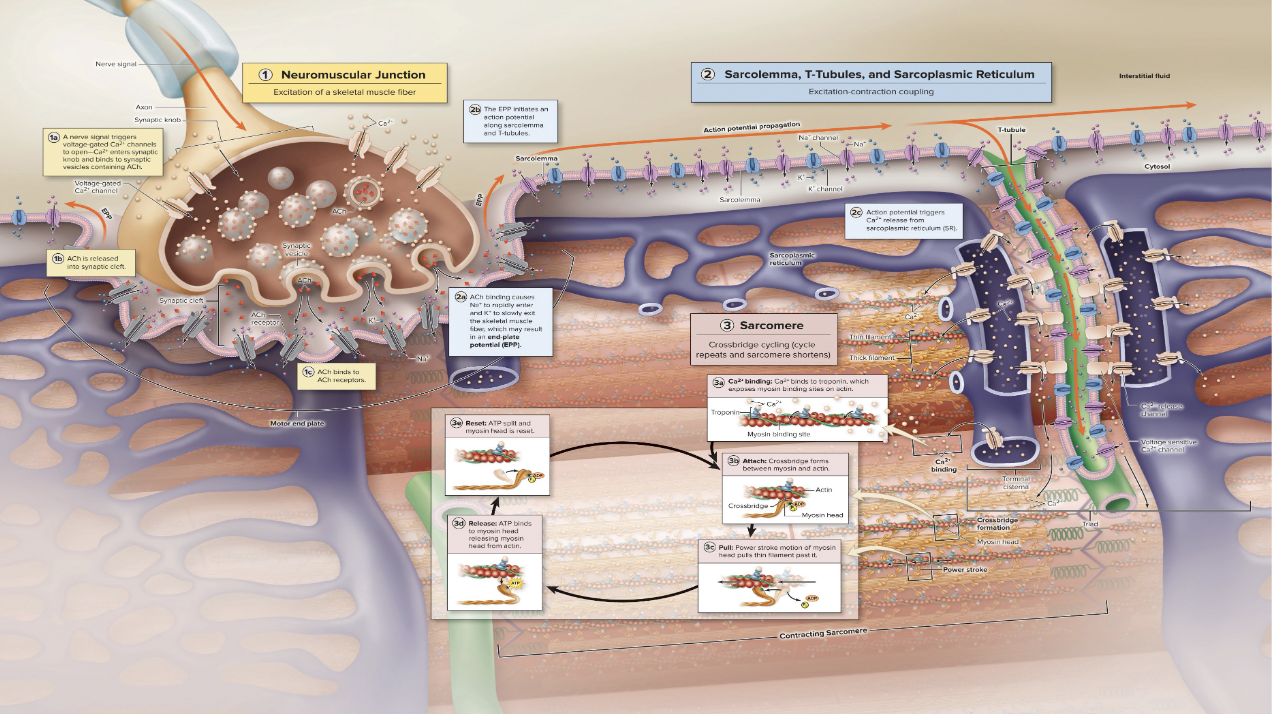
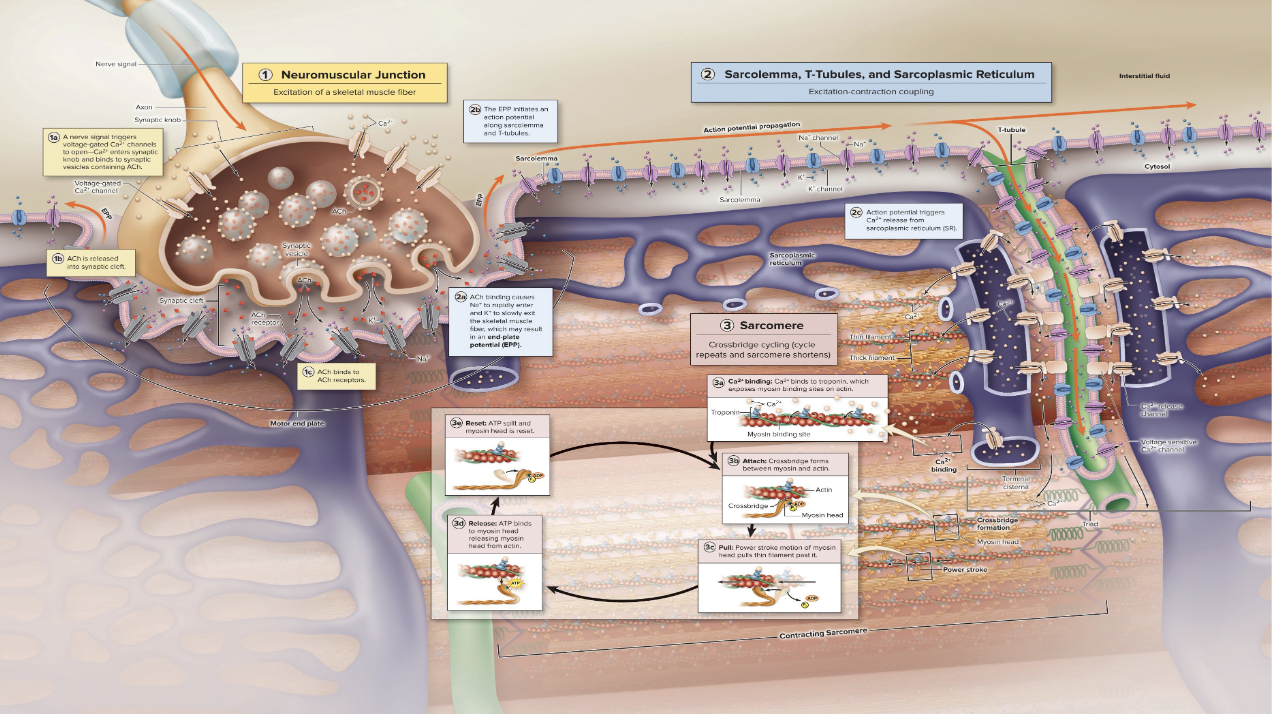
Excitation Contraction Coupling
Muscle moving = nervous system releases Accetylcholine
Accetylcholine binds with Accetylcholine receptor on the sarcolemma
This allows Na+ to come in (DEPOLARIZATION)
Voltage gates are opened, which allows more sodium in
The cell is depolarized to the point of allowing calcium out
This causes actin and myosin to come together.
Decision to move is activated by….
brain, signal is transmitted down spinal cord to motor neurons which then activate muscle fibers
Neurons and muscle cells are
excitable cells capable of action potential
Excitable cells
are capable of changing resting membrane potential voltages
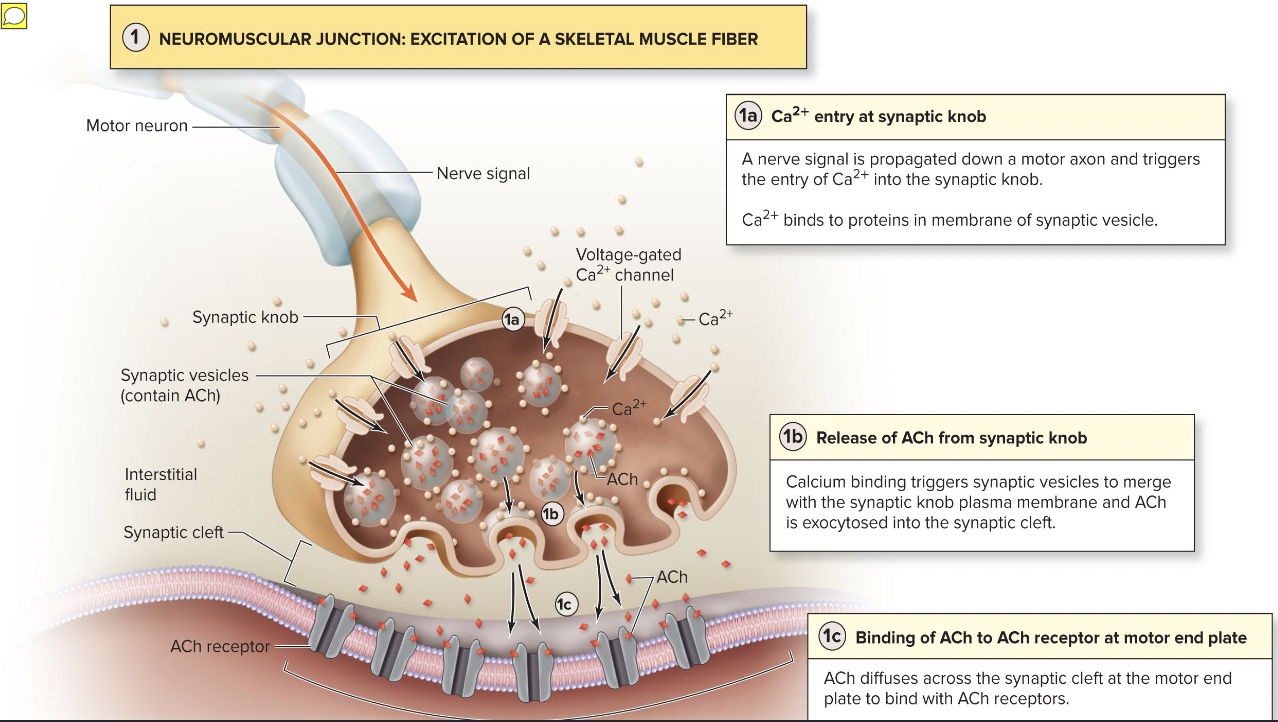
AP crosses from neuron to muscle cell via the
neurotransmitter acetylcholine (ACh)
Contraction
the activation of cross bridges to generate force
Shortening occurs when tension generated by cross bridges on thin filaments exceeds forces opposing shortening
Contraction ends when cross bridges become inactive
In the relaxed state,
thin and thick filaments overlap only slightly at ends of A band
Sliding filament model of contraction states
that during contraction, thin filaments slide past thick filaments, causing actin and myosin to overlap more
Neither thick nor thin filaments change length, just overlap more
When nervous system stimulates muscle fiber
myosin heads are allowed to bind to actin, forming cross bridges, which cause sliding (contraction) process to begin
Cross bridge attachments form and break several times, each time pulling thin filaments a little closer toward center of sarcome in a ratcheting action
Causes shortening of muscle fiber
Z discs are pulled toward M line I bands shorten Z discs become closer H zones disappear and A bands move closer to each other
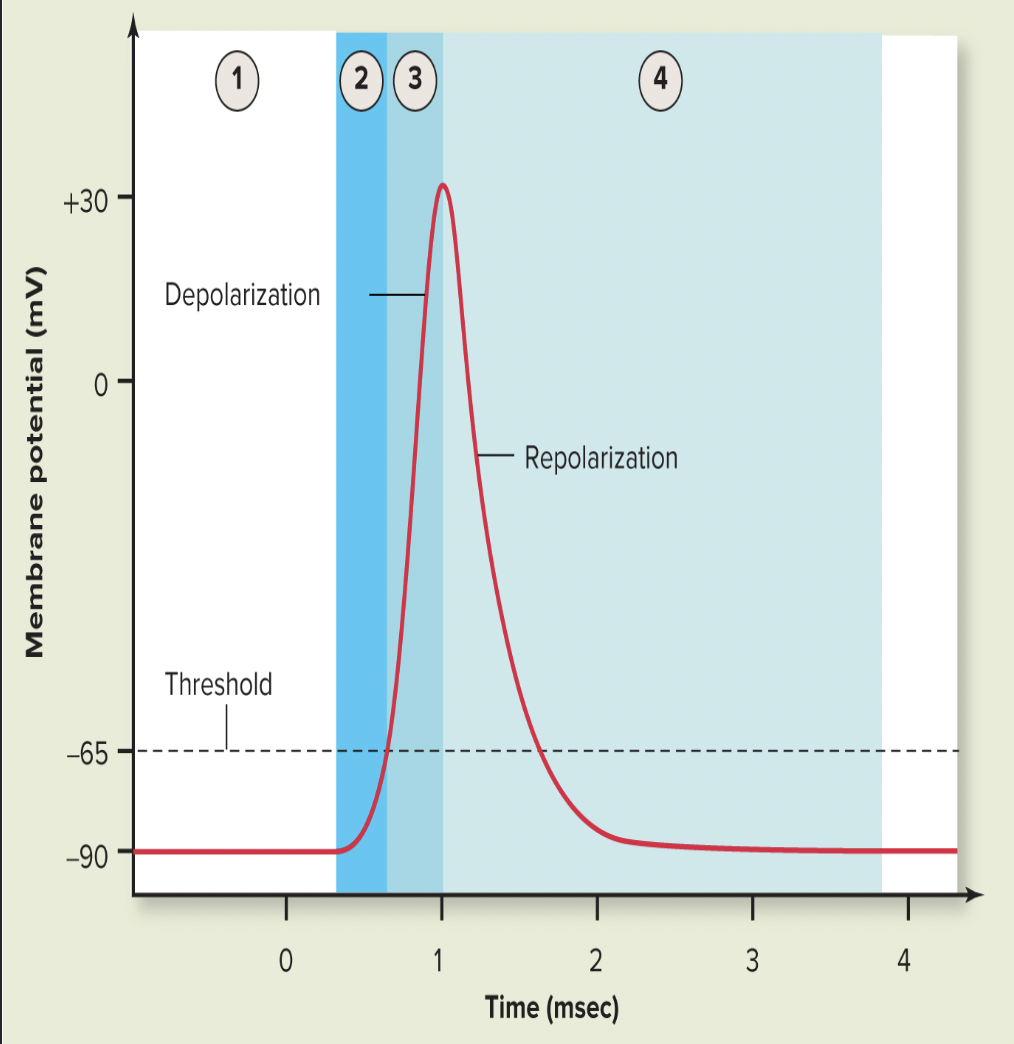
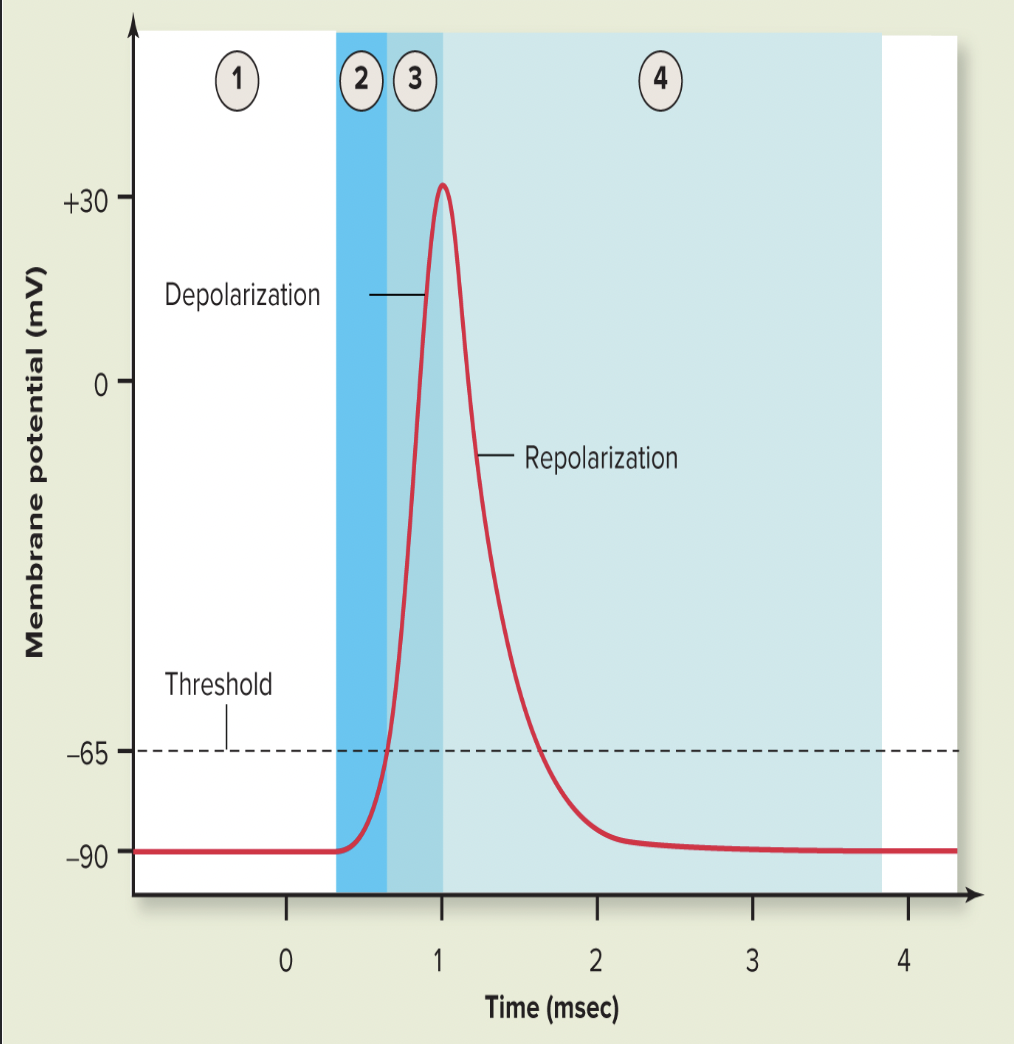
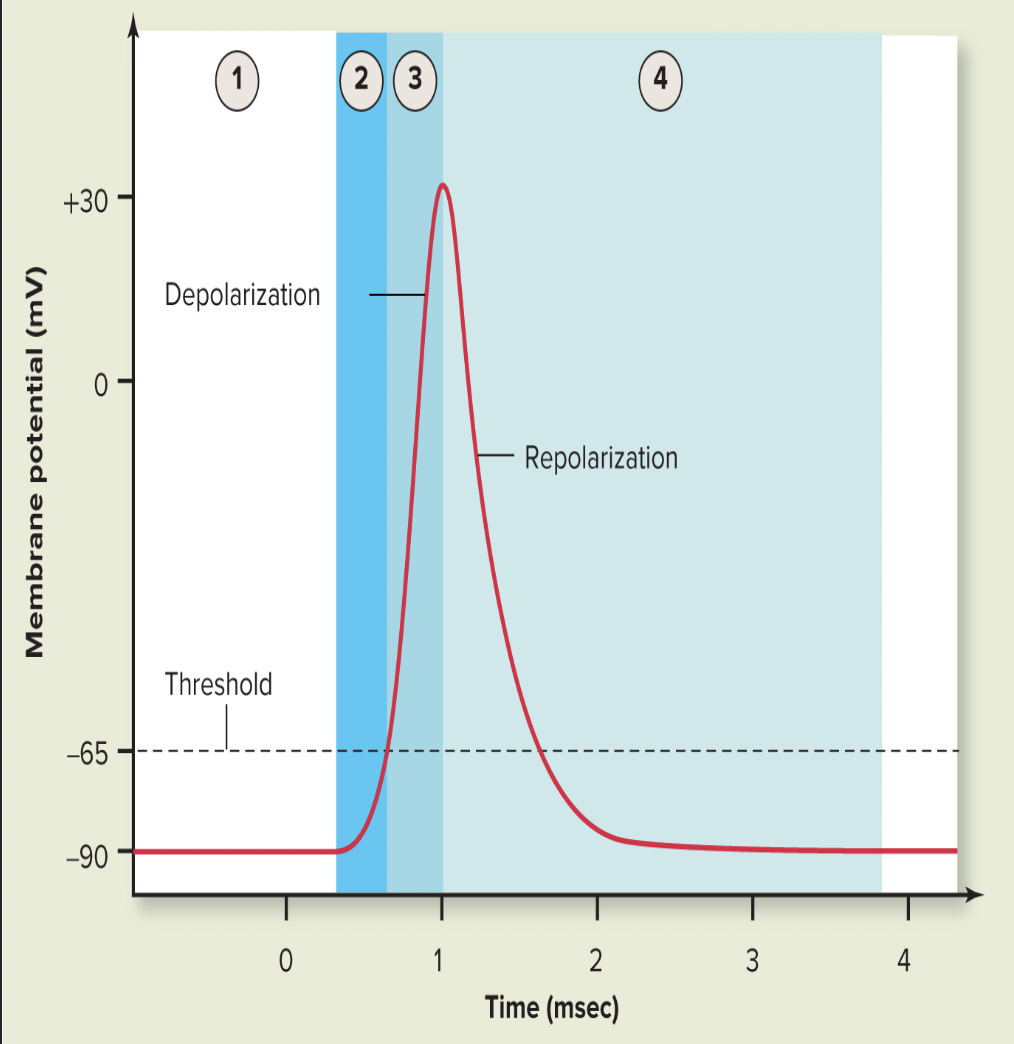
Depolarization
generation and propagation of an action potential (AP)
If end plate potential causes enough change in membrane voltage to reach critical level called threshold, voltage-gated Na+ channels in membrane will open
Large influx of Na+ through channels into cell triggers AP that is unstoppable and will lead to muscle fiber contraction
AP spreads across sarcolemma from one voltage-gated Na+ channel to next one in adjacent areas, causing that area to depolarize
Repolarization
restoration of resting conditions
Na+ voltage-gated channels close, and voltage-gated K+ channels open
K+ efflux out of cell rapidly brings cell back to initial resting membrane voltage
Refractory period: muscle fiber cannot be stimulated for a specific amount of time, until repolarization is complete
Ionic conditions of resting state are restored by Na+-K+ pump
Na+ that came into cell is pumped back out, and K+ that flowed outside is pumped back into cell
Large influx of Na+ leads to….
muscle contration
Refractory period
muscle fiber cannot be stimulated for a specific amount of time, until repolarization is complete
Excitation-contraction (E-C) coupling
events that transmit AP along sarcolemma (excitation) are coupled to sliding of myofilaments (contraction)
AP is propagated along sarcolemma and down into T tubules, where voltage-sensitive proteins in tubules stimulate Ca2+ release from SR
Ca2+ release leads to contraction
AP is brief and ends before contraction is seen
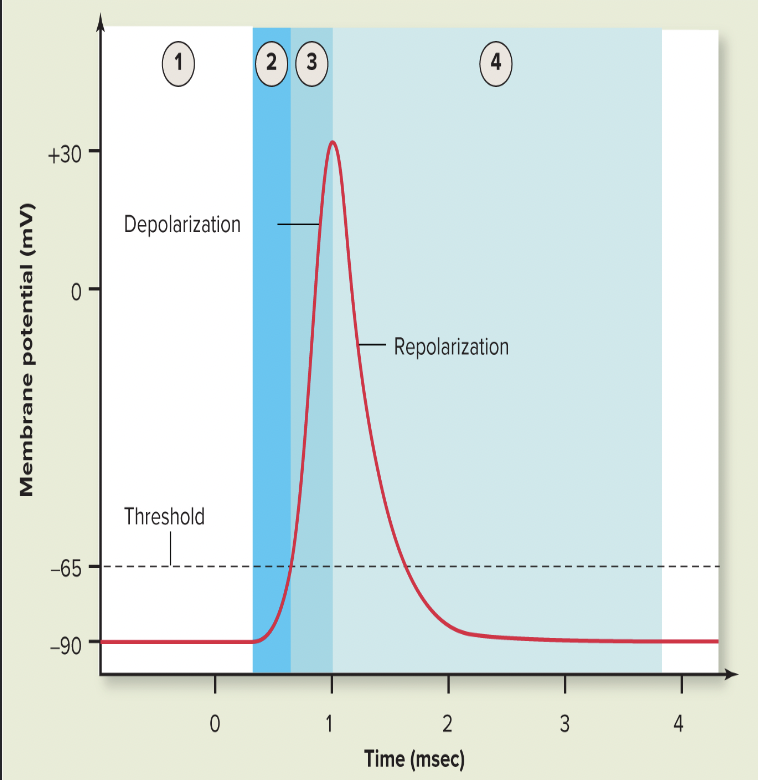
Depolarization/Repolarization Chart
Resting membrane potential of sarcolemma is -90mV
The threshold is reached when ACh receptors, which are chemically gated ion channels. Na+ enters changing the RMP fro -90mV to -65mV
THRESHOLD VALUE: -65mV
Depolarization: occurs at voltage-gated Na+ channels on sacrolemma. RMP goes from -65mV to +30mV
Repolarization occurs due to closure of voltage-gated Na+ channels and opening of voltage-gated K+ channels. This changes the RMP from +30 to -90mV
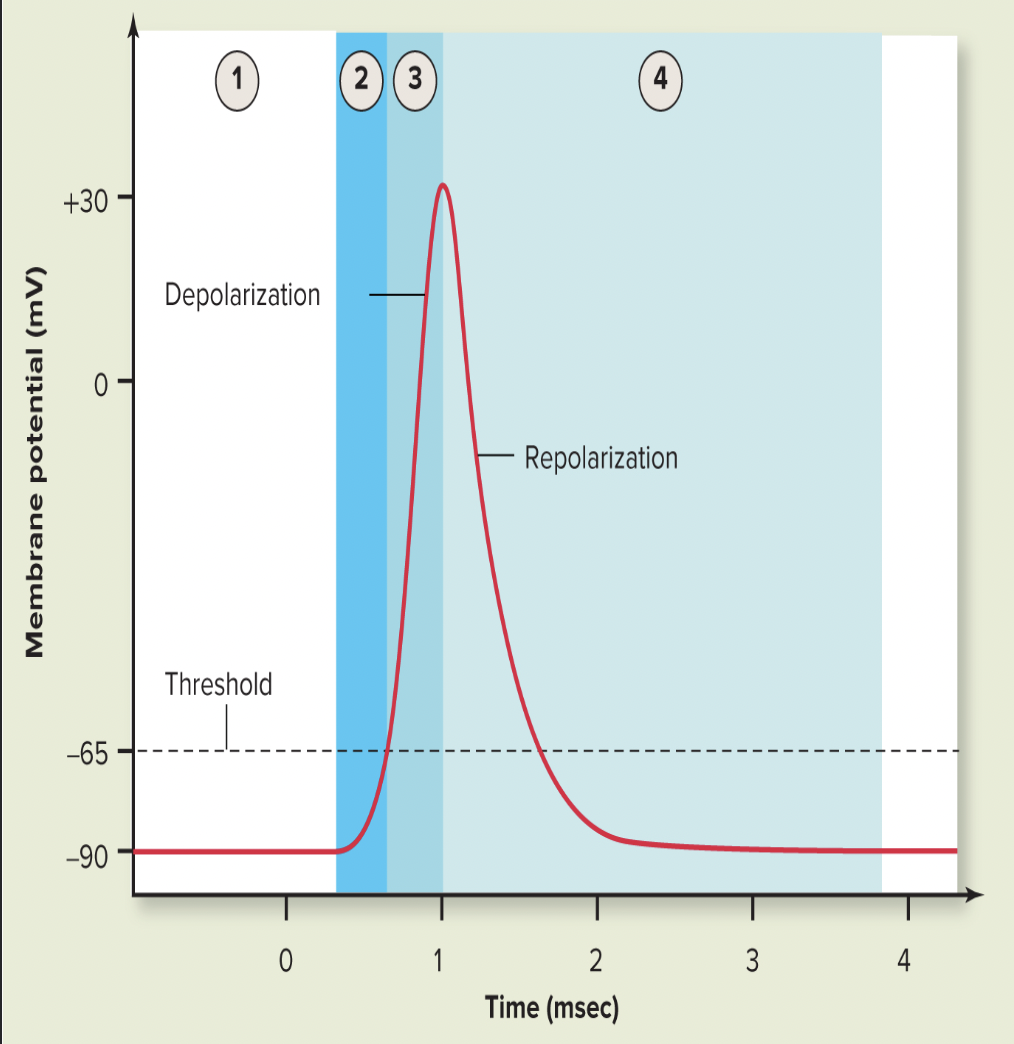
Resting membrane potential of sarcolemma is
-90mV
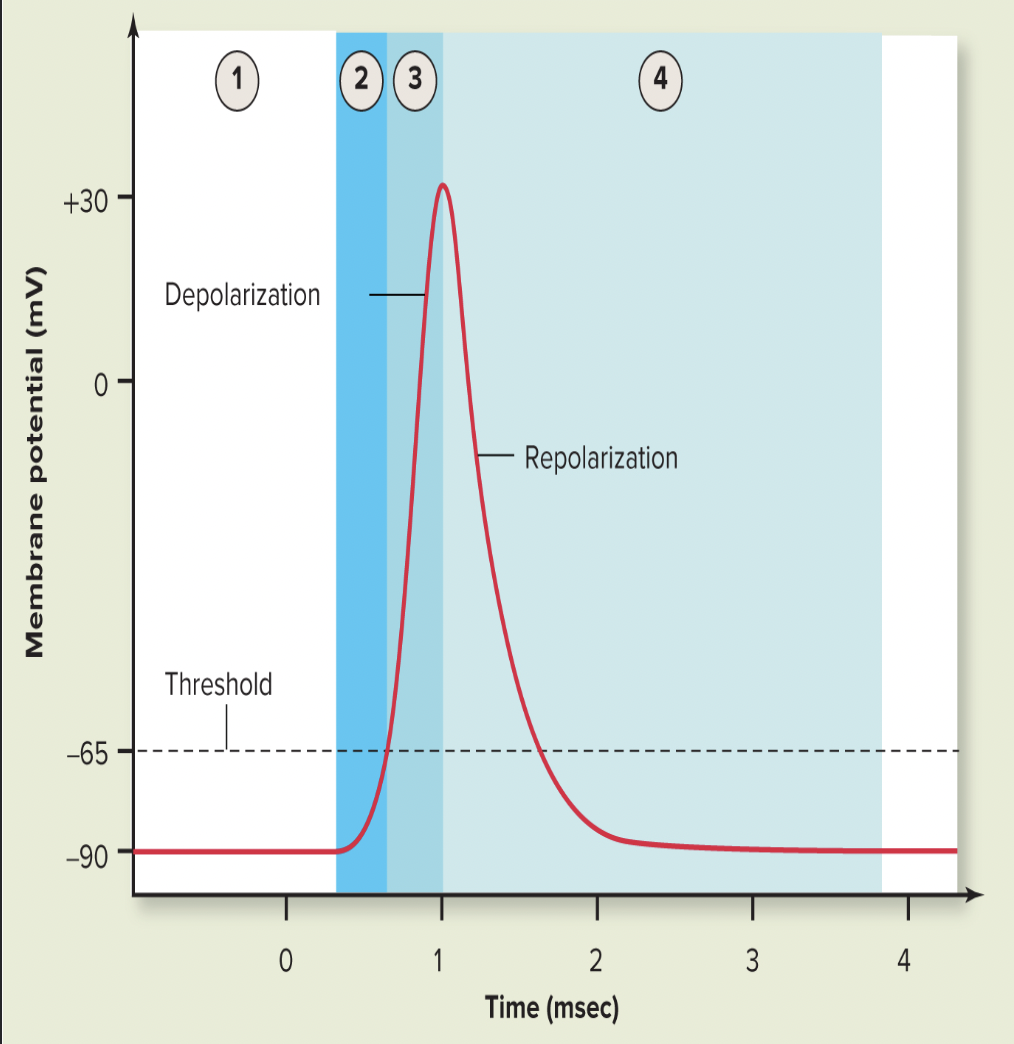
THRESHOLD VALUE
-65mV
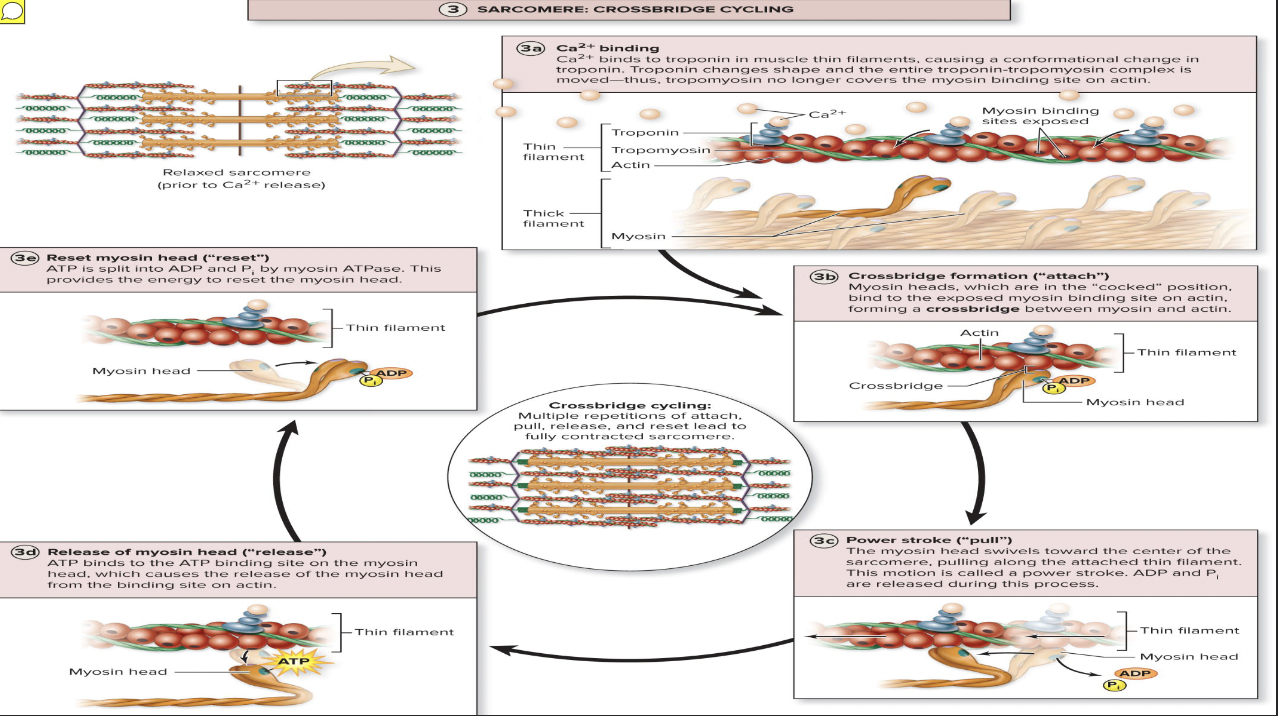
At low intracellular Ca2+ concentration: (1)
Tropomyosin blocks active sites on actin
Myosin heads cannot attach to actin
Muscle fiber remains relaxed
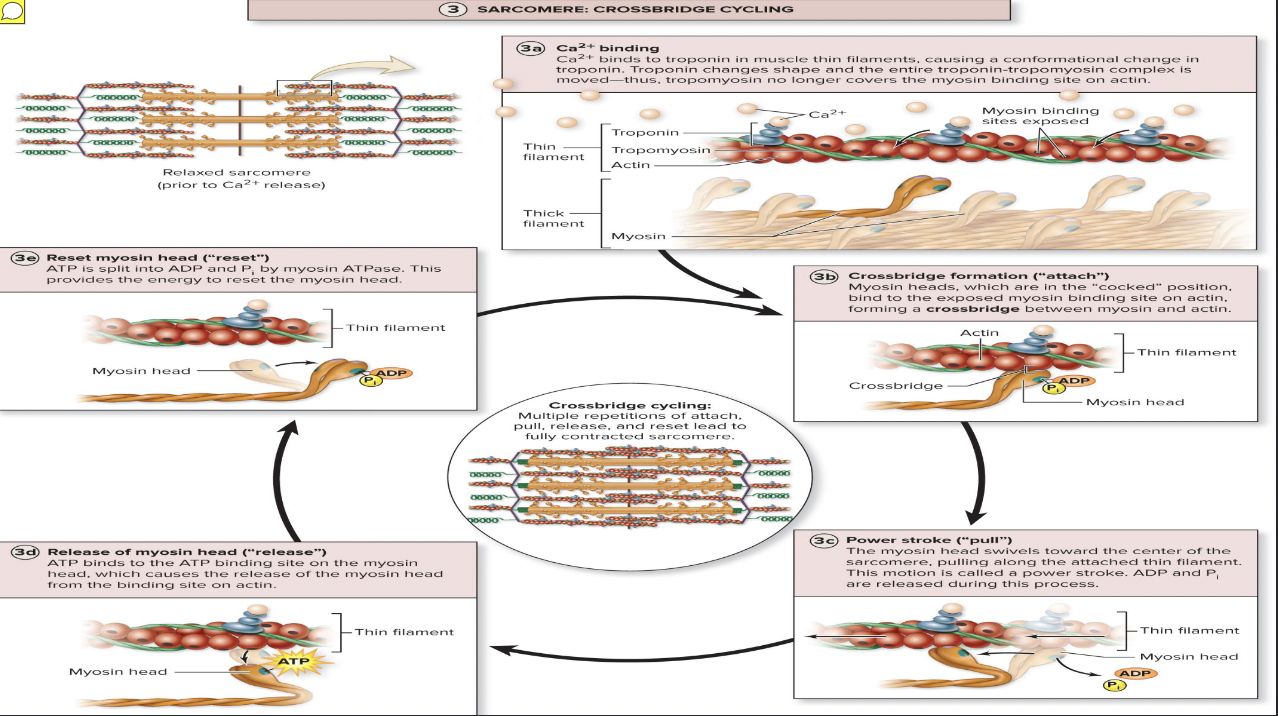
Voltage-sensitive proteins in T tubules change shape… (2)
causing sarcoplasmic reticulum (SR) to release Ca2+ to cytosol
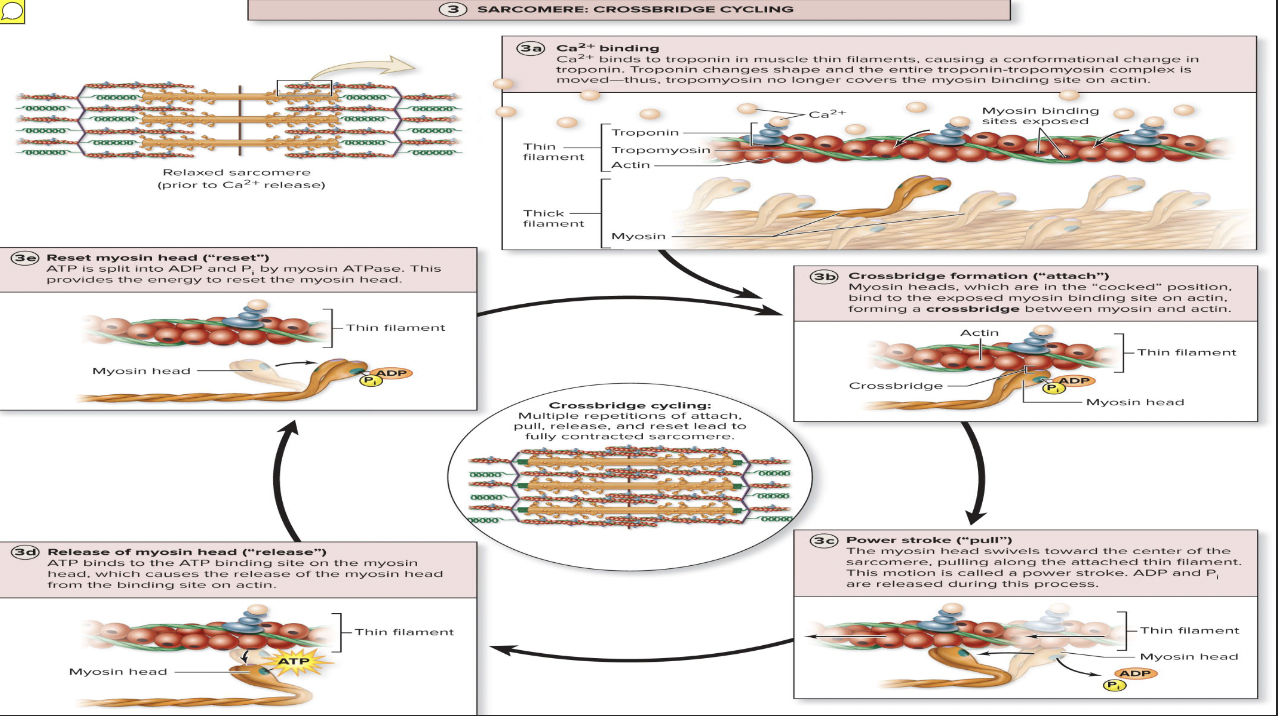
At higher intracellular Ca2+ concentrations, Ca2+… (3)
binds to troponin
Troponin changes shape and moves tropomyosin away from myosin-binding sites
Myosin heads is then allowed to bind to actin, forming cross bridge
Cycling is initiated, causing sarcomere shortening and muscle contraction
When nervous stimulation ceases, Ca2+ is pumped back into SR, and contraction ends

Four steps of the cross bridge cycle of sarcomere
Cross bridge formation: high-energy myosin head attaches to actin thin filament active site
Working (power) stroke: myosin head pivots and pulls thin filament toward M line
Cross bridge detachment: ATP attaches to myosin head, causing cross bridge to detach
Cocking of myosin head: energy from hydrolysis of ATP “cocks” myosin head into high-energy state
This energy will be used for power stroke in next cross bridge cycle
Binding site for actin
myosin head
When calcium is binded to actin….
actin and myosin come together
ATP binds and
causes release of myosin head
then ATP is hydrolyzed and another crossbridge is formed

Summary of Exciation-Coupling and Depolarization/Repolarization
When we think about contracting the muscle, the signal travels down axon of alpha motor neuron. This depolarization causing Ca2+ channels to open up
Ca2+ binds to vesicle containing ACH
ACh binds to ACh receptor, allowing Na+ in.
Local depolarization opens up voltage-gated Na+ channels.
The sarcolemma is depolarized with Na+
Depolarization travels down T tubule, which causes Ca2+ to difuse
Ca2+ binds to troponin which exposed myosin binding sites on actin
Crossbridge of myosin and actin form
To release this contraction ADP is added
Depolarization
Na+ in
Repolarization
K+ out
Contraction
produces muscle tension, the force exerted on load or object to be moved
may/may not shorten muscle
Force and duration vary in response to stimuli of different frequencies and intensities
Isometric contraction
no shortening; muscle tension increases but does not exceed load
Isotonic contraction
muscle shortens because muscle tension exceeds load
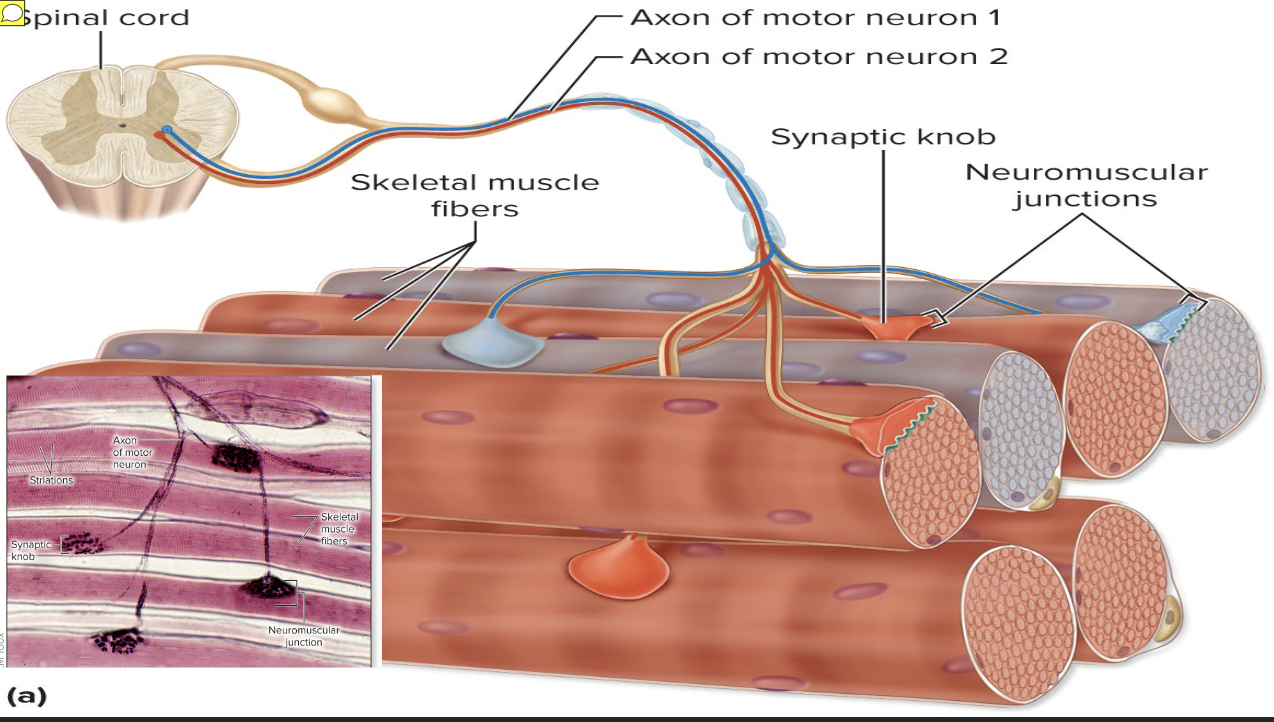
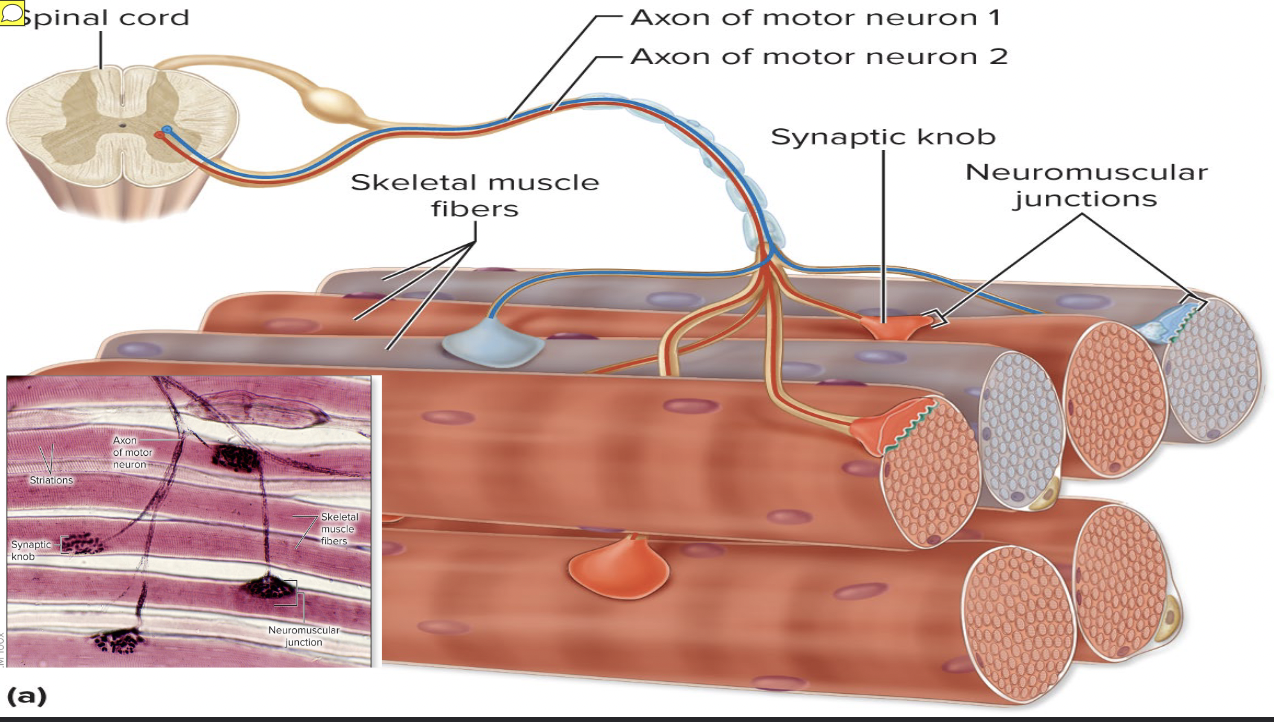
Motor nerve
Each muscle is served by at least one
contains axons of up to hundreds of motor neurons
Axons branch into terminals, each of which forms NMJ with single muscle fiber
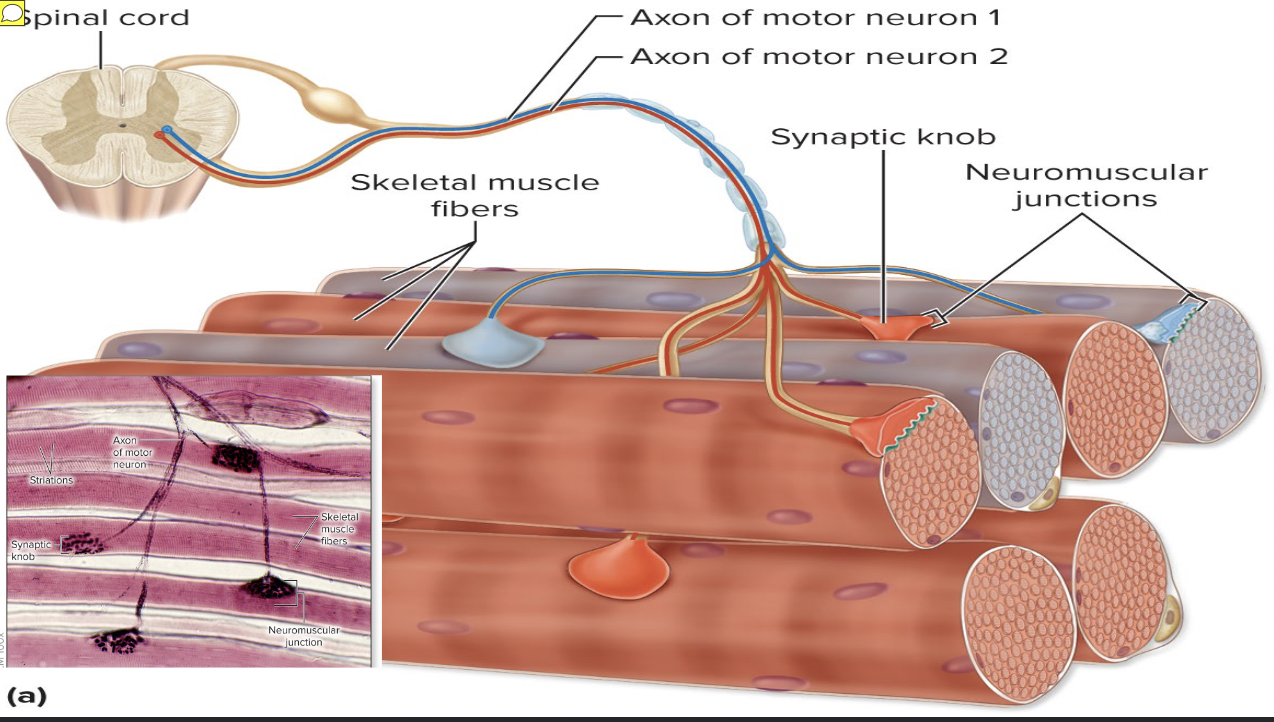
Motor unit
is the nerve-muscle functional unit
Motor unit consists of the motor neuron and all muscle fibers (four to several hundred) it supplies
Smaller the fiber number, the greater the fine control
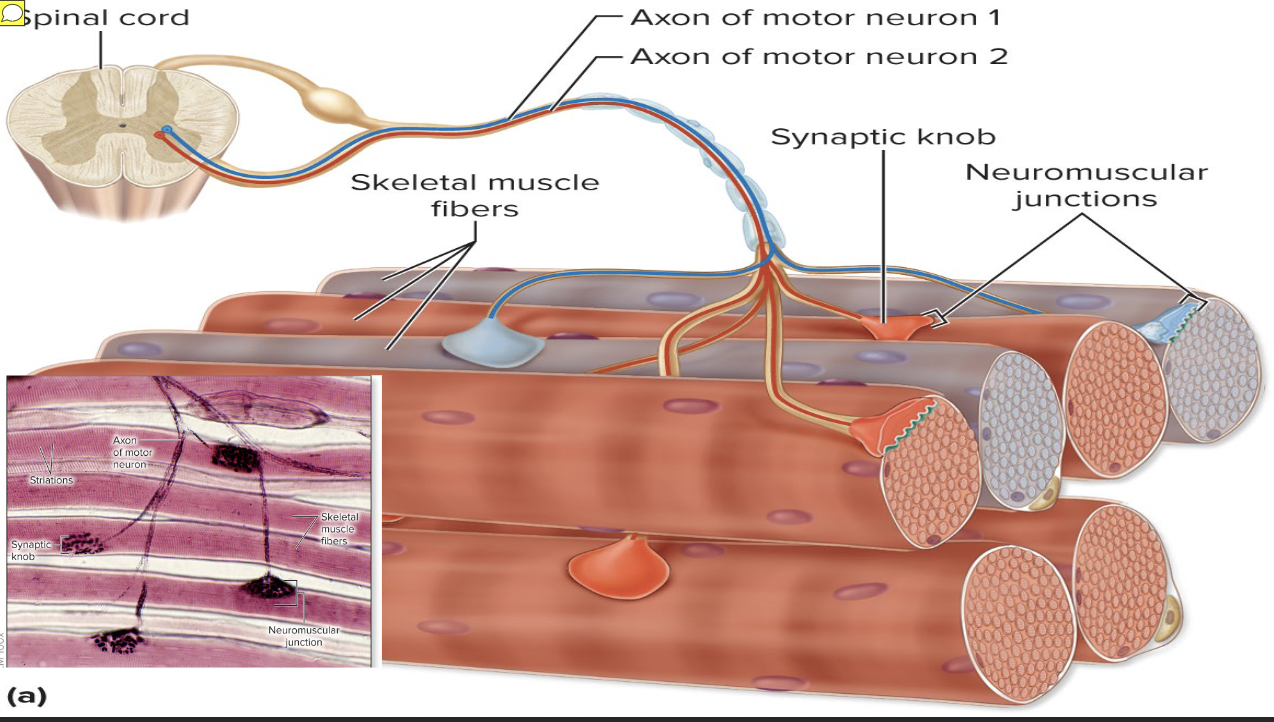
Muscle fibers from a motor unit are
spread throughout the whole muscle, so stimulation of a single motor unit causes only weak contraction of entire muscle
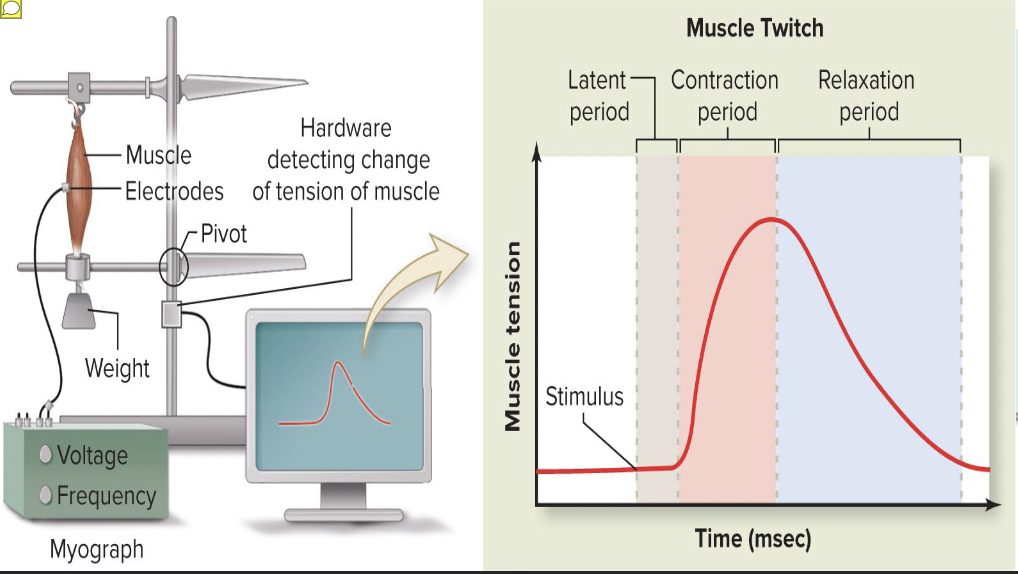
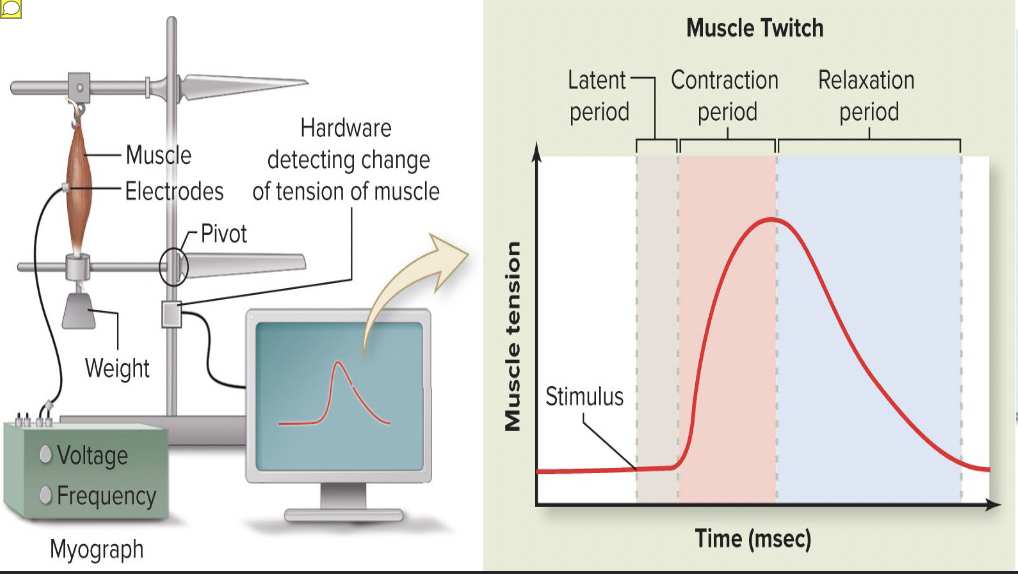
Muscle twitch
simplest contraction resulting from a muscle fiber’s response to a single action potential from motor neuron
Muscle fiber contracts quickly, then relaxes
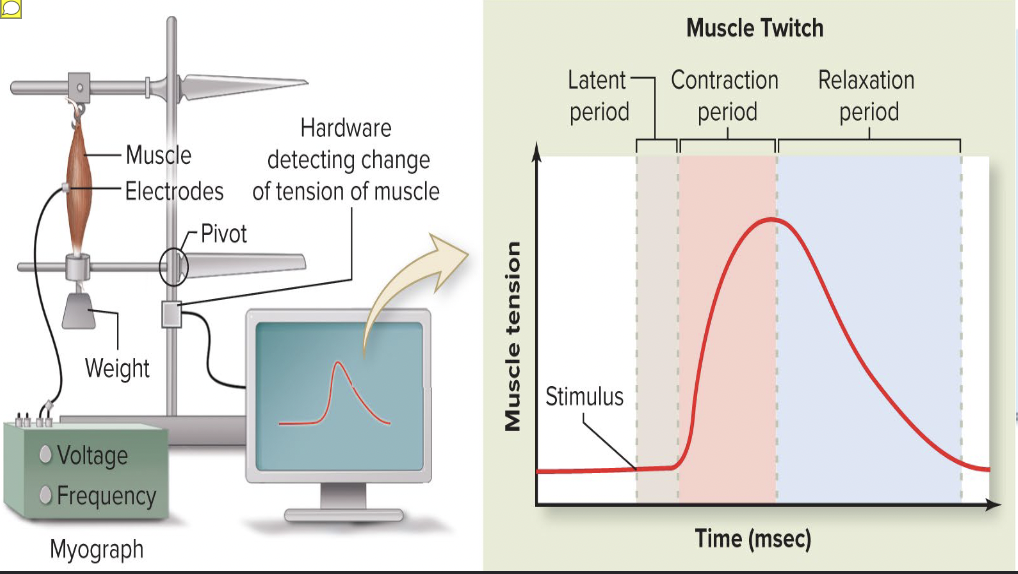
Twitch can be observed and recorded as a
myogram
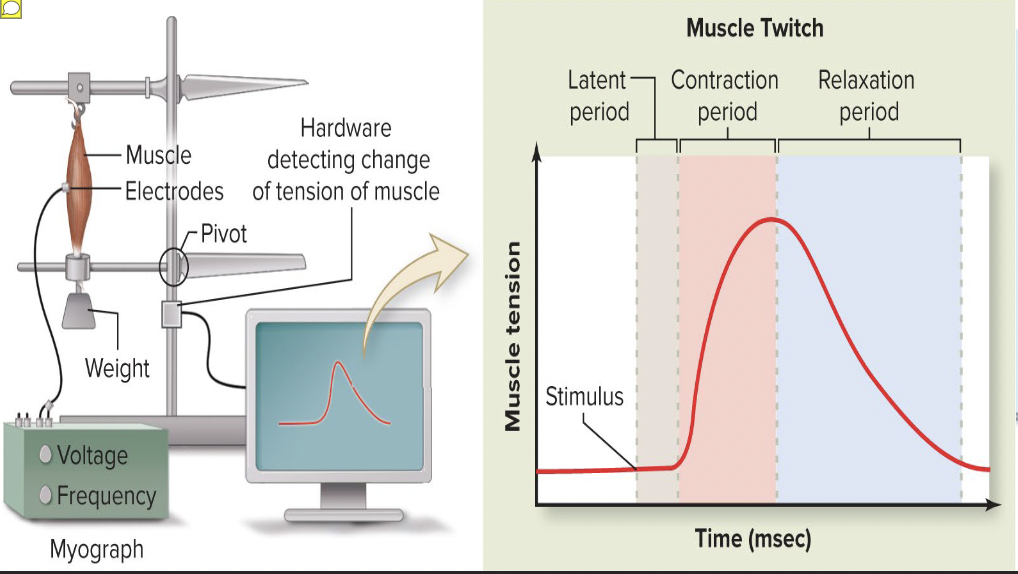
Tracing
line recording contraction activity
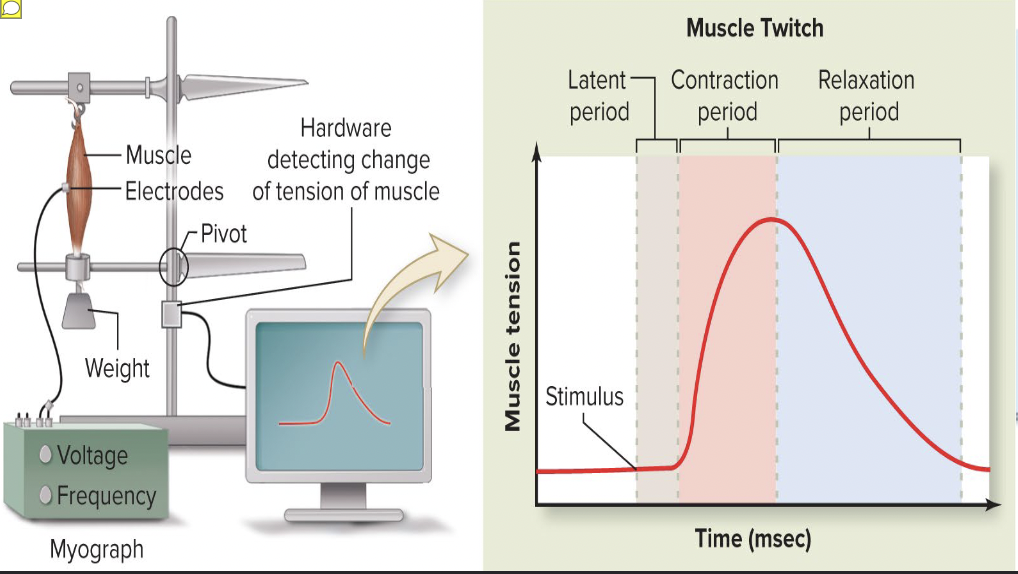
Three phases of muscle twitch
Latent period: events of excitation-contraction coupling No muscle tension seen
Period of contraction: cross bridge formation Tension increases
Period of relaxation: Ca2+ reentry into SR Tension declines to zero
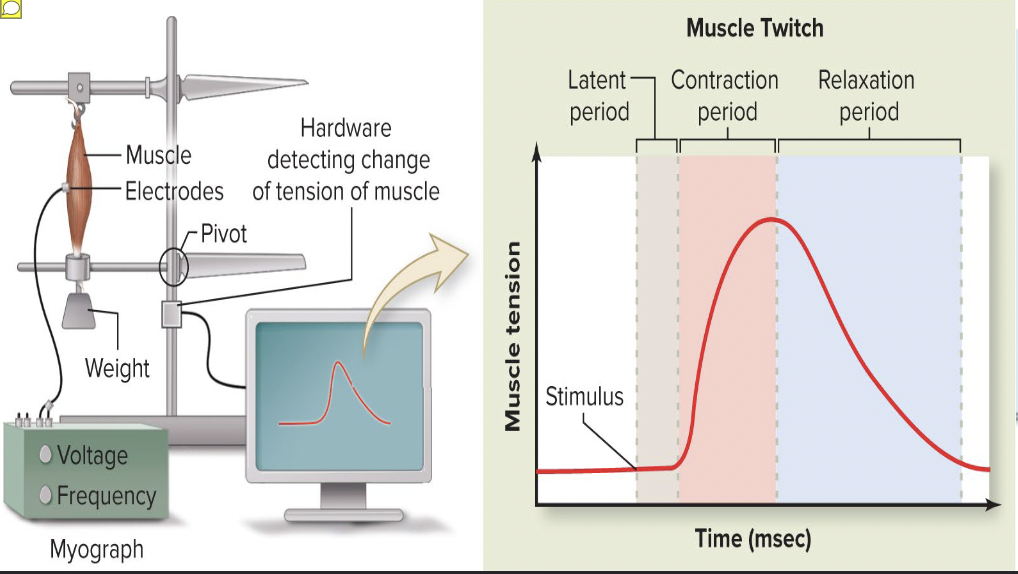
Muscle….
contracts faster than it relaxes
Differences in strength and duration of twitches are due
to variations in metabolic properties and enzymes between muscles
Example: eye muscles contraction are rapid and brief, whereas larger, fleshy muscles (calf muscles) contract more slowly and hold it longer
START ON THIS BRIEL BRIEL