Headache Classifications
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
37 Terms
Primary headache types
- migraine
- tension
- cluster
Migraine type of pain
- throbbing/stabbing
- moderate-severe
- wose w/ exertion
Tension headache type of pain
- dull and band-like tightness
- defuse pain, waxes and waines
Cluster headache-type pain
- abrupt onset
- deep, continuous
- excruciating, explosive
- stabbing quality usually near one eye
Migraine
- Location:
- Duration:
- Sx:
- Typical pt appearance:
- Location: 60-70% unilateral, often in frontotemporal region
- Duration: 4-72 h
- Sx: photo/phono-phobia, N/V, aura, sensitivity to movement
- Typical pt appearance: rest in quiet, dark room; younger female
Tension headache:
- Location:
- Duration:
- Sx:
- Typical pt appearance:
- Location: bilateral
- Duration: variable
- Sx: none, no N/V
- Typical pt appearance: can remain active or may prefer to rest (anyone)
Cluster headache:
- Location:
- Duration:
- Sx:
- Typical pt appearance:
- Location: unilateral facial pain, orbital, supraorbital or temporal pain
- Duration: 15 min-3 hr, once to multiple per day
- Sx: tearing, nasal congestion, miosis, ptosis, eyelid edema, rhinorrhea, pallor, facial sweating
- Typical pt appearance: male, smoker, restless, agitated, clutch head (ends when episode ends)
What are secondary causes of headaches?
• Head trauma
• Vascular disorders
• Infection
• Intracranial pressure (changes)
• Medications
• Metabolic disorders
• Toxic substances
• Substances of abuse
• Trauma
- Commonality for most of these causes is SERIOUS and may require medical attention to address
Secondary headache: RED FLAGS
- Acute onset of the"first" or "worst" headache ever
- Change in pattern of headaches or progressive worsening
- Onset of headache after age 50 years
- Headache associated with systemic illness (eg, fever, nausea, vomiting, stiff neck, and rash)
- Triggered by cough, exertion, Valsalva maneuver
- Abnormal neurologic exam with papilledema or change in mental status
- New-onset headache in a patient with cancer or human immunodeficiency virus (HIV) infection
Etiology of migraine
- Activation of trigeminal sensory nerves triggers the release of vasoactive neuropeptides, which interact with dural blood vessels to cause vasodilation and extravasation → inflammation
- nitric oxide, substance P, calcitonin gene-related peptide (CGRP)
- neurotransmitter release affects in other ways (serotonin in particular)
____________ mechanism provides a basis for drug targets
multi-factorial
Premonitory symptoms (Prodrome/Pre-Headache)
- anxiety, depression, euphoria, drowsiness/fatigue, hyperactivity, restlessness, irritability
- allodynia, photophobia, phonophobia, hyperosmia, difficulty concentrating
- stiff neck, thirsty, food cravings, anorexia, yawning
- polyuria, diarrhea, constipation
- about 77% of pts experience some of these warning signs hours-days before HA
Aura symptoms
- Positive features: scintillations, photopsia, teichopsia, fortification spectrum
- Negative features: scotoma, hemianopsia
- Motor/somatic: dysphagia, aphasia, weakness, hemiparesis, tingling sensation
Postdromal sx of migraine
- can occur for up to 48 hours after HA subsides
- Feel tired, exhausted, irritable, or listless. Conversely, some feel unusually refreshed or euphoric
- Impaired concentration may continue from HA
- Muscle weakness or myalgias; scalp tenderness
- Anorexia or food cravings
Risk factors for migraine
- family hx
- mood disorders
- vascular factors
- obesity
- any age, but less common w/ advancing age. first attack by age 40
- 3x more likely in women
- hormonal changes (OCPs, menstruation, preg)
- weather (changes in humidity, pressure)
- diet
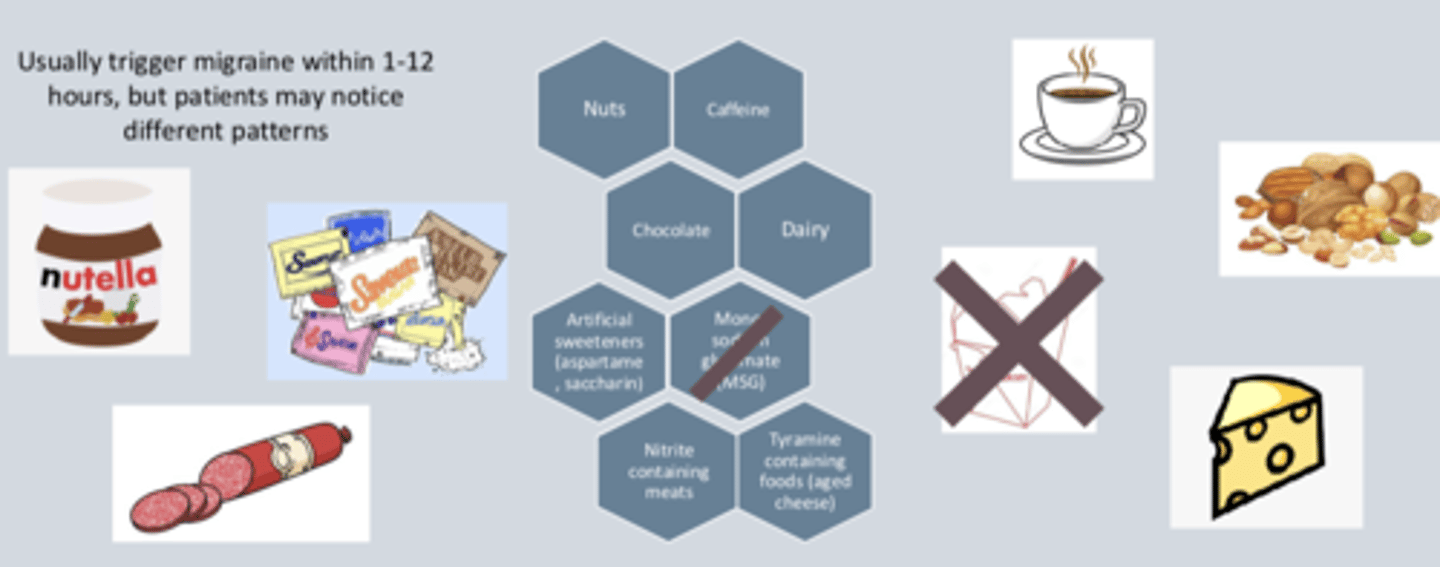
Foods that may trigger migraine
- nuts
- caffeine
- chocolate
- dairy
- artificial sweeteners (aspartame, saccharin)
- nitrate-containing meats
- tyramine-containing foods (aged cheese), fermented age/pickled foods
- alcohol
- Usually trigger migraine within 1-12 hours, but patients may notice different patterns
Environmental triggers
• Glare or flickering lights
• High altitude
• Loud noises
• Strong smells and fumes
• Tobacco smoke
• Weather change
Behavioral-physiologic triggers
• Excess or insufficient sleep
• Fatigue
• Menstruation, menopause
• Sexual activity
• Skipped meals
• Strenuous physical activity (e.g., prolonged overexertion)
• Stress or post-stress
Episodic headaches
- <15 HA days/month
- Some may be migraines, some may be tension/other types
Chronic headaches
• >15 HA days/month, for at least 3 months, (tension type and/or migraine headache)
• HAs lasting 4-72 hours
• HAs have features of migraine without aura for ≥8 days/month
Menstrual-associated headache
• Hormone-related 2 days before or first 2 days of menses
• More severe, frequent and resistant to therapy
Medication overuse headaches
• Transition from episodic to chronic
• Analgesic or triptan overuse
• Unresponsive to prevention medications
What are medication overuse headaches caused by?
- frequent use of HA medication
- use >3 times/week
- escalating use of med increases quantity/severity of HA
- withdrawal sx occur upon d/c of offending drug
Causative agents of medication overuse HA
- Analgesics, especially combination products with caffeine
- Barbiturates
- Ergotamines
- Opioids
- Triptans
How can medication overuse headaches be prevented?
When HAs are well managed, limit use of acute abortive therapy to 2-3 times/week
T/F: Tensions are the most common type of headache
TRUE
Cluster headaches are more ______________, but also most ______________________
- severe
- uncommon
Cluster headaches usually happen in...
- concentrated time frame (days to months), separated by periods of remission (months-years)
- more common at night and in spring & fall
- onset is sudden w/ pain peaking quickly and lasting 15-180 mins (3 hours)
Pain in cluster headaches
- excruciating, penetrating
- intensity near the eye or temple (unilateral)
What are cluster headaches accompanied by?
- cranial autonomic sx
- resolve when HA resolves
- potentially restlessness or agitation
Timing of cluster headaches
has been observed to happen up to 8 times a day
At least one of the following must occur in a cluster headache
◦ Conjunctival injection
◦ Lacrimation
◦ Nasal congestion
◦ Rhinorrhea
◦ Facial sweating
◦ Miosis (constriction of pupil)
◦ Ptosis
◦ Eyelid edema
What is the difference between a tension headache and a migraine? Cluster?
Migraine: throbbing, unilateral, NV, photophobia, aura
Tension: bilateral, bandlike
Cluster: unilateral, focused in one eye, nasal sx, stabbing, excruciating
What constitutes a chronic headache/migraine?
≥15 HA days/month
What are three things that can potentially trigger migraines?
- food
- hormones
- environmental
- many more
Name 2 medications that can cause medication-overuse headaches
analgesics, sumatriptan, anything used to treat migraines
(Predict) How can patients best track their headaches/migraines?
journal, diaries