Seminar 3 - transplantation and stem cells
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
Transplantation
A graft or transplant is the transfer of living tissues, organs or cells from one site to another, either within the same individual or between different individuals
Main problem of transplantation
Host’s immune system identifies donor tissue as foreign and may reject it
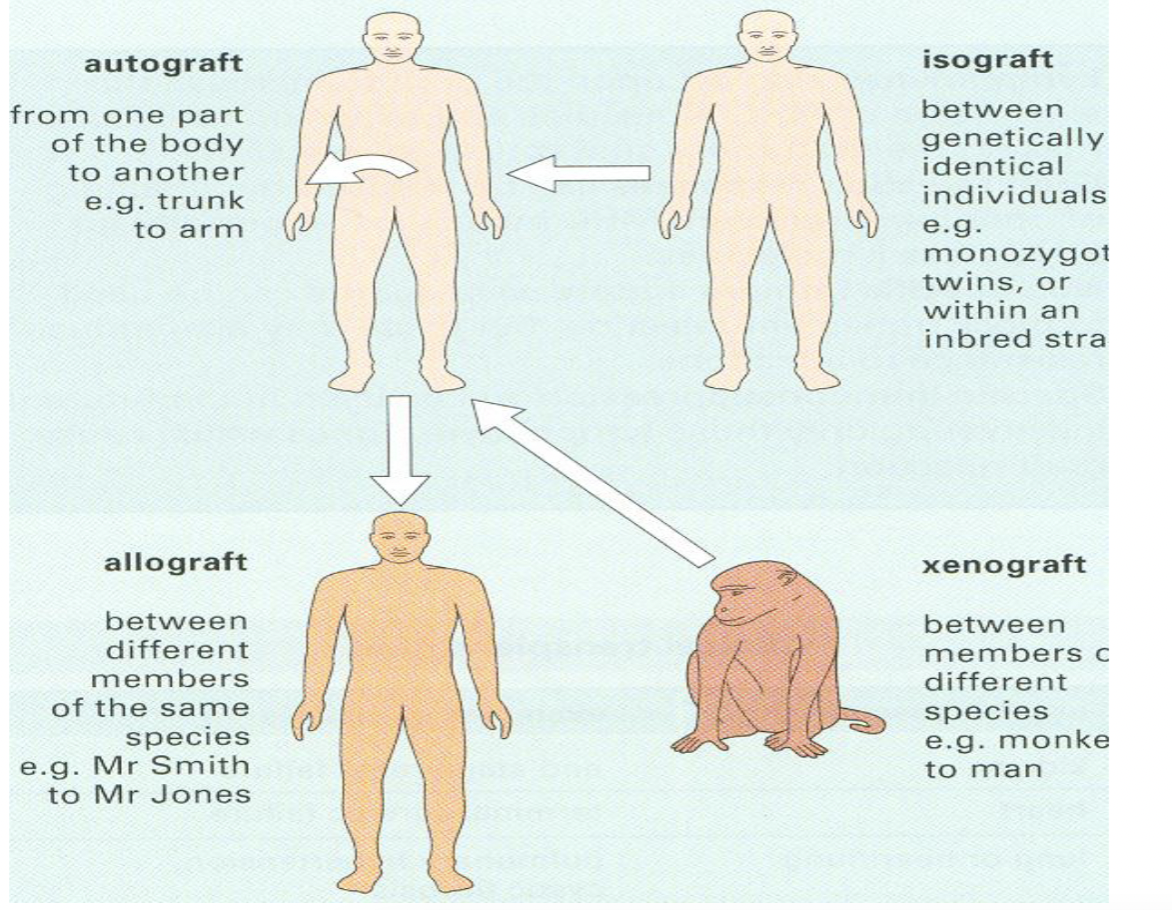
Grafts classification
Autografts - from one part of the body to another
Isografts - between isogenic individual (recipient that is genetically identical)
Allograft - between genetically different individuals from the same species
Xenograft - between members of different species (high rejection due to IgM and cell mediated immunity)
Components involved in transplant rejection
Antigen presenting cells - dendritic, macrophages and B cells, present donor antigens to recipient T cells, can migrate from graft to lymph nodes → initiating rejection
T cells - central to rejection, recognise donor MHC by recognising donor APC or recognising peptides presented by host APC
B cells and antibodies - produce antidonor antibodies that fix complement, recruit neutrophils and cause vascular injury
NK and macrophages - contribute to inflammatory response and graft damage
Alloimmunity
Immune response against donor MHC (Human leukocyte antigen - HLA)
When an organ is transplanted, recipients immune system sees the donor MHC molecules as foreign and launches immune attack
Triggers cell mediated immunity (t cells attack donor cell, activate macrophages…) and humoral (b cells produce antibodies, binds to graft blood vessels and recruit immune cells)
Alloantigens
Molecules causing immune recognition of donor tissue (MHC proteins, CD43, blood group antigens…)
Highly polymorphic → more variations → more chance of rejection
Histocompatibility antigens
MHC haplotype - set of MHC allelles inherited from each parent
Minor histocompatilitity antigens → can still cause rejection but slower
Cytokines upregulate MHC, increasing immunogenicity
Recognition of alloantigens
Direct presentation - donor MHC is directly recognised by T cells, both CD4+ and CD*+ T cells are involved
Indirect presentation - donor MHC is processed by recipient APC and presented via recipient MHC, basically processed like any foreign antigen, only involves CD4+ T cells
Experimental animals → evidence of role of T cells in rejection
Removal of thymus leads to inability to reject transplant
Removing T cells prevents rejection, adding them back restores rejection ability
Antibodies cause graft damage and macrophages are involved in inflammation
Hyperacute rejection
Minutes to hours
Caused by pre-existing antibodies in recipient
When organ is connected to recipients circulation, the antibodies immediately bind to donor endothelial cells
This activates complement system and leads to endothelial damage, platelet activation, thrombosis and necrosis of graft tissue
Irreversible and requires removal of graft
Acute rejection
Days to weeks post transplant
Type 1 - Cell mediated → CD8+ cytotoxic T cells attack graft cells directly, CD4+ helper T cells recruit macrophages, this response targets foreign MHC molecules
Type 2 - Antibody mediated → new antibodies are formed after transplant, binds to donor antigens → complement activation, inflammation and vascular injury
Can be treated
Chronic rejection
Months to years after transplantation
Slow, progressive immune response, often involves both T cells and antibodies
Can be caused by low level persistent immune activation, ischemia-reperfusion injury or repeated minor episodes of acute rejection
Resistant to treatment, may require re-transplantation
Bone marrow transplantation
For hematologic diseases (leukemis, anemia, SCID)
Recipient is immunologically suppressed before grafting
Risk - GVHD → donor bone marrow contains immunocompetent cells → graft may reject host → causes graft vs host diseases
GVHD
Occurs when donor T cells recognise recipient cells as foreign
Symptoms - diarrhea, fever, weight loss, rash, erythema, joint pain and death
Organ transplants
Kidney - diseases like diabetes and nephritis, high success and survival rate, most common
Liver - treats congenital defects and damage from viral (hepatitis) or chemical agents
Pancreas - can treat diabetes, can be combined with kidneys
Skin - used for burns, high risk of rejection due to some use of foreign skin
Xenotransplantation barriers
Natural IgM antibodies rapidly reject xenografts
What is immunosuppression
Deliberately reducing the activity of the immune system, primarily to prevent it from attacking a transplanted organ or tissue
Main immunosuppressant drugs
Cyclosporins - inhibit T cell activation (by inhibiting calcineurin - enzyme for T cell activation), prevents T cells from attacking transplant organ
Azathioprines - inhibit DNA synthesis and affect T&B cells, bone marrow suppression
Corticosteroids - like prednisone, anti inflammatory, suppress gene transcription of cytokines, reduce T cell activation and macrophage activity
Role of monoclonal antibodies in immunosuppression
Depleting immune cells (especially T cells), blocks activation pathways, inhibit cytokines, reduce inflammation and immune memory
Anti T cells antibodies target T cell markers to deplete and block T cells
IL2 receptor antagonists block receptor on activated T cells, prevent proliferation
Costimulation blockers prevent full activation of T cells
Stem cells
Undifferentiated cells with self renewal and differentiation ability
Sources - adult tissues, cord blood and embryonic tissue
Hematopoietic stem cells (HSC)
Originate in bone marrow
Differentiate into all blood cells
Used in treating leukemia, lymphoma and immune disorders
Bone marrow transplant
Involves transferring hematopoietic stem cells from a donor into recipient
The stem cells repopulate the bone marrow and restore the production of blood cells
Patient recieves high dose chemo or radiation therapy to destroy diseased or cancerous marrow, donor stem cells are then infused intravenously, cells migrate to bone marrow and engraft
Umbilical cord blood stem cells
Stem cells are harvested from the blood remaining in the placenta and umbilical cord after childbirth
They are rich in hematopoietic stem cells
Easy to collect, lower risk of GVHD (immature immune cells)
Adipose (fat derived) stem cells
Adipose tissue contains mesenchymal stem cells that can differentiate into bone, cartilage, fat and muscles
They are harvested via liposuction and are then isolated and purified in a lab
Pluripotent stem cells
Derived from inner cell mass of blastocyst and excess embryos created during IVF
They are pluripotent (into any cell type of body), can divide indefinately
Adult stem cells
Found in developed tissues throughout the body, involved in maintenance, repair and regeneration of tissues
They are multipotent (limited range of cell types, usually related to tissue of origin)
Self renewable, low risk of rejection and less tumorigenic
Mostly used for bone marrow transplants, autoimmune diseases, regenerative therapy…
Induced pluripotent stem cells (iPSC)
Adult somatic cells that are genetically reprogrammed to become pluripotent
Cloning
Making an exact genetic copy of an organism or call
Reproductive cloning (Dolly) → nucleus from somatic cell is inserted into enucleated egg, egg divides, forms embryo which is inserted in surrogate
Therapeutic cloning - used to create personalised embryonic stem cells which are genetically identical to donor
Immunology of gestation
Mentions why the fetus isn’t rejected by the mother
The placenta acts as an immunological shield by filtering anti MHC antibodies
Trophoblast is the outermost layer of fetal tissue and is in direct contact with maternal blood, it lacks strong MHC expression
Gestation
Placenta secretes neurokinin B bound to phosphocholine, this modifies how the maternal immune system perceives the placenta (helps fetus “hide”)
Fetal lymphocytic suppressor cells inhibit maternal cytotoxic T cells by inhibiting IL2 → this helps reduce the chances of immune attacks against the fetus
Trophoblast express HLA-C which highly immunogenic and helps them avoid being targed
Maternal IgG antibodies are actively transported across the placenta to provide passive immunity to the fetus
IgM antibodies (against ABO bloodtypes) are too big to cross the placenta and therefore doesnt harm the fetus