BS - 1 Ear, Oral and Eyes
1/167
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
168 Terms
Explain the process of auditory transduction
-Sound enters the ear through the external auditory canal and hits the tympanic membrane (TM), causing it to vibrate. These vibrations are transmitted through the three ossicles of the middle ear in order: malleus, incus, and stapes. The stapes pushes on the oval window, transmitting the vibrations into the inner ear as a pressure wave.
-The pressure wave enters the cochlea and first travels through the scala vestibuli, which is filled with perilymph (a fluid low in potassium). The wave then moves through the vestibular membrane, which separates the scala vestibuli from the scala media (cochlear duct).
-Once inside the scala media, which is filled with endolymph (a fluid high in potassium), the pressure wave causes the basilar membrane (located between the scala media and the scala tympani) to move. This movement causes the hair cells in the Organ of Corti to bend against the tectorial membrane. The bending of the hair cells opens potassium (K⁺) channels, allowing potassium to flow into the cells, depolarizing them.
-This depolarization triggers the release of the neurotransmitter glutamate, which excites the auditory nerve --> generates AP ---> electrical signal to the brain, where the sound is interpreted.
-The pressure wave travels through the scala tympani, which is also filled with perilymph, and is released through the round window, allowing the pressure to dissipate.
Upper chamber, filled with perilymph.
Sacala Vestibuli
Separates the scala vestibuli from the scala media.
Vestibular membrane
Middle chamber, filled with endolymph, where the hair cells in the Organ of Corti are located.
Sacla Media aka Cochlear Duct
A gelatinous membrane above the hair cells, involved in the mechanical bending of the hair cell cilia.
Tectorial membrane
Supports the hair cells; moves in response to sound waves. Located BELOW hair cells.
Basilar Membrane
Lower chamber, also filled with perilymph, through which sound pressure waves exit.
Scala tympani
Fluid high in potassium that bathes the hair cells and is responsible for generating electrical signals when the hair cells are stimulated.
endolymph (in the Scala media/cochlear duct)
Fluid that fills the scala vestibuli and scala tympani, helping transmit mechanical pressure waves.
Perilymph
The system of fluid-filled membranes, which includes the scala media (filled with endolymph) and is vital for hearing and balance.
Membranous labyrinth
Hair cells in the organ of corti have ________ on the apical membrane that are attached to the _________
Hair cells in the organ of corti have sterocilia on the apical membrane that are attached to the techtorial membrane
___________ is the sensory structure responsible for hearing within the cochlea of the inner ear.
Organ of corti
Describe the tontotopic organization of the Cochlea:
-how the ear distinguishes high and low pitched sounds
-The beginning of the cochlea (near the base, closest to the oval window) processes high-pitched sounds
- inner part of the cochlea (near the apex, the top of the spiral) processes low-pitched sounds.
Describe conductive hearing loss:
-Cause
Cause: Sound waves cannot be conducted through the middle ear due to mechanical inhibition
Describe Sensorineural hearing loss:
-Sound waves are not processed correctly
-Impaired organ of corti or its central connections (pathways to the brain)
Give some examples of conductive hearing loss:
-Cerumen impaction
-Foreign bodies
-Tumors of the middle ear
-Eustachian tube dysfunction: Problems with the tube that equalizes pressure in the ear.
-Otitis media/externa: Middle or external ear infections that cause fluid buildup, blocking sound.
-Cholesteatoma: Abnormal skin growth in the middle ear, which can erode ear structures.
-Otosclerosis: Hardening of the ligaments or bones in the ear, particularly around the stapes, limiting sound transmission.
-Carcinoma of the external auditory canal or middle ear: Cancerous growths that block sound conduction.
Otosclerosis.
-define
-does it cause conductive or SN hearing loss?
-Hardening of ligaments or bones in the ear, particularly around the stapes, limiting sound transmission.
-conductive bc its blocking transmission
Sensorineural hearing loss examples:
-Noise exposure: Long-term exposure to loud sounds can damage hair cells in the cochlea.
-Aging/Presbycusis: Age-related hearing loss due to degeneration of the inner ear structures.
-Meniere disease
-Labyrinthitis: Inflammation of the inner ear
-Ototoxicity: Damage to the inner ear caused by certain drugs (e.g., chemotherapy drugs, antibiotics like gentamicin).
-Acoustic neuroma: Benign tumor on the auditory nerve that impairs sound transmission to the brain.
-Systemic disease (e.g., Diabetes Mellitus, Paget’s disease): These diseases can cause hearing loss as a result of vascular damage or bone abnormalities.
-Congenital causes (maternal rubella, cytomegalovirus): Viral infections during pregnancy that affect fetal hearing development.
-Prematurity and traumatic delivery: Birth-related issues that may result in hearing damage.
Why do the Weber and Rene exams sometimes not work in clinic?
Bc ppl often have mixed (SN and conductive) hearing loss
Describe the components of the external ear, middle ear and inner ear:
-External: what u see externally (auricle, pinna, external auditory canal) up to AND including the tympanic membrane
-Middle: (behind the TM) Malleus, incus and stapes and the eustachian tube
-Inner: The Cochlea (hearing), Vestibule and Semicircular Canals (balance) and the Auditory nerve (carries sound signals to brain)
List some ototoxic drugs.
(memonic)
Memonic: A Little VAN May Quiet The Ears
A = Aminoglycosides (e.g., gentamicin)
L = Loop diuretics (e.g., furosemide)
V = Vancomycin
M = Macrolides (e.g., erythromycin)
Q = Quinine
T = Tobacco
E = Ethanol (alcohol)
Changes in hearing caused by aging:
Outer and middle ear changes x4
(think external ear + bones behind the TM)
1. Ceruminous glands become less active --> external ear canal drier --> cerumen impaction
2. Cartilage in the external auditory canal loses elasticity: canal thins --> less flexible, --> less effective at transmitting sound.
2. Tympanic membrane (TM) thins and loses vascularity
3. Joints of ossicles (middle ear bones) calcify: otosclerosis --> stiffens bones --> reduce ability to transmit vibration
Changes in hearing caused by aging:
Inner ear changes x4
(think chochlea)
1. Sensory Loss: The loss of hair cells and supporting cells in the cochlea
2. Neural Loss: There is a loss of afferent (sensory) neurons
3. Strial Atrophy: The stria vascularis ( the wall of scala media is responsible for concentrating K+ in the endolymph and provides nutrients for endolymph) deteriorates --> poor endolymph production --> reduces sound transmission + harder for hair cells to generate AP
4. Cochlear Degeneration: The basilar membrane and Organ of Corti --> SN hearing loss
Aging is associated with (high or low) frequency hearing loss
high
Changes in hearing loss caused by aging:
-Basilar Membrane Degeneration:
-causes high frequency hearing loss (bc high frequency sounds are typically processed at the base of the cochlea/here)
Changes in hearing caused by aging:
-Cochlear hair cell degeneration combined with the loss of auditory neurons in the spiral ganglion of the Organ of Corti leads to:
-Difficulty hearing high-pitched sounds --> difficult to understand speech
(base of cochlea = high pitched)
Changes in hearing caused by aging:
-Decreased vascularity of the cochlea and reduced function of the stria vascularis causes:
-equal loss of hearing at all frequencies and difficulty with localizing sound
(this is an issue of the entire cochlea so it affects all frequencies)
Changes in Hearing caused by aging
-Loss of cortical auditory neurons causes:
-equal loss of hearing at all frequencies and difficulty with localizing sound
(Cortical neurons in the auditory pathway help process sound once it reaches the brain--> hearing loss at all frequencies)
Inferior colliculus: located in the ______ and is a key center for __________ before the signal reaches the cortex.
Inferior colliculus: located in the midbrain and is a key center for auditory processing before the signal reaches the cortex.
How does the brain process sound from both ears to localize sound? Per brianna
-Some sound signals deccusate immediately after leaving the cochlea.
-Other sound signals stay ipsilateral
-All sound signals, whether ipsilateral or decussated, end up in the primary auditory cortex for interpretation.
-The brain uses differences in timing between signals from both ears to localize sound. --Damage to auditory cortex neurons impairs sound localization ability.
Age-related hearing loss that causes functional impairment:
Presbycusis
Etiologies of Presbycusis x4
1. Age-related degeneration: hair cell loss and stria vascularis atrophy...etc.
2. Genetic factors
3. Exposure to loud noises or ototoxic agents
4. Systemic diseases: Conditions such as diabetes can affect hearing.
Noise Trauma / Noise-Induced Hearing Loss --Pathophysiology
-Physical damage to (mostly) the outer hair cells causes sensorineural hearing loss
Describe the two ways in which one can get sensorineural hearing loss due to damage of outer hair cells:
1. Free radical formation and apoptosis: Noise exposure --> ROS --> oxidative stress --> apoptosis of hair cells
2. Glutamate excitotoxicity: Excessive release of glutamate w/ noise exposure can overstimulate and damage nerve fibers
Chronic, prolonged exposure to unhealthy/ high levels of noise (e.g., daily exposure to workplace noise or loud music) is: _____________
Noise-induced hearing loss
Acute, high-intensity noise exposure, typically from a single, extremely loud event, such as explosions, gunfire, or jet engines is ____________
noise trauma
Noise-induced hearing loss:
Permanent hearing loss can occur after continuous (chronic) exposure to noise levels of _________ or _________
-Permanent hearing loss can occur after continuous (chronic) exposure to noise levels of ≥85 dB(A) for an 8-hour period or 88 dB(A) for 4 hours.
Noise trauma:
Exposure to noise levels _______ can cause immediate noise trauma, while ________ (e.g., explosions) causes immediate and irreversible hearing loss.
(Acute/single loud event)
-Exposure to noise levels >120 dB can cause immediate noise trauma, while >140 dB (explosions) causes immediate and irreversible hearing loss.
Hearing loss often starts in the ____________ range, which corresponds to ____________ frequencies.
Hearing loss often starts in the 4 kHz to 6 kHz range, which corresponds to higher-pitched frequencies.
True or false: noise trauma and noise-induced hearing loss can both be temporary or permanent
TRUE
A hallmark of noise-induced hearing loss is difficulty hearing _______________ sounds, such as children’s voices or bird songs.
high pitched sounds
Noise trauma and noise induced hearing loss inlude the loss of certain _________ sounds that require high-frequency hearing.
-certain consonant sounds that require high-frequency hearing, such as "s," "h," "f," "th."
___________ the perception of sound when no external noise is present. It often manifests as ringing, buzzing, hissing, or other sounds in one or both ears. Tinnitus can vary in pitch (high or low), volume, and duration, and it can be temporary or chronic.
Tinnitus
Subjective tinnitus is precieved by _____________ and typically results from ___________
-precieved by only the patient
-typically results from the same conditions that cause hearing loss/abnormal nerve activity in the auditory cortex
___________ tinnitus is detectable by the clinician and typically is caused by ________________
-Objective tinnitus
-a physiologic process near the middle ear like a muscle spasm, vascular abnormalities or neurological conditions ---> a sound is being made
Is objective or subjective tinnitus more common?
Objective
Subjective Tinnitus
-pathophysiology
- not completely understood
-likely a source of dysfunction in the CNS
-Loss of cochlear input to neurons in the central auditory system (due to cochlear hair cell damage or a nerve lesion) can cause abnormal brain activity in the auditory cortex, leading to the perception of sound that isn’t there (tinnitus).
Acoustic Neuroma (AKA Vestibular Schwannoma) is usually caused by: _____________
-cell of origin: _______________
-a benign tumor of the vestibulocochlear nerve
-Schwann cells
Does acoustic neuroma more commonly develops on the vestibular portion of the nerve (responsible for balance) or the cochlear portion (responsible for hearing).
Vestibular portion of nerve (balance)
As acoustic neuroma grows it causes ___________ of the vestibulocochlear nerve and results in which sx?
-causes compression of nerve
-hearing loss and tinnitus (cochlear nerve)
-Ataxia (balance issues --> vestibular nerve)
Vestibular schwannomas are typically _________ growing tumors.
Slow growing --> symptoms can develop gradually as the tumor slowly compresses nerve fibers over time
What are the 3 etiologies of acoustic neuromas?
1. idiopathic (most common and unilateral)
2. inactivation of neurofibromatosis type 2 gene (tumor supressor gene --> usually makes protein merlin that regulate Schwann cell growth--> proliferation --> tumors (Bilateral presentation)
3. Radiation
The most common type of acoustic neuroma is idiopathic and (uni or bilateral)
Unilateral hearing loss, tinnitus and ataxia
Inactivation of neurofibramatosis type 2 gene is congenital and presents as (uni or bilateral)
bilateral hearing loss, tinnitus and ataxia
___________ is the sensation of motion, most commonly rotational motion, caused by dysfunction of the vestibular system
Vertigo!!
What are the most common peripheral causes of vertigo? (inner ear or vestibular nerve problems)
-Benign paroxysmal positional vertigo (BPPV): Caused by loose calcium crystals in the inner ear.
-Meniere's disease: Disorder causing vertigo, hearing loss, tinnitus, and ear fullness.
-Labyrinthitis: Inflammation of the inner ear, leading to vertigo and hearing loss.
-Ototoxicity: Inner ear damage from medications or chemicals.
-Acoustic neuroma: Benign tumor on the vestibulocochlear nerve causing vertigo, hearing loss, and tinnitus.
-Vestibular neuritis: Inflammation of the vestibular nerve causing sudden, severe vertigo.
What are the most common central causes of vertigo? (brain problems)
-Migraine
-Multiple sclerosis
-Cerebellar hemorrhage/infarct
-Vestibular insufficiency
-Vertebral artery dissection
______________ is caused by the displacement of otoliths/otoconia (tiny calcium crystals) in the semicircular canals of the inner ear.
not on exam
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV
-patho:
-otoliths most commonly dislodged where?
not on exam
-Normally, otoliths/otoconia crystals are located in the utricle and saccule, which detect linear motion. -When they become dislodged, they can move into the semicircular canals, particularly the posterior canal.
-As the head moves, the displaced crystals stimulate the hair cells in the semicircular canals inappropriately, causing a false sense of spinning or vertigo.
Causes of BPPV:
not on exam
-often idiopathic but it can also result from:
-Trauma (head injury).
-Vestibular neuritis (inflammation of the vestibular nerve).
-Labyrinthitis (inflammation of the inner ear).
-Meniere’s disease
BPPV clinical manifestations:
-trigger:
-timing of episodes:
not on exam
-Recurrent episodes of vertigo:
triggered by specific head movements such as rolling over in bed or tilting the head.
-Timing: The vertigo usually starts 10-15 seconds after a change in head position and lasts for less than 60 seconds.
-Feelings of imbalance: can persist for several hours after the episode.
-Nystagmus
Meniere's disease
-patho:
-Sx:
-Altered endolymph homeostasis:
injury or insult to inner ear leads to endolymphatic hydrops (excess fuid)
-possibly endolymph over-production, malabsorption or both ---> excess fluid --> affects the ionic composition of the fluid --> interferes with signal transduction --> vertigo (often associated with nausea and vomiting) and hearing loss, tinnitus, aural fullness
Meniere's disease is usually (uni or bilateral) and starts as:
-unilateral
-starts out fluctuating and at lower frequencies then progresses
Causes of Meniere's Disease:
-Viral infections (e.g., recent viral illnesses may trigger episodes).
Trauma to the inner ear or head.
Vascular factors that affect blood supply to the inner ear.
Endocrine disorders, such as hypothyroidism
Allergies
Genetics
Meniere's Disease: episode lasts
-minutes to hours to days (longer than BPPV that lasts LESS than 60 secs)
___________ refers to inflammation of the vestibular portion of the 8th cranial nerve, which can affect balance and lead to vertigo.
Vestibular neuritis (or neuronitis)
Vestibular neuritis (neuronitis)
-patho
-Inflammation of the vestibular nerve, often due to a viral or post-viral cause.
-HSV (Herpes Simplex Virus)
-VZV (Varicella-Zoster Virus)
-EBV (Epstein-Barr Virus)
-Influenza
-It can also be autoimmune in nature.
Vestibular neuritis (neuronitis)
-clinical manifestations
-Vertigo: can last from several hours up to several days.
-Nausea and vomiting (N/V)
-Gait instability: Difficulty with walking due to balance disturbances.
-Nystagmus
labyrinthitis
-patho:
-etiology:
-Inflammation of the membranous labyrinth
-Viral infections: Often preceded by an upper respiratory infection (URI). Common viruses include Varicella Zoster and Cytomegalovirus (CMV).
Bacterial infections: Can be caused by complications like otitis media (middle ear infection), meningitis, or cholesteatoma.
Autoimmune disorders: May also lead to labyrinthitis.
Labyrinthitis clinical presentation
-Acute onset of severe, continuous vertigo: Differentiates it from vestibular neuritis, which may have intermittent vertigo.
-Hearing loss
-Tinnitus
-Gait instability
-Nausea and vomiting (N/V)
BPPV
-duration of vertigo
-associated hearing loss and tinnitus
-seconds
-no
Meniere's Disease
-duration of vertigo
-associated hearing loss and tinnitus
-hours to days
-yes
Vestibular Neuritis
-duration of vertigo
-associated hearing loss and tinnitus
-days to weeks
-no
Labyrinthitis
-duration of vertigo
-associated hearing loss and tinnitus
-days to weeks
-yes
Which vertigo disorder is triggered by movement?
BPPV
Which cranial nerve is affected by an acoustic neuroma?
CN VIII
Which 2 disorders that cause vertigo are associated with hearing loss and tinnitus?
-Meniere's disease
-labyrinthitis
Which disorder is vertigo causes by endolymph hydrops?
Meniere's
Labyrinthitis is typically caused by a _________
viral infection
What cells are responsible for causing an acoustic neuroma?
Schwann cells
______________________ are painful inflammatory lesions on non=keratonized oral mucous membranes
Aphthous ulcer
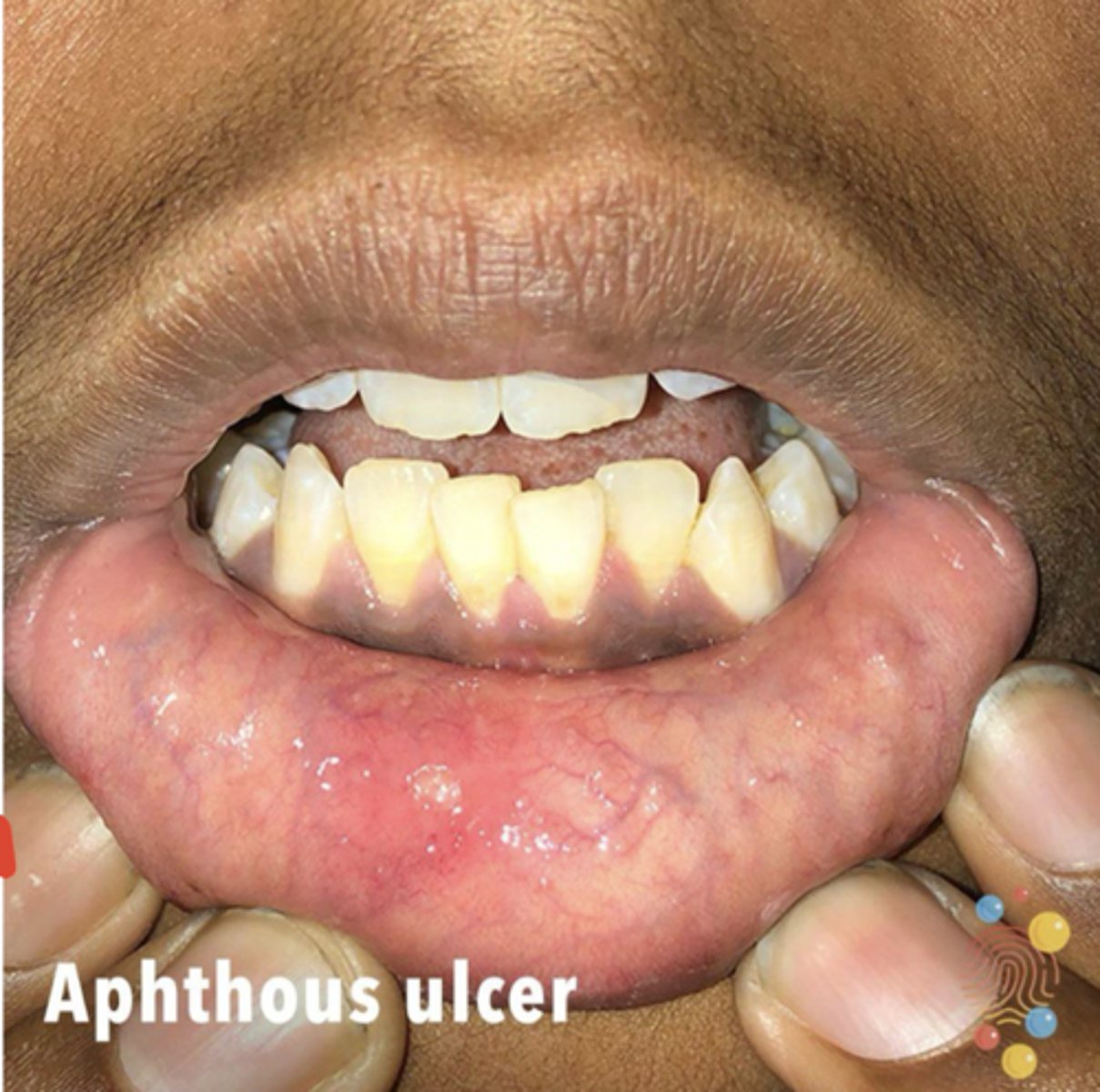
Aphthous ulcers are thought to be ______________ related
Autoimmune-related (cell mediated aka type IV hypersensitivity reaction)
aphthous ulcers
-risk factors: x3
-etiologies: x3
Risk factors:
-injuries/trauma
-stress/anxiety
-tabbacco smoking cessation--> inflamm response as immune supression improves
Etiologies:
-nutritional deficiencies (iron, folate, cobalmin)
-imflamm bowel disease
-immune deficiencies
Pathophysiology of plaque formation in conditions like gingivitis, periodontitis, and dental caries
-biofilm made up of bacteria make a slime layer
-bacteria in biofilm ferment carbohydrates (from food), producing acidic byproducts --> drop in pH --> mineral loss --> dental caries
-biofilm also triggers an inflammatory response --> gingivitis and periodontitis.
Steps of plaque formation: x6
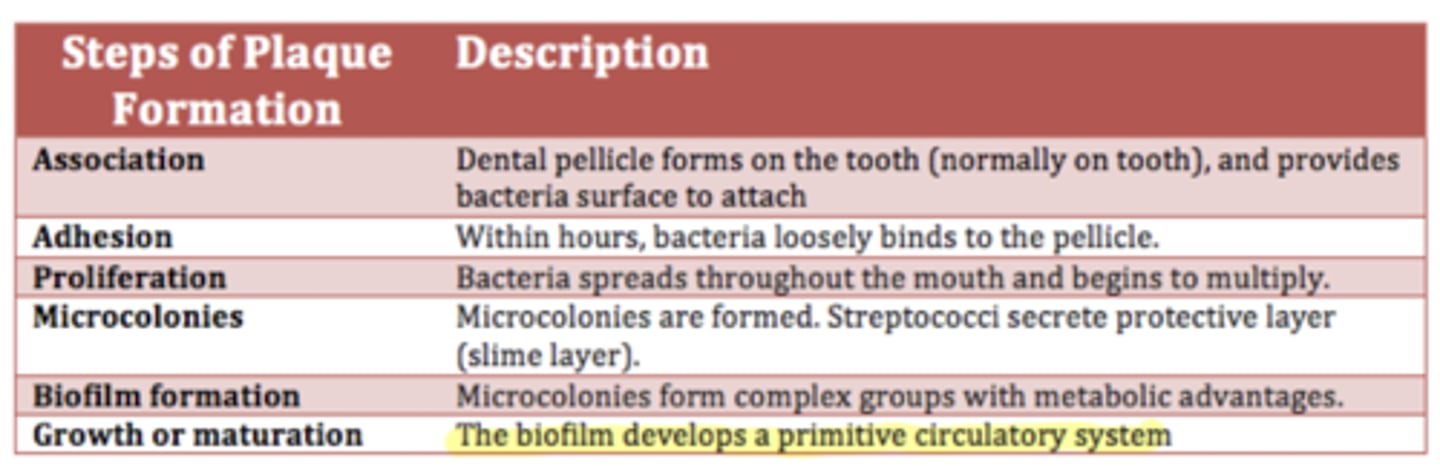
gingivitis, periodontitis, and dental caries/abscess
-risk factors: (many!)
-increasing age
-diet high in carbs
-poor oral hygiene
-smoking and tobacco use
-methemphetmaine use
-other medical conditions: Bulimia, CVD, DM, RA
-lower socioeconomic status
-infants: bottle feeding/feeding infant laying down
Describe the etiology and pathophysiology for:
dental caries
-The primary cause of dental caries is bacterial plaque --> acid byproducts from fermentation of carbohydrates --> decreased pH --> demineralizes enamel --> earliest signs are white lines --> change in color to brown = cavity advanced into deeper enamel
-usually caused by aerobic bacteria

Describe the etiology and pathophysiology + SX for:
gingivitis
-gingivitis is the body's immune response to bacterial accumulation (plaque/biofilm) along the gumline --> plaque hardens --> tartar --> resulting in inflammation, swelling, and potential bleeding of the gums, which can be reversed if addressed early.
-Affects ONLY gums
-anaerobic bacteria
-SX: Red, swollen gums, easy bleeding, no pain, and no deep pockets.

Describe the etiology and pathophysiology +SX for:
periodontal disease.
-progression from untreated gingivitis
-non-reversible
- caused by anaerobic bacteria
-more severe and chronic condition that involves infection of the deeper tissues, including bone, and can lead to permanent damage and tooth loss if untreated
-SX: receding gums, formation of deep pockets, tooth mobility, and eventually tooth loss.

Describe the etiology and pathophysiology +SX for:
dental abscesses
-localized infection at the root of a tooth or in the surrounding gum tissue
-progression of untreated infections (dental caries or periodontal disease) that have extended to deeper tissues, resulting in pus formation
-Anaerobic bacteria are often implicated in abscesses, similar to periodontitis.

Oral Leukoplakia
-patho:
-risk factors:
-patho: poorly understood
-Intermediate stage in oral carcinogenesis.
-Hyperkeratosis of the epithelium (thickening of the outer layer of cells)
-Inflammatory infiltrates (immune cells) in the tissue.
-Various levels of epithelial dysplasia
-Multiple genetic mutations
-Risk factors:
-tobacco use
-alcohol use
-candidiasis infection
*cannot be scraped off*

Oropharyngeal cancer
-patho:
-etiology x 4:
-Patho: SCC is the most common type, making up 90% of oropharyngeal cancers.
-Multiple genetic mutations: TP53 (tumor suppressor gene) and RAS (oncogene)
-Etiology:
1. Chronic alcohol use: Produces acetaldehyde --> free radicals --> damage cells --> carcinogenesis.
2. Tobacco use: direct cellular damage + decreases saliva's antioxidant capacity --> reducing the mouth’s natural defenses against cancer
3. HPV infection: strongly associated with oropharyngeal cancers
4. Immune deficiency states: Conditions that weaken the immune system, such as HIV/AIDS, can also increase the risk of cancer development.

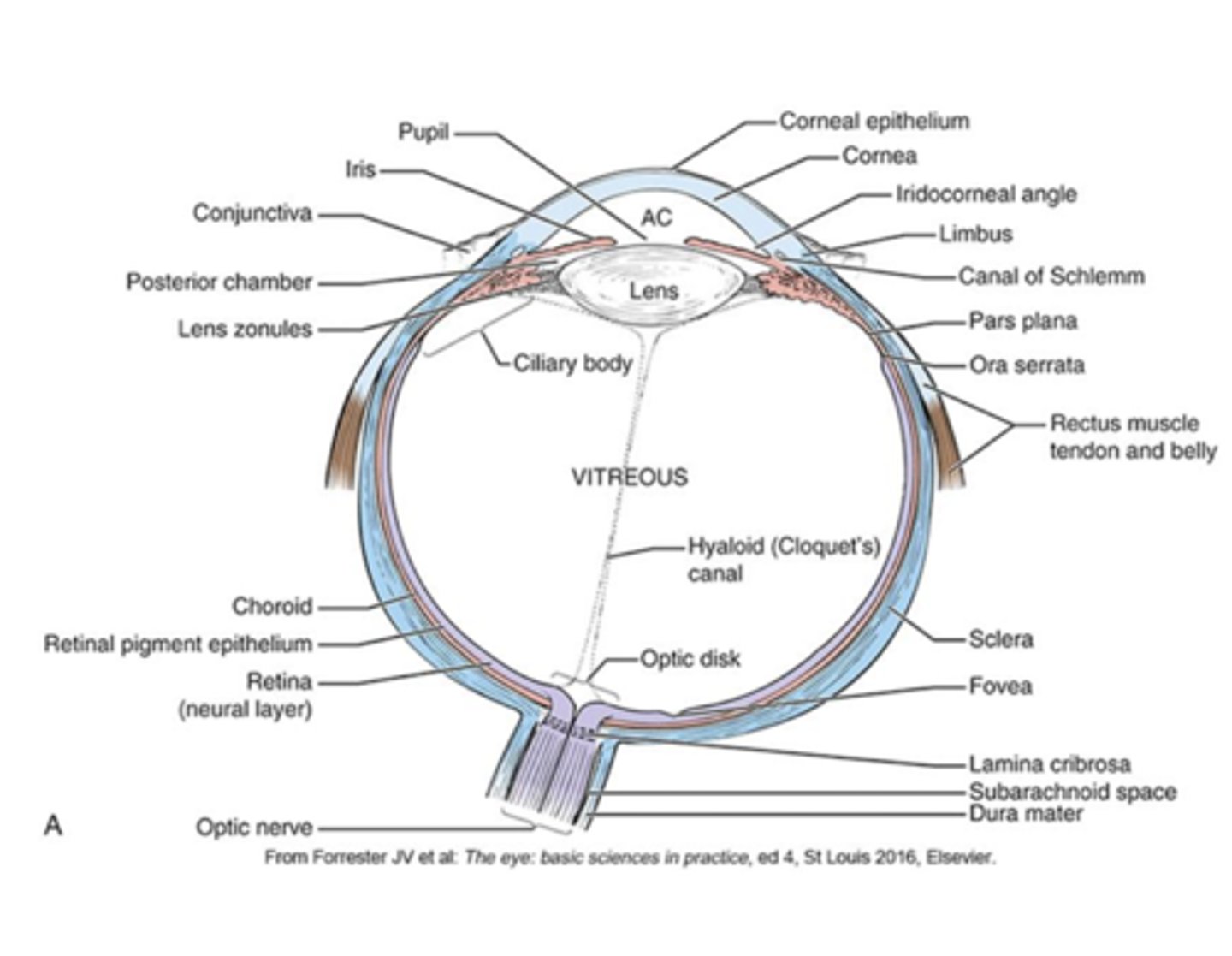
The outer, white part of the eye. It is continuous with the cornea at the front of the eye but becomes transparent in the cornea to allow light to enter.
Sclera
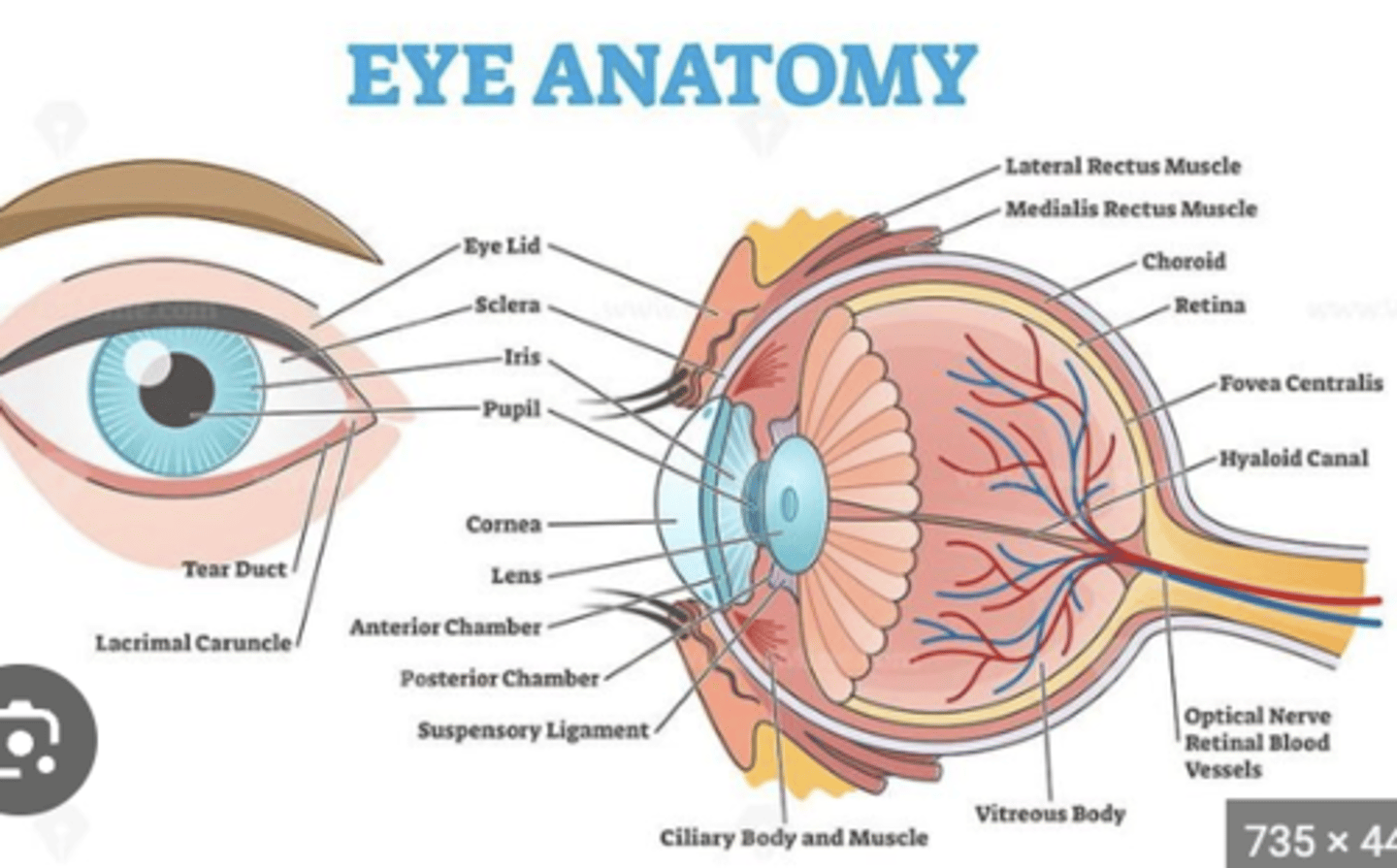
The transparent, dome-shaped front part of the eye that covers the iris and pupil. It is the first structure that light passes through when entering the eye
cornea
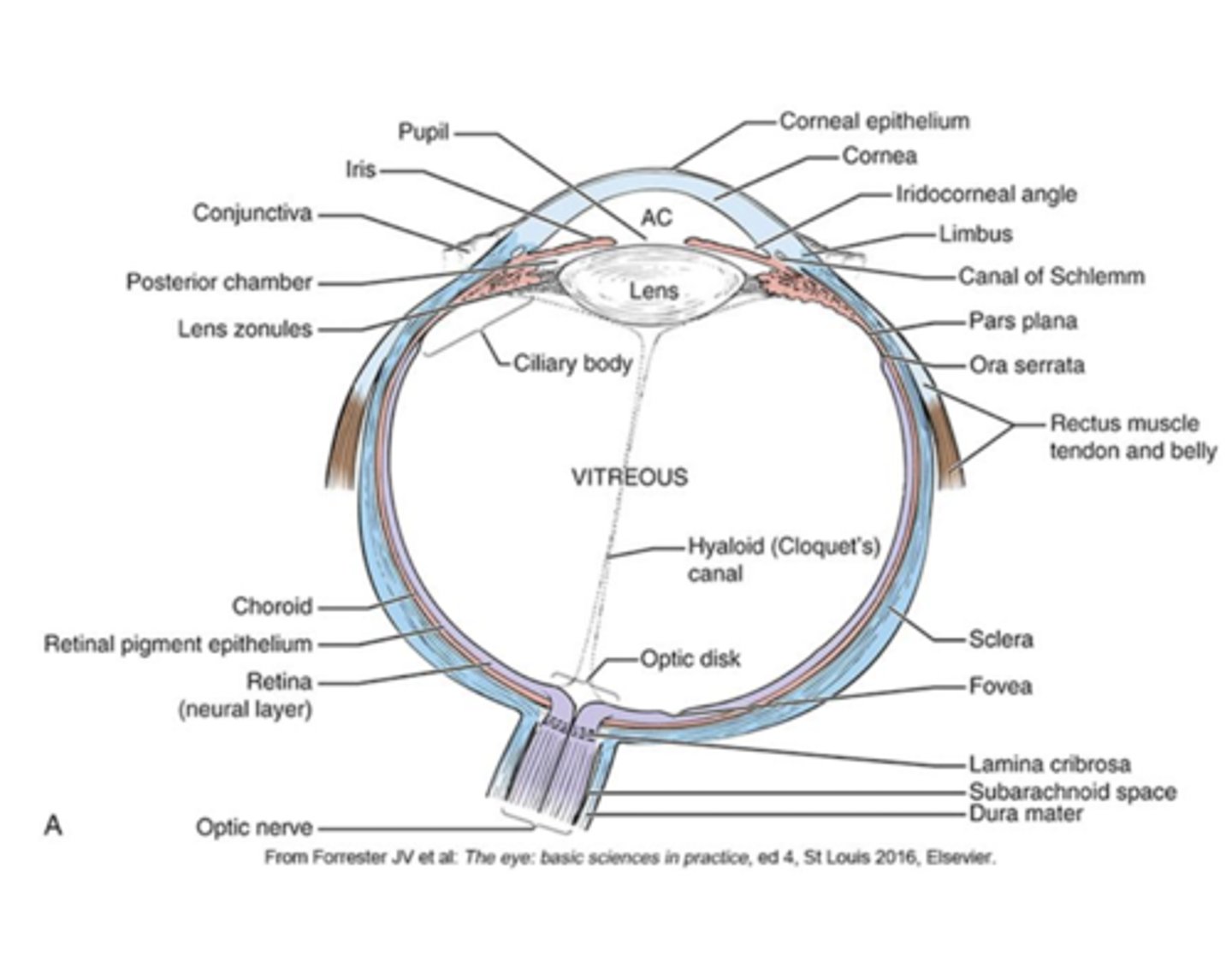
The dark, circular opening in the center of the iris that allows light to enter the eye. Its diameter is determined by the iris, which adjusts the amount of light that enters the eye.
Pupil
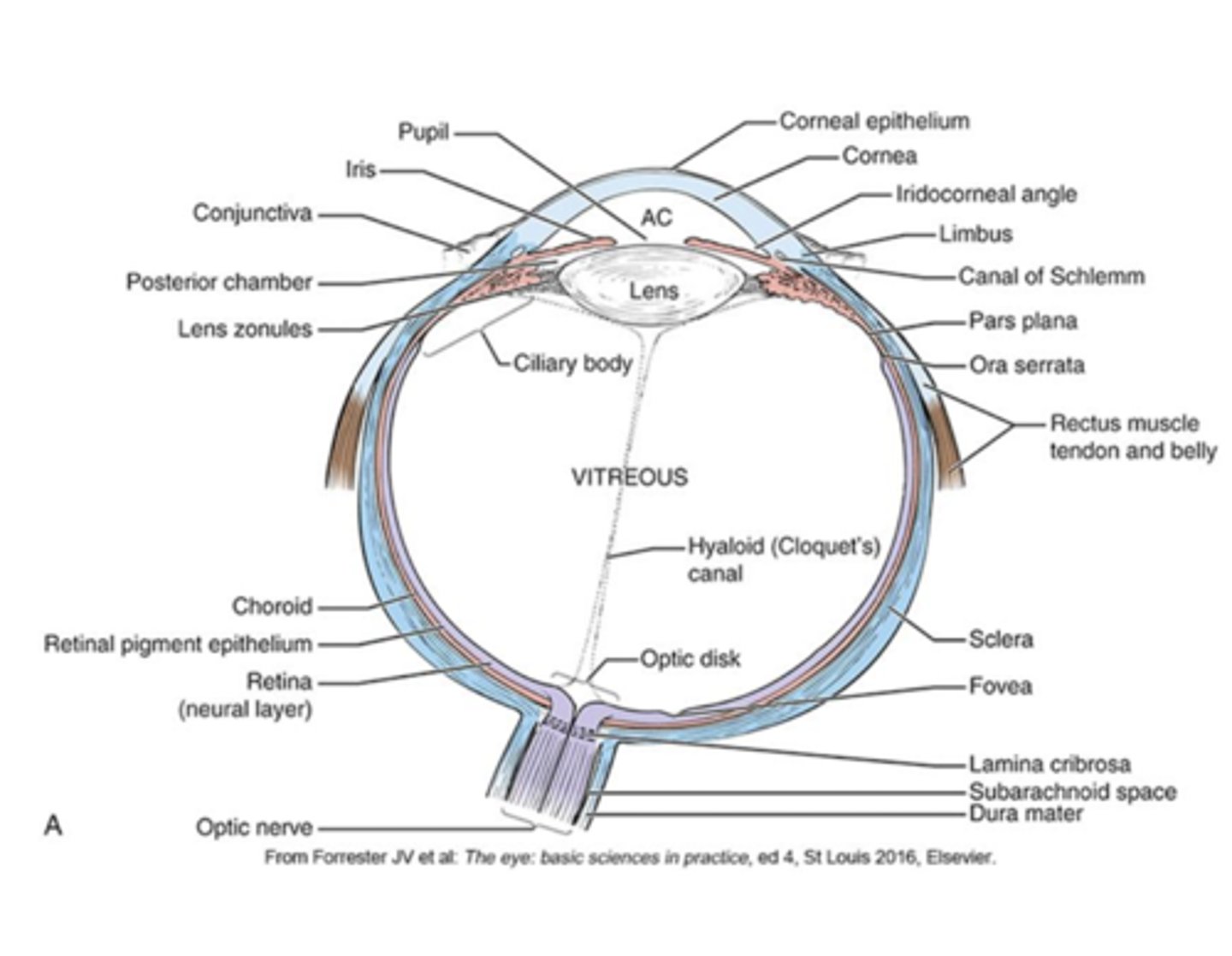
The colored part of the eye, responsible for controlling the size of the pupil. It contracts or relaxes to adjust the amount of light entering the eye
iris
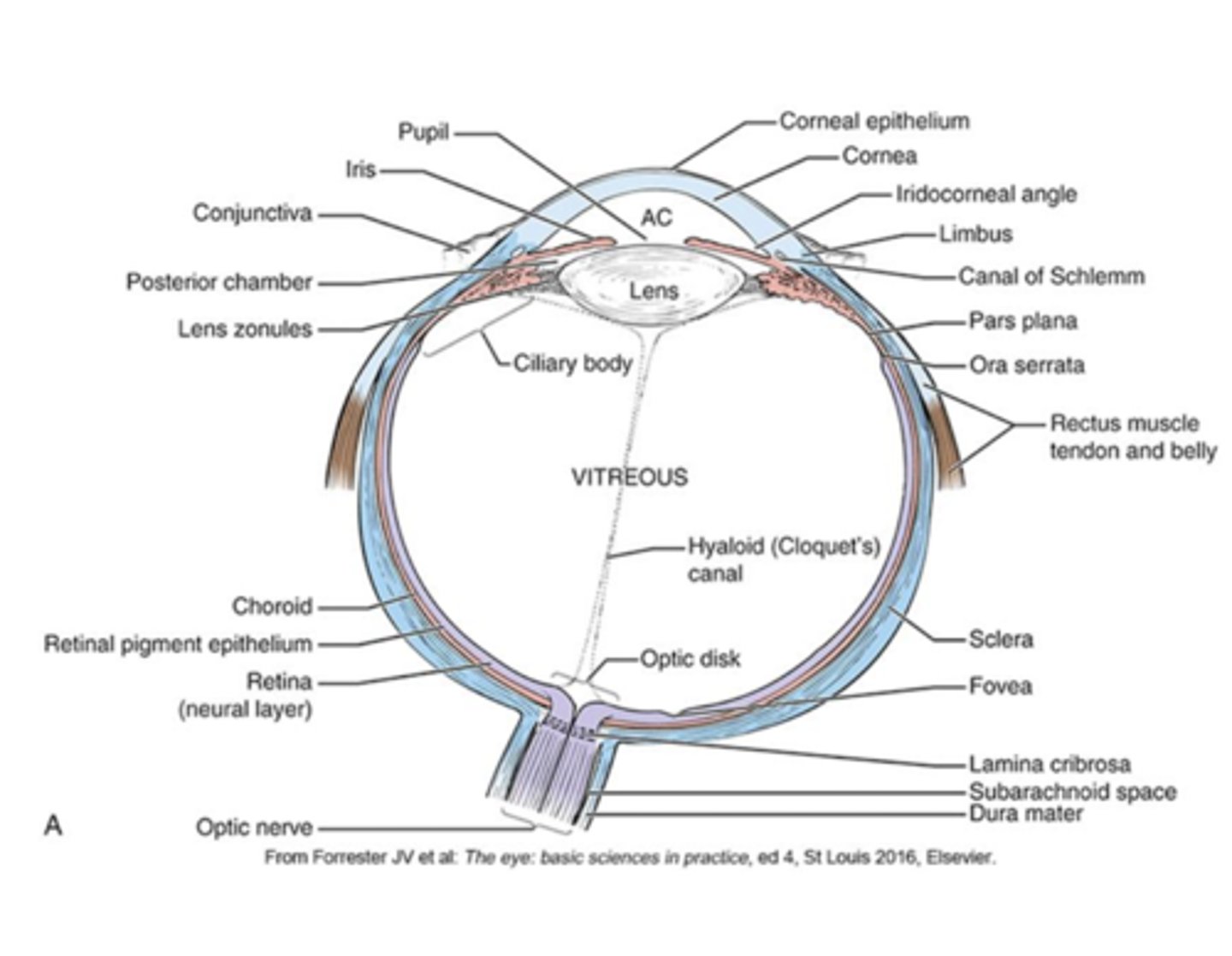
Positioned behind the iris and pupil, the _____ focuses light onto the retina.
lens
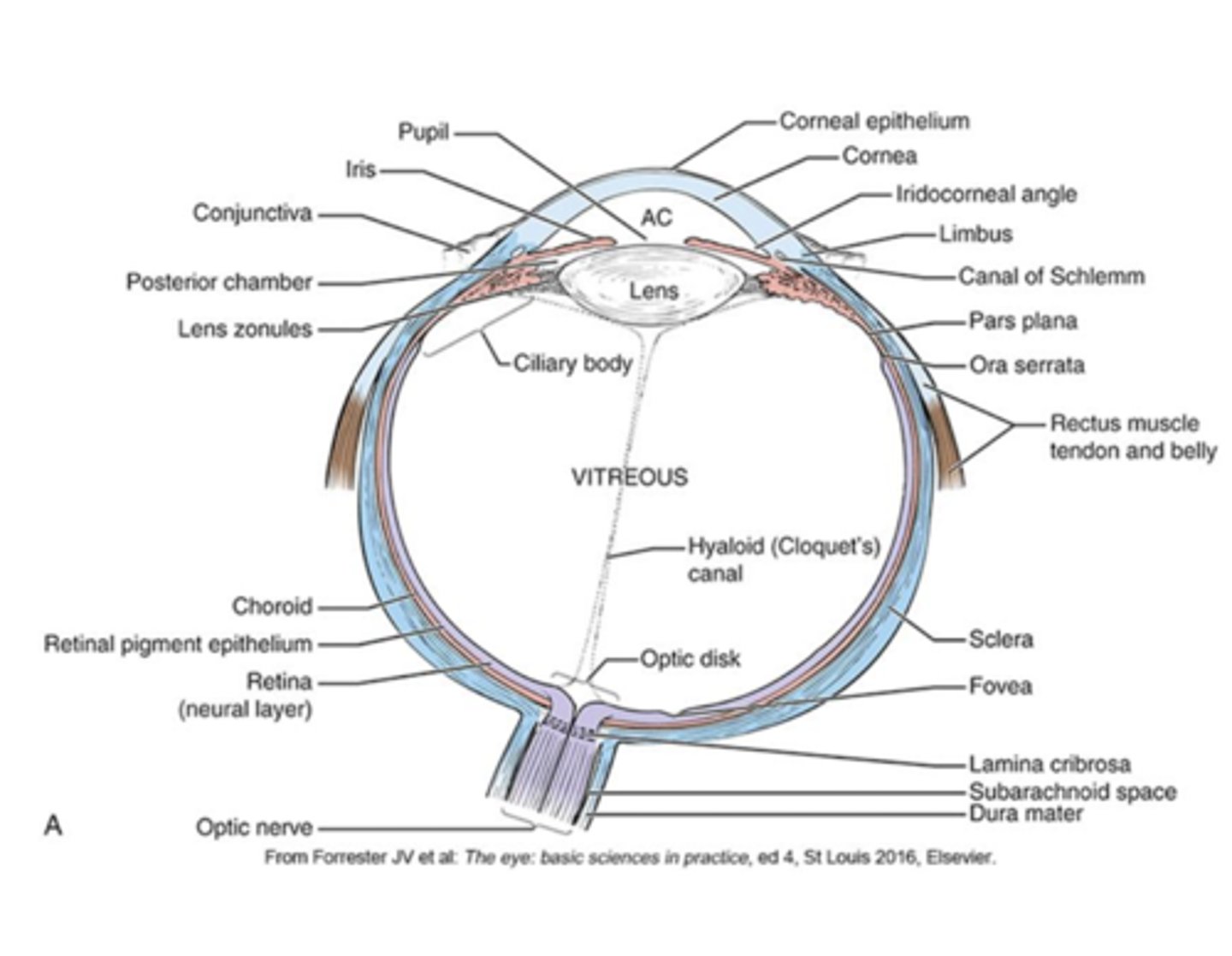
The _________ control the shape of the lens, allowing it to adjust for seeing objects at different distances (a process known as accommodation).
ciliary muscles
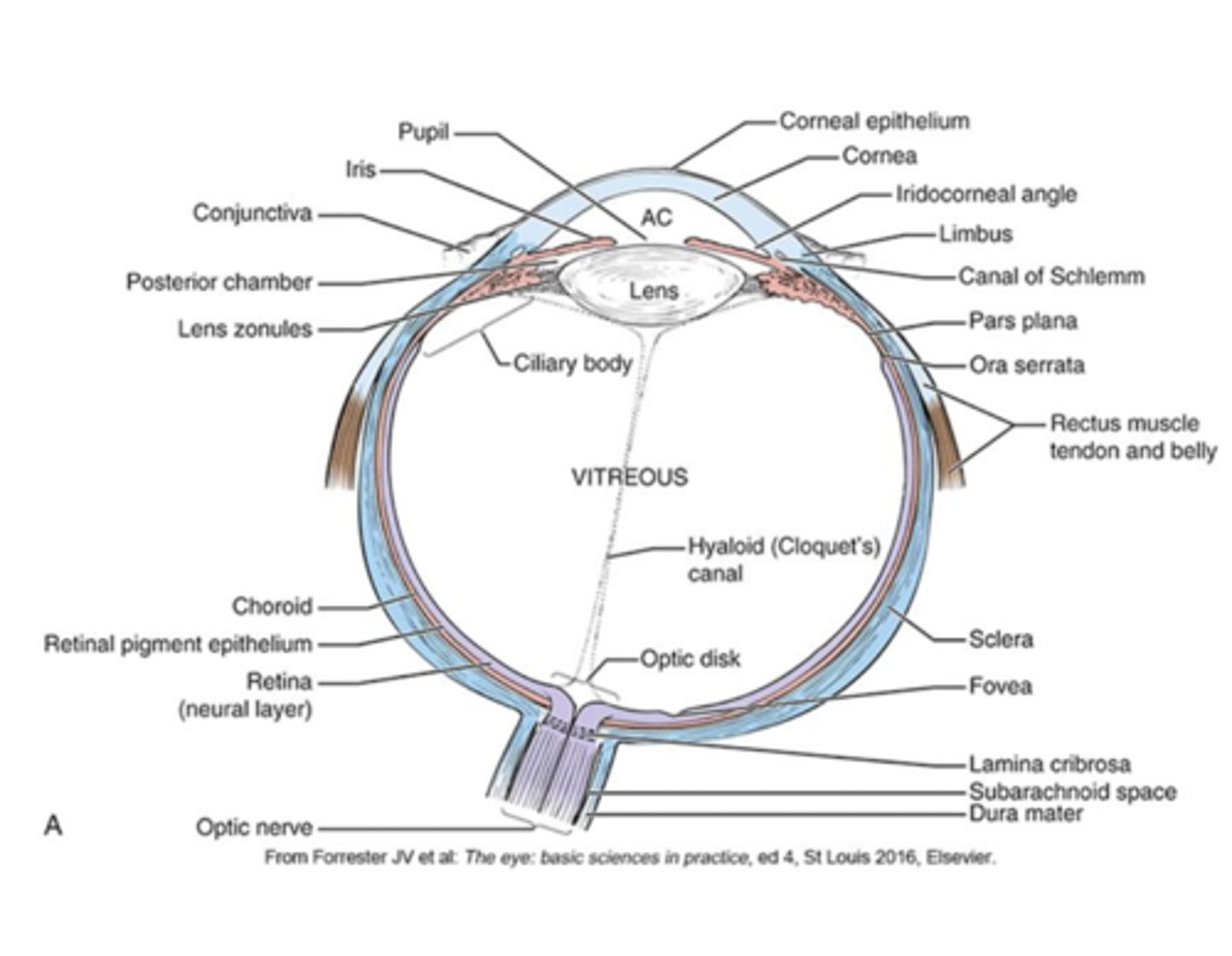
This structure produces aqueous humor, the clear fluid that fills the anterior and posterior chambers of the eye. It also contains the ciliary muscles that control the shape of the lens.
ciliary body
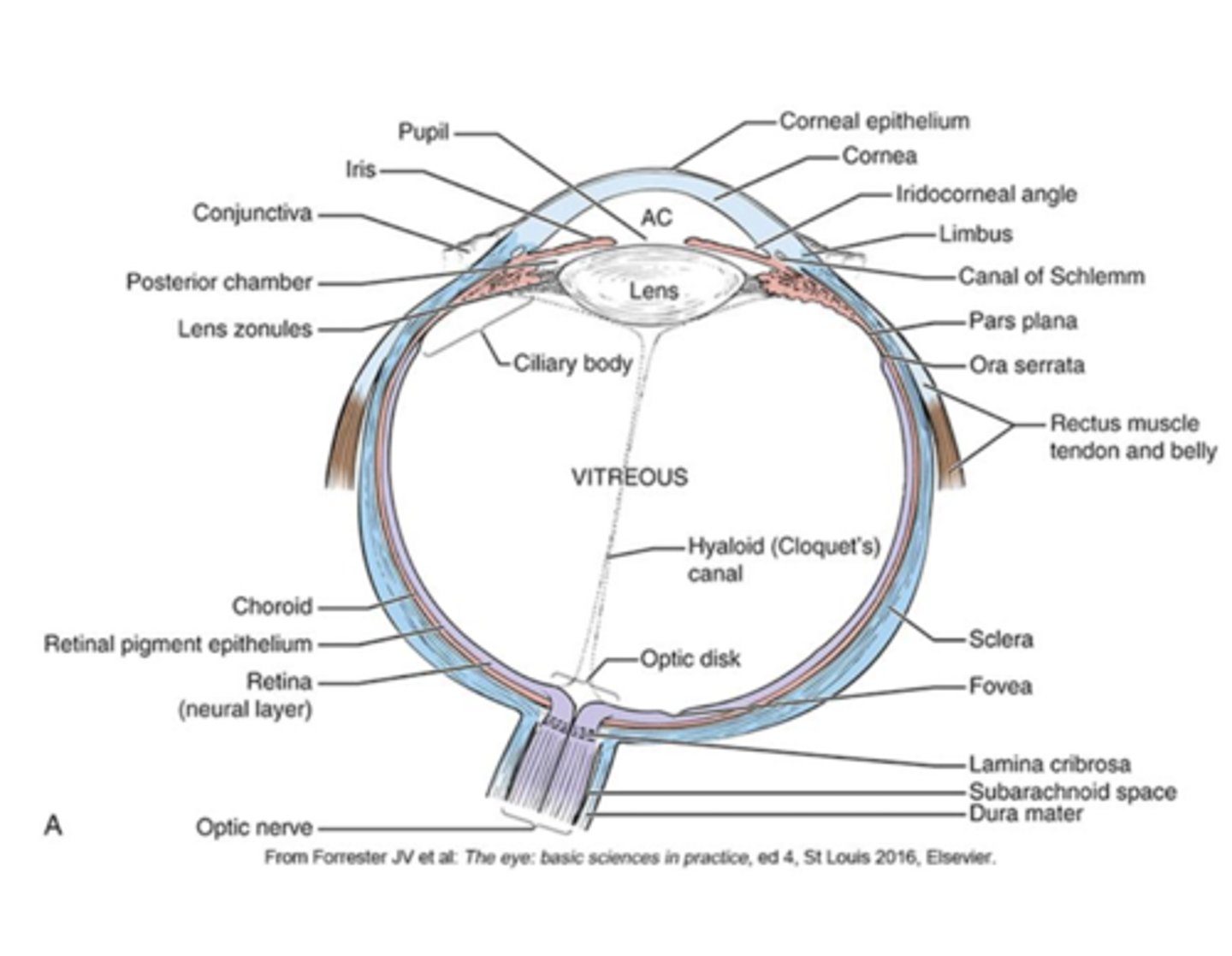
Anterior and Posterior Chambers: These chambers are filled with _____________. The _________ chamber is between the cornea and the iris, and the _______ chamber is between the iris and the lens.
-aqueous humor
-anterior
-posterior