Psychosis & Schizophrenia
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
35 Terms
What are some different characteristics of psychosis?
1. Hallucinations (can be through sight, smell, sound, taste, touch)
2. Delusions
3. Confused and disturbed thoughts
4. Lack of insight and self-awareness (unaware that the delusions or hallucinations aren't real)
What are different causes of psychosis?
- Alzheimer's, Parkinson's, Huntington's diseases
- Depression, bipolar disorder
- Some types of epilepsy
Stress, trauma
- Lack of sleep
- Drugs
- Schizophrenia
What does the word schizophrenia mean?
Schizophrenia literally means "split mind".
This describes the difference between external reality and internal thought (what is happening vs what is believed by the mind to be happening).
It does NOT mean split/ multiple personalities
What are positive symptoms in schizophrenia?
An increase in abnormal active behaviours
Give examples of positive symptoms
- Hallucinations
- Delusions
- Disordered thoughts
- Disturbed speech
What are negative symptoms in schizophrenia?
The absence of normal active behaviours
Give examples of negative symptoms
- Affective blunting (not experiencing great happiness or great sadness)
- Avolition (lack of motivation)
- Anhedonia (inability to feel joy from activities which normal cause enjoyment)
- Poverty of speech
- Social withdrawal
- Neglect of hygiene
What are cognitive symptoms in schizophrenia?
The disturbance of of normal thought processes.
Give examples of cognitive symptoms
- Poor executive function
- Poor decision making
- Poor cognitive flexibility
- Recognition deficits
- Memory problems
- Attention deficits
What is schizophrenia?
A mental illness where it is hard to discern between what is an isn't real.
When is a schizophrenia diagnosis considered?
When a patient has had at least 2 psychotic episodes
Describe the aetiology of schizophrenia
It's exact aetiology isn't known but it is known that genetics and environment play a huge rule.
1. Genetic
- Evidence: In monozygotic twins (identical twins), if one twin has schizophrenia then, there is a 50% chance the other twin will have schizophrenia
- Many genes have been implicated in it, unsure what specific genes are important.
2. Environmental
Some correlate with schizophrenia, most in childhood e.g.
- Psychosocial factors e.g. dysfunction/ challenging family environments
- pregnancy and delivery complications
- prenatal and childhood virus infection
- urban birth and residence
At what age does schizophrenia normally present?
Schizophrenia tends to show at the end of adolescence (late teens early twenties).
Describe how schizophrenia may manifest
A combination of genetic predisposition and environmental insult lead to neurodevelopment defects. This can cause structural abnormalities in the brain. These then lead to functional abnormalities shown through the cognitive, positive and negative symptoms of schizophrenia.
Describe structural changes in the brain in schizophrenic patients
In an MRI scan it shows there are differences in brain activity and gross structural differences when comparing the brain of a schizophrenic and non-schizophrenic patient.
There is/are
- enlarged ventricles in schizophrenia
- loss of neuronal tissue
Describe the relationship between schizophrenia and dopamine
The idea that dopamine was related to schizophrenia first came about because psychostimulants (e.g. cocaine and amphetamine) was shown to cause psychosis and increase dopamine. Also, all antipsychotics are all D2 receptor antagonists
In schizophrenia there could be a dopamine D2 receptor polymorphism - risk factor in schizophrenia.
There is evidence that an increase in activation of D2 receptors are likely linked to positive symptoms of schizophrenia.
Patients with schizophrenia also have decreased D1 receptors. This is likely to give rise to negative and cognitive symptoms
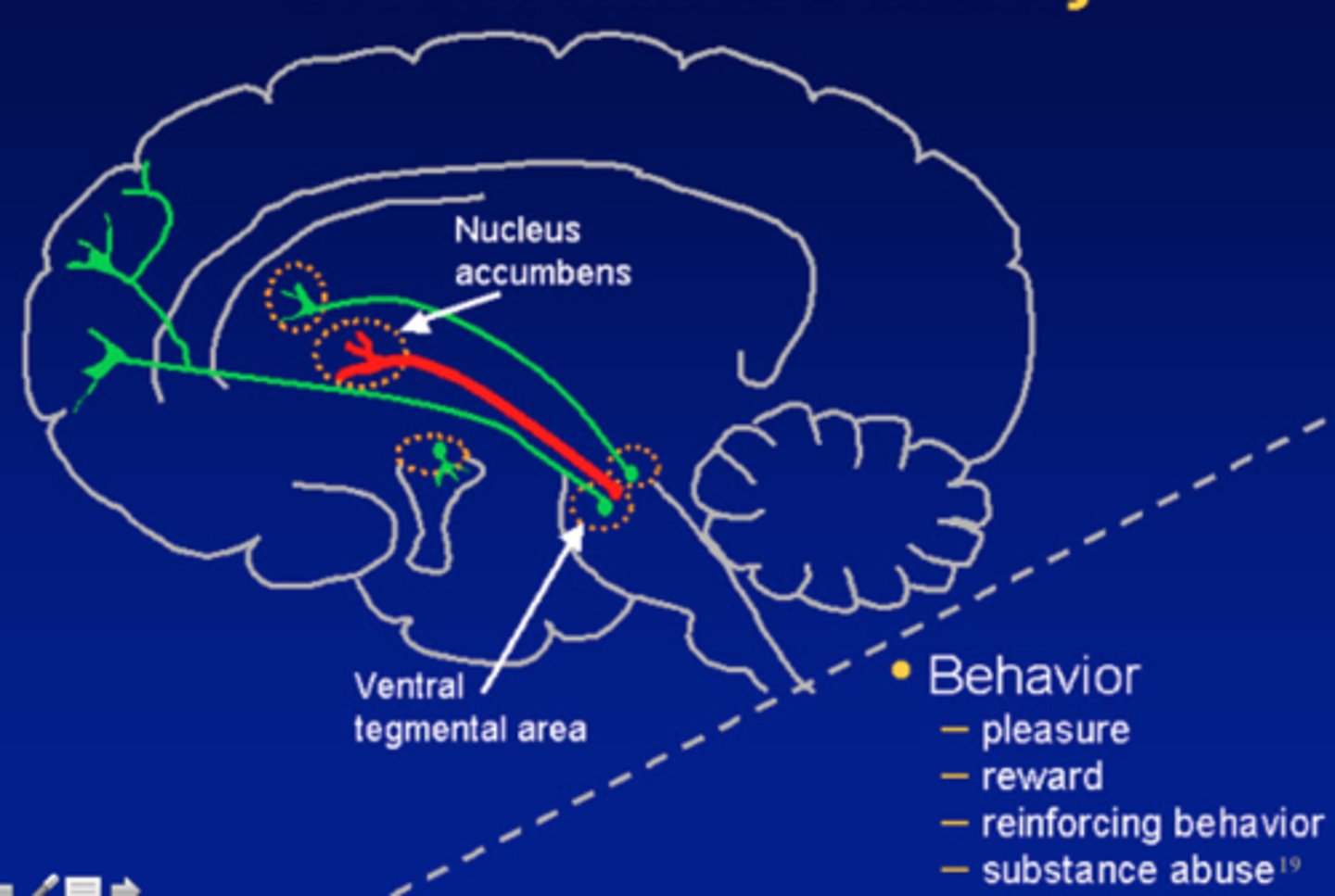
What pathways seem to be implicated in schizophrenia?
1. Mesolimbic pathway (reward pathway) - increased D2 receptor activity
2. Mesocortical pathway - decreased D1 receptor activity
There is no change in the nigro-striatal pathway in people with schizophrenia compared to people without schizophrenia.
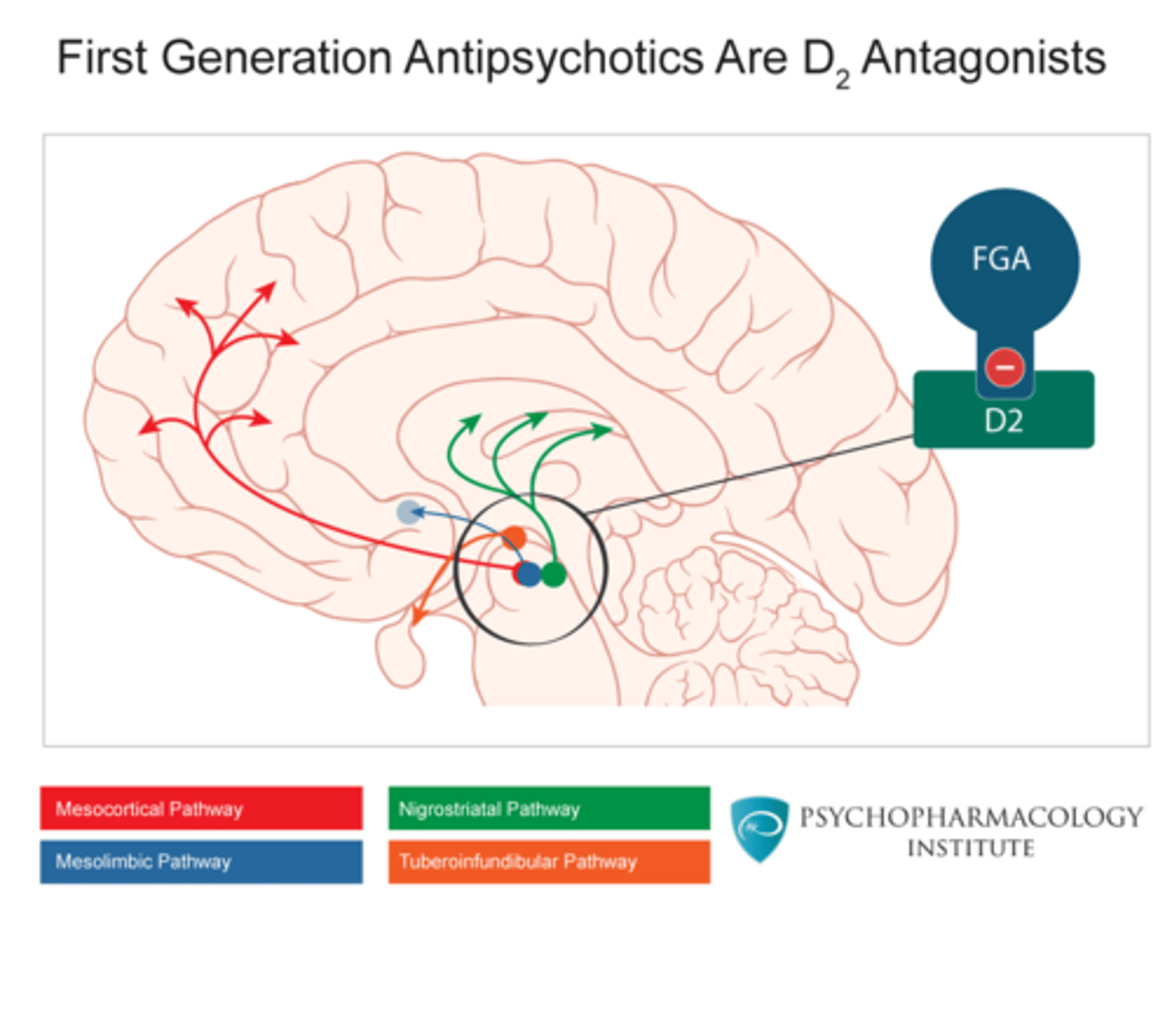
What is the mechanism of typical (1st generation) antipsychotics?
They are high affinity D2 antagonists.
They block D2 receptors in nucleus accumbens because people with schizophrenia have overactivity in D2 receptors.
- reduces positive symptoms in schizophrenia
Give examples of typical antipsychotics
Chlorpromazine and haloperidol
What are side effects of typical antipsychotics?
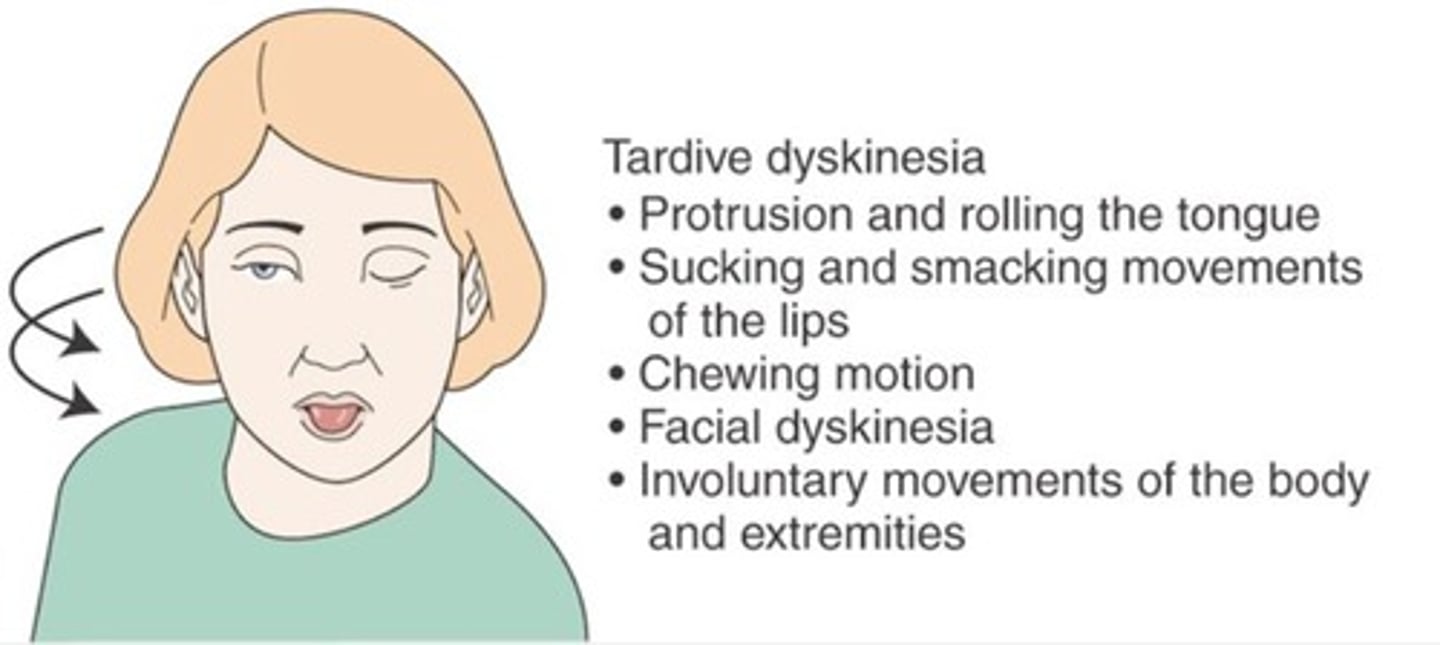
1. Motor control/ extrapyramidal side effects e.g. acute dystonia (Parkinson's like), tardive dyskinesia (Huntington's like)
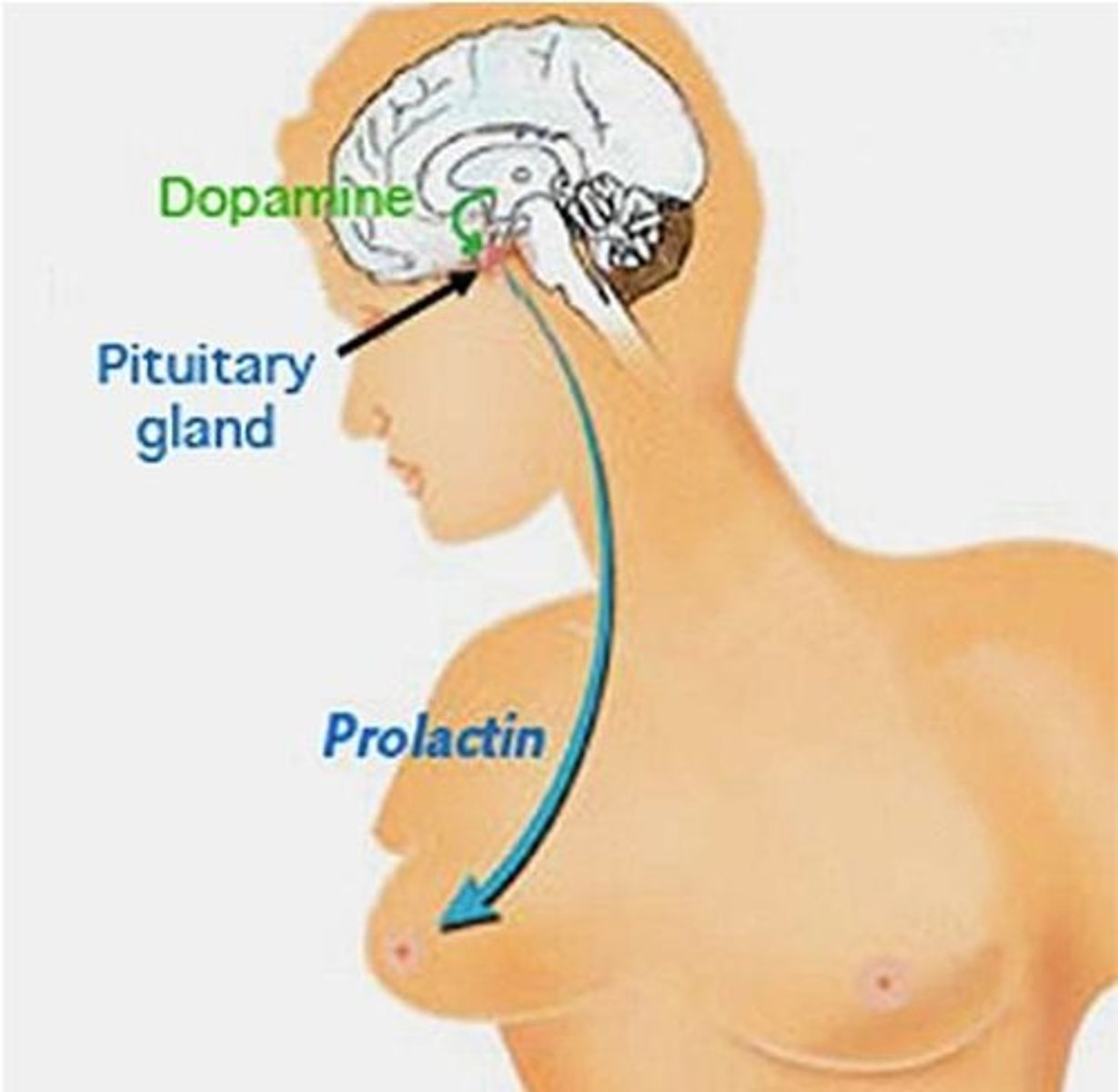
2. Galactorrhoea: excess prolactin release
3. Sedation (histamine H1 / muscarinic)
4. Hypotension (a-adrenergic)
5. Peripheral autonomic - blurred vision, dry mouth, constipation (muscarinic)
6. Sexual dysfunction (muscarinic, a-adrenergic, dopamine)
7. Reduced pleasure via the mesolimbic pathway
Describe how typical antipsychotics can cause extrapyramidal side effects
Typical antipsychotics are D2 receptor antagonists (only want to act in nucleus accumbens). Therefore, they block D2 receptors in all dopamine pathways.
There are also D2 receptors in dorsal receptors. If we inhibit D2 receptors in the caudate, this can cause the extrapyramidal side effects
Describe how typical antipsychotics can cause prolactin release
This is by the blocking of D2 receptors in another dopaminergic pathway called the tuberoinfundibular (TI).
TI pathway is from hypothalamus to pituitary gland.
How can typical antipsychotics exhibit unwanted effects on many different receptors?
These occur because they are not very specific. They act as antagonists at other GPCRs as well as D2 receptors.
How does antipsychotic efficacy correlate with D2 receptor blockade?
As affinity at D2 receptor decreases, then a higher dose of antipsychotic is required.
This is because ~80% block required for antipsychotic effect
What is the mechanism of atypical (2nd generation) antipsychotics?
They are relatively low affinity D2 antagonists and high affinity 5HT2 receptor antagonists.
Atypical antipsychotics bind to and inhibit dopamine's actions on D2 receptors on the nucleus accumbens.
They then block 5HTa receptors which increase dopamine. Usually, 5HT receptor activation results in inhibition of dopamine release.
- 5HTa can increase dopamine in cortex (mainly D1 receptors). Therefore, decreased negative symptoms from schizophrenia (as they are associated with a decrease in C1 activity).
Acts against positive and negative symptoms of schizophrenia.
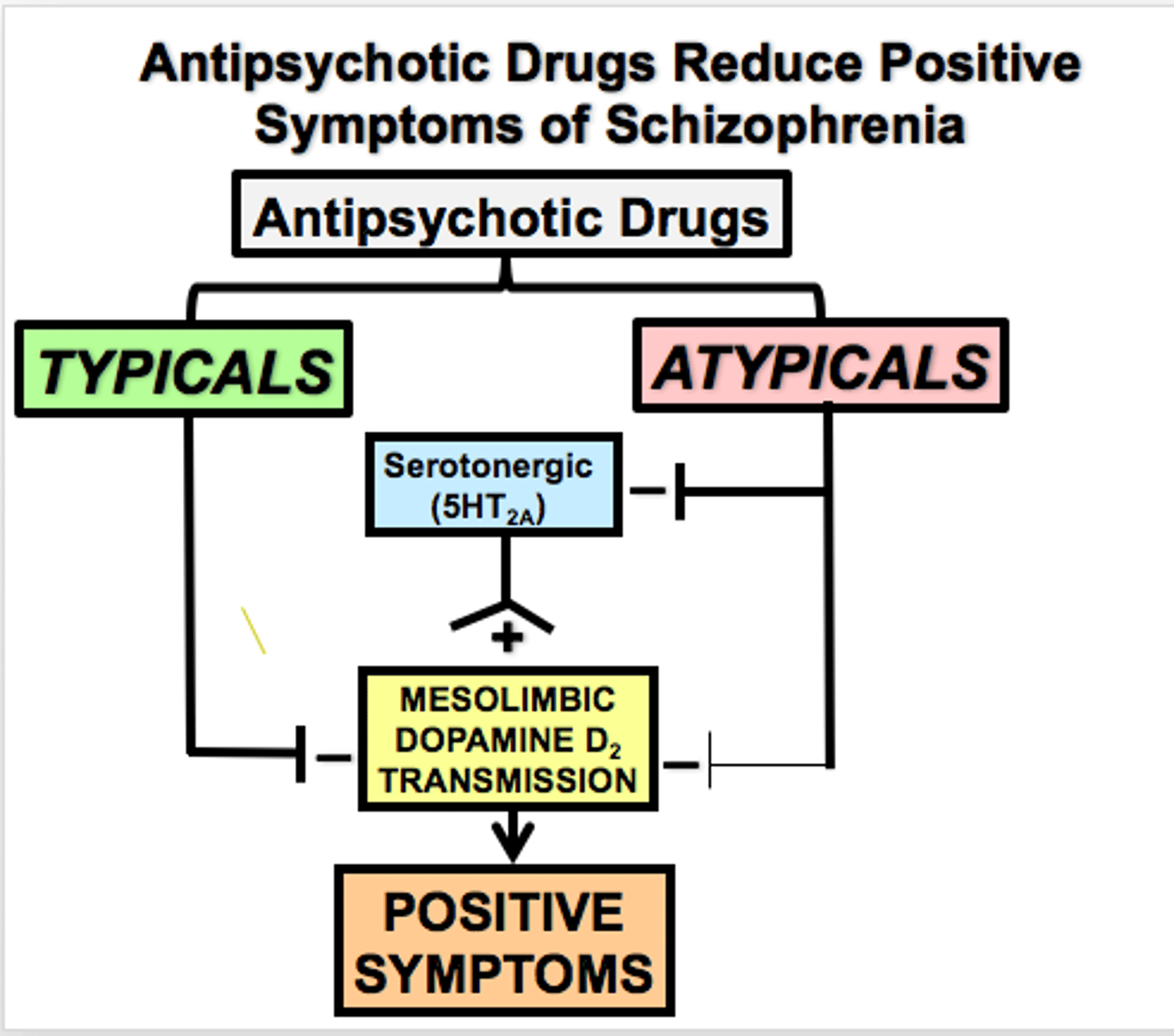
What are benefits of atypical antipsychotics over typical antipsychotics?
1. Have fewer motor control (extrapyramidal) side effects
2. Can act against positive and negative symptoms of schizophrenia
Give examples of atypical antipsychotics
Clozapine, olanzapine, risperidone, aripiprazole
What are side effects of atypical antipsychotics?
Mainly metabolic side effects:
1. Weight gain (Histamine H1, 5HT2C antagonists)
2. Diabetes
Rare but dangerous:
3. Agranulocytosis
- leukopenia (especially with clozapine).
When can clozapine be offered as a treatment for schizophrenia?
If >2 other antipsychotics are ineffective
- would require heavy monitoring
What other receptors may be involved in schizophrenia?
1. Glutamate receptors
2. Nicotinic acetylcholine receptors
3. Muscarinic acetylcholine receptors
How may glutamate receptors be involved in schizophrenia?
The Glutamate theory of schizophrenia
- There may be a loss of cortical function due to loss of glutamatergic neurons
Evidence: NMDA receptor antagonists can cause psychotic episodes in humans and used in animals to induce a psychotic like state. Glutamate binds to NMDA receptors
This may be good for cognitive symptoms if develop therapeutics targeting this.
How may nicotinic acetylcholine receptors be involved in schizophrenia?
We could use nicotinic agonists as part of schizophrenia medication for help with cognitive side effects.
- This is because, people with schizophrenia may use smoking/ vaping to self-medicate
- Nicotinic receptor activation can enhance attention, memory, 'sensory gating - aids cognitive flexibility which is something that people with schizophrenia have a deficit in.
Why must we monitor schizophrenic patients who are stopping from smoking?
Tobacco smoke induces CYP1A2 activity.
Many antipsychotics are metabolised by the CYP1A2 enzyme. Therefore, antipsychotics get metabolised better when people smoke.
But if people suddenly stop smoking, then people metabolise antipsychotics worse when they stop smoking compared to when they were smoking. Therefore, they need to be monitored to make sure that their current dose is still safe and not into toxicity range.
How may muscarinic acetylcholine receptors be involved in schizophrenia?
We could change glutamate and dopamine release in the striatum.
Describe a new drug which acts as a muscarinic acetylcholine receptor antagonist
New drug just been approves in America (still undergoing EU and UK approval) called Cobenfy (xanomeline / trospium)
It is a muscariinc receptor agonist at M1 and M4 and a peripheral muscarinic It can modulate glutamate and dopamine release in the striatum
- It should be effective against positive and negative side effects of schizophrenia