Head and Neck Cancers, Laryngectomy and Tracheostomy
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
85 Terms
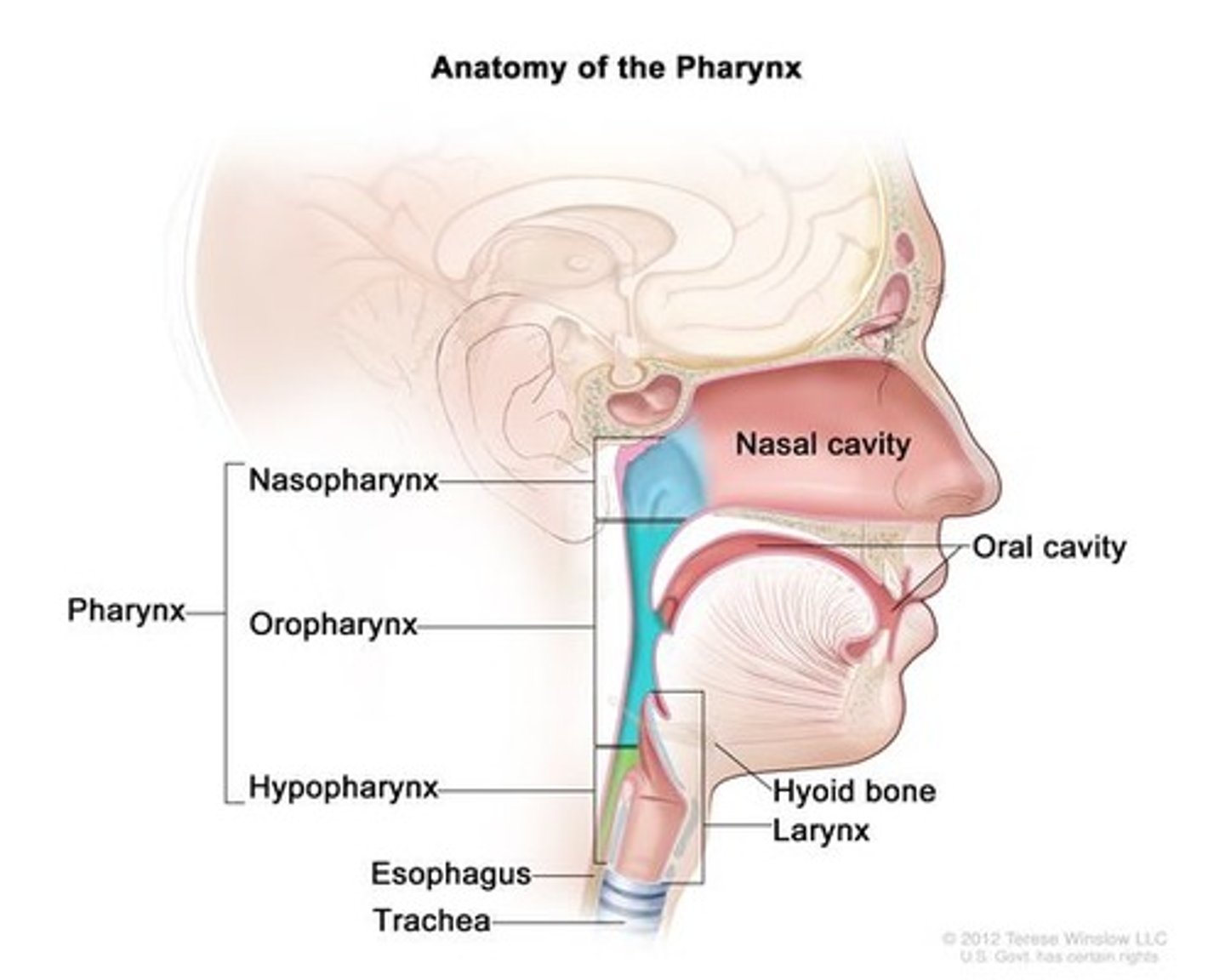
Three zones of the pharynx and there divisions
nasopharynx - posterior nasal until above the velum
oropharynx - includes velum, faucial arches and tonsils
laryngopharynx/hypopharynx - piriform sinuses, the lateral and posterior pharyngeal walls, and the posterior surfaces of the larynx
AOS
Difficulty planning or programming speech movements
Dysarthria
Weakness, poor coordination, slowness or imprecision of articulators
Aphasia
Damage to areas of the brain responsible to language. May effect ability to talk, write or understand spoken and written language.
Intrinsic muscles of the tongue
superior longitudinal (curls tips+sides), inferior longitudinal, transverse (narrows), vertical (flattens)
extrinsic muscles of the tongue
Gross movement -
Genioglossus (protrusion)
Hyoglossus (raises sides and retracts)
Styloglossus (elevates posterior)
Palatoglossus (Depression and retraction)
Three stages of swallowing
oral, pharyngeal, oesophageal
papillae
rough, bumpy elevations on dorsal surface of tongue. Contain taste buds and help grip food.
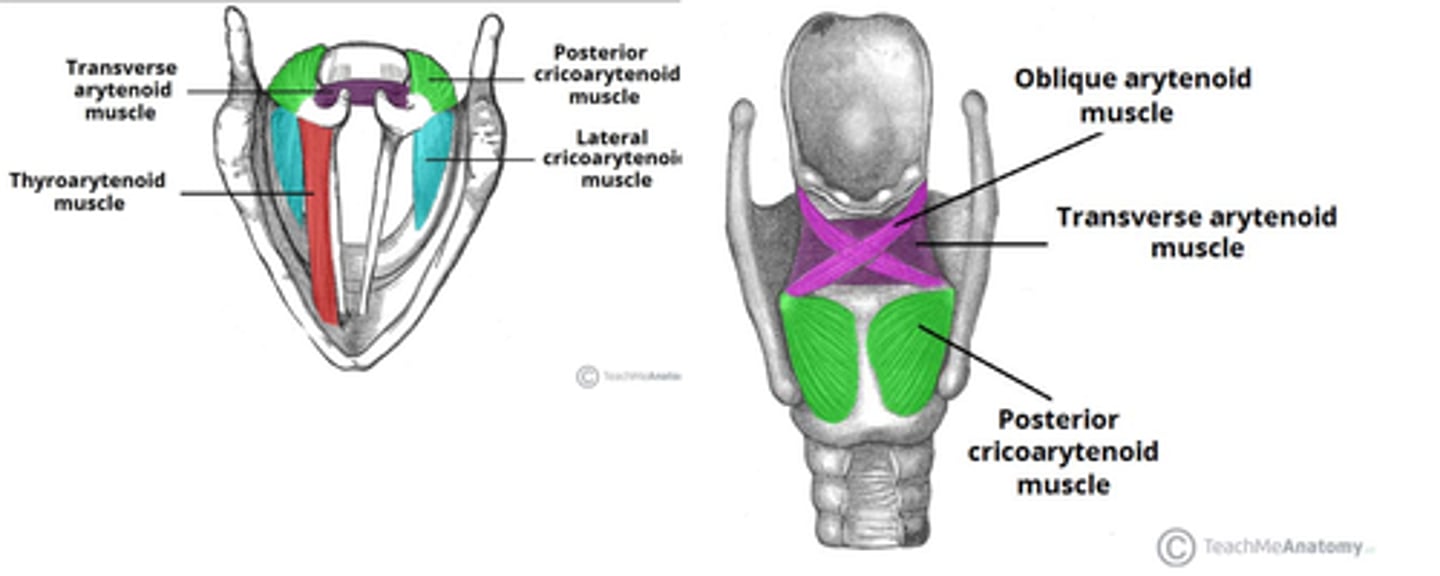
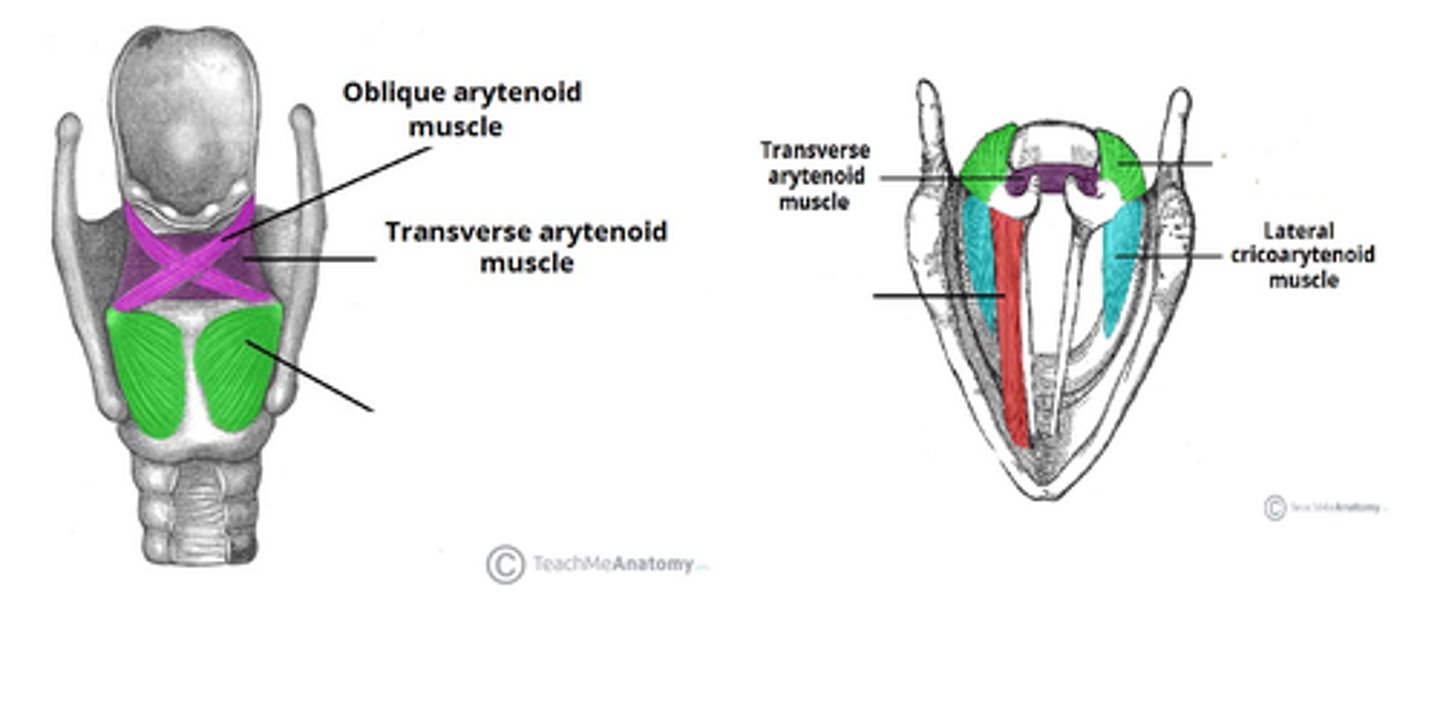
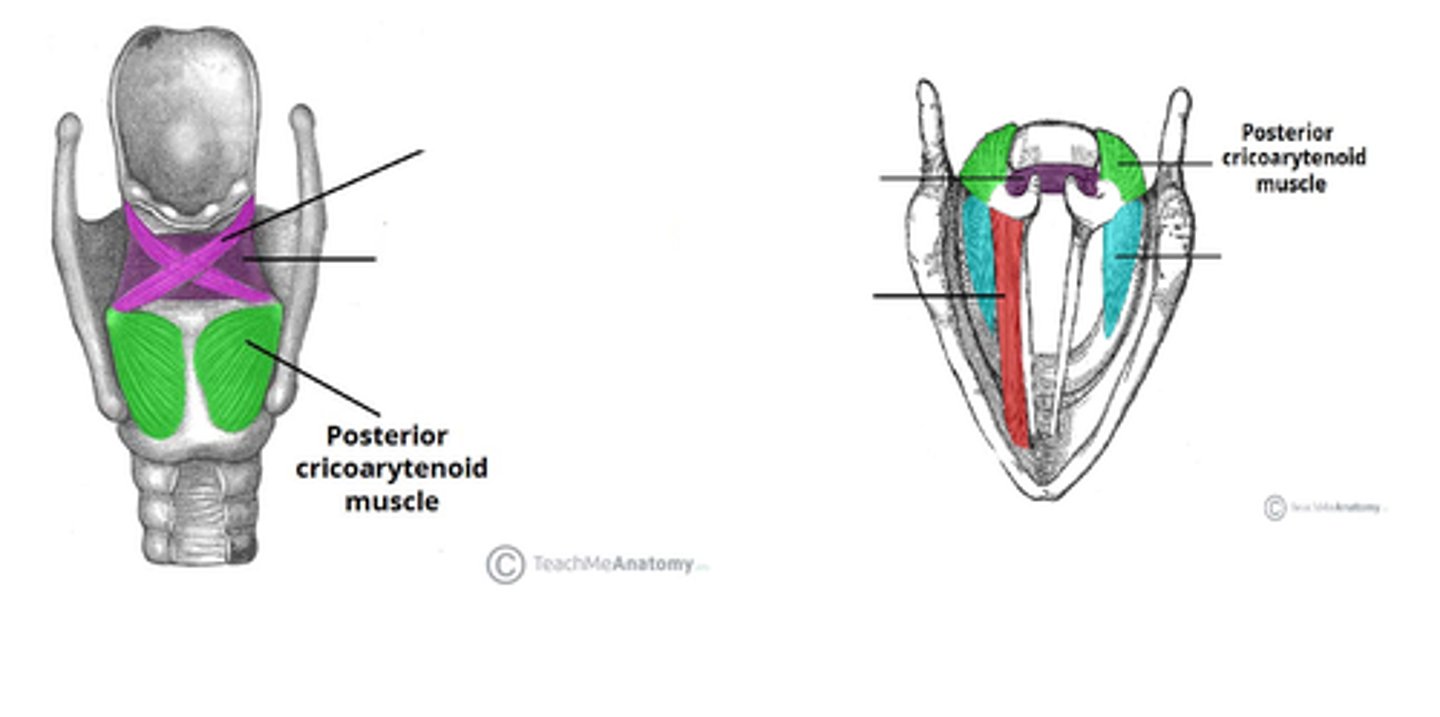
intrinsic laryngeal muscles
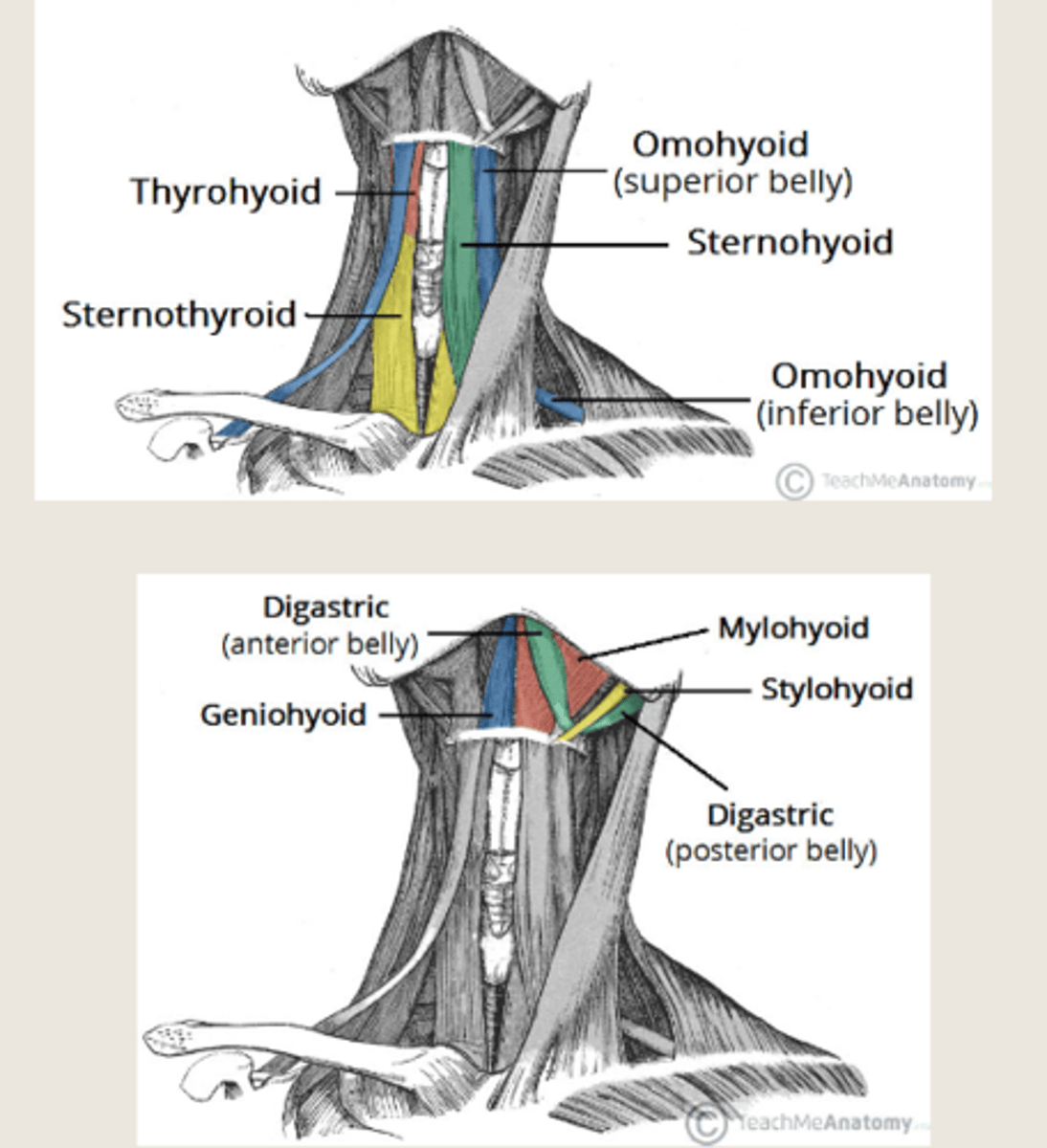
Extrinsic muscles of the larynx and their purpose
suprahyoid and infrahyoid muscle groups. Involved in gross movements e.g. swallowing.
Suprahyoid elevates
Infrahyoid depresses
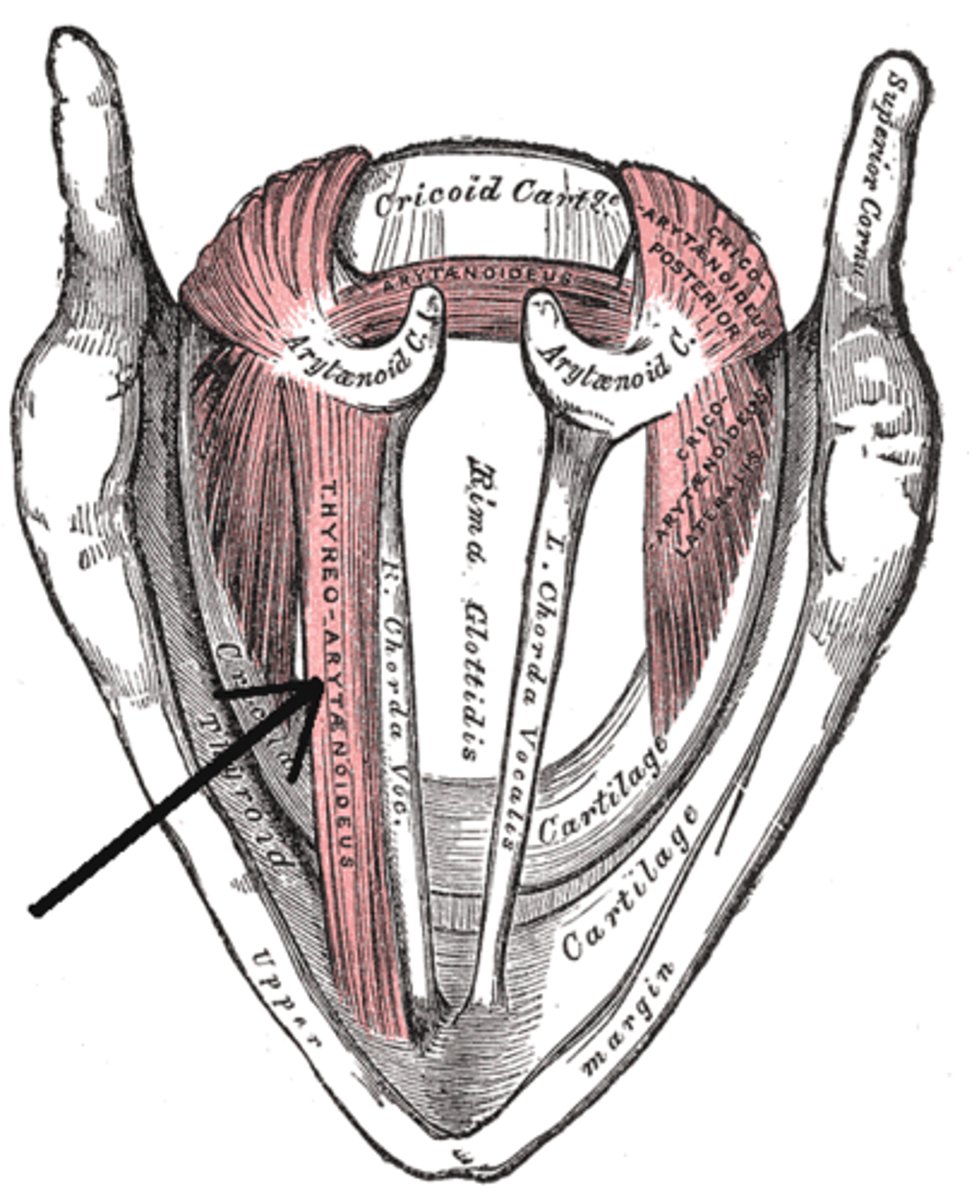
Muscles responsible for shortening of the vocal ligaments
Thyroarytenoid muscle and vocalis (Sometimes all considered to be thyroarytenoids)
Muscles responsible for lengthening of vocal ligaments
cricothyroid m. rolling the cricothyroid joint forward and down
Muscles responsible for adduction of vocal ligaments
Lateral cricoarytenoid m, transverse arytenoid & oblique arytenoid m.
Muscles responsible for abduction of vocal ligaments
Posterior cricoarytenoid m
Risk factors for head and neck cancers
- Alcohol (particularly spirits)
- Tobacco
- Betel nut
- Gender (twice as many men)
- Age
- Epstein - Barr Virus (EBV)
-Environmental/occupation (saw dust)
- Gastro oesophageal reflux disease (GORD) - Acid Reflux
T N M Staging For Cancer
E.g. T2 N2 M0
T = Primary Tumour (1-4, 1=very small and contained, 4= breached the organ and begun to spread)
N = Node involvement (0-3) Lymph Node Involvement (Cancer in the lymph nodes is a sign it has or will spread to other parts of the body)
M = Metastasis (0/1) - Any secondary cancer throughout the body (Unusual for H&NC)
(X may be used as still being determined e.g. T4 N2 Mx)
Iatrogenesis
the creation of a disorder by an attempt to treat it (e.g. During radiotherapy)
Partial, hemi, or total glossectomy
Removal of the tongue (partially, half of it, or entirely)
Effect of tumours on speech or EDS
- Structural changes to articulators e.g. tongue/pharynx
- Structural changes to resonance chambers e.g. nasal cavity/pharynx/hard palate
- Structural changes to swallowing mechanism
- Lesions occupying space needed for breathing/swallowing
- Cause build up/pouching
- Pain
Primary closure
- Tumour extracted and surrounding tissues pulled across to cover wound
- Effective only for small tumours
- Quicker healing time
- Less risk of healing complications
Reconstruction
- Led by a plastic surgery team, in conjunction with treatment team - treats a larger deficit
- Importing tissues containing a blood supply from a donor site
- Blood supply is vital so that the tissue remains alive
- Can be pedicle flaps (PF) or free flaps (FF)
Pedicle flap and Free flap
Pedicle flap= Blood supply is not cut from original arterial supply, but skin is still moved from one location to another
Free flap= Completely removed from donor site and reattached. Requires expertise microvascular surgery to reconnect blood supply.
Common donor sites for PF and FF
- Radial forearm (RFFF) - Used for small sites e.g. tongue or buccal cavity
- Antero-lateral thigh (ALTFF)
- Pectoralis major (PMPF) - Pedical flap usually
Effects of glossectomy on swallowing
- Depending on whether partial, hemi or total
- Loss of function
- Pooling and pouching
- Swelling = Breathing/swallowing problems
- Pain
- Tracheostomy
Radiotherapy
High energy radiation used to kill cancerous cells then regenerate with healthy tissue
- Can only have RT in the same area once.
- Delivered daily 5 days a week over a period of 4-6 weeks (Less frequent if palative)
- Molded masks now used to increase accuracy for HNC
- Many other healthy cells killed on entry and exit
Effects of RT on speech and swallowing
Mucositis
Erythema
Xerostomia
Oedema
Fibrosis
Mucositis (RT side effect)
- Immense pain on inside of throat. Enflamed and ulcered resulting in dysphagia.
Erythema (RT side effect)
- Skin reddening, like bad sun burn.
Xerostomia (RT side effect)
- Thick and sticky saliva/dry mouth
Oedema (RT side effect)
- Swelling, effecting breathing and voice
Fibrosis
Stiffening of tissues and can effect dysphagia or stiffening tissues
Chemotherapy (CT) / Chemoradiotherapy (CRT)
-Use of cytotoxic drugs to destroy cancer cells.
-Used to shrink tumours to manageable size prior to RT or surgery
- Delivered once a week
- Only used on relatively young and fit PTs
Effects of CRT on speech and swallowing
-Fatigue
-Nausea/vomiting
- Reduced appetite
- Infections
- Sore mouth
- Altered taste
Assessing speech and swallowing in HNC
- Take through case history
- Cancer specifics:
diagnosis TMN, planned treatment, current issues
- Relevant PMH (previous medical history) e.g. history of strokes
- Communication needs e.g. audio, reading, languages spoken
- Baseline assessments e.g. oromotor assessments, speech, swallowing, voice
Management pre treatment HNC
- Building rapport and creating support network with other HNC PTs.
- Education
- Discussing alternative feeding
- Introduction to speech therapy e.g. slowing down
Management HNC during treatment (RT/CRT)
- Monitory changes and alter management accordingly
- Work with MDT to manage symptoms
- Motivation to continue therapy and exercises
Management of HNC immediate post surgery
- Post operative input on the ward (especially after tracheostomy, laryngectomy)
- Assess eating, dirnking and swallowing
- Initiate rehab for communication/swallowing
Management HNC post surgery (longer term)
- Rehab for speech/dysphagia . Trying to return to baseline if possible, if not then setting appropriate goals.
- Monitoring and adjusting
- Possible lifelong relationship with SLT e.g. Laryngectomies
Dysphagia problems after HNC treatments
- Trismus (locked jaw)
- Tongue movement/A-P propulsion
- Lip closure
- Nasal regurgitation
- Reduced airway protection
- Pooling/residue
Odynophagia (pain in swallowing)
Interventions for dysphagia problems with HNC
- Therabite (helps with trismus)
- Oromotor exercises
- Textural modification
- Positioning
- Positioning of bolus
Stoma
Artificial opening made into a hollow organ, especially one on the surface of the body (e.g. to gut or the trachea)
Appropriate treatment for laryngeal cancer
T1, 2 or sometimes 3 = RT/CRT
T3/4= Laryngectomy (Post op RT/CRT possible)
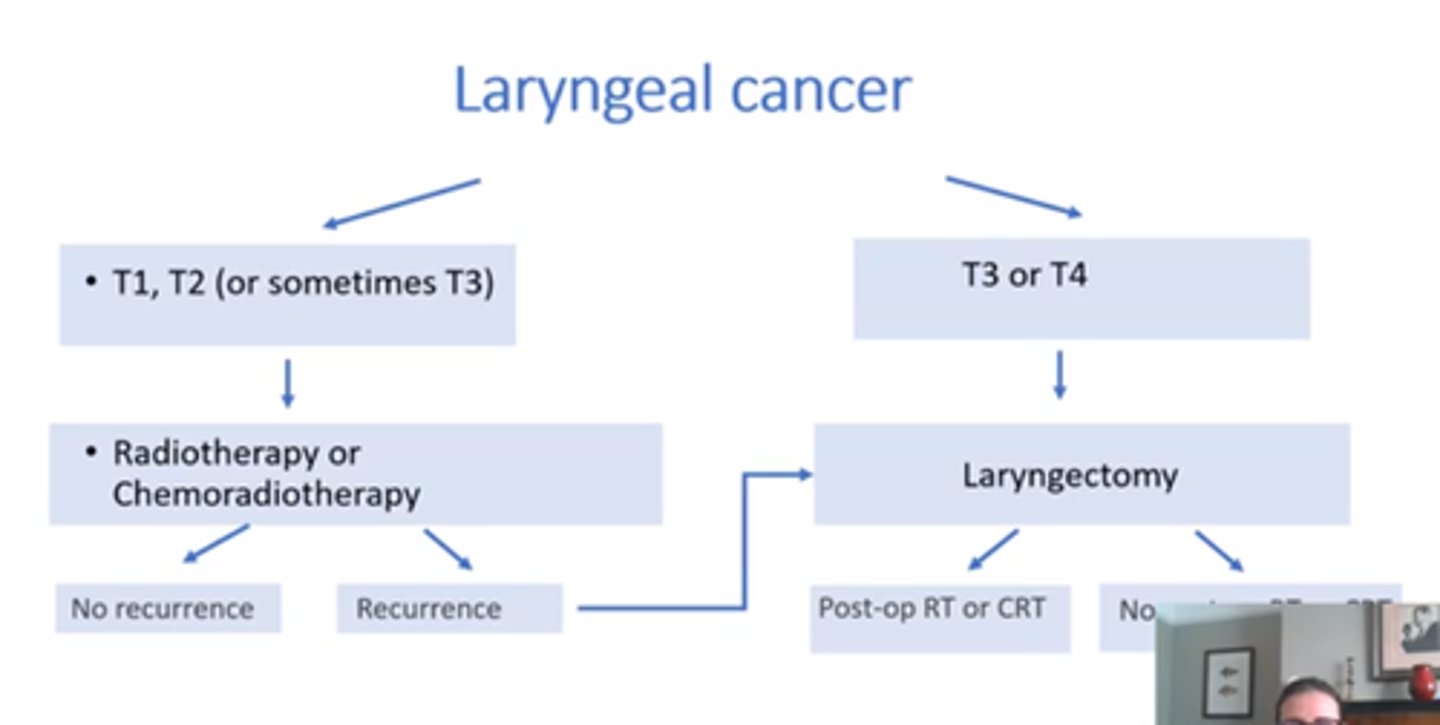
Laryngectomy
Surgical removal of the larynx
May be primary choice of treatment, or used if there is recurrence.
Sometimes used in case of non-functioning larynx.
Carried out by ENT surgeon unless requiring PF/FF then may need a plastic surgeon.
Non-functioning larynx
Caused by side effects that may occur many years down the line
- Fibrosis (leading to non functioning swallow)
- No airway protection when wallowing
- Non intensity modulated RT (receiving lots of radiation to other parts of body)
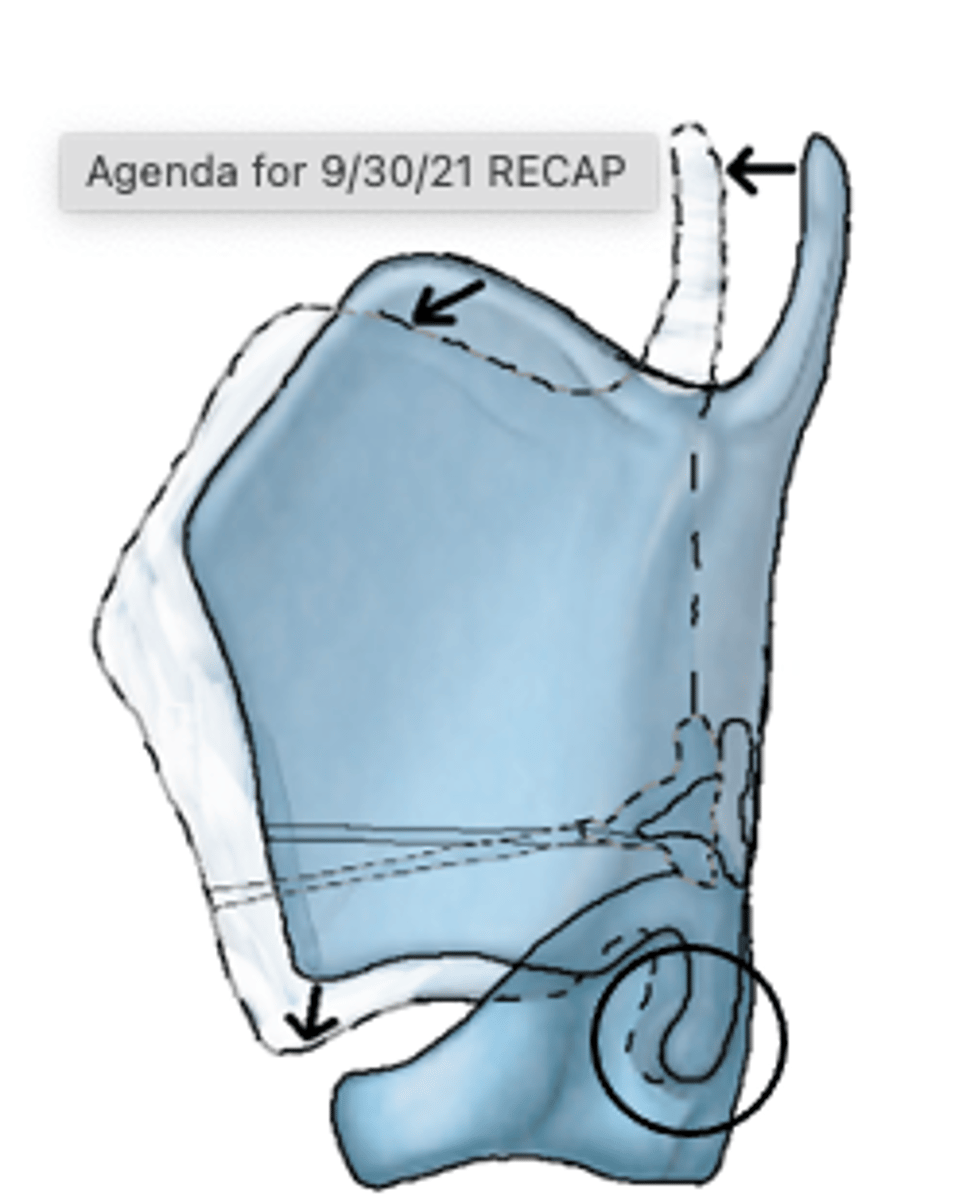
What is removed for a laryngectomy?
Entire larynx including hyoid bone, arytenoids, cricoid, thyroid, epiglottis, VFs/False Vfs, top of trachea
Trachea rerouted to a stoma in the neck.
suture
A stitch or row of stiches holding together the edges of a wound or surgical incision
Pulmonary-oesophageal (PE) narrowing
Narrowing of oesophagus in neopharynx an attempt to mimic the narrowing of glottis and real pharynx, to encourage oesophageal speech.
Upper oesophageal sphincter
Ring of muscles that remain contracted, then relax during the swallowing reflex to allow food through. Maintains acid reflux.
This is cut during a laryngectomy. Not as problematic due to no threat of aspiration, however it can make food regurgitate easier.
Also relies on gravity to bring food down, rather being pushed down.
Myotomy
surgical incision into a muscle
Myotomy of the sternocleidomastoids
Creation of a flat neck by removing muscles of the sternocleidomastoids. Helps with future rehabilitation and protection.
Change on EDS after laryngectomy
- Upper oesophageal sphincter has been cut, reducing ability to push food down
- Risk of aspiration/choking low to nil, as airways have been separated.
- If using valve/oesophageal speech, cant speak and eat, need time in between.
Options for speech after laryngectomy?
-Esophageal speech aka burping
-Electrolarynx
-Tracheo esophageal fistula: one way valve between the trachea and esophagus, producing flow of air from the trachea and forces the air up through the oral cavity
- Silent articulation
- AAC/Signs
Electrolarynx
vibrating diaphragm that is placed on the lateral aspects of the neck.
Does not require breath, just articulation in the mouth. Takes time to learn.
Electronic sound, but these are getting better with new electrolarynxes.
Oesophageal speech
A method of speaking which is used by individuals whose larynx has been removed and in which phonation is achieved by expelling swallowed air from the esophagus
Used to be the main methods prior to valves and electrolarynx.
Takes time to learn.
Tracheoesophageal fissure (TE) and speech
-Valve is inserted between trachea and esophagus that directs air from the trachea to the esophagus so that sound is produced
Cover stomer with hand or HME cassette to divert air through valve, vibration into the pulmonary-oesophageal segment.
Requires good pulmonry air support (not all able to due to COPD/smoking)
Good articulation.
Cant eat/speak at the same time.
Valve/voice prosthesis
Small silicon device that allows air one way but not the other.
Needs to be changed every few months or else it can leak to trachea.
SLT/ENT change valve, however, some PTs learn to do this themselves.
Silent articulation
No vibratory source. Articulations in the mouth. Difficulty to differentiate voiced sounds. Obvious difficulties in loud places/background noises.
Heat Moisture Exchange (HME)
Bib to catch moisture from the stoma - once moist performs a similar job to the nose - filtering and making air moist.
HME cassettes
Circular device added to a plaster like support.
Will start with higher airflow, and gradually work towards lower flow.
Management of rehabilitating smell
Politve yawn technique: place tongue on palate, pull down tingue and lower mandible as if yawning with lips closed. Negative pressure sucks in air.
Wafting/steam diffusers
Consider safety e.g. smoke detectors, gas detectors
Changes of laryngectomy effecting safety
Water safety - bathing/shower
Breath hold impossible
Respiration
CPR
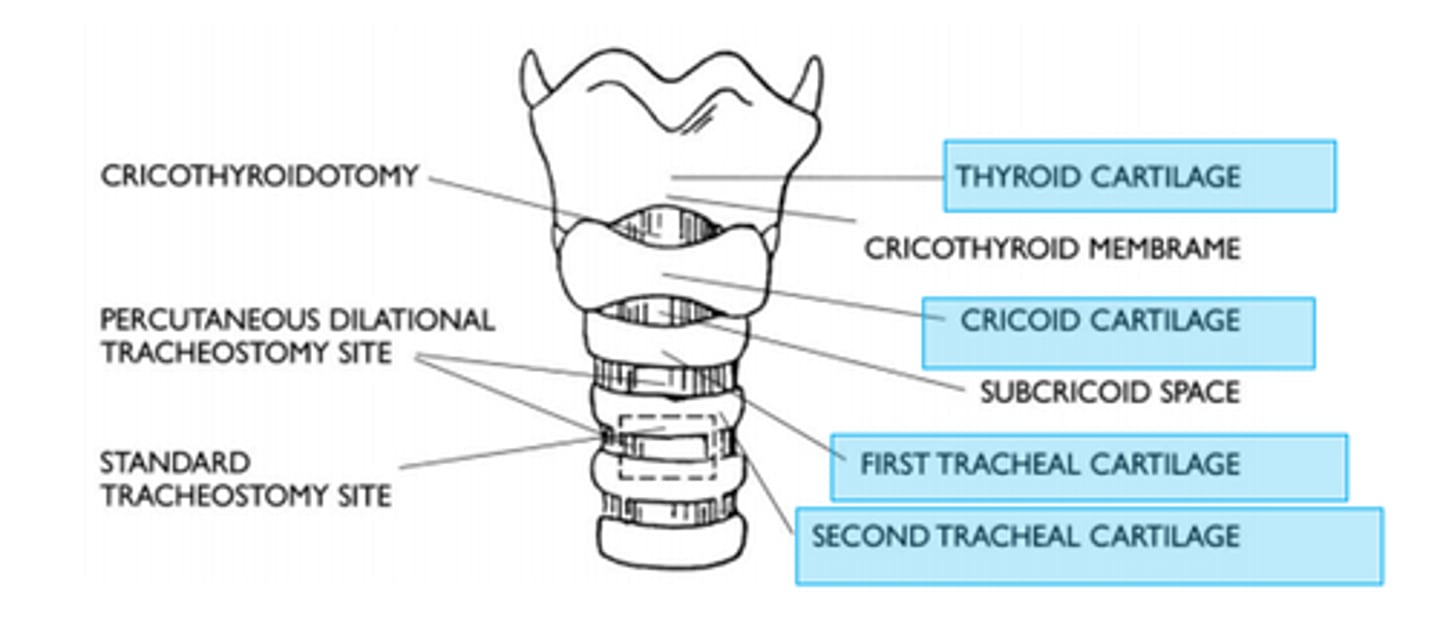
Tracheostomy
creation of an artificial opening into the trachea, usually between the second and third tracheal rings.
Nothing is removed. Tube is lightly sutured to the neck.
Cuff inflates and can stop aspirations reaching the lungs.
Tracheostomy reasons
Securing and maintaining a safe airway for pts with:
- Injuries to face/neck/head
- Following surgeris to the neck
- Laryngeal/pharyngeal obstructions
- Long term mechanical ventilation
Endotracheal tube (ET)
a short-term artificial airway to administer invasive mechanical ventilation, relieve upper airway obstruction, protect against aspiration, or clear secretions.
Requires pt sedation, hence the move to a tracheostomy tube.
elective tracheostomy
Scheduled surgery with the proper informing of the pt.
Emergency tracheostomy
Sudden acute need to establish a safe airway e.g. choking/anaphylaxis
Surgical site for tracheostomy
Between 2-3rd tracheal rings
Pilot balloon
Pilot balloon on outside of the neck inflates to tell us the cuff is inflated in the trachea
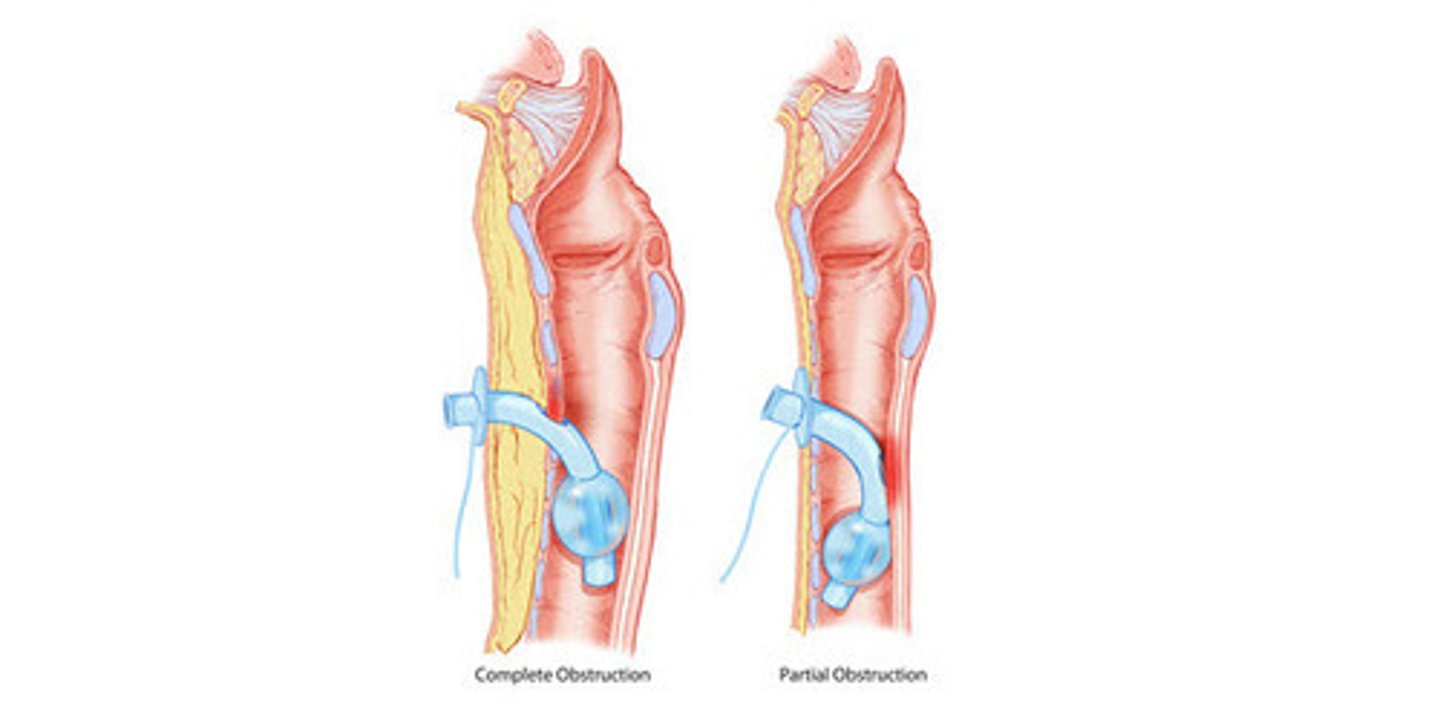
Trache cuff
When inflated no air can escape orally - all airflow through the trache.
When deflated, it can be a mixture of both orally and through trache.
Types of Tracheostomy Tubes
-Single cannula
-Double cannula -> has INNER and OUTER cannula
-Fenestrated. Has a hole to allow slight air escape during weaning process.
- Cuffed or uncuffed (look for pilot balloon)
Single vs double cannula
Single cannula tube usually for primary insertion. Usually changed to double.
Double cannula allows removal of inner one when it becomes blocked, and cleaned/replaced.
Cuffed vs uncuffed
Uncuffed - Requires safe swallow and therefore may be eating orally.
Cuffed - creates closed circuit. Used when at risk of aspirating.
- Usually patient will be NBM as it put pressure on the oesophagus.
When cuffed the trache can granulate tissues due to rubbing. - - Subglottic suctioning should be done regularly especially when new to understand how much is being aspirated.
- Disuse atrophy of the laryngeal muscles when not used for a long time.
Similarities of tracheostomy and laryngectomy
- Breathing through neck
- May be unable to speak
- Resus via neck
- Chest secretions via stoma
- HME systems needed
- Vulnerable to water entry
Differences of tracheostomy to laryngectomy
Tracheostomy:
- All structures remain present and relatively intact
- Needs tube 24/7
- High risk of losing airway of tube removed
- Regular suctioning likely needed superior to cuff.
- May achieve voicing if uncuffed
Differences of laryngectomy to tracheostomy
Laryngectomy
- Total removal of larynx - major surgery
- Most don't use tubes - singular if worn
- Permanent stoma
- Can usually cough out stoma
- No airflow through nose and mouth (unless tracheoesophageal speech)
- No traditional voicing
Weaning
Process of reducing dependency on the cuff, introducing speaking valves or moving towards decannulation
Things to consider for weaning
- Has the reason for the trache insertion been improved/resolved
- How much suctioning is being done, how much liquid being removed.
- Are they able to cough out of the tube?
- General stability?
Cuff deflation trial
- Wanting a cough reflex triggered due to new air rushing through, and small amount of saliva. No cough isnt a good sign.
- Observe closely
- May fatigue
- If coughing continues and isn't clearing, reinflation.
Fenestrated tube
Have holes at the top of the cannula. Allows twisting of the tubes holes to be open or shut.
Generally avoided now due to risk of granulation forming against or into the fenestration.
Smaller tubes used instead.
HME
Heat moisture exchange
Impact of tracheostomy on respiration and safety
- Need to filter/humidify air with HME
- Dry/sticky secretions can block the tube
- Likely to need regular nebuliser to increase moisture
- Regular subglottic suctioning
Tracheostomy impact on voice
- Cuff up = no voice
- Cuff down = may be possible, better with fenestrated tube.
- Tracheostomy speaking valve may be used if there is a safe swallow and no aspiration
Tracheostomy speaking valves
- One way valve that stops air escaping and forces it through the larynx
-DO NOT USE WITH CUFF UP
-
Tracheostomy impact on swallow
-Pt usually NBM when cuff is up
- When weaning, gradually increase liquid/semi liquid food
mandibuloectomy
removal of part of the lower jaw, usually due to a tumour