Lecture 5: Diseases of the Biliary Tract
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
54 Terms
Osteopathic findings in gallbladder disease
Referred pain (mid-thoracic region; R shoulder and tip of the R scapula)
Somatic dysfunction T5-9 on the R
Restriction of the celiac ganglion
If the diaphragm is significantly irritated, findings at C3-5
Suspect Acute Cholecystitis if at least one in each category is present
Signs of local inflammation: Murphy sign, RUQ mass, pain or tenderness
Signs of systemic inflammation: Fever, ↑ WBC, ↑ C-reactive protein
Characteristic imaging findings
Cholelithiasis
Gallstones
Cholecystitis
Gallbladder Inflammation
Choledocholithiasis
Common bile duct stones
Cholangitis
Inflammation/infection of the biliary tree
Biliary colic
Pain due to gallbladder contraction or stones/sludge
Most accurate predictor of gallstone disease
Functional gallbladder disorder
Biliary pain in the absence of gallstones/sludge
LFT’s are normal
May have low ejection fraction of the GB
Cholecystectomy
Removal of the GB
Cholelithiasis Pathogenesis
Bile produced in liver; secreted into hepatic duct; stored in gallbladder; released into duodenum to digest fats
Bile= cholesterol + lecithin + bile acids
Cholesterol insoluble so lecithin & bile acids make micelles to keep it soluble
If too much cholesterol or too little bile acids/salts, → Cholesterol supersaturation → crystals → gallstones
Decrease gallbladder motility → sludging
In the cystic duct, cause biliary colic or cholecystitis
In common bile duct, cause cholangitis and/or pancreatitis
Cholelithiasis Risk Factors
Obesity → Increase Cholesterol secretion
Increasing age
Women
Genetics
NAFLD, Hepatitis B + C, Cirrhosis → ↓ synthesis of bile salts
Postmenopausal hormone therapy or pregnancy (estrogen ↑ chol; progesterone ↓ bile salts & slows emptying)
Bariatric surgery- gallbladder stasis
Diabetes (↑l ipids; neuropathy→ gb hypomotility and biliary stasis)
Crohn’s (bile salts not resorbed)
Drugs: Ceftriaxone
Spinal cord injuries (gallbladder less motile; bile stasis occurs
Cholesterol Stones
Most common stone in adults
Cholesterol > bile acid
Common in adults with diabetes, obesity, hyperlipidemia, or multiparity
Pigment Stones
Black:
Most common stone in children
Due to hemolytic states; unconj. bilirubin precipitates; primarily made of Ca bilirubinate
Sickle cell patients
Radiopaque (Fe from the hemolyzed RBC’s shows up)
Brown: Radiolucent; infection
Symptomatic Cholelithiasis
Transient obstruction of cystic duct
Biliary colic
Epigastric/RUQ dull pressure/pain; typically lasts ~30 mins, but can last a few hrs
Usually occurs 1-2 hrs postprandial OR nocturnal
Can be triggered by a fatty meal
May radiate to the back & be assoc. with N/V
Can go hrs or years between attacks; most within 2 yrs
Not relieved or exacerbated by movement or flatus/Bowel movements
Abdominal Ultrasound most accurate if fasting >8 hrs, as stones are best seen in a distended GB filled with bile
Stones cast shadow + move around

Cholelithiasis

Cholelithiasis
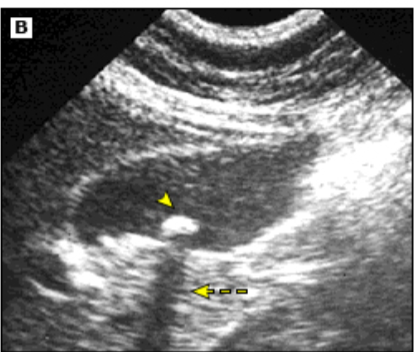
Cholelithiasis

Cholelithiasis

Calcified gallstones in gallbladder, cystic duct, and common bile duct
If no stones on US, but biliary colic
Endoscopic ultrasound
Transducer on tip of endoscope
More sensitive for sludge & small stones
Can exclude PUD


Magnetic Resonance Cholangiopancreatography (MRCP)
Noninvasive
Alternative if US negative
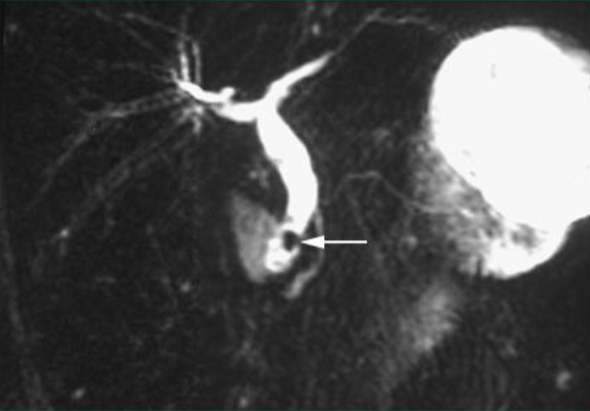
Common bile duct stone
Therapy for cholelithiasis
Symptomatic:
Acute episode: IM NSAID (diclofenac), hydration, antiemetics, followed by po NSAIDS
Diclofenac ↓ progression to cholecystitis
Definitive: Laparoscopic Cholecystectomy
Asymptomatic:
Observe
Surgery in Hemolytic/sickle cell anemia, organ transplant, ↑ risk of cancer (porcelain gallbladder, large/growing polyps)
Cholelithiasis Therapy
Oral bile acid litholysis with urso-deoxycholic acid (UDCA)
Reserved for those who can’t tolerate or refuse surgery
Complications of Gallstones
Acute Cholestasis/cholecystitis/cholangitis
Chronic cholecystitis
Gallstone Ileus- Large stone erodes through GB wall into duodenum → obstructs small bowel → Enterolithotomy
Choledocholithiasis (common bile duct stone)
Gangrene of gallbladder, perforation
Pancreatitis

Gallstone Ileus
Gallstone Ileus
When do you hospitalize a patient with biliary disease?
Intractable pain
Intractable vomiting → dehydration
Evidence of cholecystitis, cholangitis, or pancreatitis
Acute Cholecystitis Pathogenesis
Usually caused by stones impacted in cystic duct
Obstruction→↑ intraluminal pressure & supersaturated bile
Static bile→ inflammation→ distention→ poor drainage & blood flow→ infection
Acute Cholecystitis
Begins with biliary colic and becomes steady, severe RUQ pain → radiation to R shoulder and back (>6 hrs)
Ill appearing, lying still, febrile, tachycardic
N/V
Fever
Murphy’s sign: Hand placed under ribcage & pt. asked to take deep breath → as GB descends & contacts hand, pain is elicited, and breath is held
Can also be elicited sonographically
Leukocytosis, ↑ CRP (>3 mg/dl)
US—distended GB & cystic duct w/ stones, thickened wall, sonographic Murphy’s, pericholecystic fluid

Acute Cholecystitis
Thickened wall, double wall sign, sludge & stones with acoustic shadowing
HIDA
HIDA (99m technetium-labeled hepatobiliary imaging using iminodiacetic acid) / Cholescintigraphy / hepatobiliary scintigraphy
Demonstrates obstructed cystic or common bile duct
Performed if clinically cholecystitis and US is nondiagnostic
IV injected isotope “follows” bile
Liver is not visualized → liver disease
Gallbladder not visualized → cystic duct obstructed
Small bowel not visualized → common duct obstructed
If both gallbladder and small bowel are visualized with the HIDA scan, CCK can be injected to see if it functions well
Ejection fraction <35% =poorly functioning GB
Acute Cholecystitis Treatment
NPO
IV fluids/correct electrolytes
Analgesics
Antiemetic & NG tube if vomiting
Empiric antibiotics if suspected infection
Early cholecystectomy (<72 hrs)
Complications of Acute Cholecystitis
Gangrene
Perforation
Cholecystoenteric fistula—Perf into bowel
Gallstone ileus
Emphysematous cholecystitis—Crepitus in abdominal wall next to gallbladder
Caused by gas-forming Clostridium welchii
Chronic Cholecystitis
Multiple episodes of acute disease or chronic irritation by stones leads to thickening and fibrosis
Choledocholithiasis
Past history of colicky pain-now sudden onset severe pain RUQ w/ radiation
N/V
Fever if cholangitis
Obstructive jaundice → pale stools, dark urine
May develop pancreatitis
Elevated conjugated (direct) bilirubin
Elevated alkaline phosphatase
Amylase/lipase elevated if pancreatitis
Leukocytosis if also cholangitis
GGT must be elevated
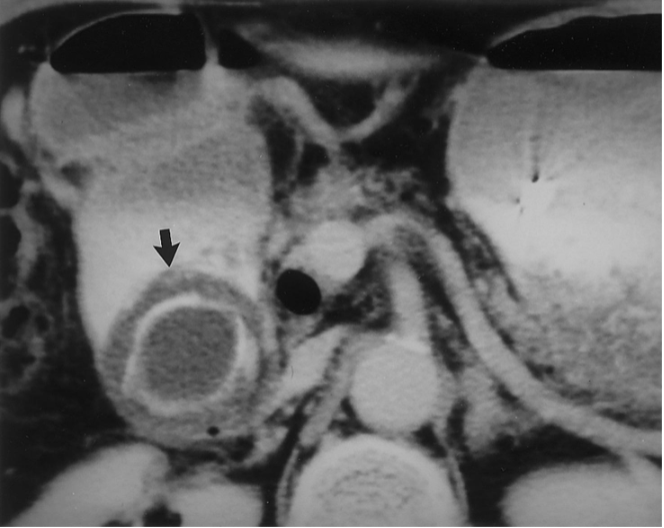
Choledocholithiasis Imaging
US: Dilated ducts and possibly stones
CT: Dilated ducts, but stones are isodense with bile so can’t be seen
MRCP
Endoscopic US

Endosonographic image of stone in common bile duct (with acoustic shadow)
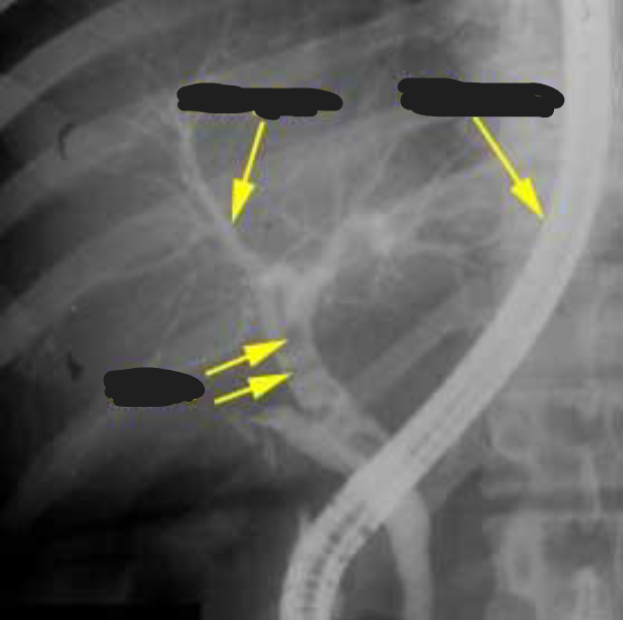
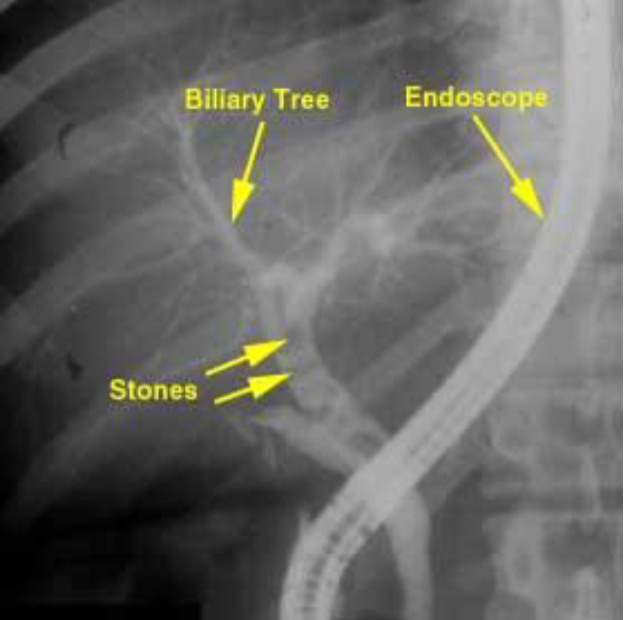
ERCP (endoscopic retrograde cholangiopancreatography)
With endoscope, cannulate duodenal papillae and view biliary & pancreatic tree
If stones present, can be removed
Allows treatment at same time as dx
Often done intraoperatively during a lap chole
Potential complication: Pancreatitis
MRCP or endoscopic US can be done first for dx, only doing ERCP if needed for stone removal
ERCP
Choledocholithiasis Treatment
IV fluids
Bedrest
Control N/V
Pain control
lap chole with intraoperative ERCP
Even if the patient is asymptomatic (unlikely), the stones must be removed
Acute Cholangitis
Ascending infection
From any obstruction of flow of bile
Serious (hypotension altered mental status); can be fatal
Infection in the biliary tree, obstruction from stones, strictures, cancer
Can lead to sepsis & death
Organisms are usually colonic origin- bacteria from duodenum can ascend through the sphincter of Oddi area after sphinterotomy, stent, or other disruption
Some bacteria passes through on its own and a stone in the common duct then acts as a nidus for infection
Charcot’s Triad
RUQ pain
Fever + Chills
Jaundice
Reynold’s Pentad
Obstructive cholangitis/high mortality
Charcot’s Triad PLUS
Mental status changes
Hypotension
Cholangitis Labs and Imaging
Leukocytosis, elevated alkaline phosphatase, GGT, & direct bilirubin; blood cultures
US: Common bile duct dilation & stones
CT with IV contrast or MRCP: Determine level & cause of obstruction
Cholangitis Treatment
ERCP with sphincterotomy (severing muscle fibers of sphincter of Oddi to enlarge outlet of biliary tree), stone removal, and biliary drainage/stent
Antibiotics
IV fluids
NPO
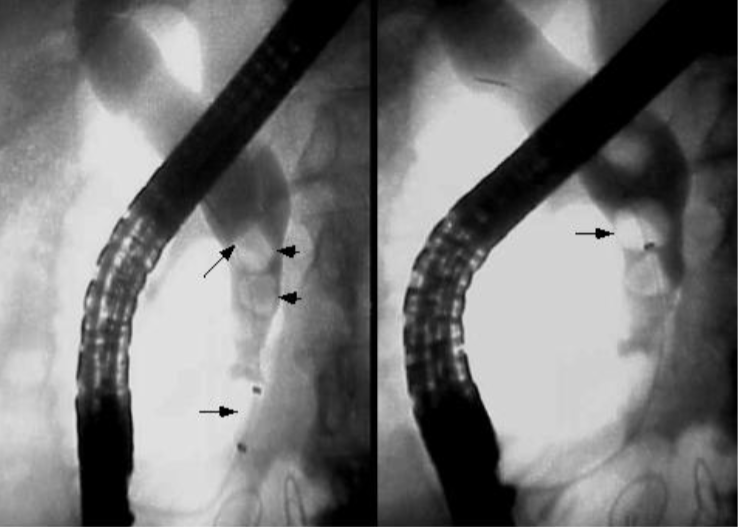
Common Bile Duct Stones
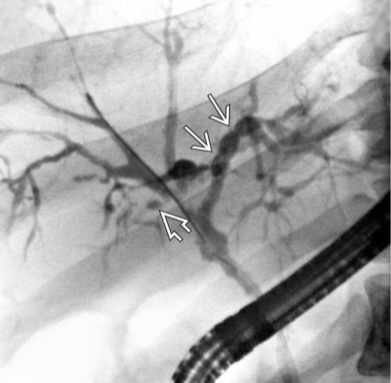
Primary Sclerosing Cholangitis
Primary Sclerosing Cholangitis
Rare, immune-mediated, men
Ulcerative colitis
Fibrosis of extra & intrahepatic bile ducts → obstructive jaundice
String of beads
Primary Biliary Cholangitis
Chronic autoimmune disease
Women >45
Inflammation/destruction/fibrosis of bile ducts (intrahepatic only)
Leads to scarring & cirrhosis

Porcelain (calcified) gallbladder
Porcelain (calcified) gallbladder
Chronic cholecystitis
Small risk for cancer
Fitz-Hugh-Curtis syndrome
Perihepatitis (inflammation of the liver capsule
Gynecologic pain