lab 13: glucose tolerance
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
blood glucose concentration is under the control of...
two pancreatic hormones released from cells in the islets of Langerhans
insulin is secreted from...
B cells of pancreas and is responsible for getting glucose into cells of the body and reducing glucose levels
glucagon is released from...
alpha cells of pancreas and is responsible for getting mobilizing stored sugars via glycogenolysis in the liver [breakdown of glycogen] or producing new sugars via gluconeogenesis also in the liver
glucagon raises blood glucose levels
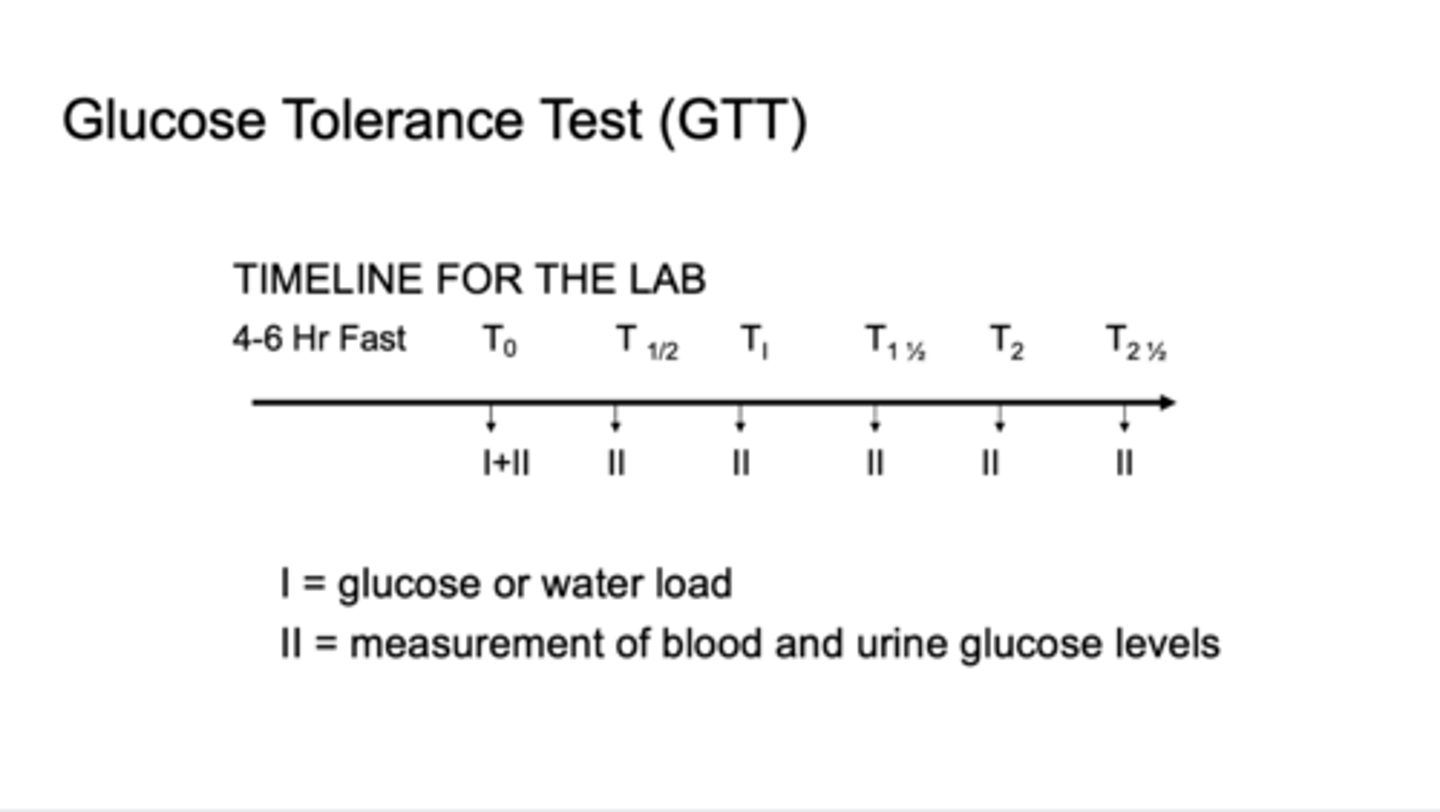
glucose tolerance test [GTT]
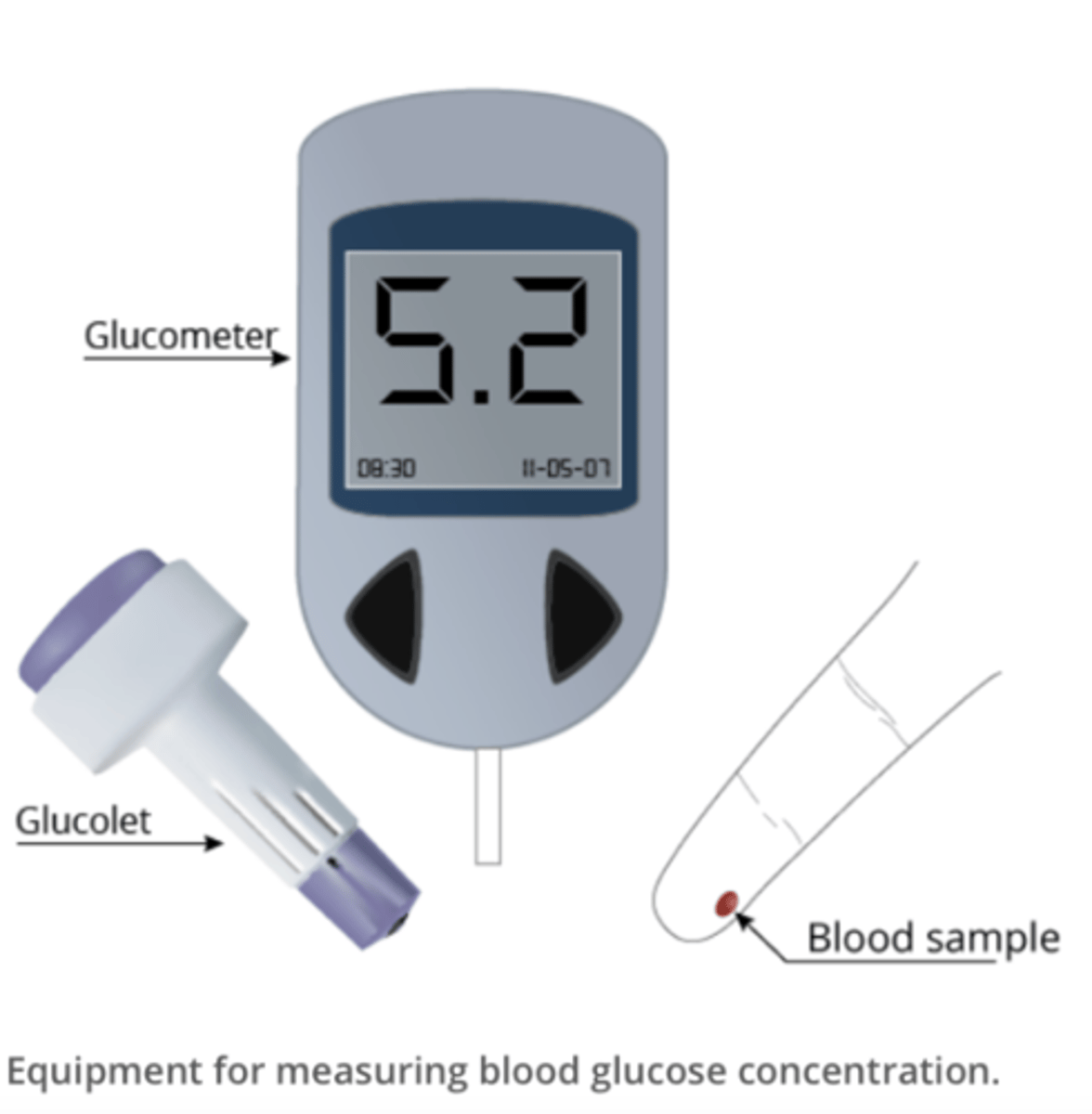
glucometer
used to measure each volunteer's blood glucose every 30 minutes for at least 90 minutes during the lab to track their blood glucose over time
typical pattern of results regarding blood glucose

explanation of results for a healthy individual with water load
their blood glucose would remain relatively unchanged, and low, over the course of the lab because they did not consume a glucose load and they fasted
explanation of results for a healthy individual with glucose load [GTT]
their baseline would be similar to the water load. we should see their blood glucose peak about 45 minutes after consuming the glucose load, and then return to pretest levels within 2 hours
explanation of results for individual with diabetes consuming glucose load [GTT]
3 main differences:
higher than normal fasting blood glucose level
blood glucose peak much higher than normal, often but not always surpassing renal threshold
takes longer for their blood glucose to return to pretest levels [3-5 hours instead of 2 hours]
what are the main differences between types I and type II diabetes
type I affects appx 10% of patients, and results from an inadequate secretion of insulin from beta cells in islets of Langerhans. destruction of beta cells is due to autoimmune disease
type II affects appx 90% of patients. insulin level is normal but either insulin receptors on cells are inoperative, there are too few receptors, or the second messenger cascade in cells is non-operational. there is a decreased responsiveness to insulin; often associated with obesity
what physiological symptoms [3 Ps] accompany type II diabetes?
polyuria
polydipsia
polyphagia
polyuria
increased urine production as a result of glucose spilling into urine and drawing water with it [osmotic diuresis]
polydipsia
increased drinking, loss of water stimulates thirst centers in the brain
polyphagia
increased eating, as cells cannot use glucose, the patient must eat more protein and lipids to compensate
relationship between obesity and diabetes
obesity is considered a trigger for type II diabetes
in these individuals, the production of insulin is unchanged. the problem is thought to be related to the insulin receptors on adipose cells
as these adipose cells enlarge, the ratio of the number of receptors per gram of tissue decreases [and/or the receptors may be stretched and damaged] and the effectiveness of sugar entry into these cells is drastically decreased
the result is hyperglycemia and the symptoms of diabetes
greatest immediate risks to life in an individual with diabetes
most threatening is the production of acidic ketones as a result of increased fat metabolism. fats stored in the liver are called upon to supply an energy source as cells cant use sugars. metabolic acidosis [ketoacidosis] may cause diabetic coma or death
insulin shock: for those taking exogenous insulin, an overdose is extremely dangerous. plasma glucose levels will drop to very low levels and CNS will fail
ketoacidosis: fats are used as an energy source instead of sugars. ketones are a by-product of fat metabolism. an abundance of these results in metabolic acidosis and in diabetic coma
high blood sugar: molecules, especially on the surface of vascular endothelial cells, become glycosylated. this results in the blockage of the vessel lumen and a reduction in circulation
what chronic health problems are diabetes at risk of developing?
high levels of glucose in the blood and the nutritional deficits suffered by cells unable to use glucose result in: blindness [retinopathy], atherosclerosis, and poor circulation [may sometimes result in susceptibility to gangrene]
by what mechanism do diabetics have problems with adequate blood flow [especially to extremities]?
in hyperglycemia molecules on the surface of capillary [and all blood vessels] endothelial cells become glycosylated and therefore 'sticky.'
a variety of substances bind to these sugars and produce a blockage of the vessel lumen
the result is reduced blood flow to particular area
what relationship exists between diabetes and gangrene?
with reduced blood flow to the extremities, peripheral neuropathies result in a decrease in sensation
individuals that lose sensation in, [ex. foot], are more likely to injure the extremity without realizing it
as a result, an untended wound will develop an infection and subsequent gangrene [tissue death]
imagine that a diabetic takes a glucose tolerance test.
does the blood sugar level ever drop in this individual? by what mechanism does the blood sugar level drop over time?
yes because some tissues such as neurons and red blood cells do not require insulin to facilitate the entry of glucose, these cells are responsible for the overall drop in blood sugar in diabetics. the drop is, of course, much slower than in non-diabetics.