Module 2 - The Autonomic Nervous System
1/51
Earn XP
Description and Tags
2/4/26 and 2/6/26 lectures
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
autonomic nervous system (ANS)
part of the central nervous system
composed of the sympathetic and parasympathetic systems
has afferent and efferent pathways
functions mostly at the subconscious level (autonomic = automatic, not within our conscious control)
functions of the ANS
controls functions of many organs and tissues in the body
innervates visceral organs, glands (e.g. sweat glands), blood vessels (walls of blood vessels → controls blood pressure)
regulates visceral organs
efferent fibers of the ANS
cell bodies are in the spinal cord and reach sympathetic ganglia
(sympathetic ganglia are located on both sides of the vertebral column)
parasympathetic efferents reach ganglia at/near organs
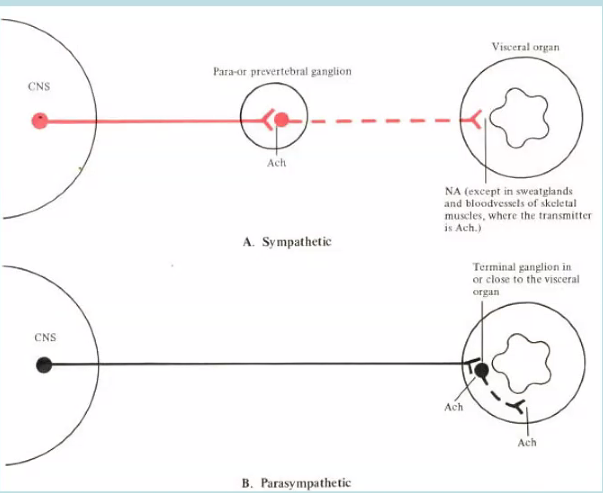
organization of the ANS
preganglionic neuron cell bodies are in the CNS
preganglionic neurons’ bodies originate the CNS
in autonomic neuroganglia: preganglionic neurons form a synapse with the bodies of postganglionic neurons
postganglionic neurons synapse on effector organs
the adrenal medulla is an example of a specialized ganglion of the sympathetic NS
adrenal medulla
a specialized ganglion of the sympathetic NS
preganglionic fibers synapse on chromaffin cells
chromaffin cells secrete epinephrine and norepinephrine (80% epi and 20% norepi) into circulation
clinical point: pheochromocytoma
adrenal medulla can form a tumor that secretes excessive catecholamines and increase excretion of VMA (3-methoxy-4-hydroxymandelic acid)
sympathetic nervous system
“fight-or-flight” system (e.g. during exercise, fear)
prepares and mobilizes body in emergency cases
stimulation leads to: increased HR, constriction of arterioles of skin and intestine, dilation of arterioles in skeletal muscle, raised BP, dilation of pupils, closing of sphincters, raising of hair, sweating
parasympathetic nervous system
“rest and digest” system
conserves and stores energy when body is relaxed (e.g. during sleep)
stimulation leads to: decreased HR, pupil constriction, increased peristalsis (increased GI motility), increased glandular activity, opening of sphincters, contraction of bladder wall
(parasympathetic is the parachute to slow down your body’s fight-or-flight)
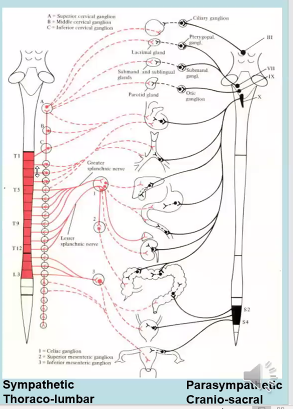
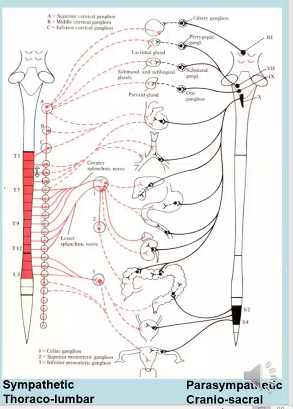
efferent origin of the ANS
spinal cord, broadly
sympathetic NS originates from thoraco-lumbar region (cell bodies in the lateral horn of T1-L2/3) (red in picture)
parasympathetic NS originates from cranio-sacral region (CN III, CN VII, CN IX, CN X, S2-4) (black in picture)
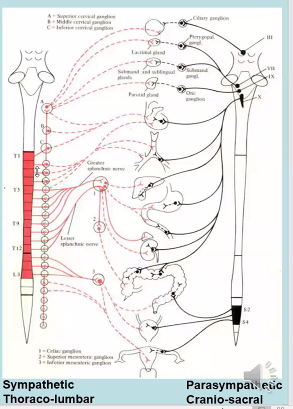
pathway of efferent sympathetic outflow
pre-ganglionic fibers originate from spinal cord → travel to sympathetic ganglion (parallel to spinal cord) → have synapse with post-sympathetic ganglion → releases neurotransmitter (ACh) → ACh stimulates post-ganglionic fiber → post-ganglionic fiber releases epinephrine → post-ganglionic fiber travels to internal organs and releases norepinephrine (norepinephrine binds to receptors on heart, etc)
in picture, circles are sympathetic ganglia (follow the red pathway)
adrenergic receptors
receptors in the sympathetic NS
receive norepinephrine
alpha receptors a-1 and a-2
beta receptors b-1 and b-2
dopamine receptors D1 and D2
effect depends on type of receptor and location on cell
cholinergic receptors
receptors in the parasympathetic NS (and sympathetic?)
receive ACh
peptidergic receptors
receptors in the parasympathetic NS
receive peptides, e.g. substance P, vasoactive inhibitory peptide
alpha-1 receptors
an adrenergic receptor
located on vascular smooth muscle of skin and splanchnic regions, GI and bladder sphincters, and radial muscle of iris
produce excitation (contraction)
equally sensitive to norepinephrine and epinephrine
^but only norepinephrine is released enough from adrenergic neurons to activate a-1 receptors
mechanism of action of an alpha-1 receptor
G-protein alpha stimulator → phospholipase C → inositol formation → IP3 → increase intracellular Ca2+ (because Ca2+ is needed for muscle contraction)
clinical point about norepinephrine
physiological effect of norepinephrine: muscle contraction and vasoconstriction
excessive release of norepinephrine or excess absorption → hypertension (side symptoms: headache, vertigo, nosebleeds, sleep disorder, excess sweating, heart palpitations)
treated with an alpha-1 receptor blocker, e.g. Prazosin
alpha-2 receptors
an adrenergic receptor
located in presynaptic nerve terminals, platelets, fat cells, walls of GI trat
often produce inhibition (relaxation, dilation)
receives only neuroepinephrine
mechanism of action of an alpha-2 receptor
G-protein alpha inhibitor → inhibition of adenylate cyclase → decrease in cAMP
beta-1 receptors
an adrenergic receptor
located in SA node, AV node, and ventricular muscle (myocardium) of heart
produces excitation (increased HR, increased conduction velocity, increased contractility)
sensitive to both norepinephrine and epinephrine
more sensitive than alpha-1 receptors
mechanism of action of a beta-1 receptor
activation of G-protein alpha-stimulator → activation of adenylate cyclase → increase in cAMP
(same as beta-2 mechanism)
clinical point: excess norepinephrine on the heart
increased heart rate
palpitations, tachycardia, arrhythmia
treated with beta-1 blockers, e.g. propranolol
beta-2 receptors
an adrenergic receptor
located on vascular smooth muscle of muscle, bronchial smooth muscle, in walls of GI tract and bladder, liver, pancreatic beta-cells
produces relaxation (dilation of vascular smooth muscle and bronchioles, relaxation of bladder wall)
more sensitive to epinephrine than norepinephrine
more sensitive to epinephrine than alpha-1 receptors
mechanism of action of a beta-2 receptor
activation of G-protein alpha-stimulator → activation of adenylate cyclase → increase in cAMP
(same as beta-1 mechanism)
clinical point about beta-2 receptors
asthmatic patients should be given beta-2 agonists, e.g. albuterol, to relax smooth muscle of bronchi
asthmatics with heart palpitations cannot be given propranolol + albuterol because propranolol blocks beta-1 and recognizes beta-2, but beta-2 doesn’t want to be blocked (would aggravate asthma)
atenolol + albuterol is better for asthmatics
key points about beta blockers and agonists
Propranolol is Beta blocker 1 and 2
Albuterol is beta 2 agonist
Atenolol is Beta 1 blocker (not Beta 2)
nicotinic receptors
a cholinergic receptor
located in autonomic ganglia of sympathetic and parasympathetic NS, at neuromuscular junction, and in adrenal medulla
^receptors are similar, not identical
activated by ACh or nicotine
produce excitation
blocked by ganglionic blockers in autonomic ganglia, but not at neuromuscular junction
mechanism of action for nicotinic receptors
ACh binds to alpha subunits of receptor
receptors also serve as ion channels for Na+ and K+
muscarinic receptors
a cholinergic receptor
located in heart, smooth muscle, and glands
inhibitory in heart
excitatory in smooth muscle and glands (decreased HR
activated by ACh and muscarine
blocked by atropine
mechanism of action of
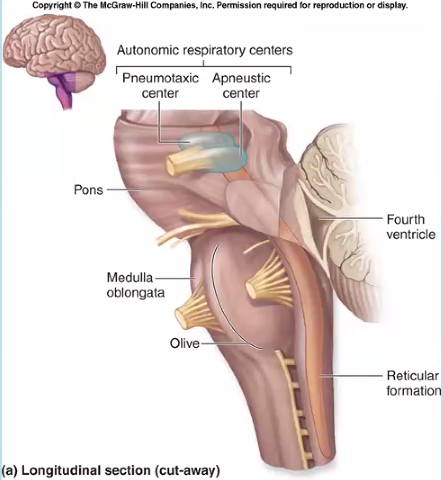
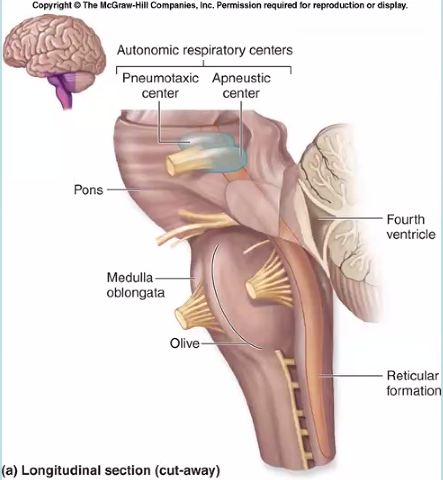
brain stem
made of the medulla oblongata, pons, and midbrain
a collection of autonomic centers
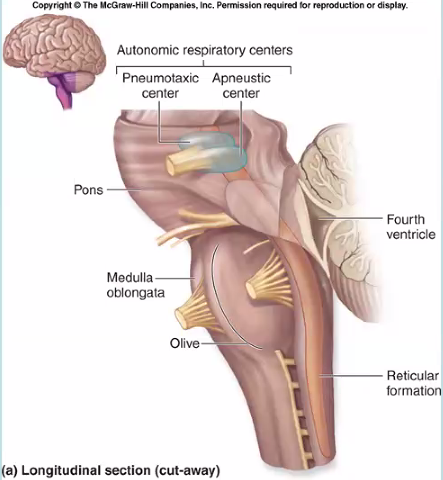
medulla as an autonomic center
vasomotor center
respiratory center
swallowing, coughing, and vomiting centers
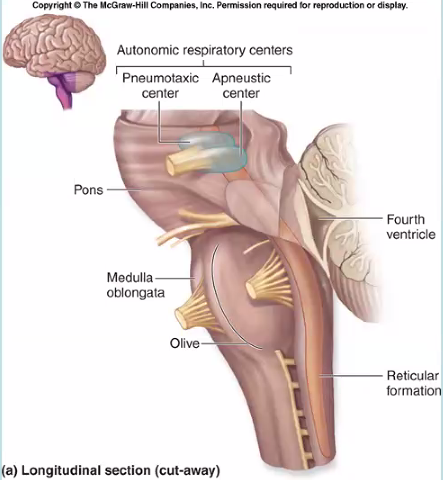
pons as an autonomic center
pneumotaxic center (part of the autonomic respiratory centers)
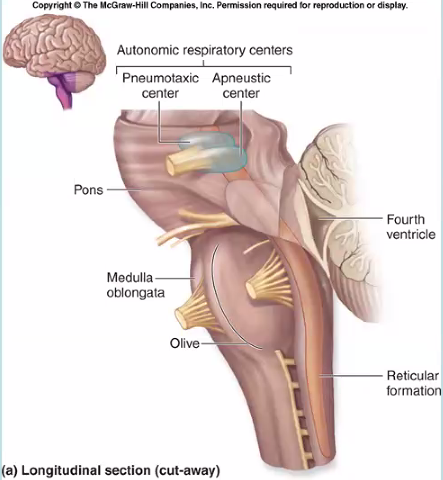
midbrain as an autonomic center
micturition center (part of the renal system)
hypothalamus as an autonomic center
temperature regulation center
thirst and food intake regulatory centers
difference in neurotransmitters of the ANS
preganglionic: ACh
postganglionic: ACh in parasympathetic, norepinephrine in sympathetic
when there is excess ACh secretion from vagus nerve in parasympathetic, what is side effect in heart?
bradycardia, decreased contractility, decreased conduction velocity
sympathetic NS effects on the eye
alpha-2 receptors dilate pupils
beta-receptors accommodate the ciliary muscle
decreased secretion in lacrimal gland
parasympathetic NS effect on eye
salivary glands
parasympathetic salivary glands
sympathetic on heart
parasympathetic on heart
chronotropic
heart rate
dromotropic
conductivity
sympathetic lungs
parasympathetic lungs
clinical case: excess ACh, what is the side effect on heart?
bradycardia
clinical case: xs ACh, side effect on GI tract?
increased peristalsis → diarrhea?
xs ACh → side effect on stomach?
increased HCl secretion for digestion → gastritis
clinical case: oversecretion of norepinephrine → side effect on heart?
tachycardia, arrhythmia, palpitations
clinical case: pt has constipation, erectile dysfunction, palpitations, hypertension
excess norepinephrine production, not enough ACh