Comprehensive Reproductive Physiology: Male and Female Systems, Fertilization, and Childbirth
1/152
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
153 Terms
What is the genetic sex determination process at fertilization?
The sperm determines the sex of the offspring; X-bearing sperm results in female (XX) and Y-bearing sperm results in male (XY).
What happens during the indifferent stage of embryonic development?
The gonads are undifferentiated and can develop into either testes or ovaries.
What triggers the gonads to develop into testes?
The presence of the Y chromosome and activation of the SRY gene around 6 weeks of embryonic development.
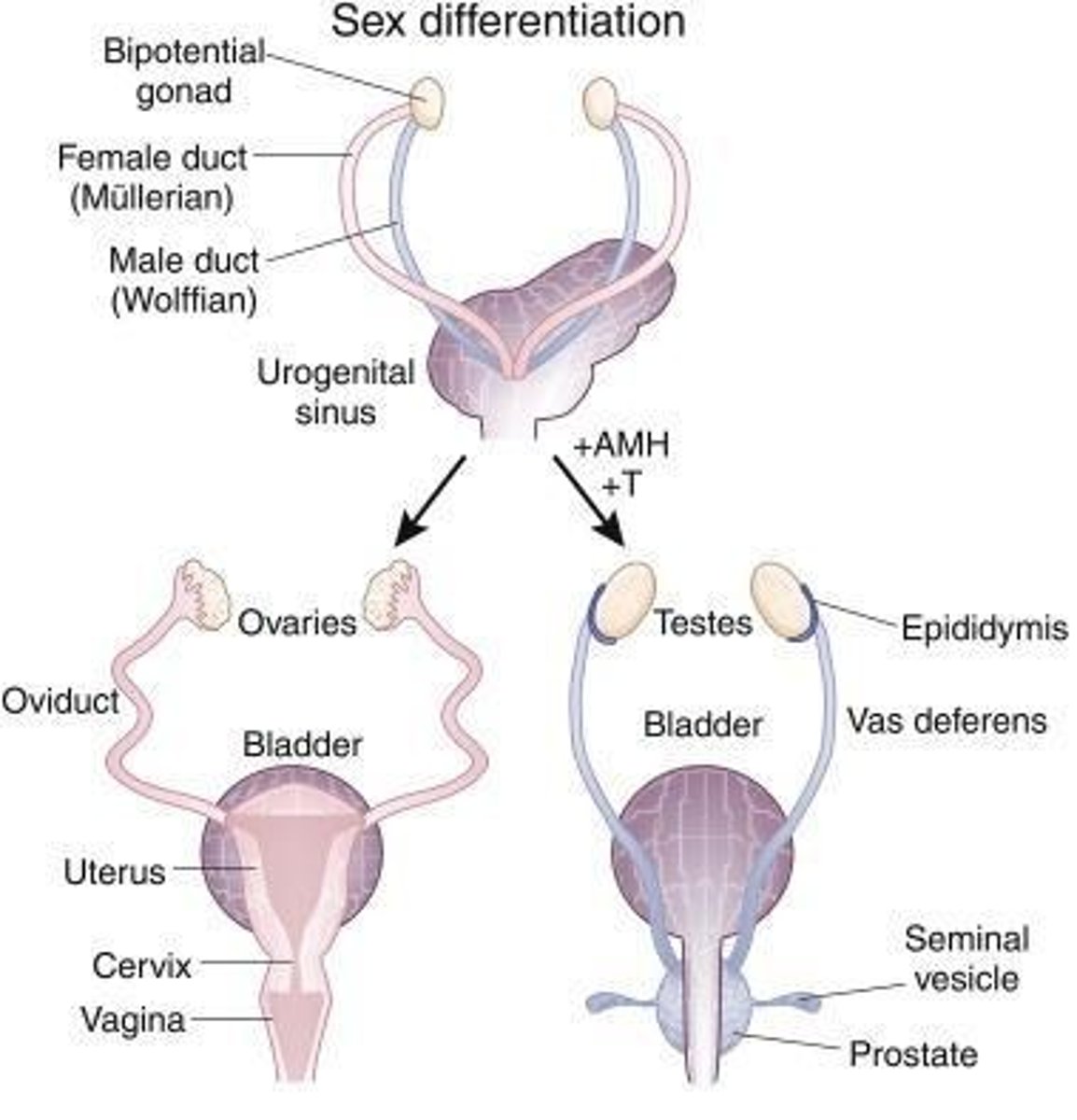
What is the role of testosterone in male sexual differentiation?
Testosterone stimulates the Wolffian ducts to develop into male internal organs and external genitalia.
What is the function of anti-Müllerian hormone (AMH) in male development?
AMH causes the regression of the female-precursor (Müllerian) ducts.
What is the primary function of the testes?
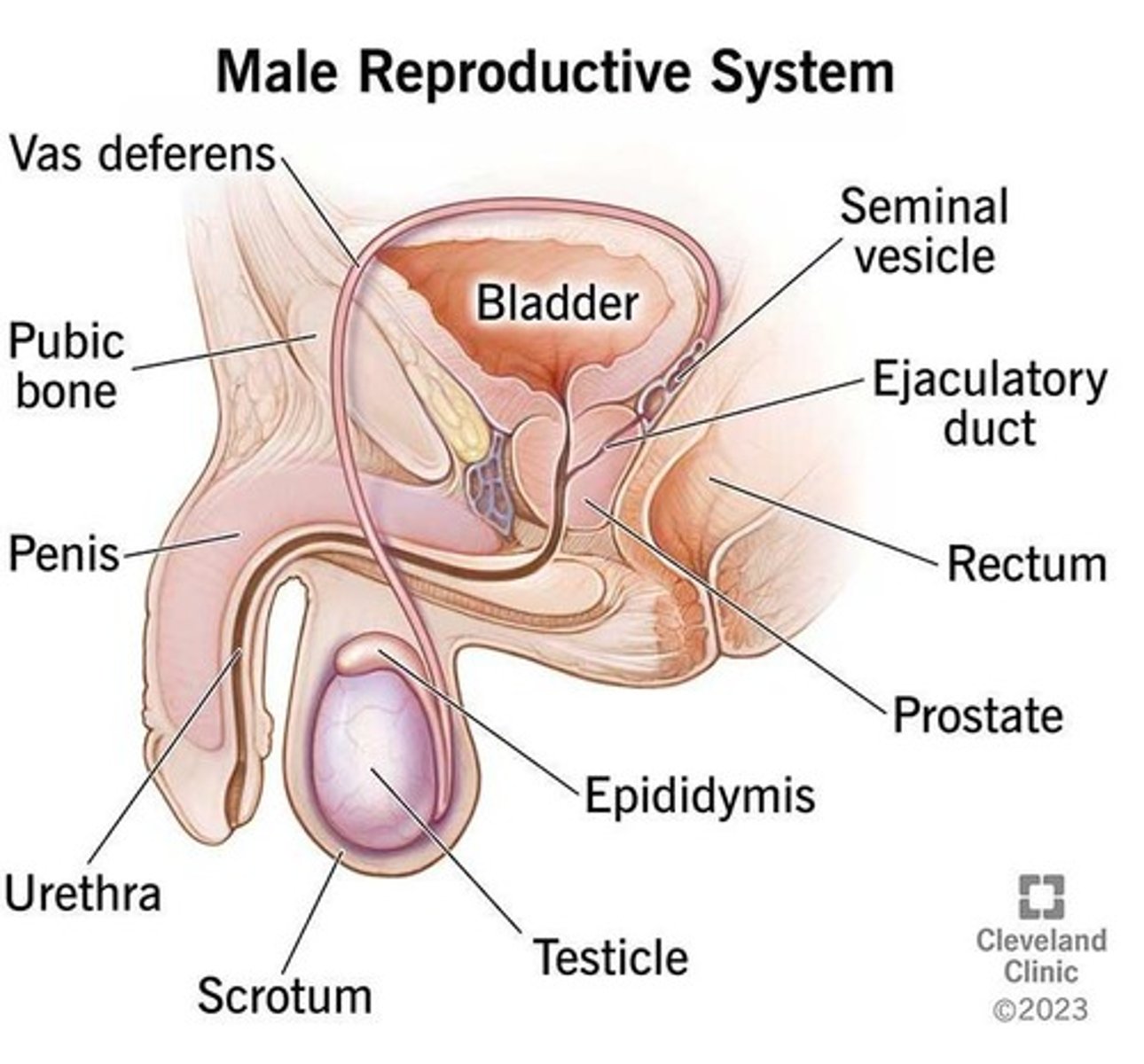
To produce sperm (spermatogenesis) and secrete sex steroids.
What is the role of the epididymis?
It is responsible for sperm maturation, storage, and development of motility.
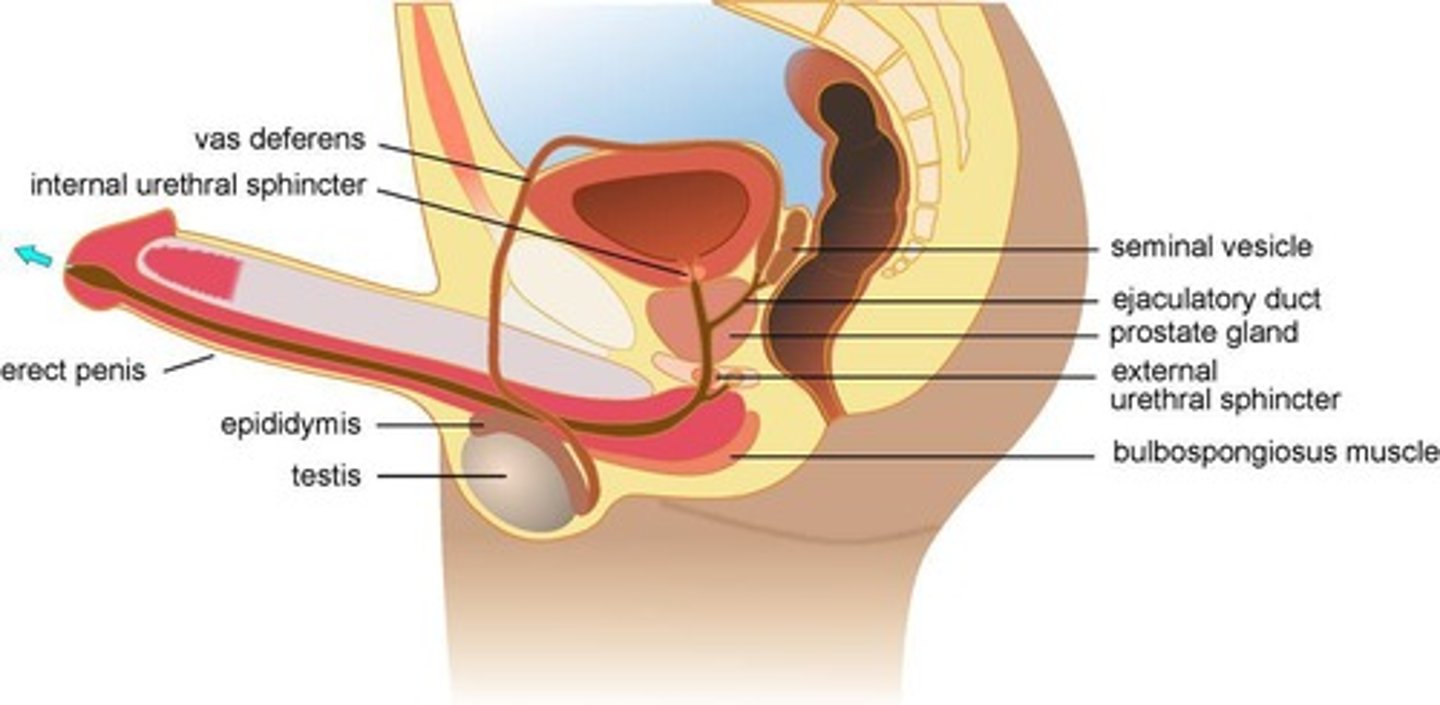
What do the seminal vesicles produce?
The majority of seminal fluid, which contains fructose and prostaglandins.
What is the function of the prostate gland?
It adds alkaline fluid to neutralize vaginal acidity and activates sperm.
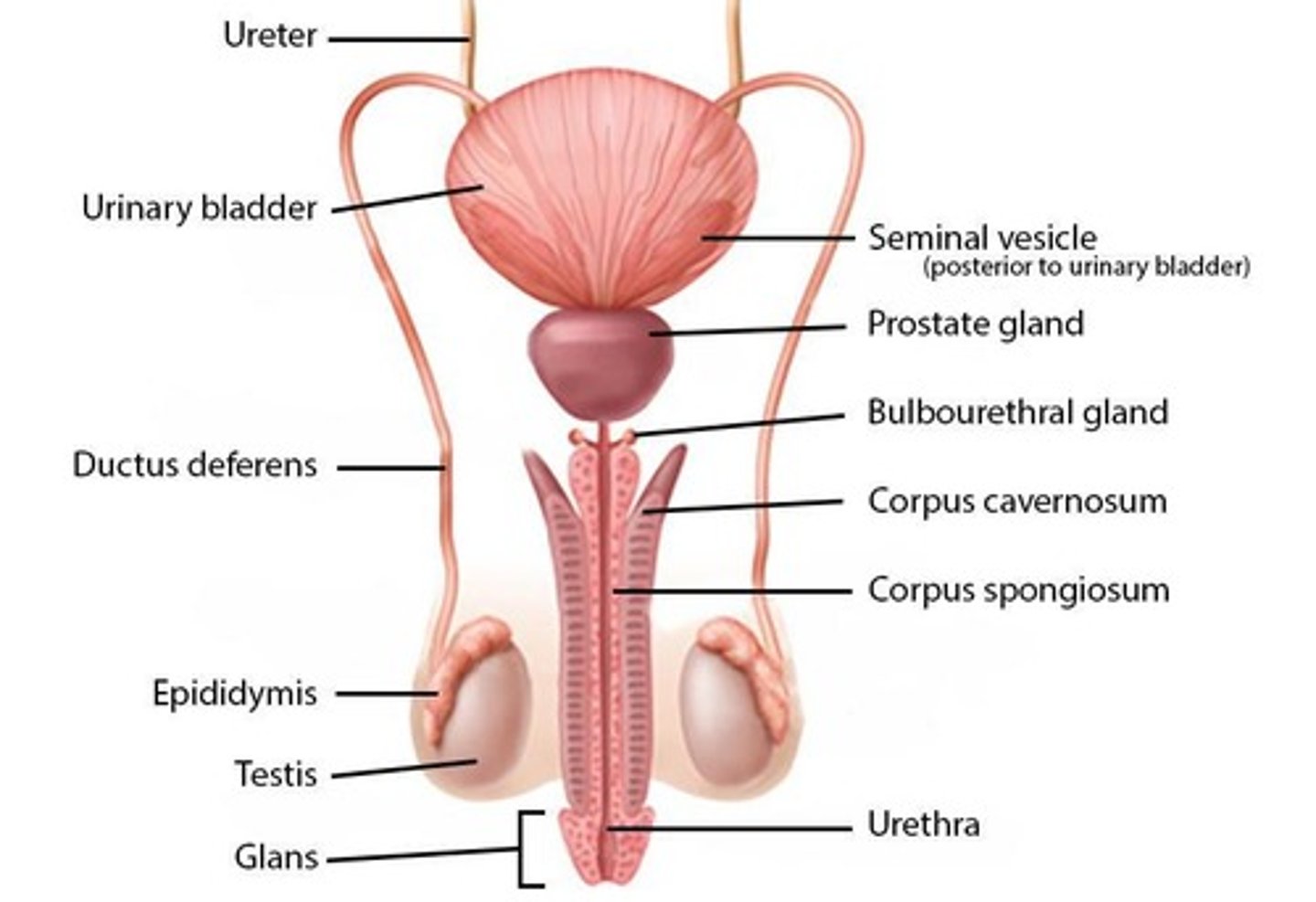
What is the role of the bulbourethral (Cowper's) glands?
They produce pre-ejaculate for lubrication and urethral cleansing.
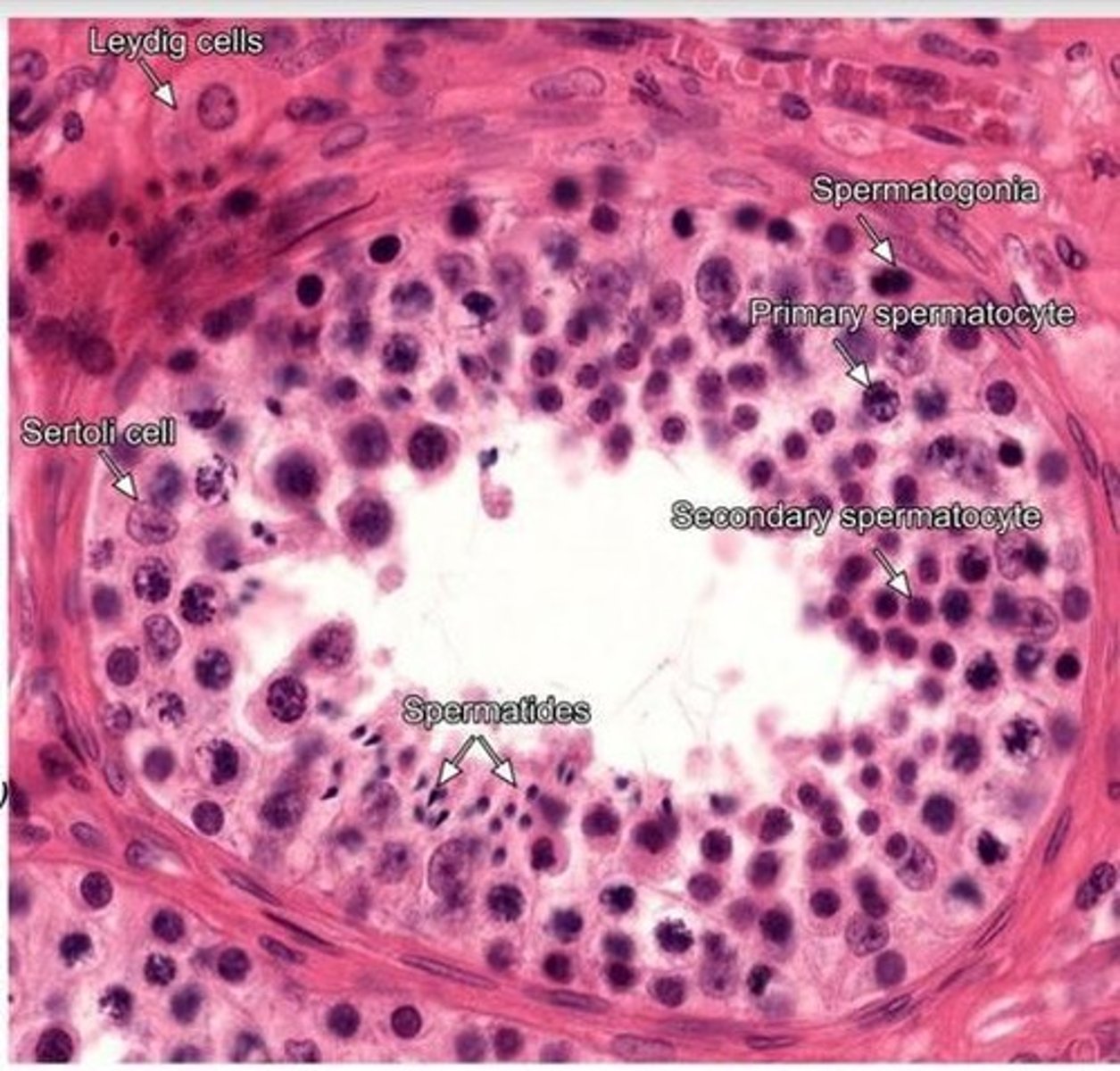
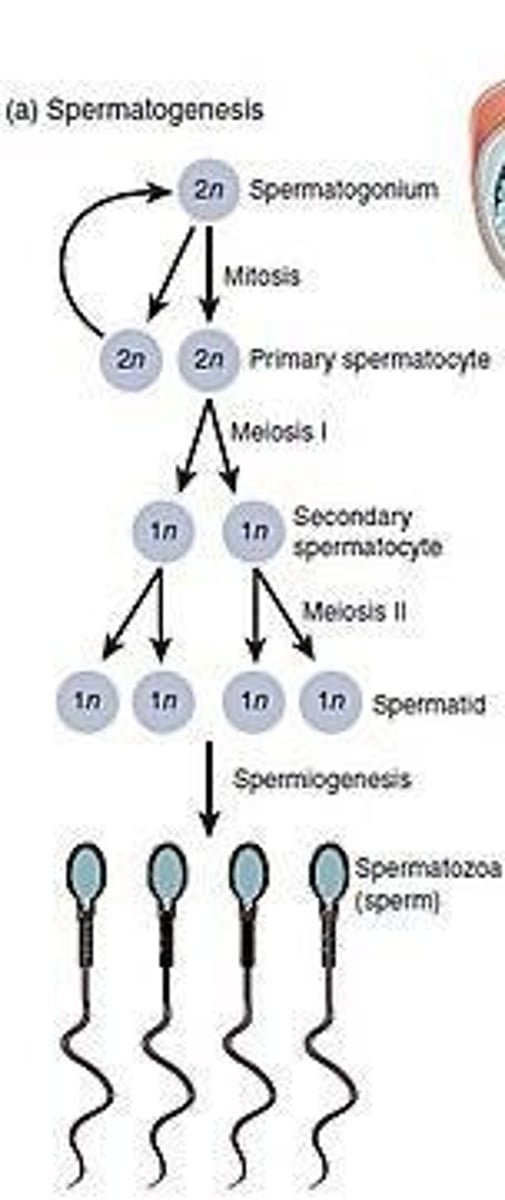
What is spermatogenesis?
The production of mature spermatozoa from germ cells, occurring in the seminiferous tubules of the testes.
At what age does spermatogenesis typically begin?
Around puberty, approximately 13 years old. It continues throughout life, but declines with age.
What is the duration of the full spermatogenesis process?
Approximately 74 days.
What do primordial germ cells become?
Spermatogonia in the embryonic testes, and these are dormant until puberty.
What occurs during mitosis stage of spermatogenesis?
Spermatogonia produce primary spermatocytes, diploid becomes diploid. We have 46 chromosomes at this point
What occurs during meiosis 1 stage of spermatogenesis?
Primary spermatocytes move toward the lumen and become secondary spermatocytes. We have 23 chromosomes, they are haploid but double chromatids.
What occurs during meiosis II stage of spermatogenesis?
Secondary spermatocytes produce 4 spermatids. Haploid produces haploid, and chromatids split.
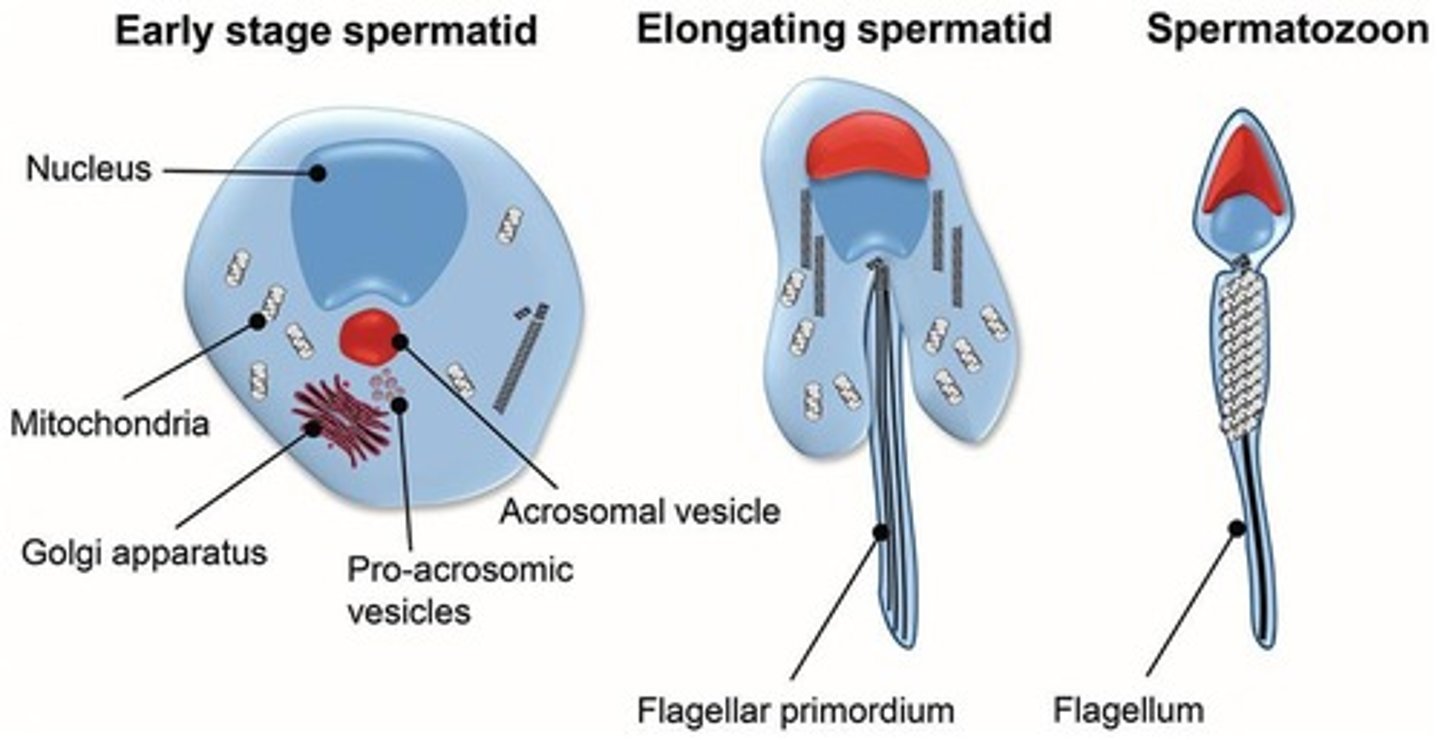
What occurs during spermiogenesis stage of spermatogenesis?
Spermatids enter the lumen of the seminiferous tubule and undergo spermiogenesis and acquire a tail and turn into a sperm. These are morphologic changes only!
What is the process of spermiogenesis?
The maturation of spermatids into sperm, acquiring a tail and becoming motile.
What are the two main types of cells involved in spermatogenesis?
Leydig cells (testosterone factories) and Sertoli cells ("nurse cells" that support and nourish developing germ cells).
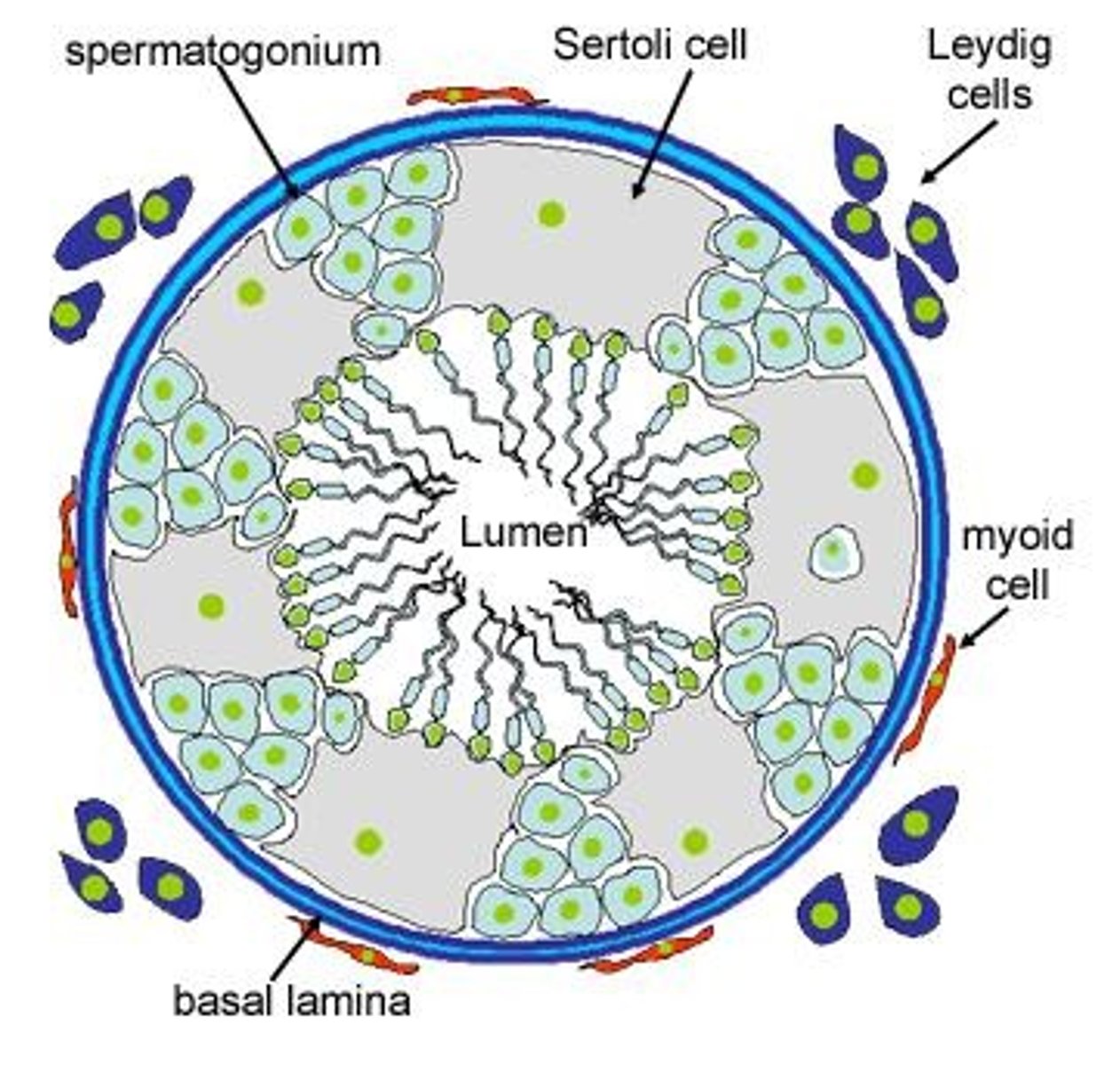
Where are Leydig cells?
Located in interstitial space between seminiferous tubules
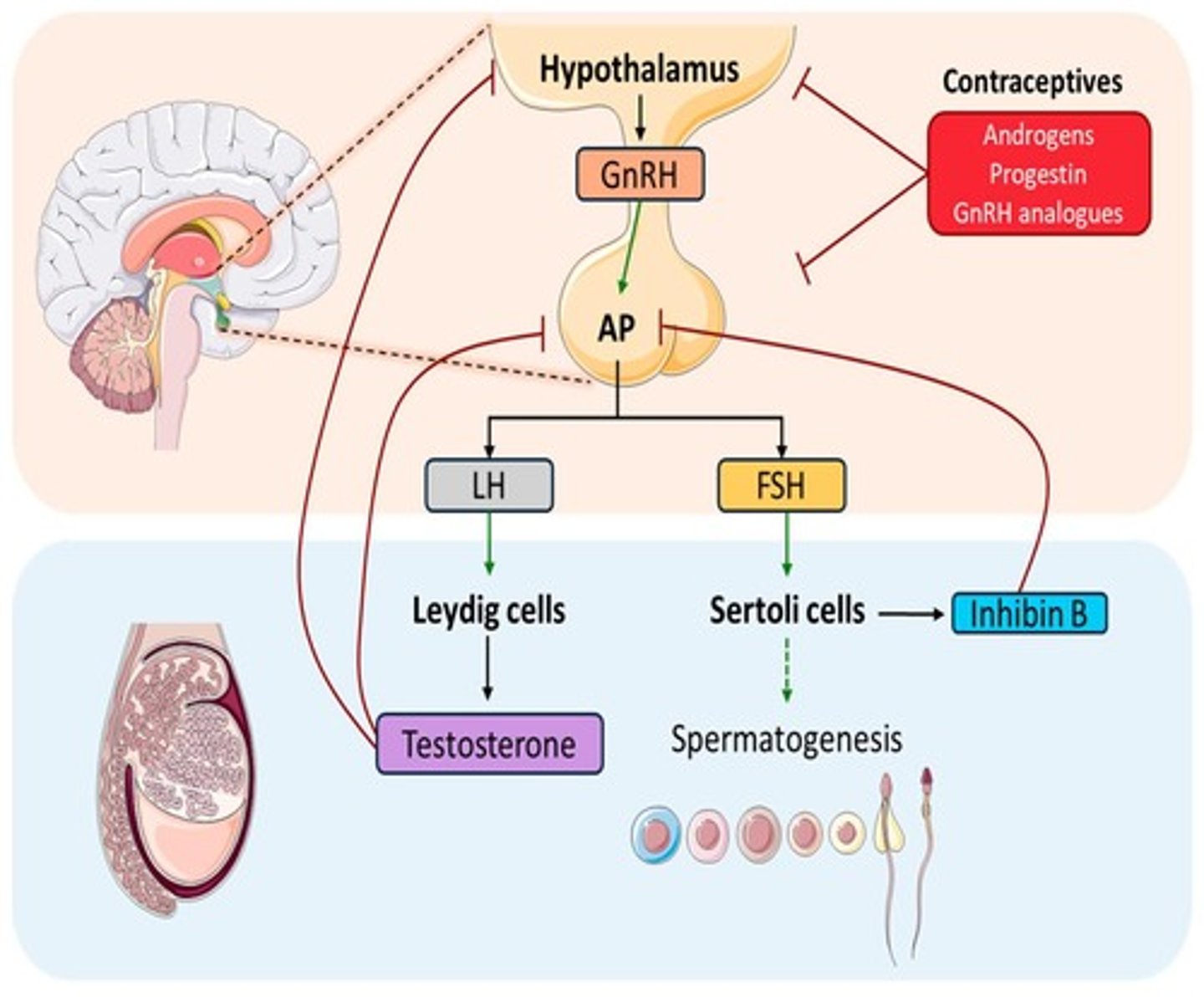
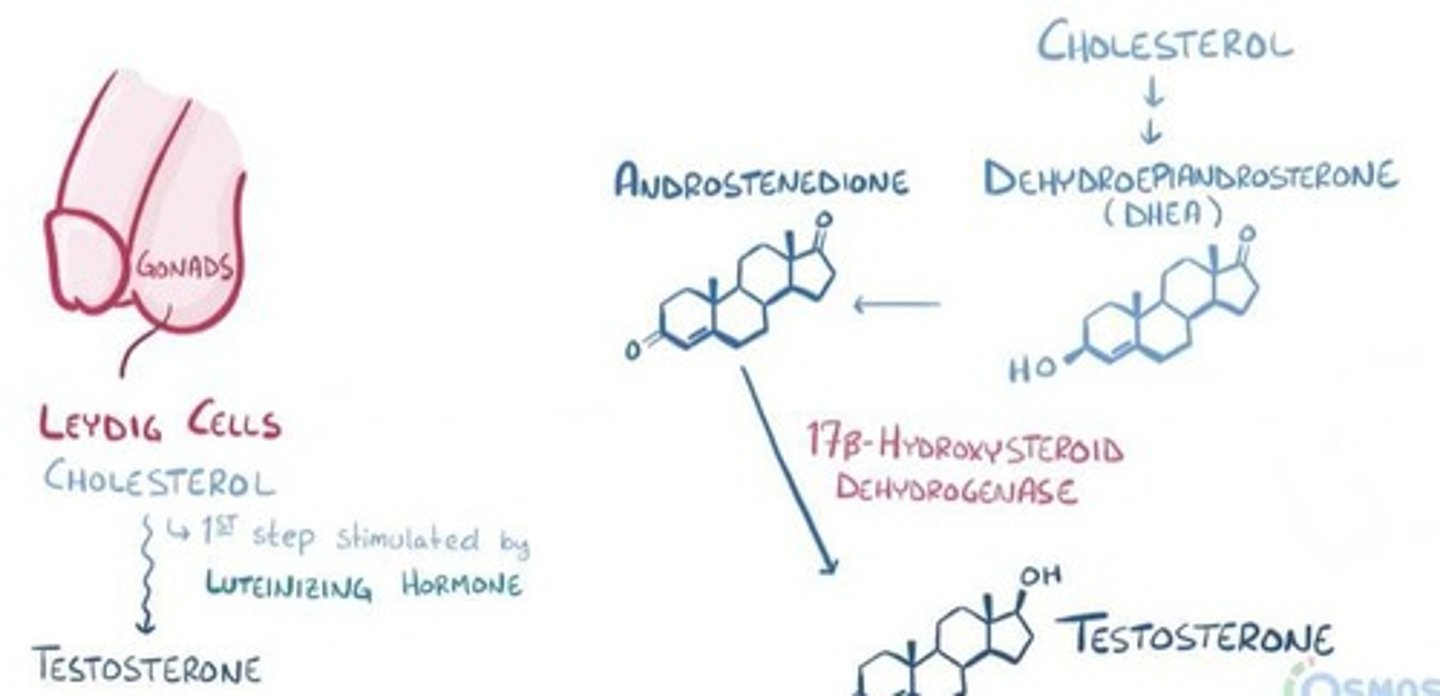
What hormone stimulates Leydig cells to produce testosterone?
Luteinizing hormone (LH).
What is the role of Sertoli cells in spermatogenesis?
They provide support and nourishment for developing germ cells, form the blood-testis barrier, produce androgen-binding protein and secretes inhibin B
What is the role of follicle-stimulating hormone (FSH) in spermatogenesis?
FSH acts on Sertoli cells to produce androgen-binding protein, allowing testosterone to enter the seminiferous tubules and support sperm development. x
What gets spermatogenesis going?
Increased concentration of FSH, LH and testosterone
What is the significance of inhibin in spermatogenesis?
Inhibin suppresses FSH secretion from the pituitary gland, preventing overproduction of sperm.
Where is GnRH released from?
Hypothalamus in pulsative pattern at puberty.
What is the role of GnRH in reproductive physiology?
It stimulates the anterior pituitary to secrete LH and FSH.
What negative feedback mechanisms maintain hormone balance?
Inhibin goes to the pituitary and reduces FSH to prevent an overproduction of sperm. Testosterone circulates back to hypothalamus causing a decrease in GnRH, LH and FSH.
What are the primary functions of testosterone?
Drives male sexual development, supports libido and fertility, and has anabolic effects on muscle and bone.
What is the metabolic origin of testosterone?
Testosterone is synthesized from cholesterol in Leydig cells, stimulated by LH.
How is testosterone transported in the body?
It circulates mostly bound to sex hormone-binding globulin (SHBG) and albumin.
What is the biologically active form of testosterone?
Free testosterone, secreted at much lower level
What are the two mechanisms of action for testosterone in target tissues?
Direct action of testosterone binding to intracellular androgen receptors and conversion to DHT via 5-alpha reductase.

Where does direct action of testosterone predominantly occur?
In skeletal muscle, bone, brain, and testes (spermatogenesis).
What is DHT and how does it compare to testosterone?
DHT (dihydrotestosterone) is a more potent androgen, 3-5 times stronger than testosterone.
In which tissues does DHT predominantly act?
In the prostate gland, external genitalia, hair follicles, epididymis, skin, and urethra.
What are the effects of dihydrotestosterone (DHT) in males?
It promotes prostate growth, external male genital development, and male pattern hair growth.
What effects do testosterone and DHT have on gene expression?
They activate gene expression leading to muscle growth, bone development, and differentiation of male reproductive structures.
What is the structure of a sperm head?
It contains a condensed nucleus with paternal DNA and is covered by an acrosome filled with enzymes.
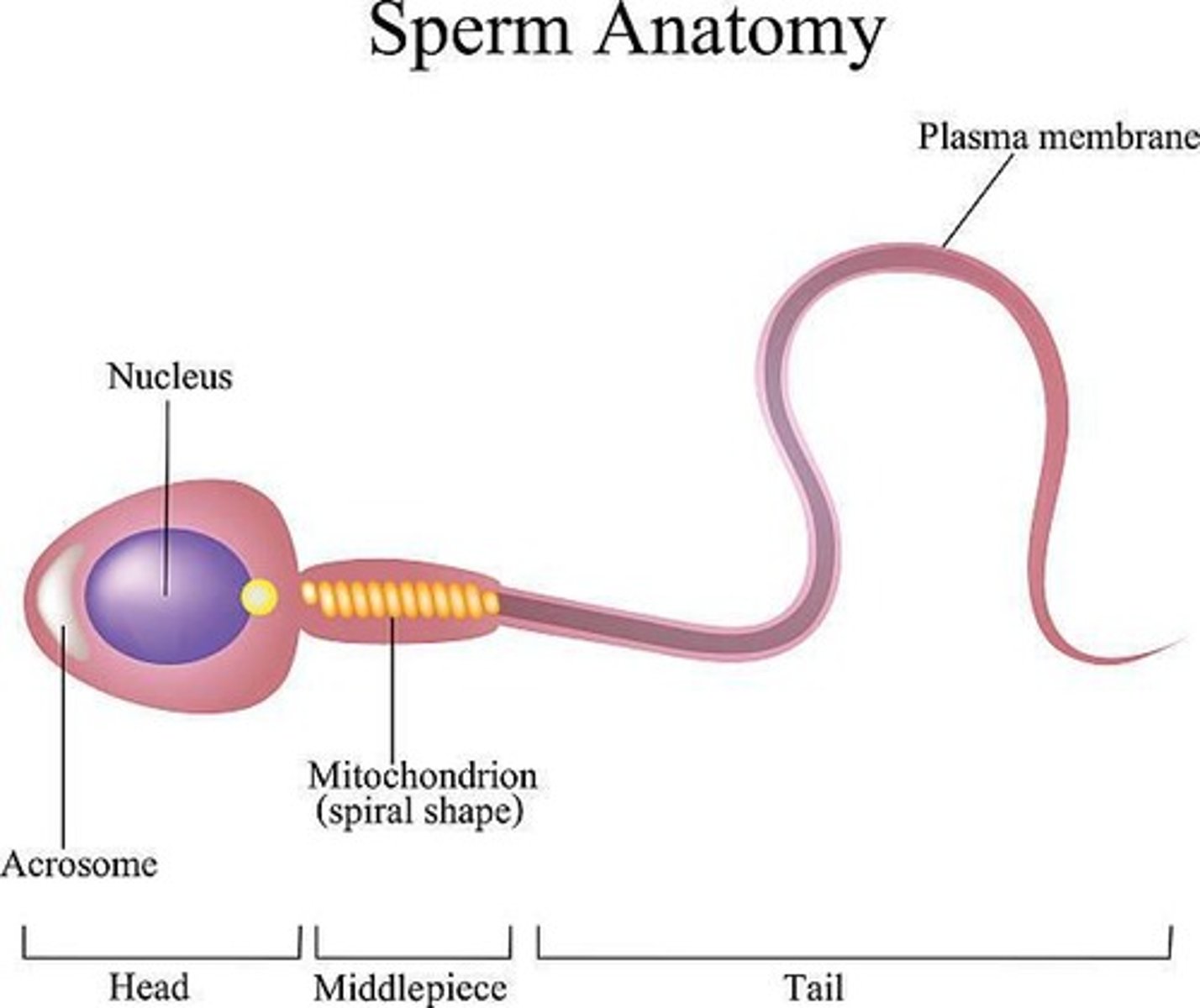
What is the function of the acrosome in sperm?
It's a cap filled with enzymes (hyaluronidase and proteolytic enzymes) that helps sperm penetrate the oocyte during fertilization.
What is packed in the body/midpiece of a sperm?
Mitochondria that provide ATP needed for tail movement and motility.
What is the tail of the sperm made of?
An axoneme, similar to cilia, surrounded by a thin plasma membrane.
How are newly formed sperm transported from the seminiferous tubules?
They are moved by peristaltic contractions to the epididymis. They are non-motile and need to learn to swim!
What occurs during sperm maturation in the epididymis?
Sperm gain motility (learn to swim), undergo final biochemical changes, and are stored for several days.
What do inhibitory proteins in epididymal fluid do?
They keep sperm immobile until ejaculation.
What happens to sperm during ejaculation?
Sperm move from the epididymis through the vas deferens, ampulla, ejaculatory duct, and prostatic urethra.
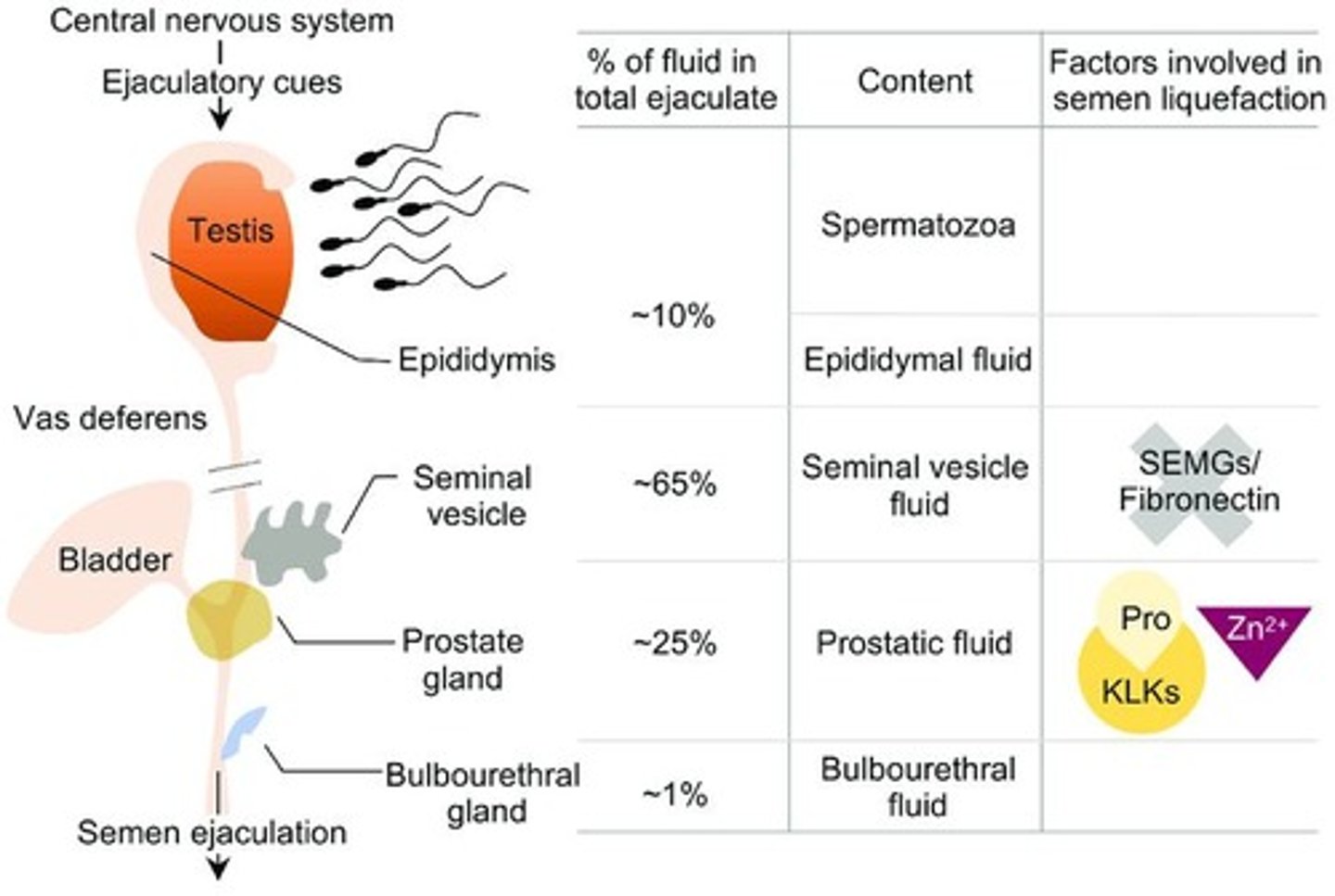
What does sperm mix with?
Seminal vesicle fluid, prostatic fluid and bulbourethral gland mucus.
How does alkaline prostate fluid affect vaginal acidity?
It neutralizes vaginal acidity.
What is capacitation in sperm?
It is the final activation of sperm that occurs upon exposure to female fluids, removing inhibitory proteins, enabling hyperactive motility, acrosome reaction and the ability to fertilize an oocyte.

What components make up semen?
10% fluid and sperm from the vas deferens, 60% from seminal vesicles, and 30% from the prostate.
What role do prostaglandins play in semen?
They make cervical mucus more receptive to sperm movement and cause reverse peristalsis in the uterus and tubes, which moves sperm towards ovaries.
What is the pH of prostatic fluid and why is it important?
It is alkaline (about pH 7), which supports sperm motility and protects sperm in the acidic vagina.
What is the overall pH of semen?
Approximately 7.5
At what pH do sperm become optimally motile?
At pH 6.0 to 6.5.
What is the role of prostatic secretions in semen?
They enhance sperm survival and motility.
What happens to semen after ejaculation?
It coagulates due to clotting factors.
What dissolves the semen clot after several minutes?
Profibrinolysin.
When does sperm become fully active?
Once it's liquefied
What is the primary erectile tissue responsible for erections?
Corpus cavernosum.
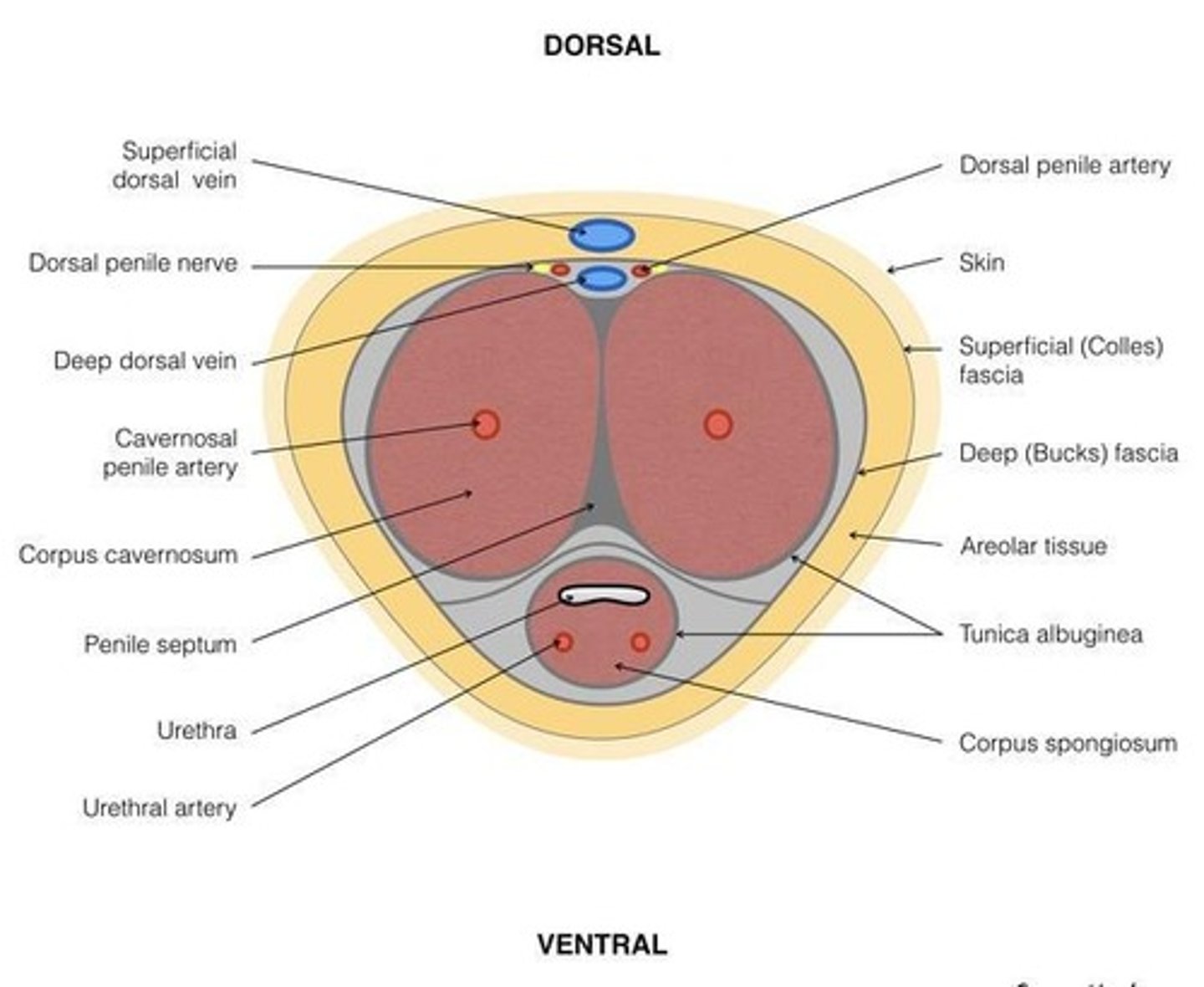
What role does the corpus spongiosum play in erection?
It contains the urethra and prevents urethral compression.
What is the primary trigger for reflex pathways during male sexual response?
The glans penis.
Which nerve is responsible for sensory innervation in the male sexual response?
Pudendal nerve.
What is the parasympathetic nerve responsible for erection?
Pelvic nerve (S2-S4). (point)
What sympathetic nerves are involved in emission and ejaculation?
Hypogastric plexus (T12-L2). (shoot)
What drives the male sexual response?
Psychogenic input and reflexogenic input
How do sensory impulses from the glans penis travel to the brain?
Travel through the pudendal nerve, into the sacral spinal reflex center, where they are integrated within the spinal cord and relayed to the brain.
What is psychogenic input?
Input from the brain leading to erection and ejaculation. Can result from tactile, visual, olfactory, emotional or filling of internal organs. As we knew, anything gets a man off.
What is reflexogenic input?
Local stimulation, which is direct genital stimulation, activating spinal reflex circuits on its own.
How can an erection or ejaculation be triggered without brain involvement?
Through spinal reflexes, and local stimulation.
What neurotransmitters are released during erection (parasympathetic mechanism)?
Nitric oxide (NO), vasoactive intestinal peptide (VIP), and acetylcholine (Ach), which forms cGMP
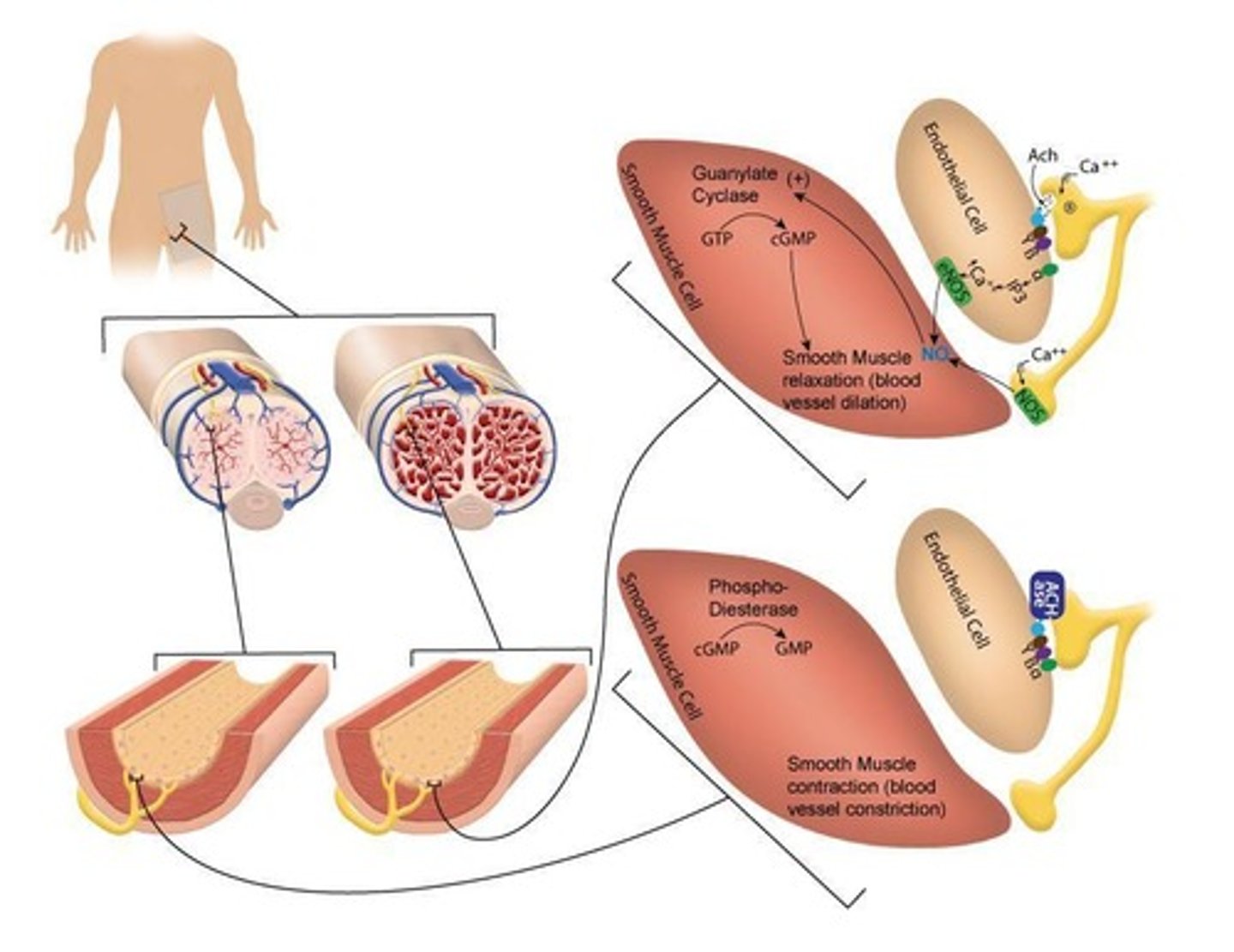
What is the result of increased cGMP in erectile tissue?
Relaxation of cavernosal arteries, and trabecular smooth muscle. This increase arterial inflow, leading to corpora cavernosum to engorge with blood.
How is the venous outflow decreased during an erection?
Tunica albuginea compresses subtunical veins.
What happens during emission?
Sexual stimulation intensifies, reflex centers of the spinal cord shift to sympathetic output and pass into genital organs.
What triggers emission during male sexual response?
Contraction of the vas deferens and ampulla.
How is fluid added during emission?
Seminal vesicles and prostate contracting
What triggers ejaculation phase?
Semen in urethra triggers sensory input, signaling pudendal nerve and spinal cord.
Where is semen formed?
Prostatic urethra
What occurs during ejaculation?
Fullness in genitals triggers rhythmic contractions of ischiocavernosus and bulbocavernosus muscles and smooth muscle in genital ducts. As pressure increases, semen is expelled through urethra.
What prevents retrograde ejaculation?
Contraction of the bladder sphincter.
What is the resolution phase?
Loss of parasympathetic tone, erection loss, after ejaculation.
What are common causes of erectile dysfunction?
Neurologic causes, deficient testosterone levels, drugs, psychological factors, and vascular disease.
How do PDE-5 inhibitors treat erectile dysfunction?
They increase cGMP levels by inhibiting the enzyme phosphodiesterase-5.
What are the main internal structures of the female reproductive system?
Ovaries, fallopian tubes, uterus, cervix, and vagina.
What hormones do the ovaries produce?
Estrogen and progesterone.
What are the main external features of the female genitalia?
Mons pubis, labia majora, labia minora, clitoris, vestibule
What is the role of theca cells in the ovaries?
They form the outer layer of the follicle, LH binds and triggers cell to synthesize androgens, and provide structural support for follicle.
What is the function of granulosa cells?
Crucial for egg maturation and producing hormones like estrogen, inhibin and progesterone. They also support follicular development.
What does FSH binding to granulosa cells result in?
Production of aromatase, which is then used to convert androstenedione (from theca cells) into estradiol.
What are the stages of oogenesis?
1. Pre-natal development, 2. Growing follicle phase, 3. Pre-ovulatory maturation, 4. Fertilization.
What is stage 1 of oocyte development?
Occurs from prenatal to puberty, and primary oocytes are arrested in prophase 1
How many oogonia will become primary oocytes?
2 million out of 7 million, when they enter meiosis 1.
During what gestational weeks will multiplying of diploid oogonia occur?
From weeks 9-22
What is phase 2 of oogenesis/oocyte development?
Growing follicular phase, occurring at puberty.
What occurs during stage 2 of oocyte development?
Multiple follicles (5-20) begin the maturation sequence. These cells are still stuck in prophase I. Granulosa and theca cells, proliferate, antral fluid forms, estrogen production increases.
What is the maturation sequence?
Primary follicle → secondary → tertiary (Graafian)
How long is stage 2 of oocyte development?
About 75-80 days
What is stage 3 of oocyte development?
Pre-ovulatory maturation
When does phase 3 of oocyte development begin?
When Graafian follicles are ready, this occurs during the follicular phase
What triggers the completion of Meiosis I in oocyte development?
The dominant Graafian follicle forms a secondary HAPLOID oocyte and first polar body.