RCC 1001 Final
1/133
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
134 Terms
In the closed sandwich technique, at what thickness is the liner applied?
0.5 mm
- In the open sandwich, applies as >1.0 mm base
In the open sandwich technique, the GI/RMGI must form the contact with the adjacent teeth. (T/F)
False
- Must NOT form the contact (must be below)
Conventional GI provides a significant increase in dentine hardness at the cervical margins, while RMGI does not. (T/F)
True, creates highest amount of calcium -> decreases caries risk
GIC/RMGI are useful in a restoration because they provide:
A better seal at dental margins (stabilize adhesive interface) and release fluoride
- Requires composite lamination to improve resistance to forces
All of the following are advantages of deep marginal elevation, except:
A. Supragingival elevation of margins
B. Seals dentin
C. Creates undercuts to stabilize restoration
D. Geometry for inlay/onlay restorations
C, fills undercuts and reinforces undermined cusps
Overall, DME is a successful long-term solution
Surefill SDR is a bulkfill flowable with less shrinkage, but it should not be placed on what surfaces?
Occlusal and proximal, due to its low filler content
Enamel is avascular, while the dentin-pulp complex is vital and responds to injuries. (T/F)
True
The dentin-pulp complex has a cellular-driven defense against:
pH fluctuations in the biofilm
- Tubular/peritubular mineralization, tertiary dentin
Deep dentin has less tubules with smaller diameters. (T/F)
False, more tubules (38,000-45,000) with larger diameter (1.6-2.5 micrometers)
Adhesive binds better at the superficial dentin. Why?
Less water content, and the adhesive is hydrophobic
- Deep dentin has more peritubular dentin (greater SA), however its high water content makes adhesion more difficult
When does the DPC react to caries?
Early, before demineralization reaches DEJ or enamel breakdown
- Pre-dentin reduction, pulp cells in cell-free-zone, and dentin hypermineralization (tubular sclerosis)
Tubular sclerosis forms a ___________ zone.
Translucent (minerals in tubules gives homogenous appearance)
In the progressive stages of lesion formation, what is the first zone to form?
Translucent (sclerotic) zone, followed by zone of demineralization
- Reactive dentin is next, and the zone of bacterial invasion forms last
Tertiary dentin is not as hard as primary dentin. (T/F)
True, less mineralized and irregular tubules
Histology of primary dentin
- Smooth odontoblastic processes
- No intratubular crystals
- Intertubular dentin cross-banded collagen and dense-apatite crystals
Hard, only cut by bur or sharp cutting intstrument
Secondary dentin has the same histology and clinical appearance
How does sclerotic dentin differ from primary dentin?
Dark and harder
- Can be seen before demineralization reaches dentin
Sclerotic vs tertiary dentin
Sclerotic
- Translucent zone
- Responds to aging, mild irritation
- Seal dentinal tubules to wall of lesion
- Crystalline material precipitates
- Harder than normal dentin
Tertiary
- Reaction = reparative
- Responds to caries, attrition, and operative
- Localized dentin deposit
- Not as hard as primary
Affected dentin contains less bacteria than infected dentin. (T/F)
True
Firm dentin is infected dentin. (T/F)
False, it is affected
- Infected dentin is soft dentin
Histologically, firm dentin may be referred to as:
Demineralized intertubular dentin
- Collagen cross-linking remains
- Remineralizable as long as pulp stays vital
- Formation of intratubular fine crystals
- Transparent appearance
All of the following is a characteristic of soft dentin, except:
A. Denatured collagen
B. Bacteria
C. High mineral content
D. No self-repair
C, low mineral content
The transition between soft and firm dentin has a ____________ texture.
Leathery
The difference between the zones becomes less distinct with rapidly progressing lesions. (T/F)
True
Infected dentin is remineralizable. (T/F)
False
What is considered hard dentin?
Tertiary dentin, sclerotic dentin, and normal (or sound) dentin
In slow progressing lesions, what occurs with the tubules?
Sealing of tubules and occlusion
- In rapid lesion odontoblast processes are destroyed with open tubule pathway
Diagnosis of reversible pulpitis includes:
- Presence of pain
- Color
- Periapical lesions
Diagnosis of irreversible pulpitis includes:
- Controlled bleeding
- Infection/trauma?
- Cold test response
If bacterial invasion penetrates the tertiary dentin,
A severely inflamed pulp occurs, followed by necrosis
Cavitated lesions cannot be arrested in their progression. (T/F)
False, cavitated or intact can be arrested by plaque control
When reducing cusps for a complex restoration, how much should functional cusps be reduced?
2-2.5 mm
- Non-functional cusps should be reduced 1.5-2 mm
Functional cusps are 2x more likely to fracture than non-functional cusps. (T/F)
False, less likely
- Buccal cusps fracture more for maxillary arch and lingual cusps fracture more for the mandibular arch
Retention grooves should be placed ______ mm (inside/outside) the DEJ.
0.2 mm, inside the DEJ
- With depth of 0.3-0.5 mm (1/4 round bur or 169L)
What bur is used for a horizontal slot?
Round bur #1, 0.5 mm inside the dentin
What burs are used for placing an amalgam pin and at what depth?
#330 or #245 at a depth of 1-1.5 mm
- The #4 round bur is used to contra-bevel on the junction of the pulpal floor
As a rule, one metal pin per missing line angle should be used. (T/F)
True
The preparation prior to placement of a metal pin should be _______ in depth.
4 mm
- 2 mm for amalgam, 2 mm for metal pin
Metal pins can only be placed vertically. (T/F)
False, vertically and horizontally
What should the position of the metal pinhole be?
No closer than 0.5-1 mm from DEJ or 1-1.5 mm from external tooth surface
- Should be placed parallel to external surface of tooth
Complex amalgam restorations have proven longevity. (T/F)
True
What is the resistance form for complex amalgam?
90 degree CSM, rounded internal angles, and a depth of at least 1.5 mm
What is the retention form for complex amalgam?
Convergent, dove tails, retention features (slots, coves, box, pin)
What are the indications for a complex RBC restoration?
- Provisional restoration for teeth with questionable prognosis
- Interim restorations during disease control process
- Financial cost
How can you prevent errors in axial contour during a RBC complex restoration?
Use the appropriate band and wedge
How does vital pulp therapy preserve pulpal health?
Formation of tertiary reparative dentin or calcific bridge
Electric pulp test stimulates a ______________ sensation. A reading between _________ represents vital pulp.
Tingling, 1-79 (necrotic = 80)
In reversible pulpitis, the response to cold is grossly exaggerated. (T/F)
False, slightly exaggerated (hyperresponsive)
- Requires stimulus for painful response of short duration
How is asymptomatic irreversible pulpitis diagnosed?
Clinic and radiographic observation of caries extending to pulp
Symptomatic irreversible pulpitis' EPT is WNL. (T/F)
True, only hyper-responsive (grossly exaggerated) + prolonged (>10 s) response to cold
- Spontaneous severe pain can occur
________________ is a prerequisite for reparative bridge formation.
Moderate inflammation, for tissue repair following pulp capping
Indirect pulp therapy has a better prognosis than direct. (T/F)
True (90% vs. 80%)
- Best prognosis overall: shallow pulpotomy and root canal (96%)
Components of indirect pulp caps
From most deep to shallow:
1. Demineralized (affected) dentin
2. Bactericidal liner (seals dentin) -> calcium hydroxide and RMGI sealing liner
3. Restorative material (placed 8-12 weeks later)
All of the following are contraindications for indirect pulp capping except:
A. Periradicular lesion
B. Pain lingers following thermal test, after return to mouth temperature
C. Pulpal response to tests is WNL or slightly exaggerated
D. Spontaneous pain
E. Percussion sensitivity
C
A mechanical exposure in what region would not be suitable for direct pulp capping?
Cervical level (class IV)
- Pulp coronal to exposure may have compromised blood supply
A vital pulp is not required for direct pulp capping. (T/F)
False, required and should be asymptomatic + WNL (same requirements as indirect)
- Exposure should also be small w/ minimal pulp trauma
What needs to be controlled prior to direct pulp capping procedure?
Bleeding (hemostasis using 3% sodium hypochlorite solution)
- If bleeding is not easily controlled, perform endo treatment instead
What is the coding for direct pulp capping?
3110 (3120 for indirect)
Factors that have a poor prognosis for pulp capping
- Large, lateral pulp exposure
- Prior symptoms of spontaneous, percussion, + heat
- Older patient
- Contamination
- Poor patient health
- Calcifications (decrease blood supply)
- Hyperocclusion
What is involved in caries diagnosis?
Determine caries activity by detection + patient factor
- Detection: extend of bacterial destruction
- Patient factors: salivary flow, social factors, diet, etc.
What instruments can be used for tactile caries detection?
Probe and blunt explorer
- Use gentle pressure
Caries progression through enamel is slow, and can take _________ (months/years)
6-8 years
Occlusion lesions are difficult to see radiographically. Why?
Superimposition of dense B and L cusps
- Can only see on a radiograph when lesion has passed the DEJ
Proximal lesions are better diagnosed radiographically or visual-tactile?
Radiographically, as difficult to perform visual tactile exploration
- Usually "kissing lesions" at/apical to the contact point
D1 lesions are indications for use of ortho bands. (T/F)
True, if no cavitation is present visually (need to perform tactile exam)
How does the DIAGNOdent work?
Infrared laser light -> fluoresce enamel -> determines extent of demineralization -> numeric score 0-99 (30+ = caries)
- Caries can also be heard (prior to visual detection)
- Tip must be rotated around vertical axis for proper reading
Caries increase tooth fluorescence. (T/F)
False, decrease due to increased scattering
The electrical conductance measurement shows how caries conduct electricity better than sound tooth structure. (T/F)
True, due to much lower electrical impedence
How does an inactive lesion appear with visual tactile examination?
- Enamel yellowish white, dentin brown-black
- Free from plaque, dry
- Smooth, shiny, hard surface
Enamel defects during matrix formation (_________ phase) is called:
Secretion phase, called hypoplasia (external defect on thinnest portion of affected enamel)
How can fluorosis be differentiated from caries?
Fluorosis has a symmetric distribution on homologous teeth (seen on multiple teeth)
What process does fluorosis interfere with?
Enamel mineralization, reducing the deposition of mineral and withdrawal of the organic matrix and water
- Hypomineralization (increased porosity) of subsurface layer
The brown lesions of molar-Incisor hypomineralization (MIH) are caused by:
High protein content
- Subject to enamel breakdown soon after eruption -> caries

What two factors are used to determine the ICDAS score?
Visual appearance and histological depth (after sectioning)
ICDAS scores
0. Sound enamel
1. White/brown, confined to fissure (80% outer enamel, 10% dentin)
2. White/brown, beyond fissure (no loss of surface integrity, 50% inner enamel and 50% into outer 1/3 of dentin)
3. Microcavitation of enamel (lesion depth 77% in dentin)
4. Shadow of dentin (intact walls and ridges) (lesion depth 88% into dentin)
5. Distinct cavitation w/ exposed dentin (less than 1/2 tooth structure, 100% in dentin)
6. Extensive cavitation (100% in dentin, reaching inner 1/3)
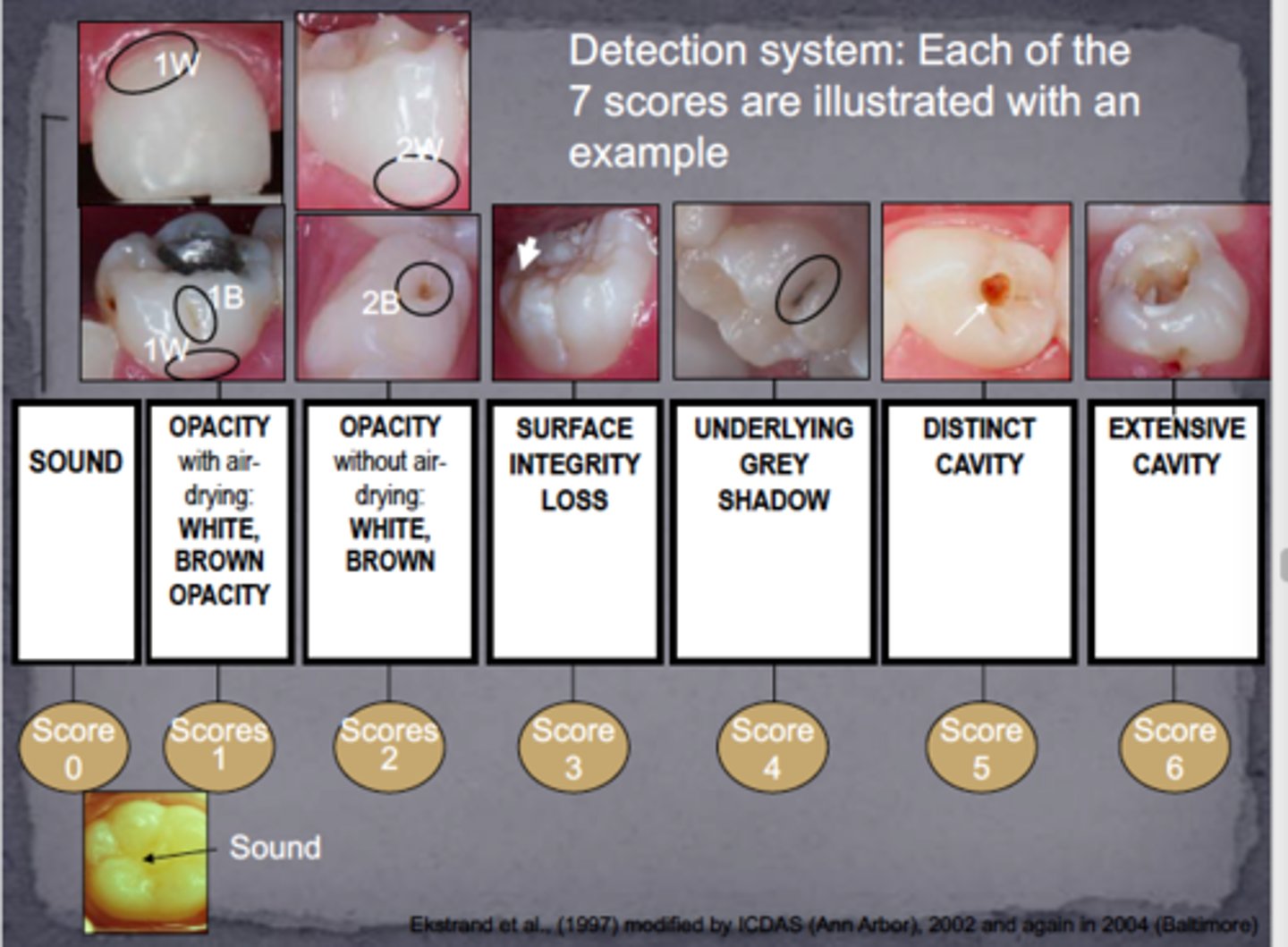
In the ICDAS system, obvious decay is seen at:
Codes 4-6
In ICDAS code ____, a caries biopsy should be carried out in medium and high risk patients if the DIAGNOdent reading is _____________.
Code 2, 20-30
Five or more caries lesions in the last 3 years is indicative of a high caries risk. (T/F)
False, 3 or more
- Xerostomia, suboptimal fluoride exposure (+ other factors that increase caries risk) -> high caries risk
What is the most powerful indicator of caries risk?
Past (fillings, etc.) and current (active) caries experiences
What is the resting and stimulated SFR for a high caries risk individual?
- Resting: <0.2 ml/min
- Stimulated: <0.7 ml/min
In a moderate caries risk patient, you would recall the patient every ________ months and perform bitewings every ______ months.
Recall every 3-6 months, perform bitewings ever 12-18 months
If the patient has one tooth missing due to caries, they are placed in the _________ risk category.
High
- Other factors include frequent meal exposures, mother had caries lesion in last 6 months, special health care needs (6-14 years old), radiation therapy, xerostomia
A high caries risk patient presents with caries that have not progressed into the dentin. What is the appropriate treatment?
Seal (E1) or seal + PRR (E2)
The mechanism of action of fluoride is dependent on the ______________ of oral fluids.
Ion availability (in both saliva and biofilm fluid)
Prescription fluoride toothpaste (1.1% NaF) is contraindicated for:
Children under 6, pregnant + nursing mothers, elderly with renal impairment
Fluoride varnish (5% NaCl) is useful for:
Remineralization of non-cavitated lesions
Fluoride and chlorhexidine should be used simultaneously to reduce caries risk. (T/F)
False, cancel each other out
- Wait at least 1 hour after chlorhexidine (chemical antiseptic) use to use fluoride
To be effective, xylitol dosage should be __________ daily.
6-10 grams
- After 2 years, all plaque bacteria removed from all oral surfaces + teeth are hard, shiny, and white
Arginine increases caries development. (T/F)
False, present in saliva (50 uM) -> converted to ammonia (base to counteract acidic foods) via ADS -> caries-free mouth
Abfraction
Cervical loss of tooth structure due to flexural forces (non-carious)
- Fracture of enamel rods on facial
Abrasion lesions present as:
Smooth, U/V-shaped concave lesion on facial root surface
Abrasion alone is not damaging to teeth, it is the combination of it with acids. (T/F)
True
- Toothpaste + acid -> loss of 1 mm of enamel in 2 years
Extrinsic causes of erosion appear on the ___________ surfaces.
Occlusal and labial
Intrinsic causes of erosion appear on the __________ surfaces of maxillary teeth and the ___________ surface on mandibular teeth.
Occlusal and lingual of maxillary and facial of mandibular
Why do NCCL occur in the cervical region?
Prismatic + brittle enamel and stress concentrates there
Theory of thermal shock
Thermal shock transferred from oral cavity through restorative material to the pulp
- Suggests thermal insulating base for amalgam (max 0.75 mm thickness)
Theory of pulpal hydrodynamics
Gap between prep + restorative material -> dentinal fluid flows through -> with cold, fluid contracts + flow increases -> generates action potential in nerves -> perceived by mechanoreceptors as pain
RBC should only be used for a class V restoration if there is perfect isolation and enamel is present. (T/F)
True, and if restoration is not complex
- Otherwise, use amalgam or RMGI
Amalgam preparations for class V restorations involve ___________ for improved retention.
Four-cove retention
- Use 1/4 round bur, depth of 0.25 mm
When should lesions be restored?
Cavitated, active, noncleansable, and not amenable by fluoride
Asymptomatic, non-cavitated D2 and D3 lesions should not be restored. (T/F)
False, can be restored, depending on patient's caries risk and consent