RESPIRATORY SYSTEM: LECTURE 17
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
43 Terms
Oxygen Transport in Blood:
Binds with haemoglobin
Dissolves in plasma (0.2ml/L at PO2 of 80mmHg)
Carrying Capacity of Blood for Oxygen:
200mls of oxygen per litre of blood
1g of Hb can transport 1.39mL oxygen when fully saturated.
Haemoglobin (Hb) Molecule:
Contains a & b polypeptide chain (globin) & 4 ferrous iron groups (haem) which binds 1 O2 molecule using a salt bridge in a co-operative fashion
allosteric: changes shape to expose haem binding sites
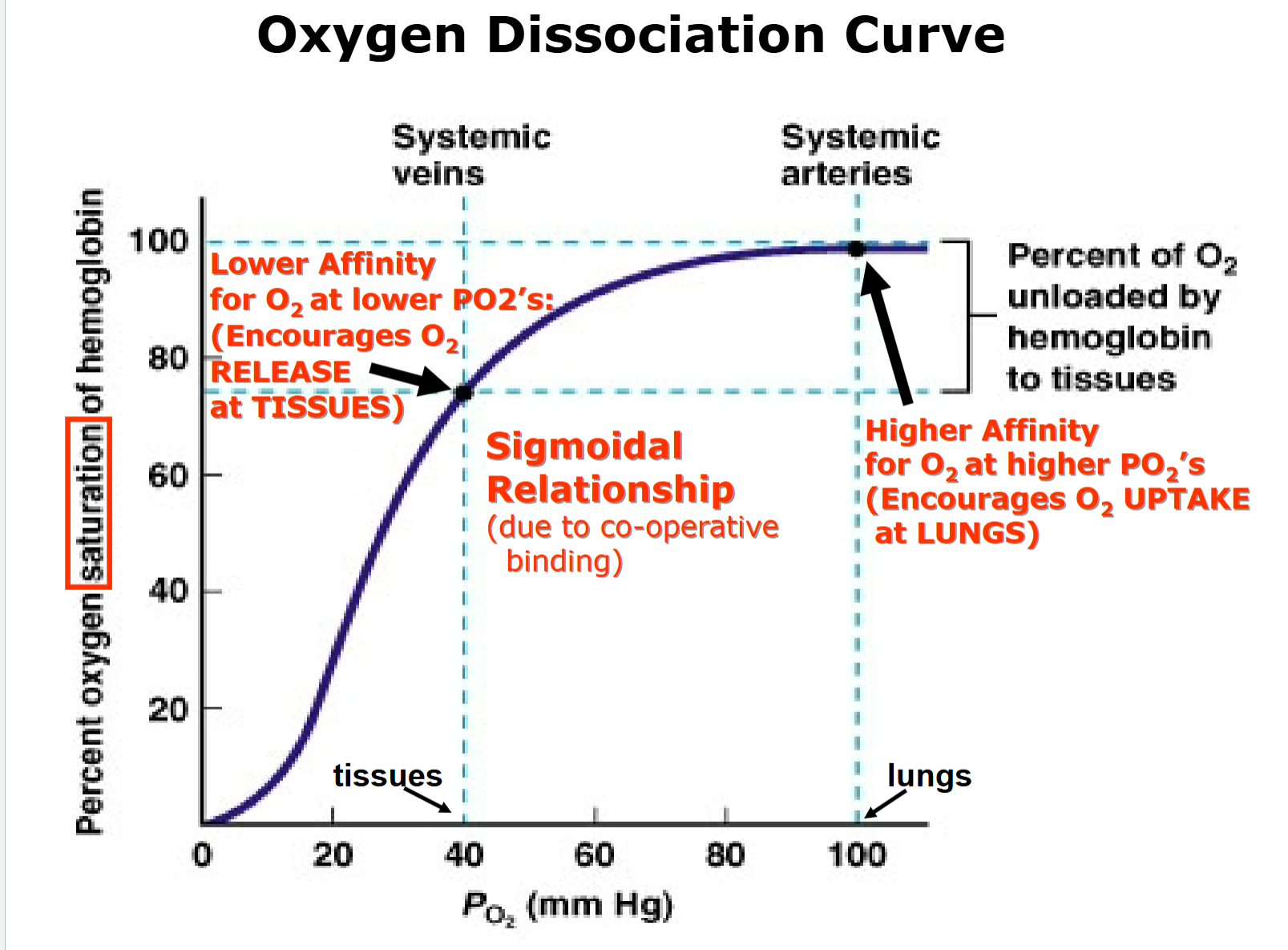
Oxygen Dissociation Curve:
Sigmoidal Relationship due to co-operative binding
Haemoglobin has greater affinity for oxygen at lungs than tissues.
Higher affinity for O2 at higher PO2’s, encourages O2 uptake at lungs
Lower affinity for O2 at lower PO2’s, encourages O2 release at tissues.
Partial Pressure of Oxygen (PO2)
160 mmHg reduced to 100 mmHg in alveoli.
Higher up = lower partial pressure (vice versa)
Why does Haemoglobin’s affinity for O2 decrease in tissue
Generation of H+
CO2 + H2O ⇌ H2CO3 ⇌ HCO3- + H+ (catalysed by carbonic anhydrase in RBC)
H+ binds to haemoglobin, losing its affinity for oxygen and giving up oxygen
Factors affecting Haemoglobin Affinity toward Oxygen:
At tissues → more CO2, [H+], temp, DPG → decreases O2 affinity (releases)
At lungs → less CO2, [H+], temp, DPG → increases O2 affinity (takes)
Diphosphate glycerine (DPG)
One product of aerobic metabolism & can also bind & displace oxygen from haemglobin.
Tissue & DPG
Metabolically active & generate diphosphate glycerine & heat
Bohr Shift:
For a given PO2, more O2 is given up
Lower affinity of Haemoglobin for O2.
Shifting Oxygen dissociation Curve:
Left = higher O2 affinity (vice versa)
Fetal Haemoglobin:
Has higher affinity for O2 than adult haemoglobin, helping move oxygen across placenta.
Myoglobin:
Very high affinity for oxygen
Oxygen store, found in heart & skeletal muscles.
Oxygen Saturation:
Proportion of haemoglobin bound in blood.
Oxygen Content:
Amount of oxygen in blood
Physiological Advantages of O2 dissociation curve.
Steep lower part of tissues, Haemoglobin releases lots of O2 for only a small drop in PO2.
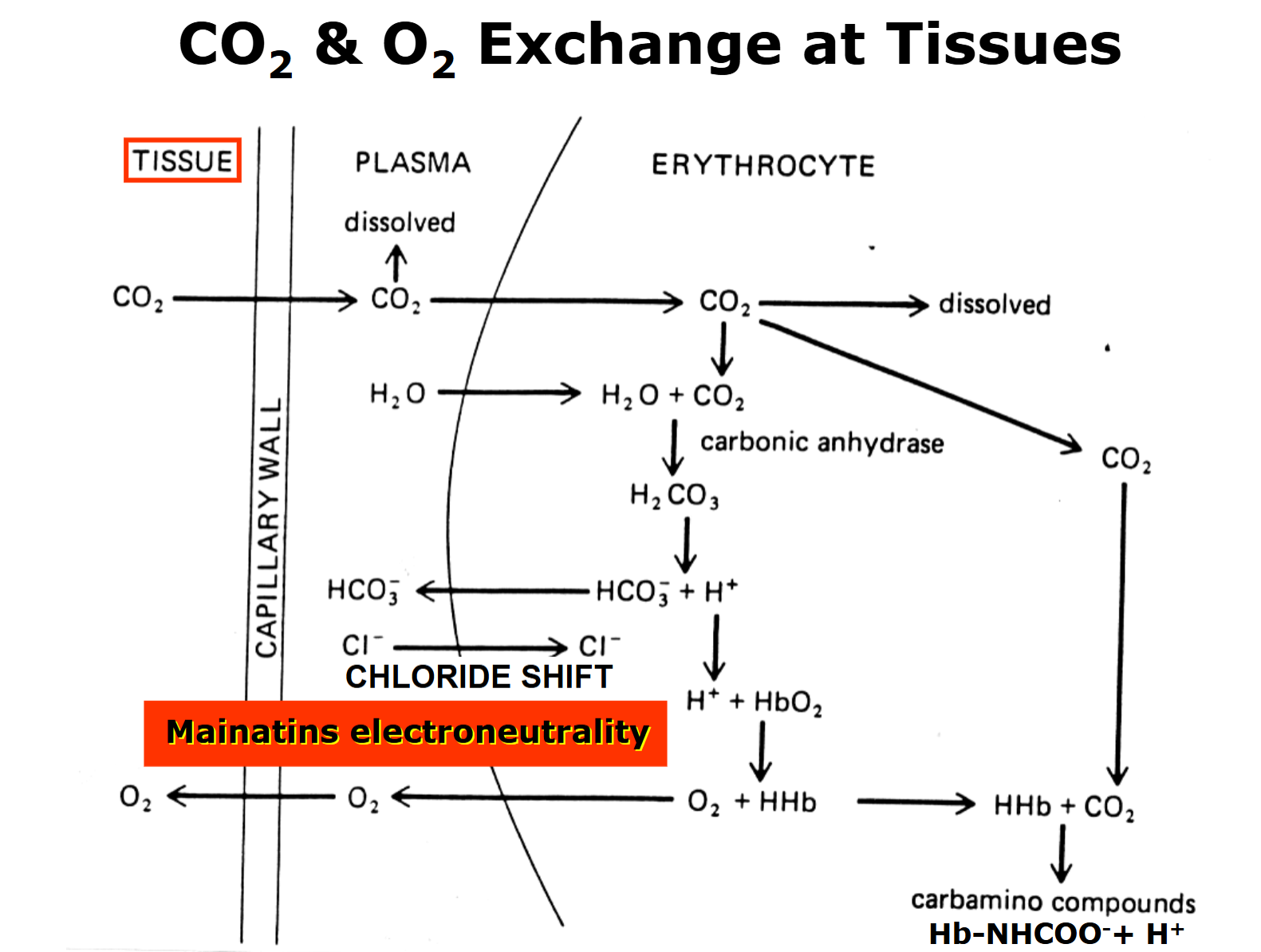
Carbon Dioxide Transport in Blood:
RBC: 30%
Plasma: 70%
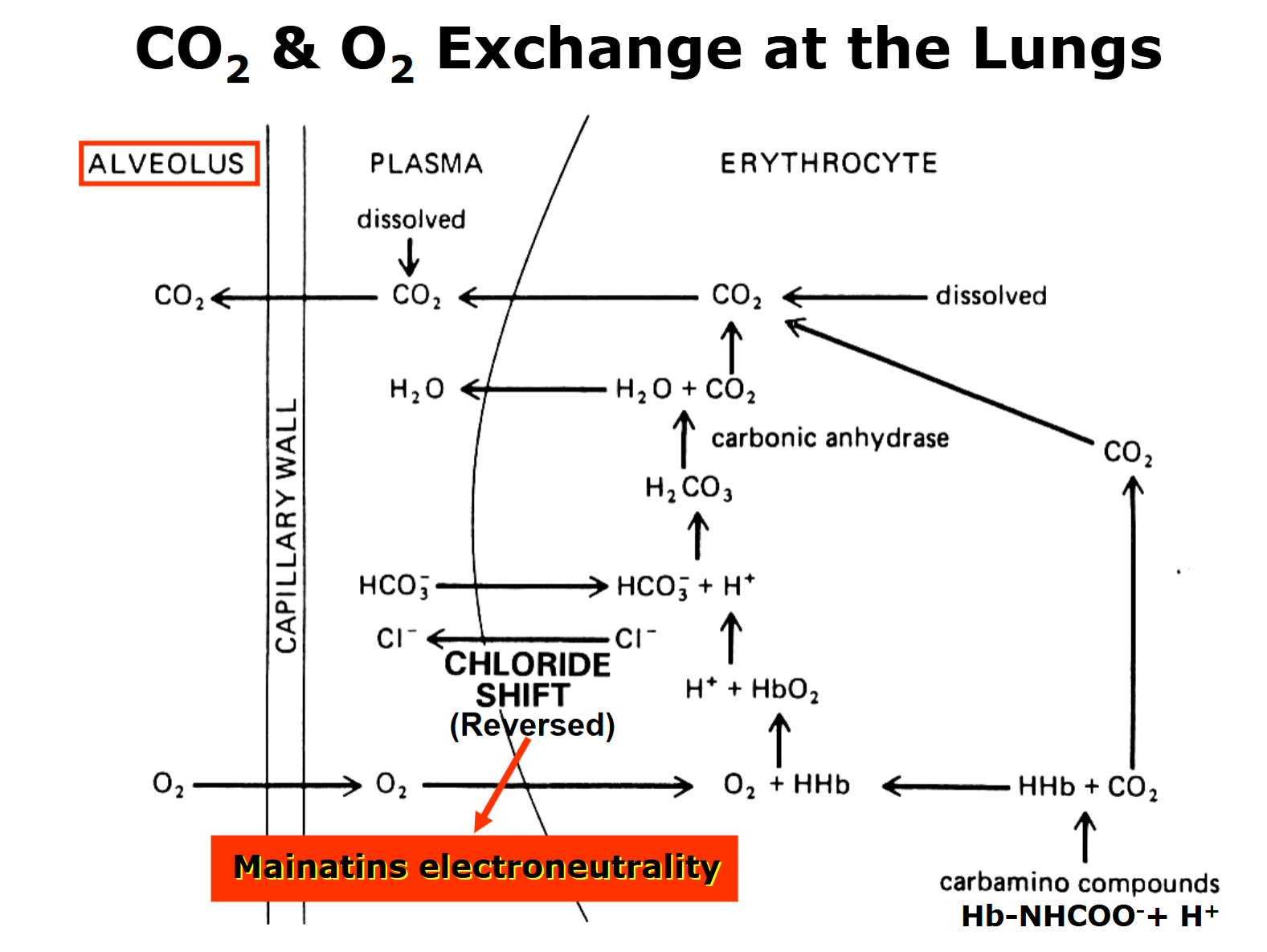
Majority of CO2 carried in plasma as HCO3-, rapidly formed in RBC in presence of carbonic anhydrase & diffused out into plasma.
In plasma
Dissolves in solution (CO2aq) [HCO3-]
Combines to amine groups (NH2)
Red Blood Cells:
Carried in HCO3- form (lots of CO2 → forward reaction, vice versa)
Carbon Dioxide Transport in Blood Notes:
Carbonic anhydrase speeds up reaction in RBCs
H+ buffered by haemoglobin, favouring forward reaction (mass equilibrium theory)
Chloride Shift:
In RBC, HCO3- exits cell down its conc gradient, allowing more HCO3- to form via mass equilibrium theory.
Entrance & exit of CL- ions maintains cellular electroneutrality.
CO2 & O2 exchange at the tissue:
Lower PO2 → H+ displaces O2 bound to Haemglobin → releases O2 into tissue
CO2 & O2 exchange at the lungs:
Higher PO2 → displaces H+ bound to Haemglobin
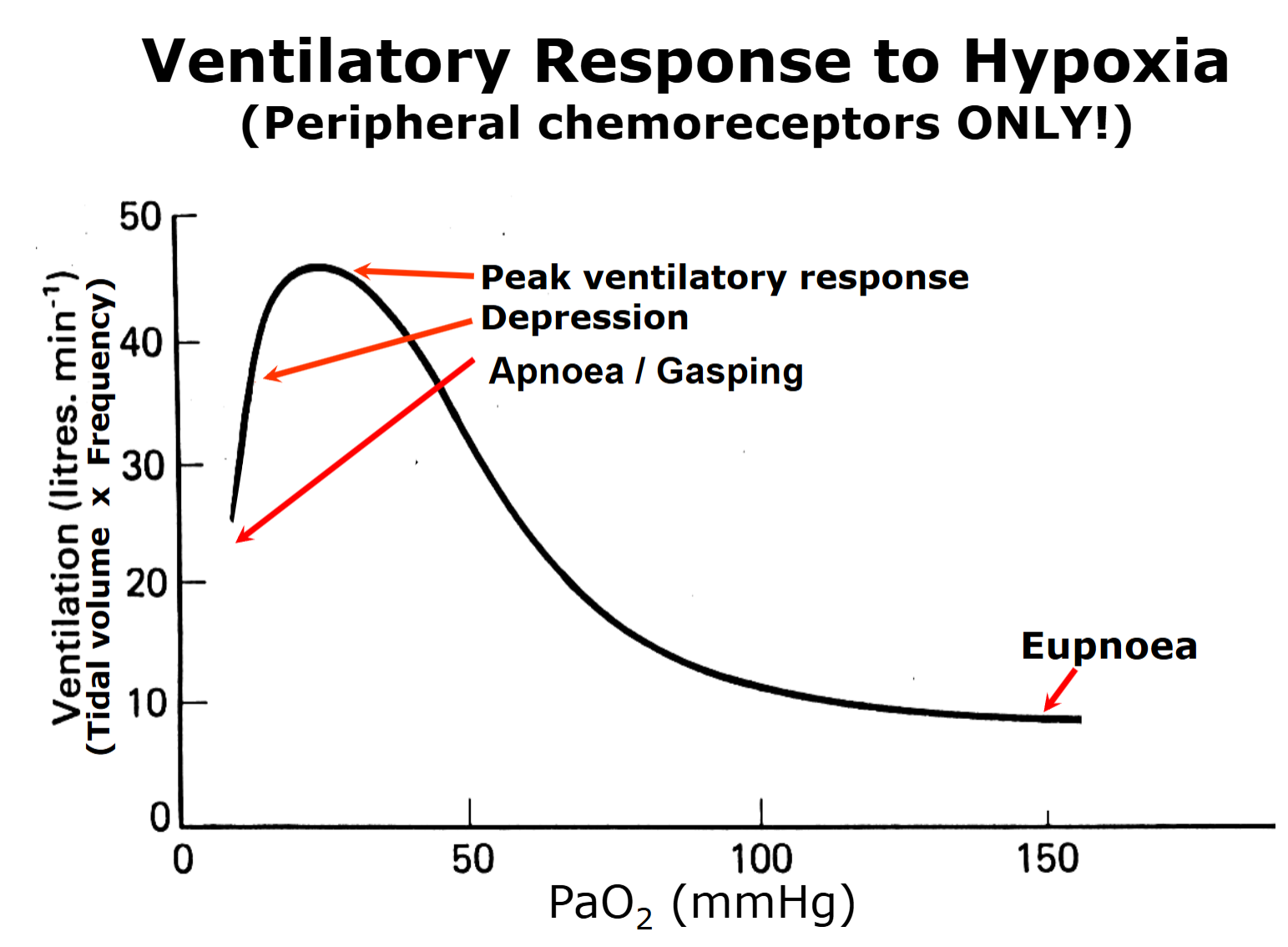
Eupnoea:
Normal breathing
Apnoea:
No breathing
Dyspnoea:
Sensation of breathlessness
Hypoxia
Low oxygen levels
Anoxia:
No oxygen
Asphyxia
Deprived of oxygen
Hypercapnia
High CO2
Hypocapnia:
Low CO2
Hyperventilate:
Excessive breathing
Hypoventilate
Shallow breathing
Ischaemia
Inadequate blood supply to tissues
Low O2 & high CO2
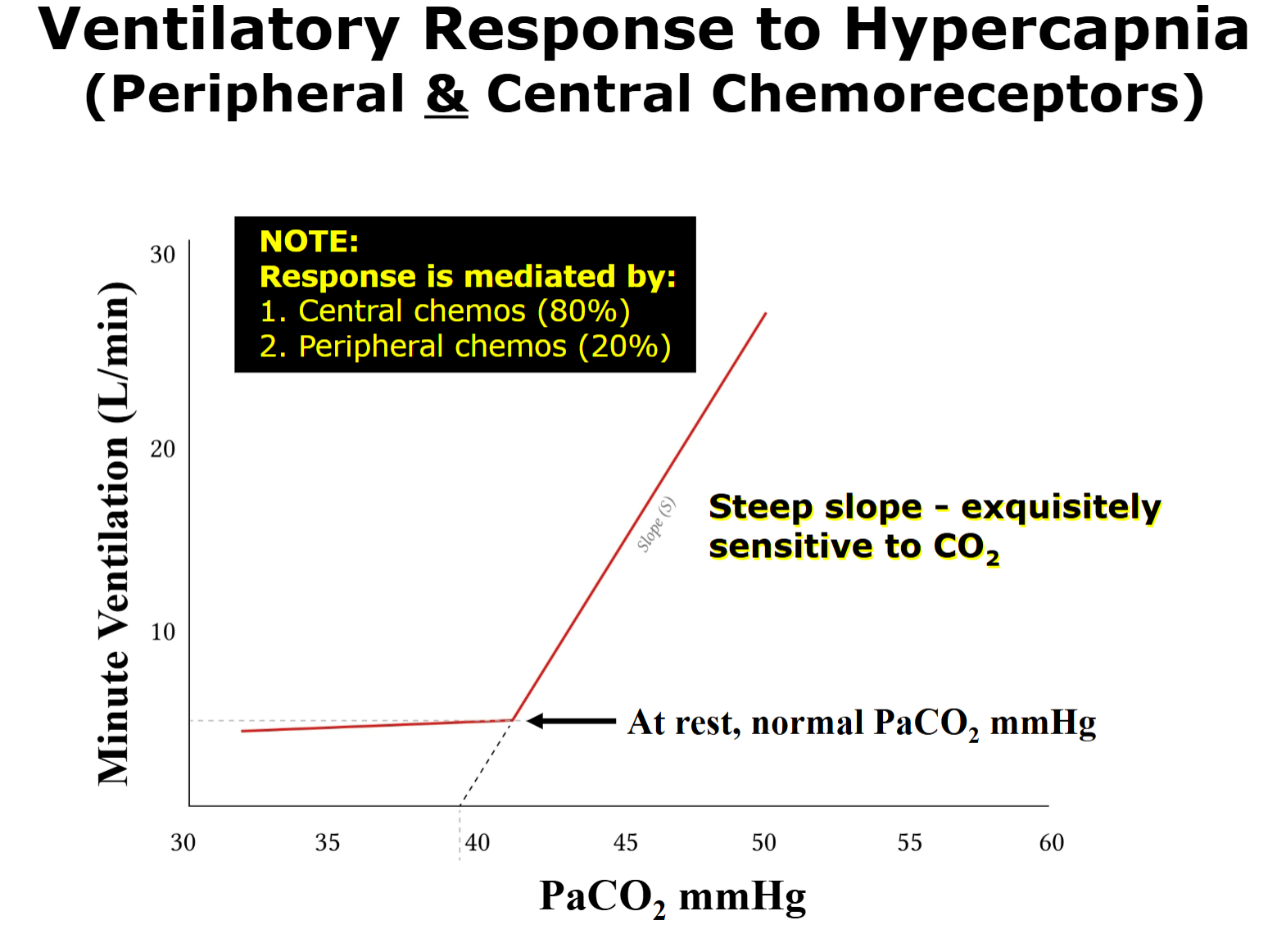
Chemical Control of Respiration
Control of ventilation by chemoreceptors (peripheral & central)
Peripheral Chemoreceptor: Location
Carotid artery bifurcation (carotide bodies) connected to carotid sinus nerve → medulla oblongata.
Peripheral Chemoreceptor:
Hypoxia (low PO2)
Hypercapnia (high PCO2)
Haemorrhage
Acidosis (decreased blood pH)
Increased sympathetic activity
Sodium cyanide (low dosage, mimics low O2 levels)
Fast response time
Gasping: Auto resuscitated mechanism
euponea → decreasing PO2 → oxygen remains not reinstated → gasping
Central Chemoreceptors:
Major chemical control of ventilation via CO2
Slow response time due to limited carbonic anhydrase → slow H+ production
Central Chemoreceptors: Location
Ventral surface of medulla oblongata
Central Chemoreceptors: Stimulants
Sensitive to H+ liberated when CO2 diffuses across blood brain barrier & dissolve in CSF (catalysed by carbonic anhydrase → H2CO3 → H+ + HC03-)
Reflex Response:
Increases minute ventilation by acting on brainstem respiratory network, an increase in PaCO2 above 42 mmHg → steep increase in minute ventilation mainly driven by central chemoreceptors.
80% central & 20% peripheral chemoreceptors
Ondine’s Curse/Congenital Hypoventilatory Syndrome:
Lack of central chemoreceptors → no breathing in sleep → possible death in sleep