🧬 Genetics: Mutations & Diagnostic Methods – Ultimate Flashcards (16)
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
15 Terms
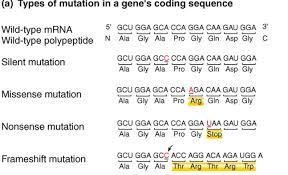
What are the four main types of small-scale DNA mutations?
Missense: One amino acid is changed for another.
Nonsense: A base change creates a premature STOP codon.
Splicing: Mutation at the exon-intron boundary affecting mRNA processing.
Frameshift: Insertion/deletion that shifts the "reading frame" of the entire gene.
Which mutation type is the most difficult to interpret clinically?
Missense mutations. It is hard to predict if changing one amino acid will actually "break" the protein or if it is just a harmless variation (VUS).
What is "Nonsense Mediated Decay" (NMD)?
A cellular surveillance mechanism that destroys mRNA containing a premature stop codon to prevent the production of toxic, truncated proteins.
In genetic nomenclature, what do "p." and "c." stand for?
p. (Protein level): e.g., p.Trp44Ter (Tryptophan at position 44 became a Stop).
c. (Coding DNA level): Describes the specific base change in the DNA sequence.
What is Familial Hypercholesterolaemia (FH) an example of?
A Heterogeneous disorder, meaning mutations in different genes (LDLR, ApoB, or PCSK9) can all cause the same clinical disease (high cholesterol).
What is a "Proband" and why are they tested first?
The Proband is the first affected family member to seek medical attention. We test them first to identify the "causative mutation" for the whole family.
When is Sanger Sequencing the "Gold Standard"?
For Targeted Testing: Confirming a mutation in a Proband or checking family members for a known mutation (Cascade Testing). It is very accurate for small regions (<900bp).
What is Next Generation Sequencing (NGS)?
Also called Massively Parallel Sequencing. It allows for the sequencing of millions of DNA fragments at once, making it fast for screening multiple genes at once.
What are the "cons" of NGS in a clinical lab?
Requires massive computing power (Bioinformatics) to analyze the data and a longer preparation time before the run starts.
How is a Polymerase Chain Reaction (PCR) used in diagnosis?
It is used to amplify (make millions of copies of) a specific region of DNA so there is enough material to be analyzed by Sanger sequencing or electrophoresis.
What samples are suitable for genetic testing?
Any sample with nucleated cells: Venous blood (most common), Newborn blood spots, Buccal swabs (cheek cells), or even Urine and CSF.
What is "Tiered Testing" in FH diagnosis?
A strategy where you test the most common gene first (LDLR); if negative, you move to ApoB, then PCSK9. (NGS panels are now replacing this).
What is the significance of a "Frameshift" mutation?
It usually results in a completely different amino acid sequence downstream and almost always leads to a premature STOP codon, causing a Loss of Function.
Why do we use Sanger sequencing to confirm NGS results?
Although NGS is fast, it can occasionally make errors. Sanger is used as a "second check" to ensure the mutation is real before telling a patient.
How does "Cascade Testing" work in families?
Once a mutation is found in the Proband, we use Targeted Sanger Sequencing to test all first-degree relatives. This allows for early treatment (e.g., Statins) before a heart attack occurs.