Introduction of Medical Imaging
1/11
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
12 Terms
What are the five Diagnostic Imaging techniques used and their function
Detect and diagnose diseases, determine disease severity
X-ray radiography
Computed tomography (CT)
Magnetic resonance imaging (MRI)
Ultrasound (US)
Nuclear medicine
What are the three Therapeutic imaging techniques used and their function
Guide procedures such as surgery or radiation therapy
Fluoroscopy
Angiography
Interventional radiology
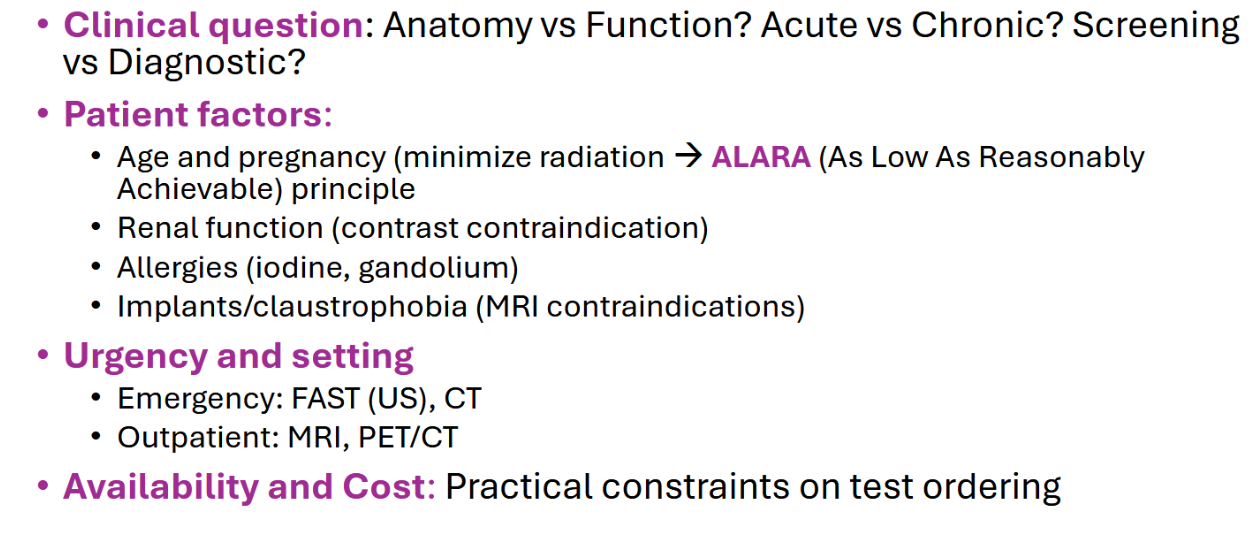
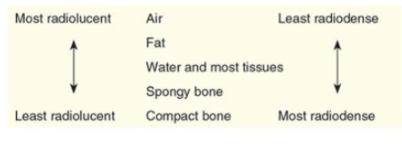
General concept, Key concepts, Clinical Strengths, Limitations of X rays
Principle: Uses external X-rays that are differently absorbed (attenuated) by tissues.
X-ray: Single burst of X-rays creates a 2D shadowgram
Key concepts:
Radiodensity (Air<Fat<Water/Soft tissue<Bone<Metal)
Superimposition of structures
Contrast agents (Barium, Iodinated)
Clinical strengths (High-yield uses)
Skeletal: Fractures, dislocations, arthritis
Chest (CXR): Pneumonia, pneumothorax, heart failure, lung masses
Abdomen (KUB): bowel obstruction, free air (perforation)
Screening: Mammography
Limitations: Poor soft tissue detail, radiation dose (low), 2D view
What do we use contrast materials for? Examples of procedure used? Examples of compounds used?
Used to enhance plain radiography:
Angiography, urography, upper and lower GI studies
We use Barium or Iodine containing compounds
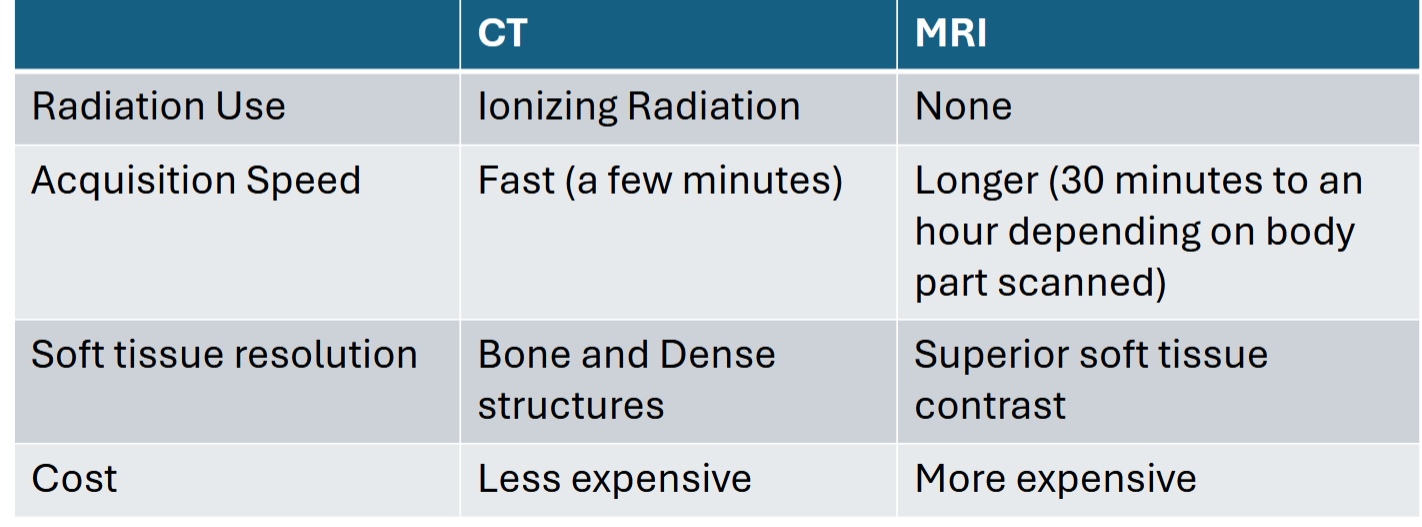
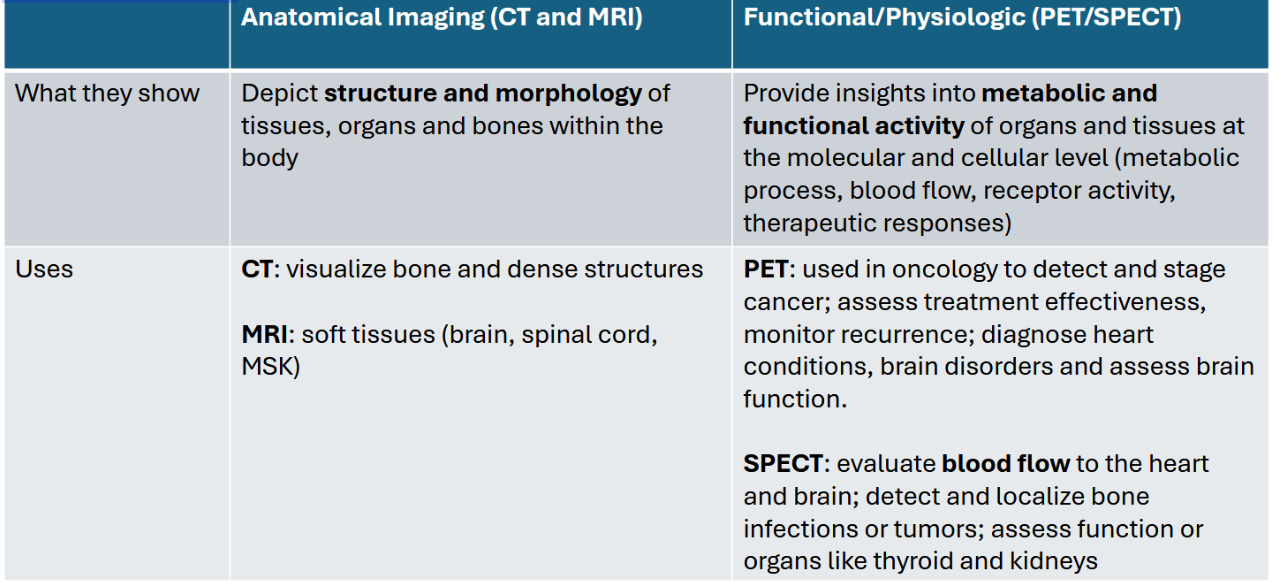
General concept, Key concepts, Clinical Strengths, Limitations of Computed Tomography (CT)
Rotating X-ray gantry and detectors create cross-sectional “slices”, computer reconstructs 3D data
Key Concepts:
Hounsfield Units (HU) for quantitative density
Use multi-slice detector which can acquire multiple images
IV contrast (Iodinated): Assesses vascularity, organ perfusion, inflammation
CT Angiography (CTS) and Venography (CTV)
Clinical strengths (The “Workhorse”)
Emergency/Trauma: Head injury, internal hemorrhage, aortic dissection
Oncology: Cancer staging, detecting metastases, treatment response
Vascular: Pulmonary embolism (PE), aneurysm, stroke evaluation
Abdomen/Pelvis: Appendicitis, diverticulitis, kidney stones, pancreatitis
Limitations: Significant radiation dose, risks of IV contrast (nephropathy, allergy), metal artifacts
General concept, Key concepts, Clinical Strengths, Limitations of Imaging with Sound waves
Principle: Non-ionizing; uses high frequency sound waves and their echoes to create images
Transducer sends/receives sound waves; image is generated in real-time
Key concepts:
Echogenicity (hyperechoic, hypoechoic, anechoic)
Acoustic shadowing (e.g. by gallstones) and enhancement
Doppler: Assesses presence, direction and velocity of blood flow
Clinical strengths (Safe and Dynamic):
Obstetrics/Gynecology: fetal assessment, ovarian/uterine pathology
Cardiology: echocardiography (cardiac structure and function)
Abdomen: Gallbladder, liver, kidneys, aorta
Vascular: Deep vein thrombosis (DVT), Carotid Stenosis
Point-of-care (POCUS): FAST exam (trauma), guiding procedures (central lines, biopsies)
Limitations: Highly operator-dependent, limited by bone and gas, poor penetration in obese patients
What are the advantages of Ultrasounds? Which frequencies do we use?
Advantages:
portable
real-time
no ionizing radiation
fetal imaging
inexpensive
Produces images via backscattering of mechanical energy from boundaries between tissues
Frequency: typically 1 to 10 MHz
Use lower frequencies for deep-lying structures
Higher frequencies for superficial structures
General concept, Key concepts, Clinical Strengths, Limitations of Imaging with MRIs
Principle: Non-ionizing; uses a powerful magnet and radio waves to
manipulate body protons to generate images
Protons align in magnetic field radiofrequency pulse knocks them out of alignment → signal is emitted as they relax → computer creates detailed image
Key concepts:
T1 vs T2 weighting: The fundamental contrast mechanisms (T1: fat is bright; T2: water/pathology is bright)
Gadolinium (IV contrast): shortens T1, highlights vascularity, inflammation
Functional MRI (fMRI): measures brain activity via blood flow changes
Clinical strengths (The Soft Tissue Specialist):
Neurology: Brain tumors, stroke, spinal cord injury, multiple sclerosis
Musculoskeletal (MSK): ligament/ tendon tears, cartilage, joint pathology
Abdomen/Pelvis: Liver/biliary characterization, female pelvic pathology
Limitations: Slow, expensive, contraindications (pacemakers, certain metal implants), claustrophobia, noise, NSF risk with gadolinium
General concept, Key concepts, Clinical Strengths, Limitations of Imaging with Nuclear Medicine (Planar scintigraphy, SPECT, PET)
Principle:
Patient is given a radioactive tracer, a detector captures radiation emitted from the body to show physiological processes
Radiopharmaceutical is designed to accumulate in a target organ or tissue based on its metabolic activity
Over time the radioactive isotope will decay, emitting gamma radiation, which is then detected with a gamma camera increased uptake in areas with increased metabolic activity
SPECT: Single photon emission computed tomography (3D view)
PET: Positron emission tomography (higher resolution, quantitative)
Hybrid imaging (PET/CT, SPECT/CT): fuses
Functional data with anatomical CT data for precise localization
Clinical strengths (The "How is it working " scan)
Oncology (PET/CT): The standard for cancer staging, restaging and assessing treatment response
Cardiology (SPECT): Myocardial perfusion scans (stress tests)
Endocrinology: Thyroid scan, parathyroid scan
Skeletal: Bone scan for metastases, infection, osteomyelitis
Neurology (PET): Dementia evaluation (e.g. Alzheimer’s vs FTD)
Limitations: High radiation dose (internal) low spatial resolution, expensive, limited availability
Compare and contrast CT and MRI
Discuss the use of Anatomical information (CT, MRI) VS
Functional/Physiological information (PET, SPECT)
What are some factors in choosing the right test