Sepsis and shock
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
77 Terms
What is shock
tissue perfusion is inadequate to deliver oxygen and nutrients to support cellular function
three physiologic responses that are common to all types of shock
Hypoperfusion of tissues
Hypermetabolism
Activation of the inflammatory response
Hypovolemic shock
Loss of plasma or blood volume of at least 15% to 30%.
What can lead to hypovolemic shock?
Excessive fluid loss from diuresis, vomiting, or diarrhea;
Blood loss secondary to surgery, trauma, childbirth, burns, and diabetic ketoacidosis.
Older adult clients are more prone to dehydration
Cardiogenic shock
Cardiac pump failure due to a direct cardiac cause
What can lead to cardiogenic shock
MI, heart failure, cardiomyopathy, dysrhythmias
Older adult clients are at increased risk for MI and cardiomyopathy.
Obstructive shock
Cardiac pump failure due to an indirect cardiac factor
What can lead to obstructive shock
blockage of great vessels, pulmonary artery stenosis, pulmonary embolism, cardiac tamponade, tension pneumothorax, and aortic dissection.
Septic shock
Toxins and bacteria causing an inflammatory response and subsequent massive vasodilation
Neurogenic shock
Head trauma, spinal cord injury, and epidural anesthesia are among the causes.
Distributive shock
vasodilation
3 types of distributive shock
Septic: resulting from acute infection causing relative vasodilation
Neurogenic: resulting from loss of sympathetic tone causing relative vasodilation
Anaphylactic: resulting from severe allergic reaction producing acute systemic vasodilation
4 stages of shock
Initial (early) ***
Compensatory
Progressive
Irreversible (Refractory)
Initial stage of shock (what is it and what are some s/s)
Decrease in MAP, but BP remains normal
Small increase in HR. Otherwise little to no symptoms
Compensatory stage of shock (what is it and what are some s/s)
Lower BP but still WNL, Increased HR to compensate and increase cardiac output to restore tissue perfusion and oxygenation.
High RR d/t acidosis. May cause compensatory respirtroy alkalosis
Cold/clammy skin r/t blood shunting to vital organs. Leads to UO decreasing
PTs can start to get confused/agitated
SNS causes vasoconstriction, increased HR, increased heart contractility to maintain BP, CO
Perfusion of tissues is inadequate
Acidosis occurs from anaerobic metabolism
Confusion, agitation may occur
Progressive stage of shock (what is it and what are some s/s)
Compensatory mechanisms begin to fail. Severely hypotensive, decreased MAP
Rapid RR, crackles, hypoxia, Severely tachycardic, Decreased LOC, decreased UO
HR still high but BP and MAP decrease
All organs suffer from hypoperfusion (due to poor CO!)
Lungs begin to fail, alveoli collapse, pulmonary edema occurs
Inadequate perfusion of heart leads to dysrhythmias, ischemia
As MAP falls below 70, GFR cannot be maintained
Acute kidney injury may occur
Disseminated intravascular coagulation (DIC) may occur as cause or complication of shock
Metabolic acidosis from lactic acid build up
Hypotension SBP <90, MAP <65 = NOT GOOD PERFUSION
Skin starts to mottle
Pt now lethargic
Irreversible stage of shock (what is it and what are some s/s)
Organ damage so severe that the patient does not respond to treatment and cannot survive.
BP unresponsive to measures to increase
Renal, liver failure
Anaerobic metabolism worsens acidosis
Multiple organ dysfunction progresses to complete organ failure
Pt needs intubation
unresponsive to vasopressors and fluids
Skin is jaundiced r/t liver failure
No urine output r/t kidney failure
Pt unconscious
procalcitonin and CRP are
inflammatory markers
ABG lab results for someone in shock
acidosis
serum lactic acid lab results for someone in shock
Increases due to anaerobic metabolism
prolactin lab results for someone in shock
elevated
CRP lab results for someone in shock
elevated
serum glucose lab results for someone in shock
elevated
electrolytes lab results for someone in shock
elevated
cardiac enzymes (Creatine phosphokinase, troponin, etc) lab results for someone in shock
increased
Hgb and Hct lab results for someone in shock
Decreased with hemorrhage, increased with dehydration
what cultures should you collect from a pt in shock
blood, urine, wound
what are some diagnostics you should run for a pt in shock
hemodynamic monitoring
EKG
echo
CT
CXR
EGD/colonoscopy
general shock management strategies
Fluid replacement to restore intravascular volume
Vasoactive medications to restore vasomotor tone, improve cardiac function
Nutritional support to address metabolic requirements (not immediate)
nursing interventions for pt in shock
monitor VS frequently
keep pt warm
I&O’s
O2 therapy
shock position
frequent VS
telemetry monitoring
LOC
cap refil
call rapid response if signs of worsening
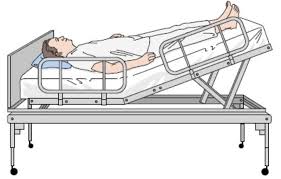
what is the shock position
The shock position (passive leg raise) flat on their back while their legs are passively raised to a 45 degree angle. Purpose = elevate the legs so that blood can flow from the lower body to the heart.
crystalloids used for fluid replacement
Normal saline- usually start with this and then for large volumes switch to LR. can cause hypernatremia
LR- better for large volume
colloids used in fluid replacement
albumin- keep fluid in vasculature
dextran- may interfere with platelet aggregation
complications of fluid replacement
respiratory issues, electrolyte disturbances, hypothermia, FVO, pulmonary edema
what should you do before administering fluids
warm the fluids to avoid hypothermia
when would you give vasoactive medications instead of fluids?
when Fluid may be contraindicated – such as in acute HF, decompensated HF, and chronic kidney failure. and use vasoactive meds if non responsive to other methods (fluid therapy or leg raise dont do anything)
intropic agents pros and cons
Improve contractility, increase stroke volume (volume ejected), increase cardiac output
Disadvantages 🡪 Increase oxygen demand of the heart, high risk for arrythmia
intropic agents examples
dobutamine, dopamine, epinephrine, milrinone
vasodilators pros and cons
Reduce preload and afterload, reduce oxygen demand of heart
Disadvantages 🡪 Cause hypotension
vasodilators examples
nitroglycerine, nitroprusside, nicardipine, labetalol
which two meds are BEST for cardiogenic shock/decompensated HF
Dobutamine and Milrinone = Great for cardiogenic shock/decompensated HF because they are INODILATORS
vasopressors pros and cons
Increase blood pressure by vasoconstriction, increase afterload
Disadvantages 🡪 Increase afterload, thereby increasing cardiac workload; compromise perfusion to fingers, toes, skin, kidneys, lungs, gastrointestinal tract, can cause arrythmias
vasporessros shunt blood to core so make sure to monitor distal extremities. check cap refil.
vasopressors examples
norepinephrine, dopamine, phenylephrine, vasopressin, epinephrine
arterial line care
used to monitor MAP
can be used for ABG and lab draws
inserted by trained MD
NO IV MEDICATIONS through this line.Tubing is usually streaked Red on the outside.
IMC/ICU care required
Goal MAP
Goal MAP Above 65 for pressors
Goal MAP Below 100 or 80 for conditions such as post op CABG, Aortic Dissection/Repair, Stroke
normal CO
4-8 L/min
hallmark signs of cardiogenic/obstructive shock
Hallmark signs = Increased preload (CVP, PA, Wedge), Increased Afterload (SVR), Decreased Contractility
Cold and Clammy – can also be hypotensive! (Good example of how BP does not always equal blood volume)
what is Pulmonary artery Catheter used for
Continuous monitoring of Preload (CVP, PA pressures, Can obtain Wedge pressure)
Can measure cardiac output in multiple ways , check invasive blood temperature monitoring
need CXR to confirm placement that the distal PA is in the right or left pulmonary artery
can draw mixed venous oxygen saturation (SVO2)
RN CAN NOT Reposition this catheter or Wedge
Mixed Venous Oxygen Saturation – SVO2 – Why Is this helpful? Where would we draw this from and why?
Indicator of oxygen delivery and oxygen consumption – helps differentiate cardiogenic from septic shock and to see improvements if therapy is working!
draw from pulmonary artery catheter
intra aortic balloon pump (IABP)
Helps with coronary perfusion, reduces afterload. Risks include improper timing of balloon inflation and deflation, BEDREST if in femoral artery (can also be axillary) Helps pre-CABG, Pre-Heart transplant .
impella (percutaneous LVAD)
Guarantees a set amount of CO to assist the native heart. Offloads the LV. Helps assist in cath procedures, post MI, C shock, and Pre-transplant. Risk for bleeding, hemolysis, BEDREST if femoral artery. Can be axillary.
LVAD (left ventricular asssit device)
Durable – can go home with this. Connected to drive line, power cables. Can not swim. Must have batteries charged if traveling. Risks include driveline infections, risk of bleeding, risk of clots/stroke. CAN NOT TURN OFF – FATAL. Surgically sewn into LV and Aorta. CPR precautions – Avoid CPR when able – can dislodge LVAD
ECMO (Extracorporeal Membranous Oxygenation)
bypass machine to allow for out of body oxygenation and circulation. Mechanical circulatory support. Greatest amount of support – high mortality.
s/s of neurogenic shock
Evidenced by signs of parasympathetic stimulation
Hypotension
Bradycardia
Temperature dysregulation
neurogenic shock treatment
stabilize spinal cord injury
discontinue spinal anesthesia
prevention- proper positioning with spinal/epidural
vasporessors, atropine, inotropic agents
s/s of anaphylactic shock
Acute onset of symptoms
Presence of 2 or more symptoms - respiratory and/or cardiac compromise, reduced BP, GI distress, and skin or mucosal tissue irritation
headache, lightheadedness, nausea, vomiting, acute abdominal pain, feeling of impending doom.
anaphylactic shock treatment
vasopressors
histamine blockers
bronchodilators
corticosteroids
MULTIPLE ORGAN DYSFUNCTION SYNDROME (MODS)
Presence of altered function of two or more organs in an acutely ill patient such that interventions are necessary to support continued organ function
Shock untreated = MODS
treatment/management of MODS
dialysis
surgery for obstructions
intubation
ECMO
Promoting adequate organ perfusion
Providing nutritional support
nutritional therapy should also administer what to increase survival rates
Glutamine increases survival rates -> restores cell energy that is lost during shock
H2 blockers prevent excess acid production during times of stress
what is sepsis?
Life-threatening organ dysfunction caused by a dysregulated host response to infection
what are some things that can increase risk for sepsis
surgery, central lines, catheters, double rooms, intubation, immunosuppression, prosthetic materials (ex valves and joints), chemo
SYSTEMIC INFLAMMATORY RESPONSE SYNDROME (SIRS) criteria
you have two or more of the following:
Temperature of 101F OR less than 96.8F
Heart rate >90/min
RR of 20 or PaCO2<32
WBC count >12 or <4, or >10% bands
sepsis criteria
SIRS plus evidence of infection (known or suspected)
Lactic > 2
severe sepsis criteria
SEPSIS PLUS ORGAN DYSFUNCTION, HYPOTENSION, OR HYPOPERFUSION
(LACTIC ACID >4
SBP <90 OR MAP <65
DECREASED URINE OUTPUT)
septic shock criteria
HYPOTENSION (DESPITE FLUID RESUSCITATION) PLUS HYPOPERFUSION ABNORMALITIES
major difference between severe sepsis and septic shock
if you tried and intervention and it did not work it is shocxk
why measure lactate?
Marker of hypoperfusion and ischemia = inadequate oxygen delivery
normal lactate level
Normal level: 0.5-1
lactate level where you should suspect sepsis
lactate greater than 2
lactate level in severe sepsis
lactate greater than 4
how often do you need to check lactate?
Half life is 20 minutes. Check serially to assess response to intervention. at least every 4hrs
progression of sepsis
body over responding to bacteria in sepsis. inflammtory response activates clotting cascade
causes widespread systemic response and low perfusion causing tissue injury
common to see DIC with severe sepsis
Primary bacteremia =
unknown source of infection
bacteremia means bacteria in bloodstream
bacteremia does not always equal sepsis
sepsis bundle
1) Measure lactate level*
2) Obtain blood cultures prior to administration of antibiotics
3) Administer broad spectrum antibiotics
4) Begin rapid administration of 30 ml/kg crystalloid for hypotension or lactate ≥4mmol/L
5) Apply vasopressors if hypotensive during or after fluid resuscitation to maintain a MAP >65
*Remeasure lactate if initial lactate elevated (>2)
MANAGEMENT OF THE PATIENT WITH SEPSIS
Monitor access sites, monitor MAP, monitor BP, VS at least Q2H x 6 hrs and after every fluid bolus, call provider if urine output less than 0.5 ml/kg/hr, strict I and O, fluid challenges as specified, initiation of antibiotics, trend lactic acid level, neuro checks, telemetry monitoring,
lactate clearance that can assess response to fluid resuscitation
Lactate clearance of at least 10% at a minimum of 2 hours after resuscitation initiation is a valid way to assess initial response to resuscitation in severe sepsis.