SSS Week 6
1/16
Earn XP
Description and Tags
Dermatological Emergencies
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
Steven Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TENS) Presentation, characteristics, complications, management
Presentation
1-3 days of prodromal sore throat, fever malaise and conjunctivitis
followed by skin blistering and skin loss in sheets leaving painful raw areas
characteristics
characterised by necrosis and detachment of epidermis
erosions of mucosal surfaces including conjunctiva, oropharynx, oesophagus, urethra and vagina
SJS tends to be on the trunk and face but TENS is generalised (TENS can have multi-organ failure)
almost always drug related (antibiotics, anticonvulsants etc) and there are also HLA associations in some races to anticonvulsants and allopurinol
common agents
Co-trimazole
Lamotrigine
carbamazepine
phenytoin
allopurinol
piroxicam and meloxicam (NSAID)
Systemic involvement
hepatitis
pancytopenia
DIC
acute resp distress syndrome
GIT bleeding
sepsis
Complications
Severe ocular complications, pigment alteration, sicca syndrome,
scarring to mucosal surfaces and vagina and esophageal stricture
Management
Cease all suspected drugs
ICU / burns unit
Erythema Multiforme characteristics, aetiology, diagnosis, management
Characterised by classic targetoid lesions, raised, round papule with a darker, blistered centre surrounded by a pale oedematous ring with a red edge in crops DOES NOT MIGRATE (Unless urticaria which is Ddx)

affects only skin and mucous membranes
most common cause is HSV infection
TWO TYPES: EM minor, EM major
EM minor: usually result of HSV and occasionally drugs
EM major: usually HSV and Mycoplasma pneumonia
EM minor is limited to the skin and mainly on the extremities whereas major is where mucosal membranes are also affected, and large areas of skin are involved
Dx : skin biopsy with histology
Management
treat underlying cause
symptomatic relief
EM major can cause significant morbidity but not life threatening, usually lasts 2 weeks
DRESS (drug reaction with eosinophilia and systemic symptoms) what is it, what drugs, management
DRESS is a severe, potentially fatal, drug hypersensitivity reaction characterized by a high fever, malaise, facial oedema and generalised morbilliform rash which can progress to erythroderma, eosinophilia (high eosinophil counts), and can have additional symptoms such as (lymphadenopathy, hepatitis, nephritis, pneumonitis, myocarditis) that typically develops 2–6 weeks after starting a new medication
What drugs are involved
anticonvulsants
antibiotics including minocycline
allopurinol
terbinafine
antiretrovirals
azathioprine
dapsone
Management
oral steroids
Type I anaphylactic reactions (aetiology, ddx, management)
Anaphylaxis, urticaria, angioedema
Urticaria
classical lesion is a wheal which indicates dermal oedema (erythematous raised lesion, annular or polycyclic or targetoid)
due to histamine release
does not involve the epidermis so no scale, blistering or disruption of skin, only involves dermis
in very young children, urticaria may appear purple and may be followed by bruising cus of vessel fragility
Aetiology
food allergens
insect toxins
inhaled substances
medications
ACE Inhibitors
blood products
IV contrast
viral infectiosn, occasionally worms
physical urticaria can also be induced from cold, sweating, water, vibration and pressure, scratching skin (dermographism - a common form of physical urticaria, occurs when skin is stroked or scratched)
Ddx (urticaria is the only one that migrates)
erythema nodosum
cellulitis
drug reactions
Management of acute vs chronic urticaria
Acute
withdraw the cause if found
antihistamines (H1) less sedating (loratadine) vs sedating (promethazine)
if response to antihistamines 1 is poor then use a H2 histamine eg. ranitidine
NO STEROIDS cus its pureply histamine reaction
Chronic >6-12 weeks
specific cause unlikely to be found
investigations TFT, RAST, FBC, hepatitis serology, analogous serum skin testing,
treatment includes trial elimination diet
avoid NSAIDs and aspirin
antihistamines and if that fails immunosuppressants (regular IV injections)
Angioedema
involves deeper tissues compared to urticaria, presents with areas of skin coloured swelling (usually face, eyelids, hands and feet) and can obstruct airway
Anaphylaxis
Anaphylaxis is a life-threatening emergency caused by massive release of histamine
first sign is often dizziness and skin itching and burning
may have wheezing, feelings of panic and anxiety, and gi involvement (vomiting and abdo pain)
frequently an urticarial rash, and angioedema of face, neck and airway
patients may progress rapidly to circulatory collapse leading to hypotension and shock
laryngeal oedema and bronchospasm lead to respiratory arrest
Management
ABC
any suspect drug should be ceased immediately
administer oxygen 6-8+ L/minute
adminster adrenaline IM, may be repeated every 5 minutes and may be given IV
lay patient flat and elevate legs, monitor vitals and ecg
if hypotensive, rapid IV replacement
if there is severe laryngospasm, bronchospasm, shock or patient is unconscious, u must intubate and commence positive pressure ventilation and call MET
stridor: nebulised adrenlaline, intubation if needed
wheeze: salbutamol or adrenaline by nebuliser
monitor for at least 4-6 hours for biphasic reaction
later… organise epipen for patient, medical alert bracelet and establish anaphylaxis action plan
SOFAH
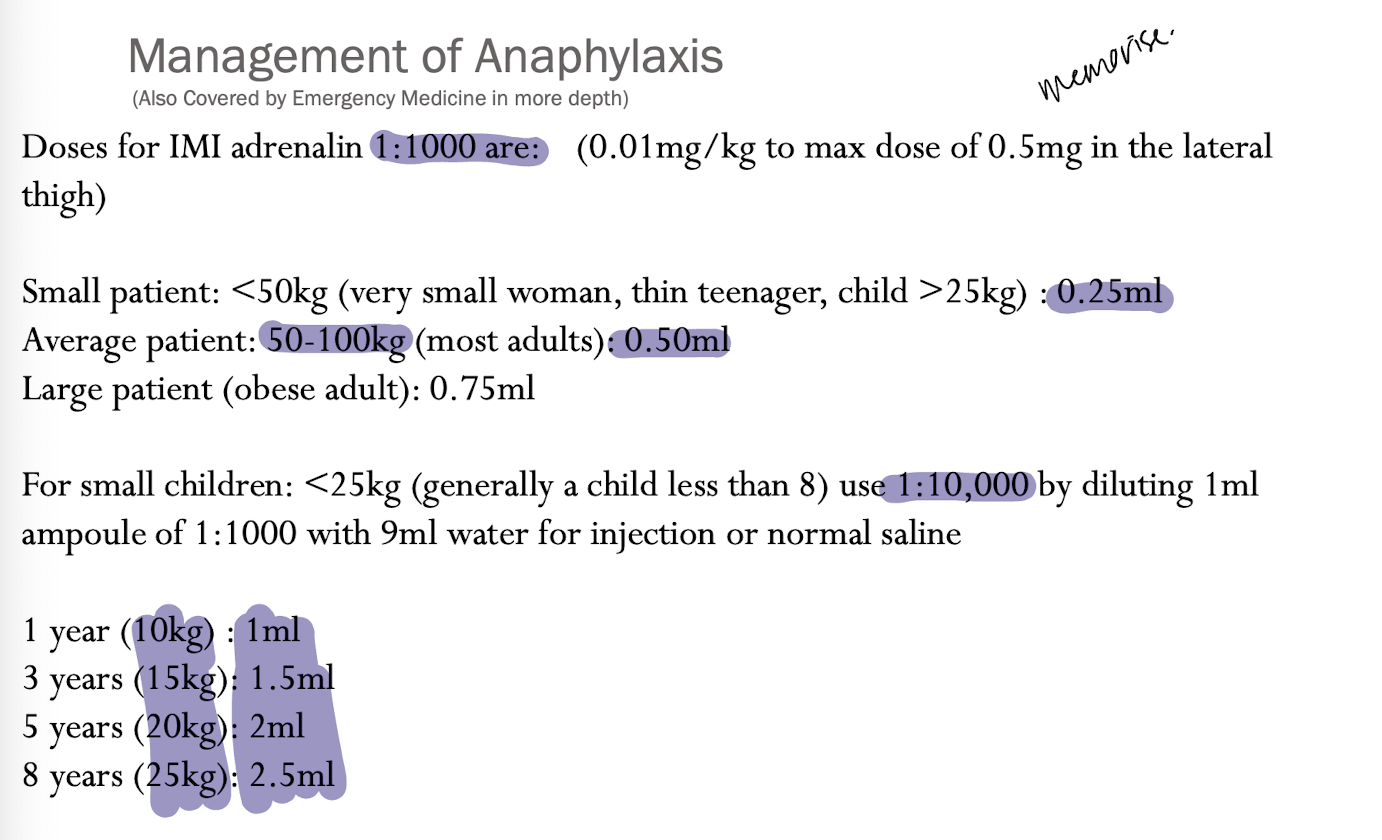
just remember for adults, 0.25, 0.5, 0.75 and for kids divide by 10
Erythema
used to describe any skin disease that involves 90% or more of the body surface area
can be inflammatory , erythematous or scaly
loss of skin barrier can cause systemic disturbance. like hypothermia, fluid and protein loss, electrolyte disturbance and cardiac failure
FIVE MAIN CAUSES
dermatitis
psoriasis
cutaneous lymphoma
drug reactions (DRESS)
pityriasis rubra pilaris (very rare)
Types of cutaneous drug reactions
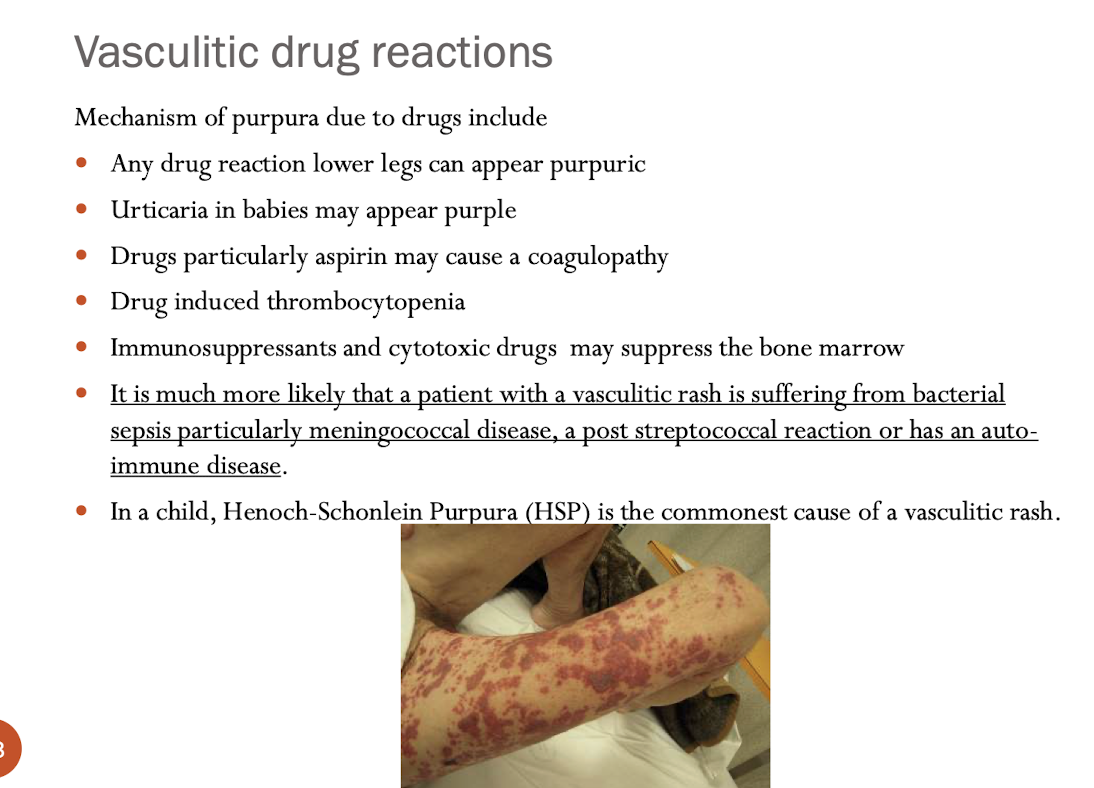
Vasculitis (type 3 immune complex mediated) - characteristics, aetiology
vasculitis - inflammation of blood vessels
(size of blood vessels affected determine the clinical appearance of the rash)
superficial:
palpable purpura, ulcers and necrosis, no blanch, most likely found in areas where immune complexes settle due to gravity (so lower legs or for bed bound patients, the back, buttocks and legs)
histopathology is damage to vessel walls by PMN leukocytes
examples
acute meningococcaemia (spread by resp droplets, neisseria meningococcus (fever, severe headache, photophobia, neck stiffness, myalgia and arthralgia)
IgA medicated vasculitis : Henoch-Schlonlein purpura (in kids, rarely in adults, palpable purpura associaed with arthritis, abdo pain and nephritis)
acute haemorrhagic oedema (in babies and toddlers, probably viral)
urticarial vasculitis (persistent urticarial-like wheals but does not migrate, leaves bruising and hyperpigmentation)
Medium sized vessel vasculitis
most common is polyarteritis nodosa
presents with nodules, livedo reticularis and ulcers
systemic disease is common, affecting joints, peripheral nerves, muscles, myocardium and kidneys
Mixed (small and medium vessels involved)
most common is granulmatosis with polyangiitis
presents with severe necrotising and ulcerating skin lesions, with involvement of upper and lower respiratory tract and kidneys
deeper and larger: nodules and plaques
other presentations include urticarial lesions, bruises, blisters, livedo reticularis, vesicles and pustules
also a HALLMARK of meningococcal infection
aetiology
50% is idiopathic
iral and bacterial infection, particularly meningococcal disease but accompanying any form of sepsis (meningococcus, strep, hep b and c, hiv)
underlying connective tissue disease - SLE and rheumatoid arthritis (immune complex)
hypersensitivity reaction to drugs (immune complex)
in chiildren 3 main causes KNOW THEM
infection most often strep
henoch schlonlein purpura, a characteristic IgA mediated vasculitis
acute haemorrhagic oedema
Management
uncomplicated small vessel vasculitis is usually benign, and self-limiting, resolved once underlying trigger removed
examine for systemic disease signs like hepatosplenomegaly, lymphadenopathy, ocular involvement, CNS abnormalities and joint swelling
urinalysis
skin biopsy with immunofluorescence for IgA
FBC
ESR
U&E
LFT
ASOT?
for larger vessels ANCA - detects anti-neutrophil antibodies
possible connective tissue screening if SLE is suspected
Toxic shock syndrome clin features
multisystem disease resulting from exotoxin from S.aureus or S.pyogenes
varicella may precede strep toxic shock, associated with retained tampon
clin features
fever
malaise
headache
pharyngitis
myalgia
erythematous macular or scarlatiniform rash most obvious in the flexures and on hands and feet
oedematous face, hands and feet too
enanthem (rash of mucous membrane) with reddened lips and tongue and mild conjunctivitis
multiorgan involvement can occu
otne leukocytosis and raised LFTs
platelet count may be low and DIC can occur
usually desquamation 2-3 weeks after rash
hair loss and nail dystrophy may occur
Kawasaki disease
multisystem vasculitis with cutaneous, mucosal and systemic manifestations
affects kids aged <5
The most sinister association of this condition is coronary artery lesions in about 20% of cases. If left untreated this can lead to aneurysm, thrombosis, myocardial infarction and death.
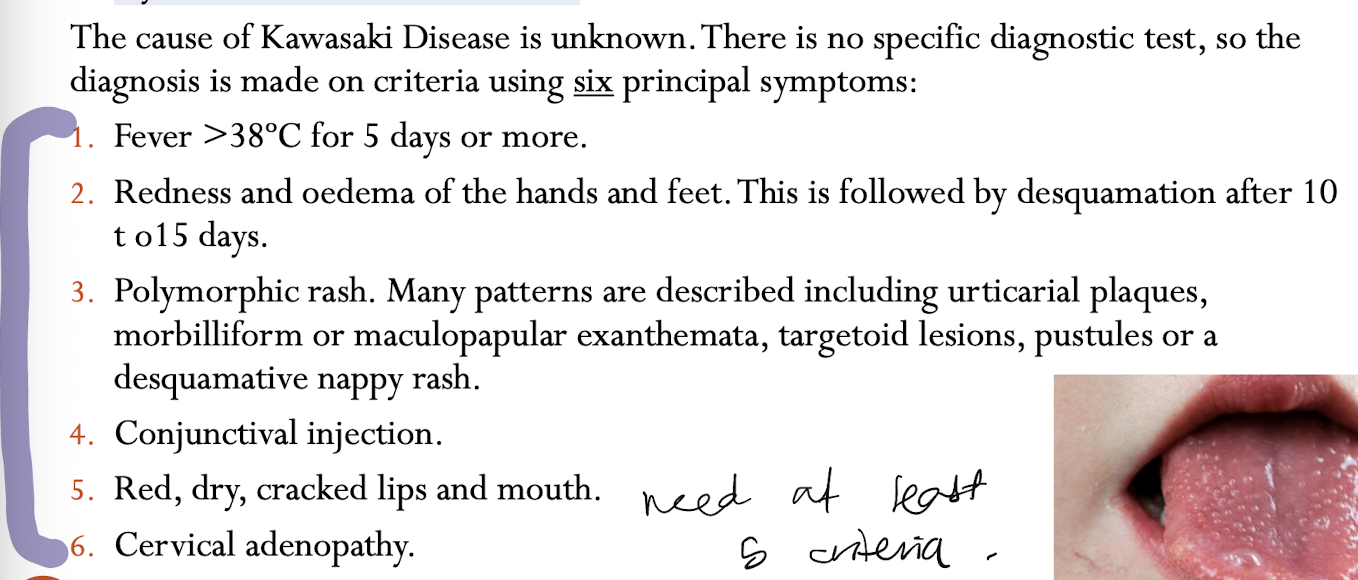
no known cause, no specific diagnostic test, blood tests aren’t diagnostic. there is commonly leukocytosis, thrombocytosis and raised ESR and CRP
SSSS clin features
caused by exotoxins of S.aureus
like kawasaki disease children aged <5
clin features
fever, macular erythema (like superficial burn) and then superficial blistering
treatment
early oral antibiotics
late IV and hospital
Patient with multiple blisters and pustules causes
majority of conditions are not life-threatening (except SJS, TENS, and EM)
causes can be
infection (varicella zoster, HSV (eczema herpeticum), staph. folliculitis, bullous impetigo, SSSS, bacterial:necrotising fasciitis)
allergic reactions (contact dermatitis, allergen contact w skin, type iv reaction, drug reactions (doxy (photoallergic reactions) AGEP, TENS), rash is usually erythematous, oedematous)
pustular psoriasis, rare erythroderma with tiny sterile pustules, need to exclude infection and needs hospital admission)
immunobullous diseases rare, bullous pemphigoid
pompholyx (dyshidrotic dermatitis)
Eczema Herpeticum (definition, clin features, complications, management)
Definition:
Eczema herpeticum is a disseminated viral infection characterised by fever and clusters of itchy blisters or punched-out erosions. It is most often seen as a complication of atopic dermatitis/eczema.Clinical Features:
Extensive crusted papules, blisters, and erosions
Primary HSV infection presents with fever and malaise
Complications:
Systemic dissemination of herpes with hepatitis, encephalitis, DIC, and death in immunocompromised patients
Management:
Treat underlying atopic eczema
Antivirals
Necrotising Fasciitis (definition, aetiology, risk factors, clin features, complication)
Definition:
Infection of deep fascial planes leading to necrosis of subcutaneous tissue and skin.Etiology:
Usually Group A Streptococcus
Epidemiology / Risk Factors:
50% occur in healthy individuals
Risk factors: skin trauma, abdominal surgery, diabetes, immunosuppression
Clinical Features:
Severe pain in affected area
Oedema, foul-smelling exudate
Skin blistering, necrosis
Patient is systemically unwell
Complications:
Streptococcal toxic shock may occur
Management of drug eruptions
identify causative drug
investigations (no diagnostic test, eosinophilia and raised LFTs often occur - skin biopsy may be helpful but not diagnostic)
stop suspected drug and replace with chemically unrelated drug (may continue under certain circumstances but seek advice first - is essential, no substitute, used for short time, no urticaria or skin blistering, anaphylaxis or severe reactions)
further management: most reactions cease within 1-2 weeks EMOLIENTS AND STEROID CREAMS (MAINSTAY), antihistamines for urticarial drug reactions, oral steroids for 1-2 weeks for very itchy and uncomfortable exanthematous
Management of Severe Drug reactions
requires dermatological opinion in hospital
needs FBC, LFT, urinalysis and skin biopsy
ophthalmology opinion if conjunctivitis
mycoplasma serology, CXR and viral swabs on admission
management: as discussed for DRESS and erythema multiforme and TENS (cease drug, oral steroids?, burns unit for TENS?)
prevention: emergency bracelets, first degree relatives at risk so take precautions
Different types of cutaneous drug reactions
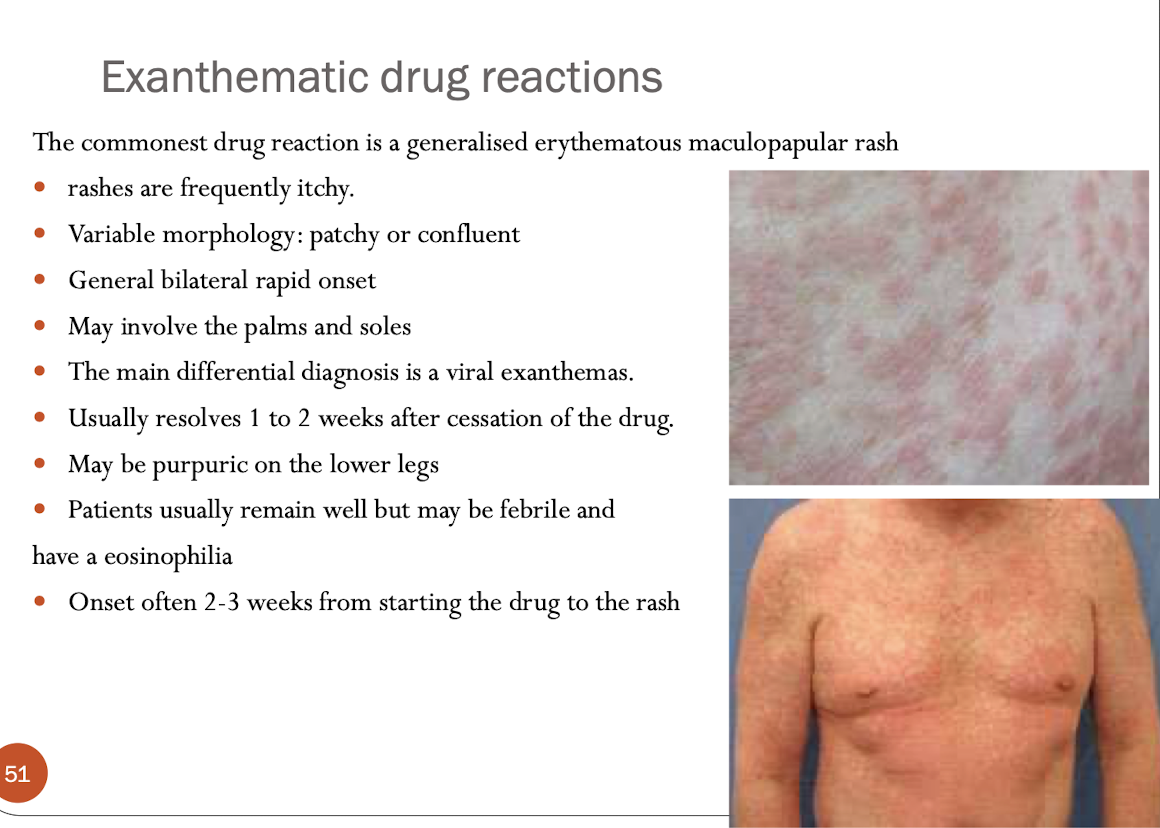
things to remember:
Any widespread rash occurring within 2-3 weeks of commencing
a new drug should be suspected of being due to the drug.
it is necessary to sort them
into those that have been most recently commenced and are
temporally related to the onset of the rash
There is no one diagnostic tests however an eosinophilia and
raised LFT's often accompany drug reactions. Skin biopsy may be
helpful
If a patient has been able to tolerate a drug several times in the past without a reaction, it is also very unlikely for them to suddenly become allergic to it.
Antihistamines will only be effective for urticarial drug reactions. There is no value
in administering them for any other type of drug reaction.
Types of drug reactions (in simplified table form)
Type | Key Features | Onset | Common Drugs | Notes |
|---|---|---|---|---|
Exanthematous | Diffuse red maculopapular rash | 2–3 weeks | Antibiotics, anticonvulsants | Most common |
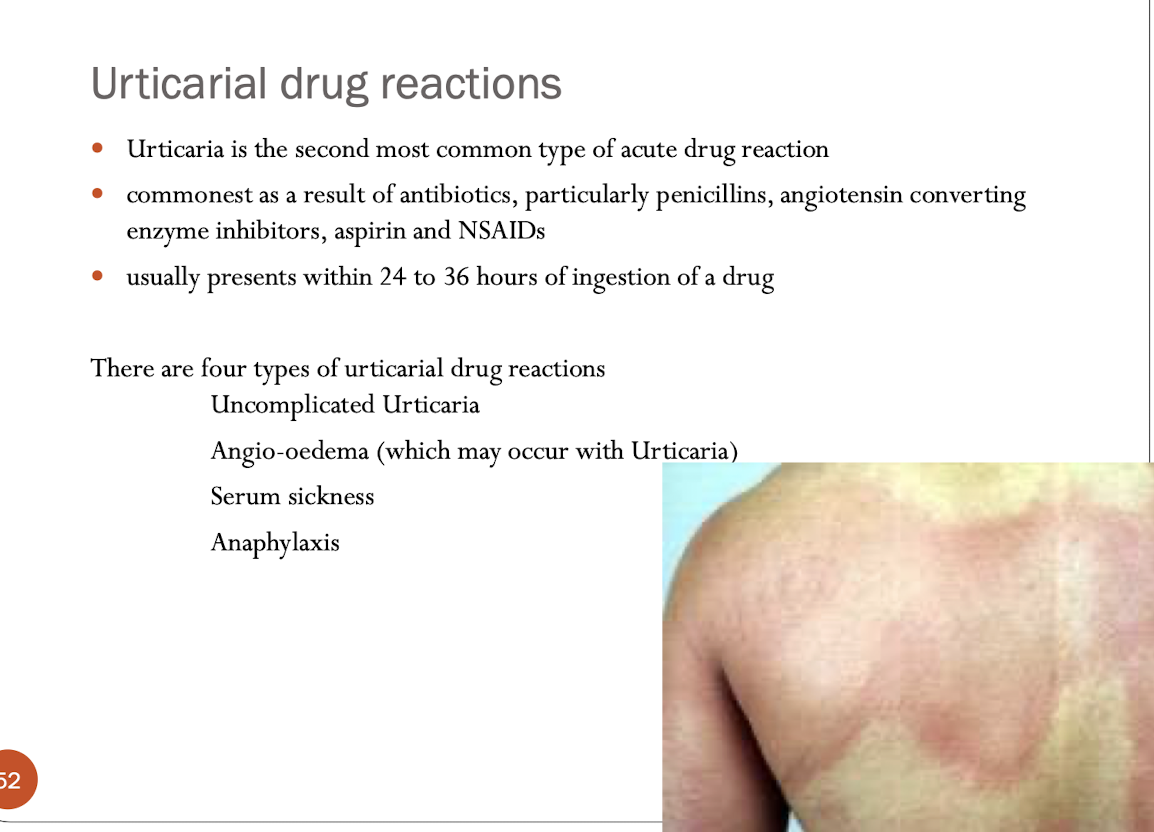
Urticarial | Hives, itching | 24–36 hrs | Penicillins, NSAIDs, ACEi | May progress to anaphylaxis |
Vasculitic | Purpura (esp. legs) | Variable | Aspirin, cytotoxics | Rule out infection |
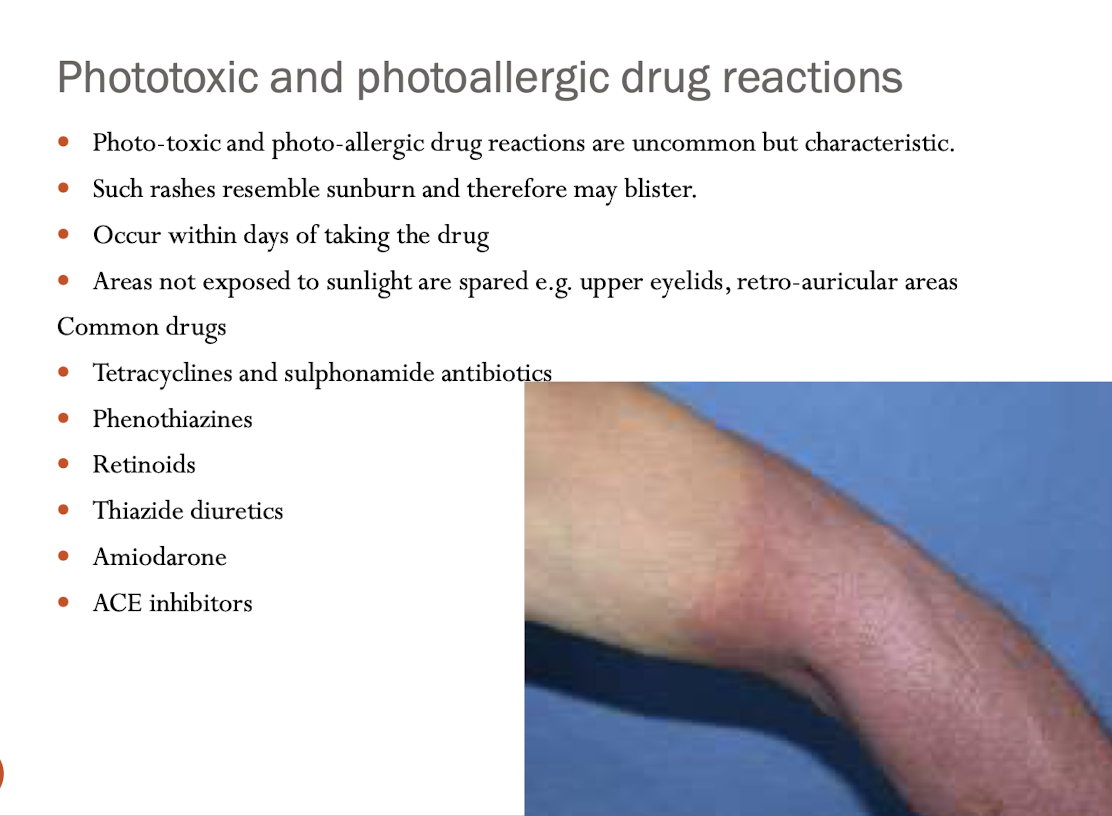
Phototoxic | Sunburn-like rash | Days | Tetracyclines, amiodarone | Sun-exposed areas only |
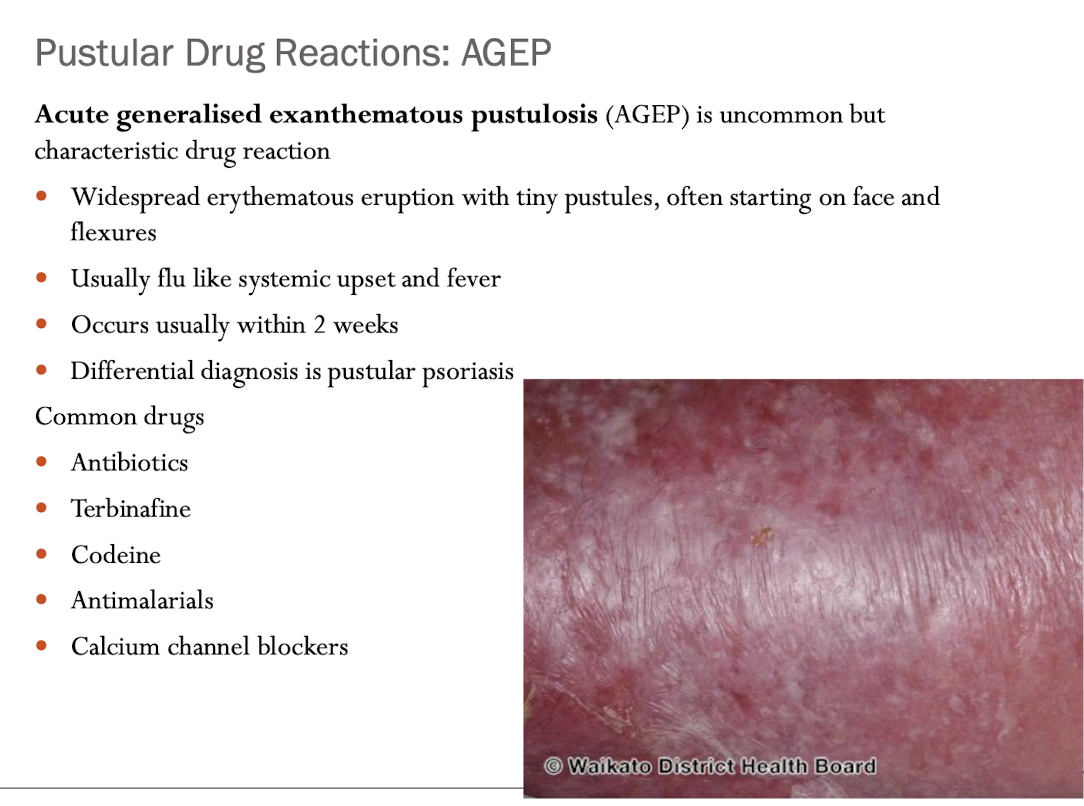
Pustular (AGEP) | Small pustules, fever | ≤2 weeks | Antibiotics, terbinafine | Looks like pustular psoriasis |
Eczematous/Lichenoid | Chronic eczema-like | Variable | Thiazides, gold | Rare |
Fixed drug eruption | Recurs in same spot | Hours–days | Sulfonamides, NSAIDs | Heals with pigmentation |