lower airway and pleural space sx
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
113 Terms
what are considered part of the lower respiratory system?
trachea/bronci
lungs
pleural sapce
thoracic wall
what is the anatomy of the trachea?
34-44 C shaped cartilagnious rings
annular ligaments
dorasl tracheal membrane
vascular supply - segmental
recurrent laryngeal nerves
what is the dorsal tracheal membrane made up of?
mucosa
connective tissue
trachealis muscle
what is the vascular supply of the trachea?
cranial and caudal thyroid arteries
bronchial arteries
where do the recurrent laryngeal nerves span?
from dorsolateral edges of trachea cranial to heart
what is the common surgical approach to the cervical trachea?
ventral midline skin incision and spread the muscles apart
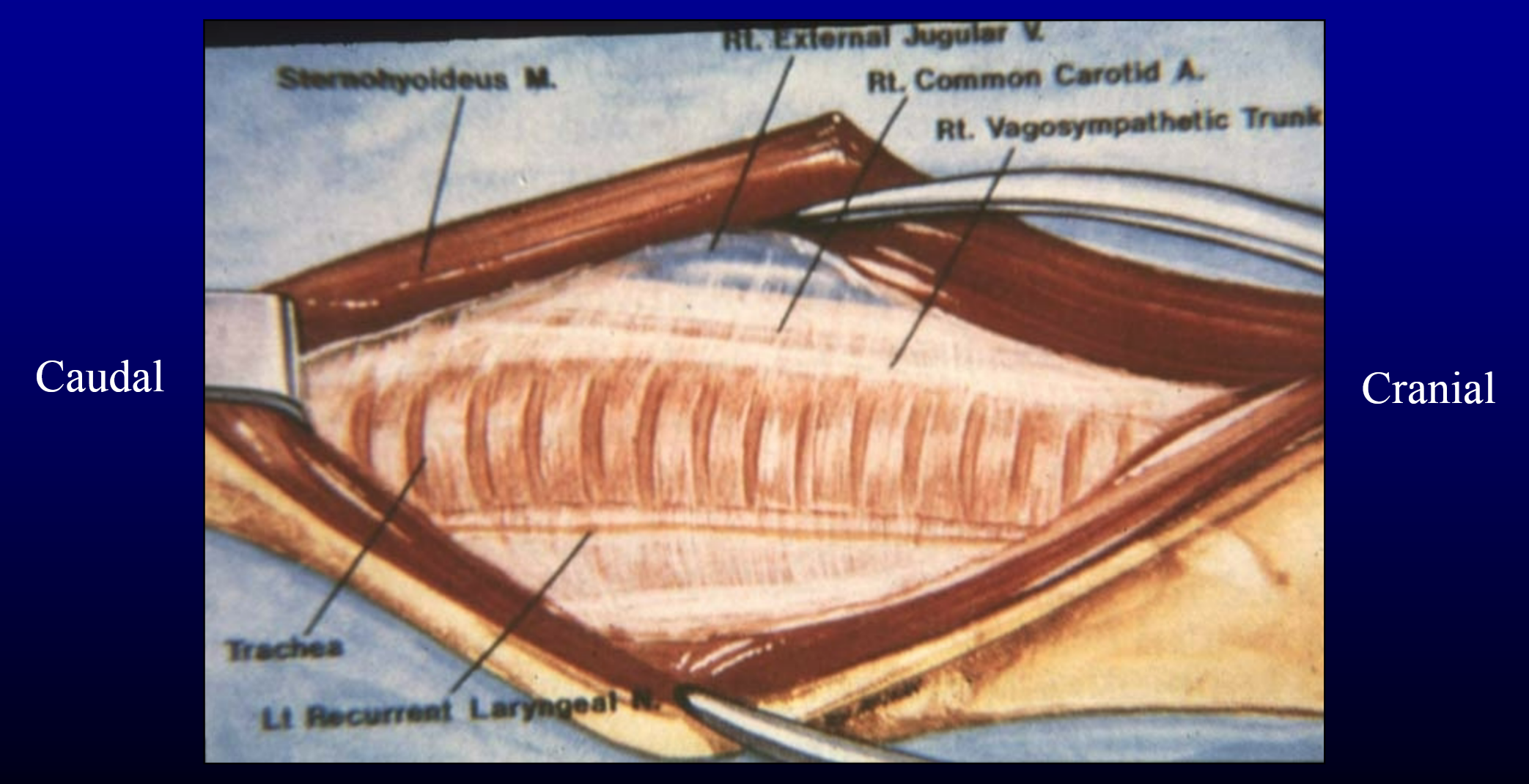
what is the surgical approach to the thoracic trachea?
right 3rd or 4th intercostal thoracotomy
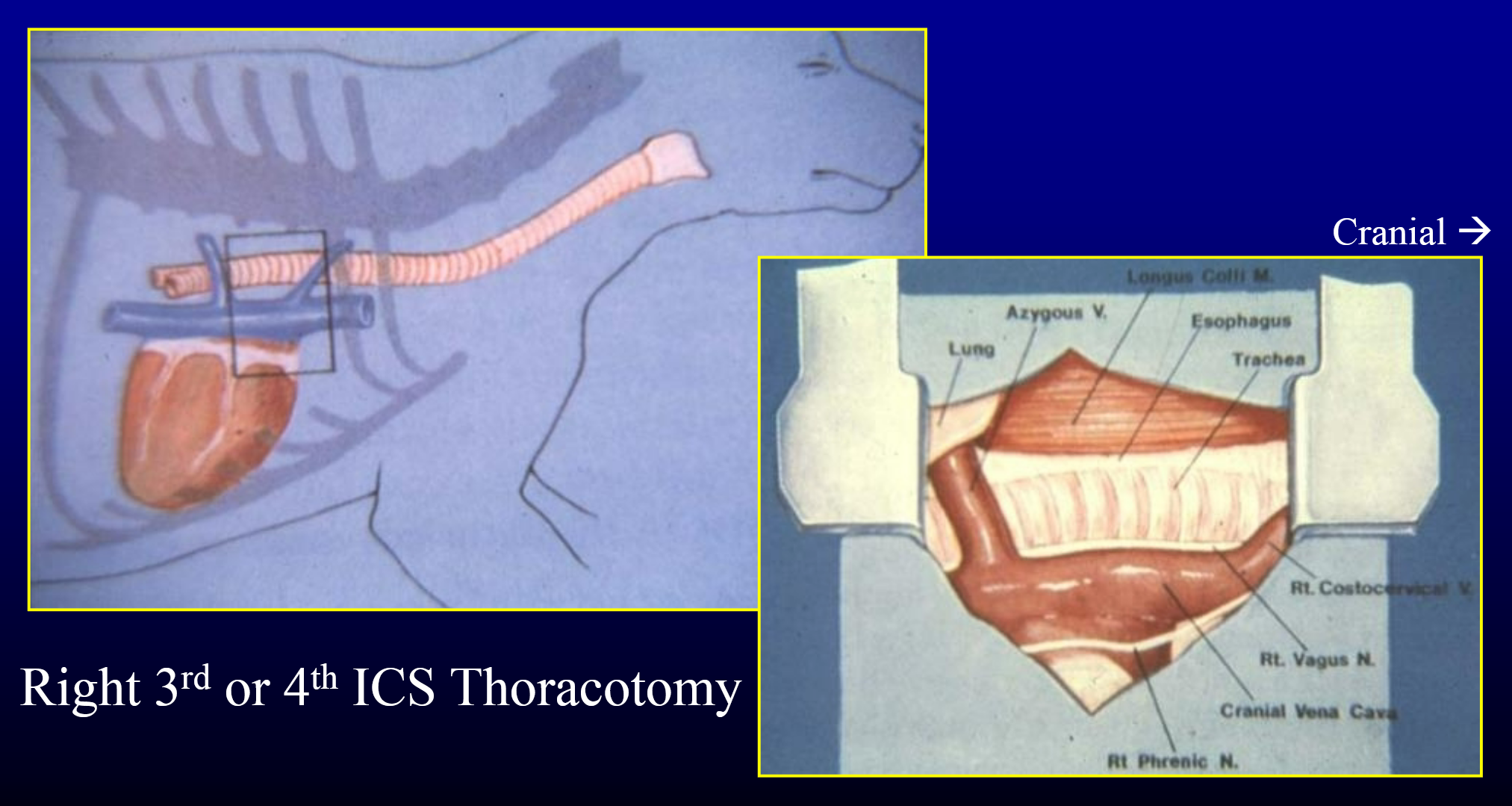
why do we go on the right side of the thorax?
to avoid the esophagus
what are the congential diseases of the tracheal and bronchi?
tracheal collapse
tracheal hypoplasia
what is the signalment and clinical signs of tracheal collapse?
primarily miniature and toy breeds
typical age at dx = 7 years old
coughing
dyspnea
on inhalation, what section of the tracheal collapses?
cervical
on exhalation, what part of the trachea collapses?
thoracic
what is the pathology of tracheal collapse?
congenitally hypoplastic or fibrodystrophic cartilaginous rings
redundant or weak dorsal tracheal membrane
may involve both cervical and thoracic trachea
may extend to mainstem bronchi (and lower)
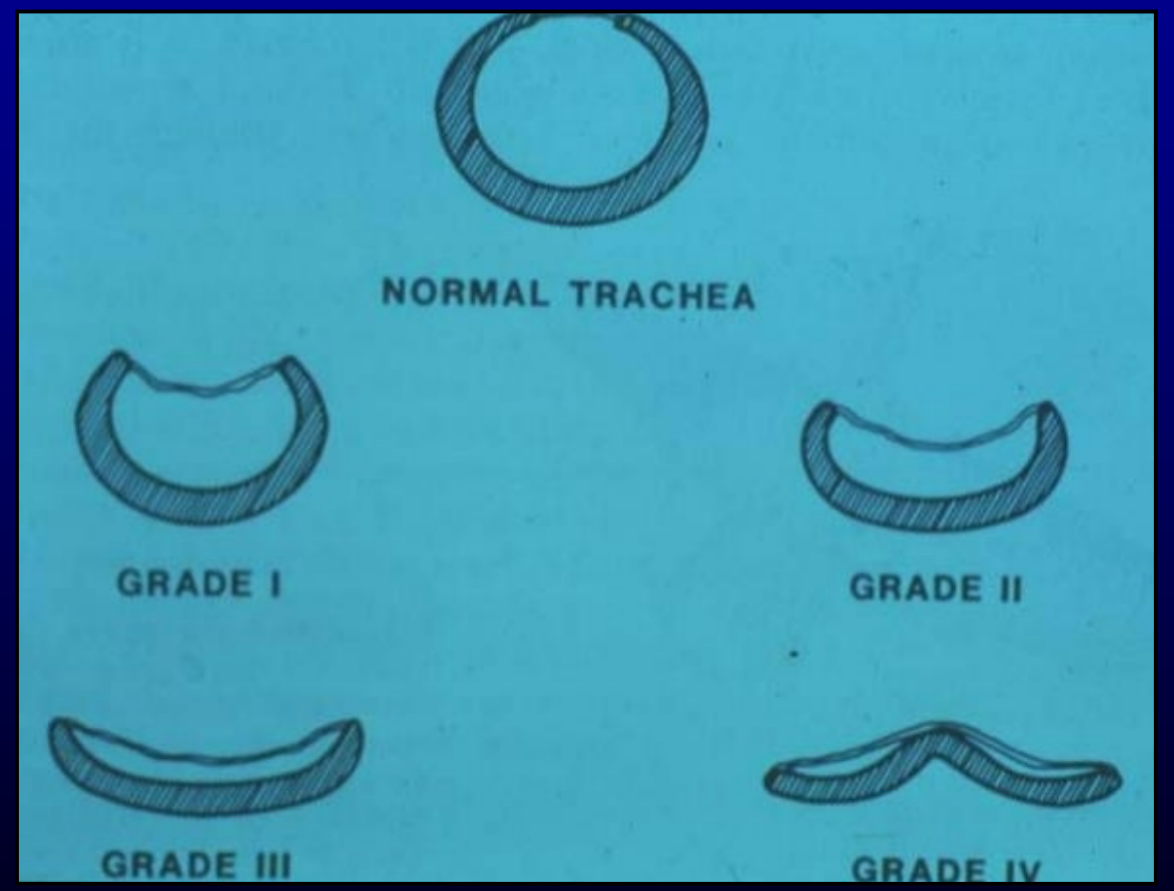
four grades of tracheal collapse based on % of lumen reduction
what are the grades of tracheal collpase?
grade 1 = 25% lumen reduction
grade 2 = 50% lumen reduction
grade 3 = 75% lumen reduction
grade 4 = almost no lumen
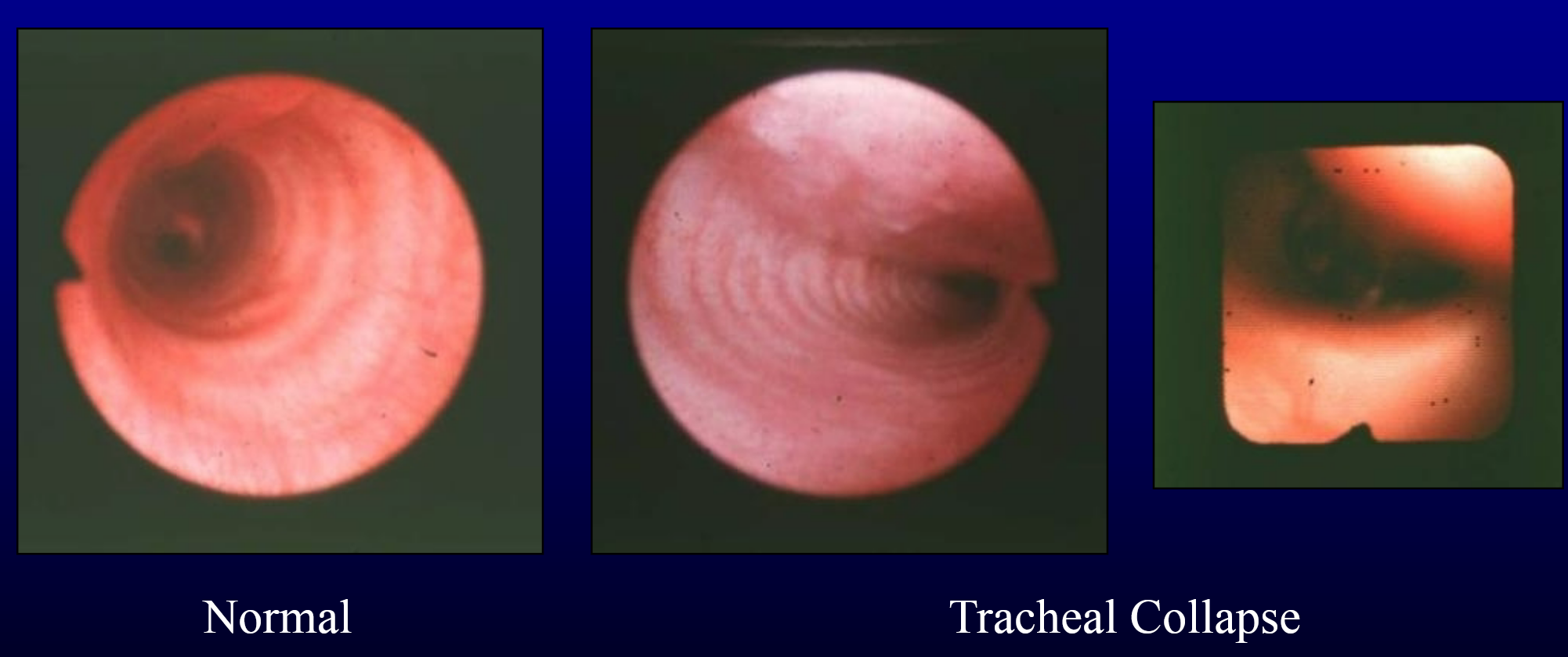
how to dx tracheal collapse?
cervical palpation
radiography
inspiratory/expiratory cervical and thoracic rads
fluoroscopy
tracheoscophy (with bronchoscopy)
grade collapse
rule out concurrent disease (cytology and culture)
laryngoscopy
rule out concurrent laryngeal paralysis
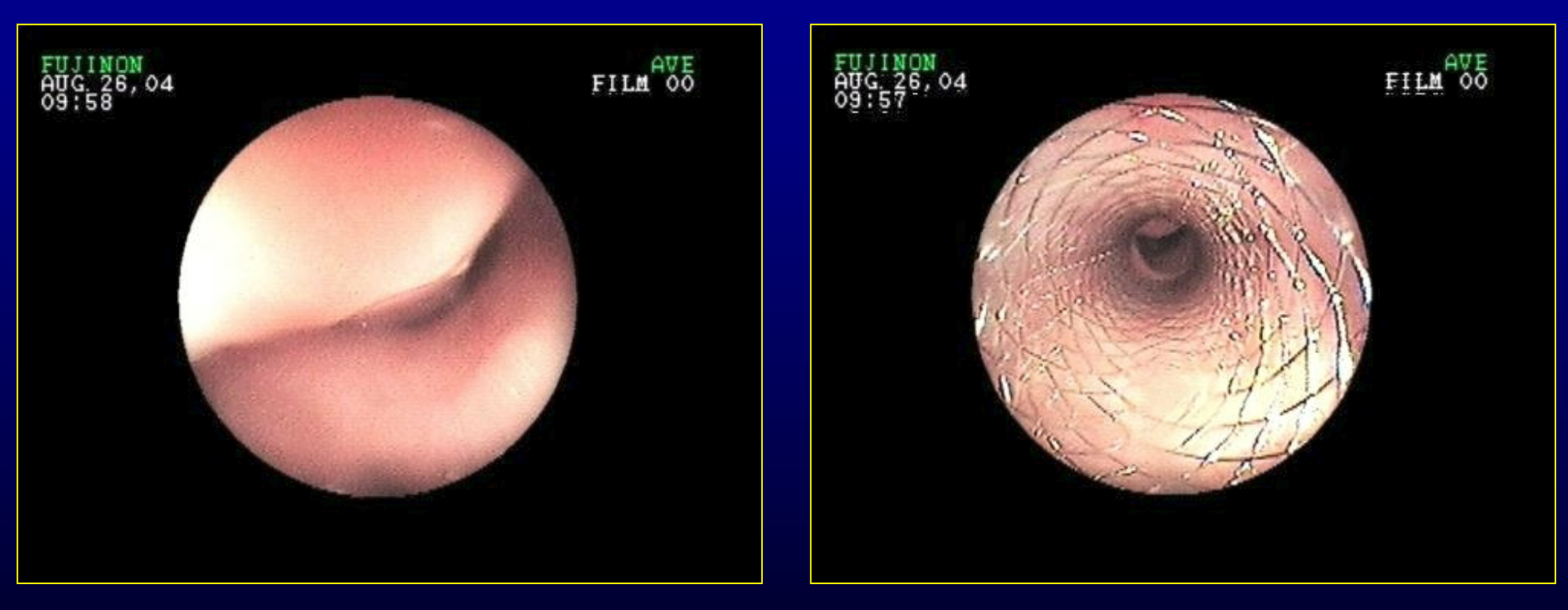
what is the tracheoscopic appearance of tracheal collapse?
C or D shape to lumen
what is the medical treatment of tracheal collapse?
typically preferred vs sx, esp for grade 1 and 2
cough suppressants
bronchodilators
antibiotics → if complicated by bacterial infection
control complicating factors
obesity
heat stress
leash irritation
when is surgical correction indicated for tracheal collapse?
when medical treatment cannot control clinical signs
what is the caveat to surgical treatment for tracheal collapse?
limited ability to alleviate bronchial collapse
what is sx treatment for tracheal collapse?
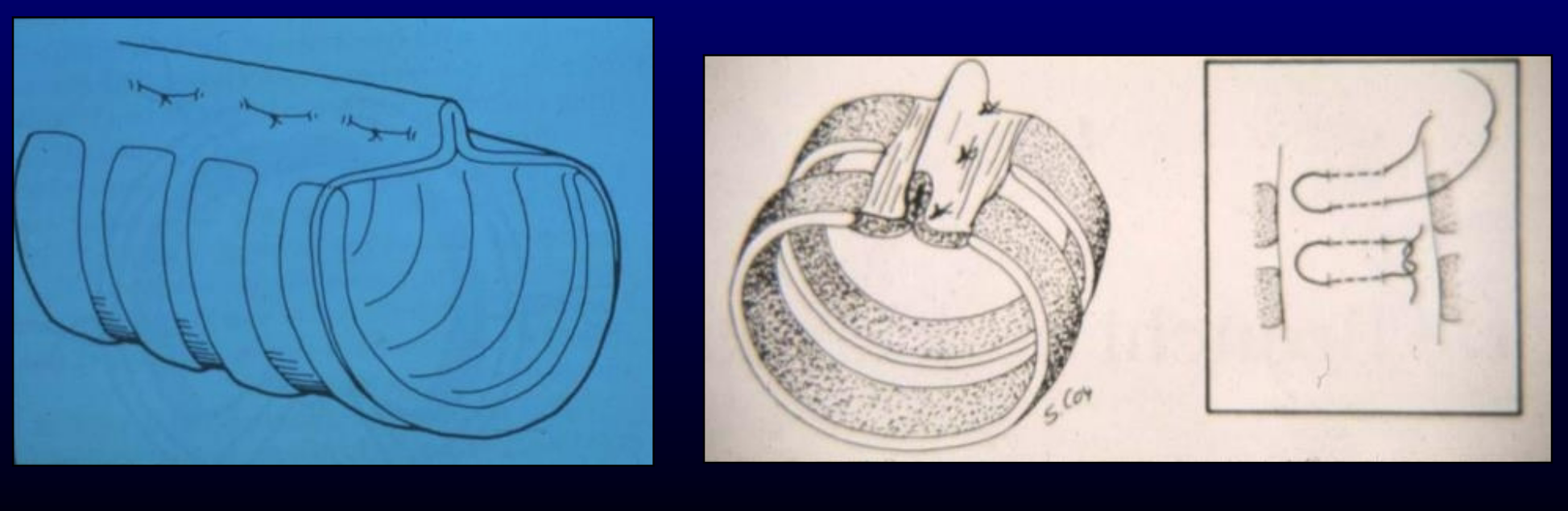
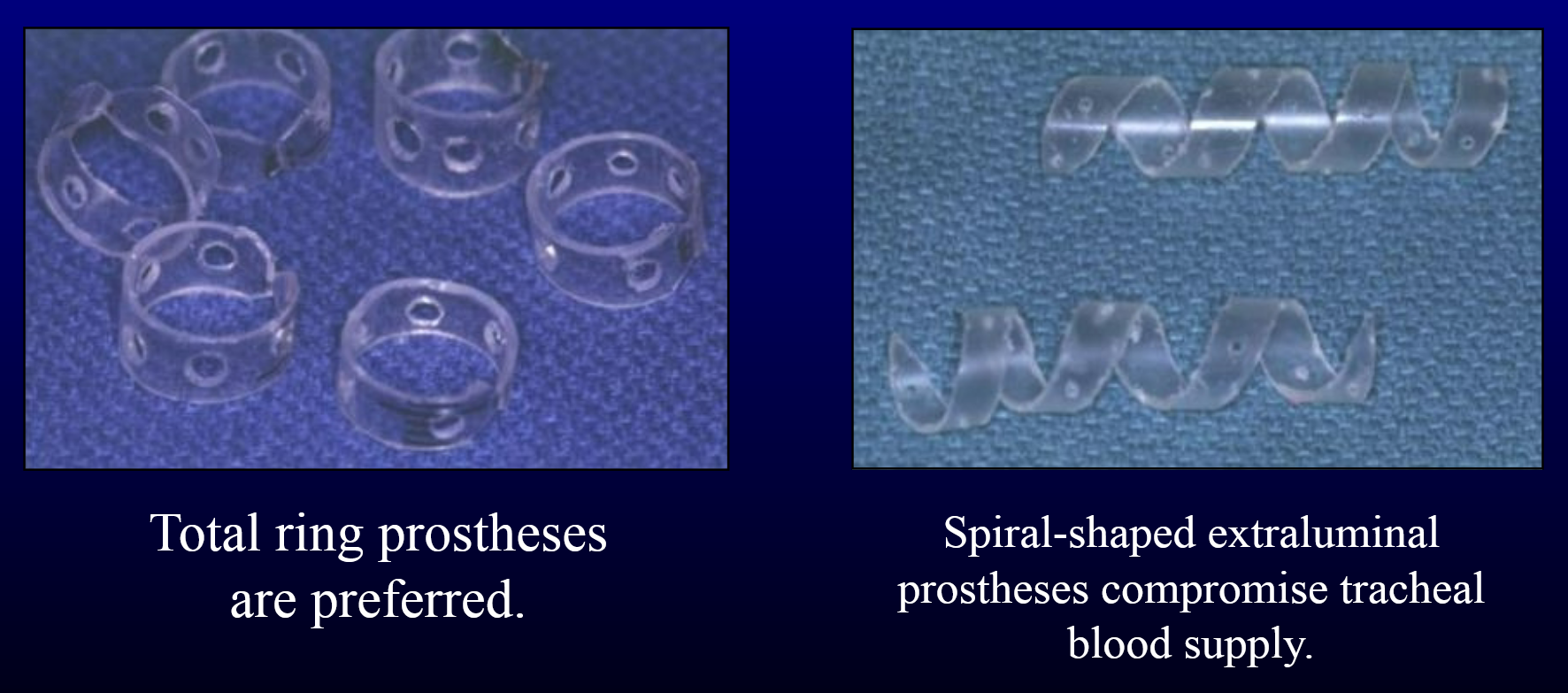
intraluminal stents or extraluminal prostheses
how is an intraluminal stent placed?
placed with aid of fluoroscopy or tracheoscopy
What is dorsal tracheal membrane plication?
plicating the dorsal portion of the trachea, HOWEVER not typically performed because it requires relatively normal tracheal cartilages
what are extraluminal prostheses made from?
polypropylene syringe or syringe cases
what is tracheal hypoplasia?
dorsally closed tracheal rings
small, firm trachea on palpation
small diameter trachea on radiographs
english bulldogs predominately
no surgical cure and no treatment
what are the consequences of injury to trachea and bronchi?
may result in air leakage and/or stenosis
what causes internal injury?
intubation
foreign bodies
what causes external injury?
blunt or penetrating trauma
what is tracheal stenosis?
narrowing of the trachea from scar tissue due to trauma
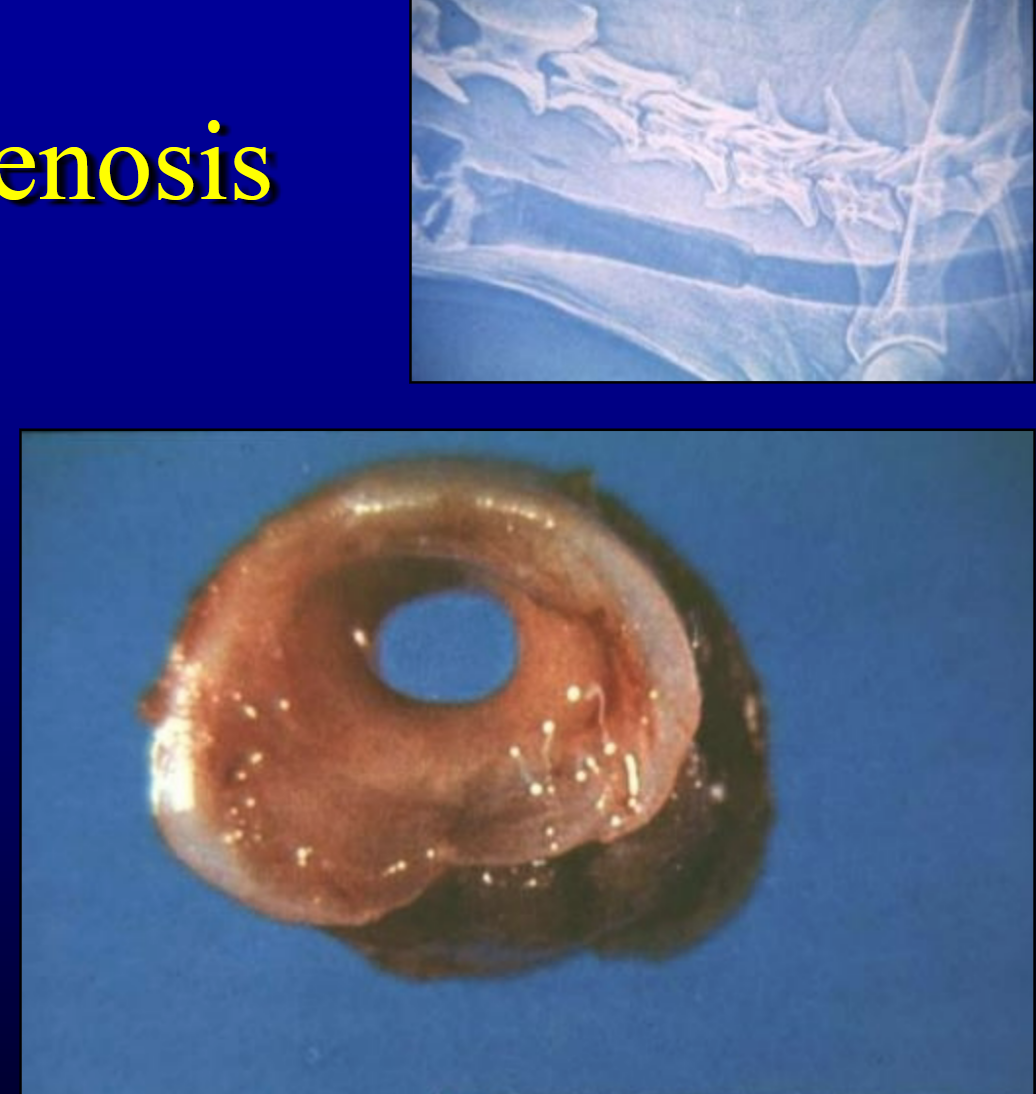
how to dx tracheal stenosis?
radiography
tracheoscopy
tracheal stenosis treatment options?
bougienage → dilation
balloon dilatation
stent → scar tissue may be too mature
resection/anastomosis
tracheal and bronchial foreign bodies
clinical signs = acute cough, sometimes dyspnea
dx = radiography and tracheobronchoscopy
treatment = endoscopic retrieval, tracheotomy or bronchotomy, lung lobectomy
tracheal blunt or penetrating clinical signs
persistent peritracheal, subcutaneous, and/or mediastinal emphysema
what is the treatment of tracheal trauma?
most tears resolve without surgical intervention
what is the emergency care of cervical trachea trauma?
may require orotracheal intubation or intubation through tracheal defect
wound management
what is the emergency care of thoracic trachea (and bronchi) trauma?
monitor for pneumothorax and treat as indicated
T/F most tracheal lacerations are self-limiting
true
what are the surgical treatment options for tracheal lacerations when needed?
can perform primary repair if there is reason to surgically expose the affected area
consider temp tracheostomy to decrease airway resistance → rarely necessary
resection/anastomosis if severe trauma or if stenosis results
exploratory thoracotomy if unable to resolve pneumothorax
what is a tracheal transection?
near the carina, the trachea is ripped off the lungs
this occurs in cats
what is the surgical treatment of tracheal transection?
right 3rd and 4th intercostal thoracotomy for anastomosis
requires delicate maneuvering of endotracheal tube and trachea
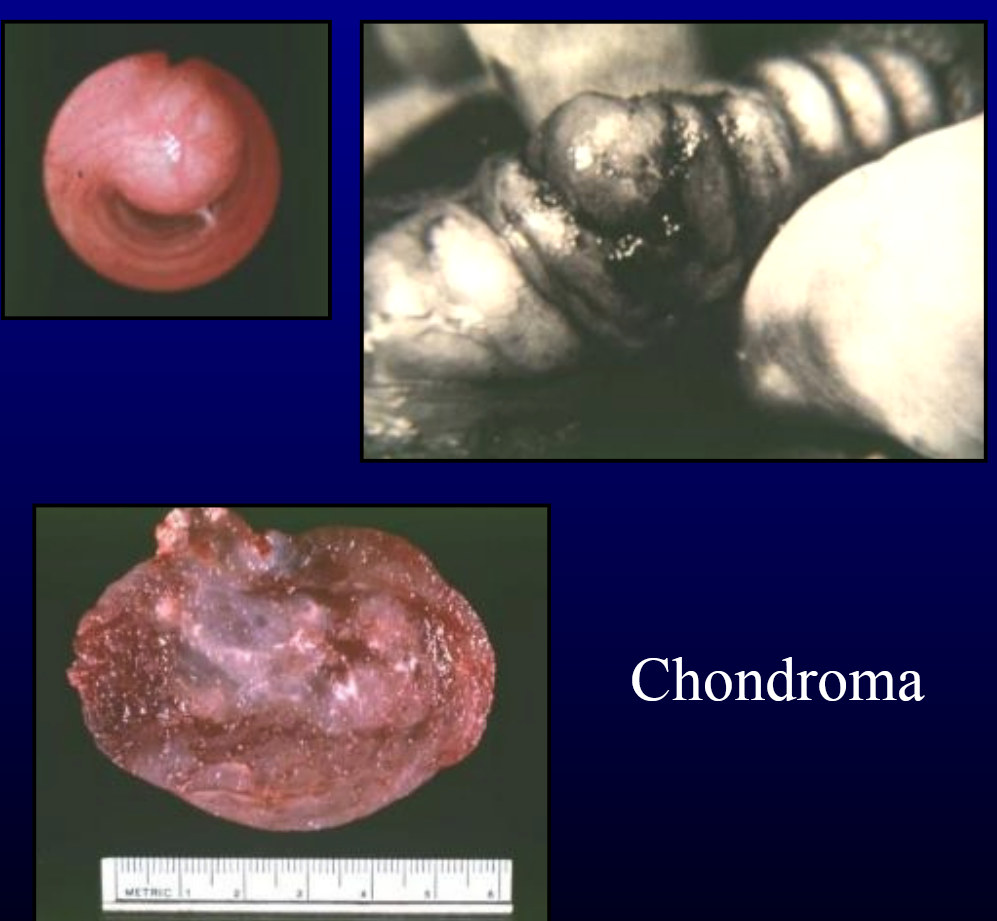
T/F neoplasia of the trachea and bronchi is very common
FALSE → uncommon
what are the complications that neoplasia of the trachea and bronchi?
intraluminal and/or extraluminal obstruction
progressive dyspnea
what is the highest number of tracheal rings successfully resected in a dog?
17
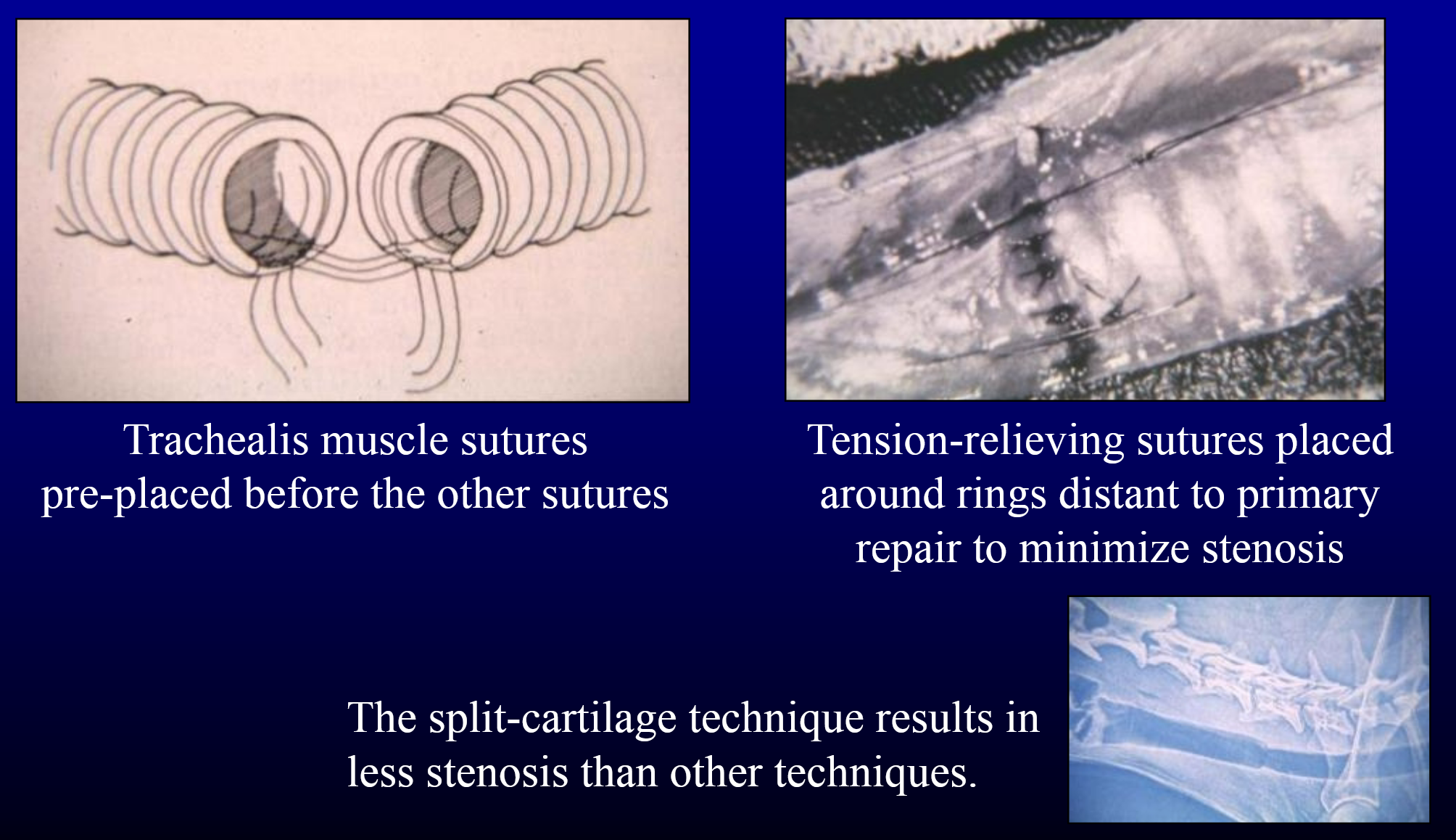
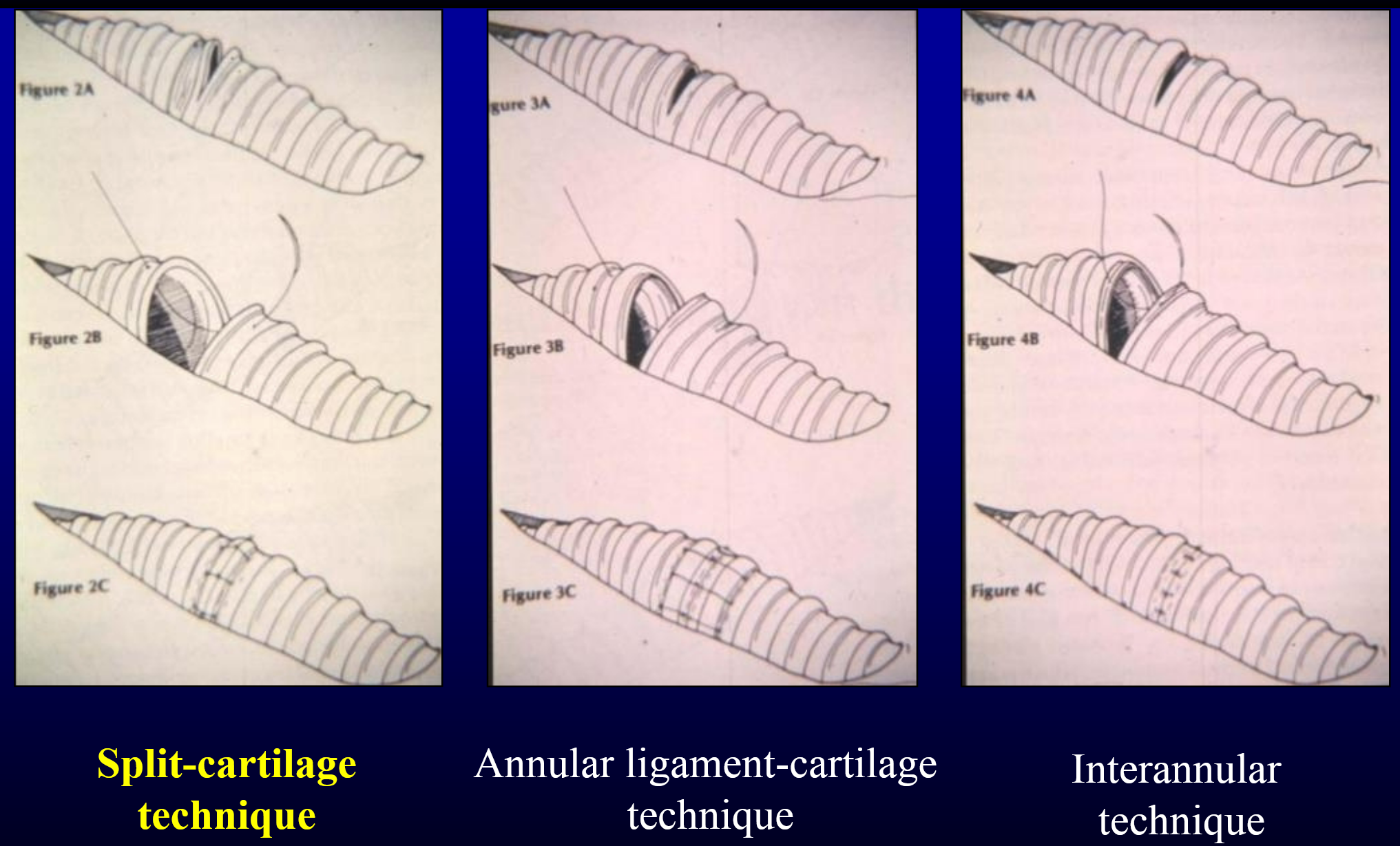
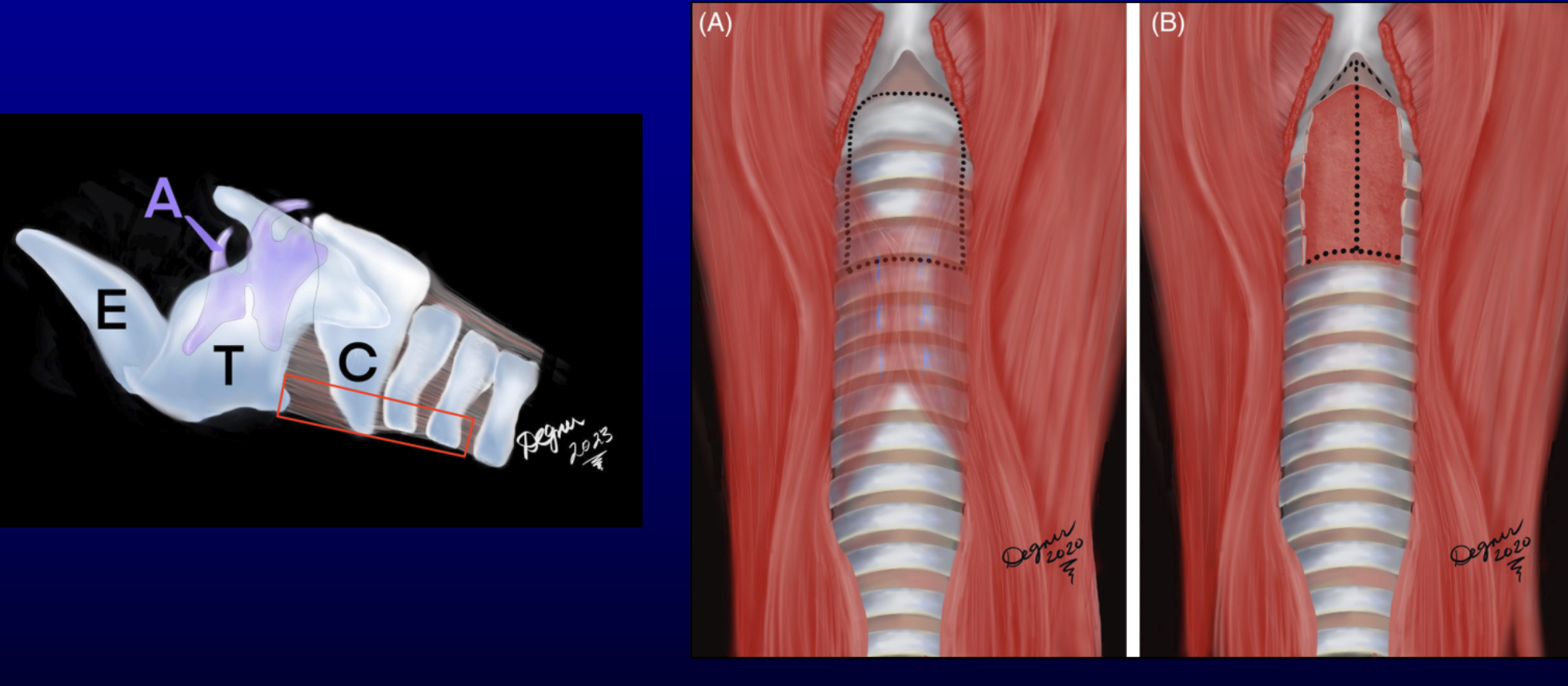
what are the 3 anastomotic techniques for tracheal anastomosis?
split-cartilage technique
annular ligament-cartilage technique
interannular technique
need tension-relieving sutures
what is partial replacement of tracheal reconstruction sx?
periosteum, polypropylene mesh, silicone rubber, vascularized pedicle flaps (diagram, stomach, sternohyoideus muscle)
what is segmental replacement of the tracheal?
1-4 cm circumferential segment
rib periosteum, auricular cartilage
are synthetic replacement of tracheal sucessful?
tend to fail due infection and stenosis
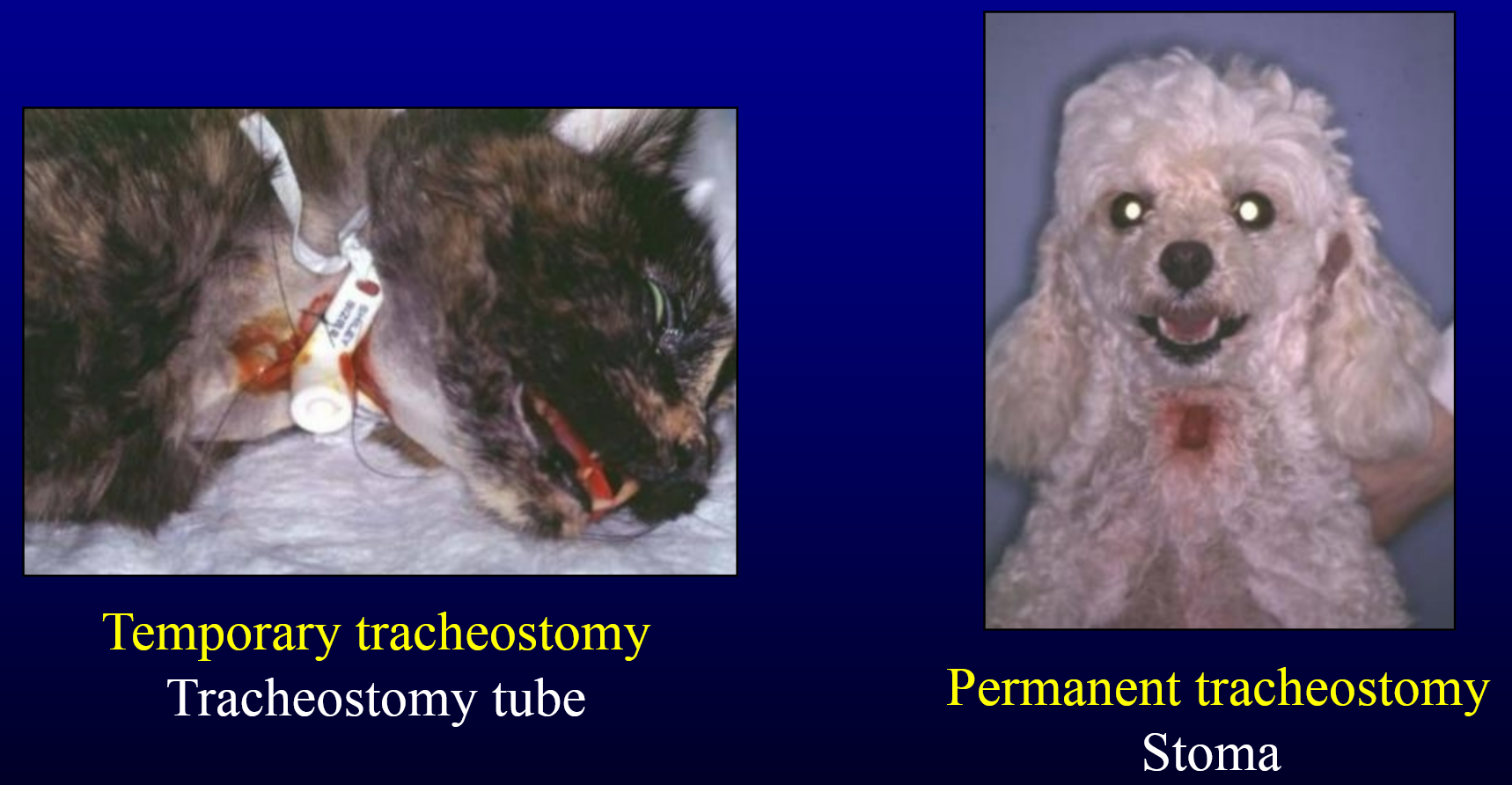
what are the 2 types of tracheostomy?
temporary tracheostomy
permanent tracheostomy
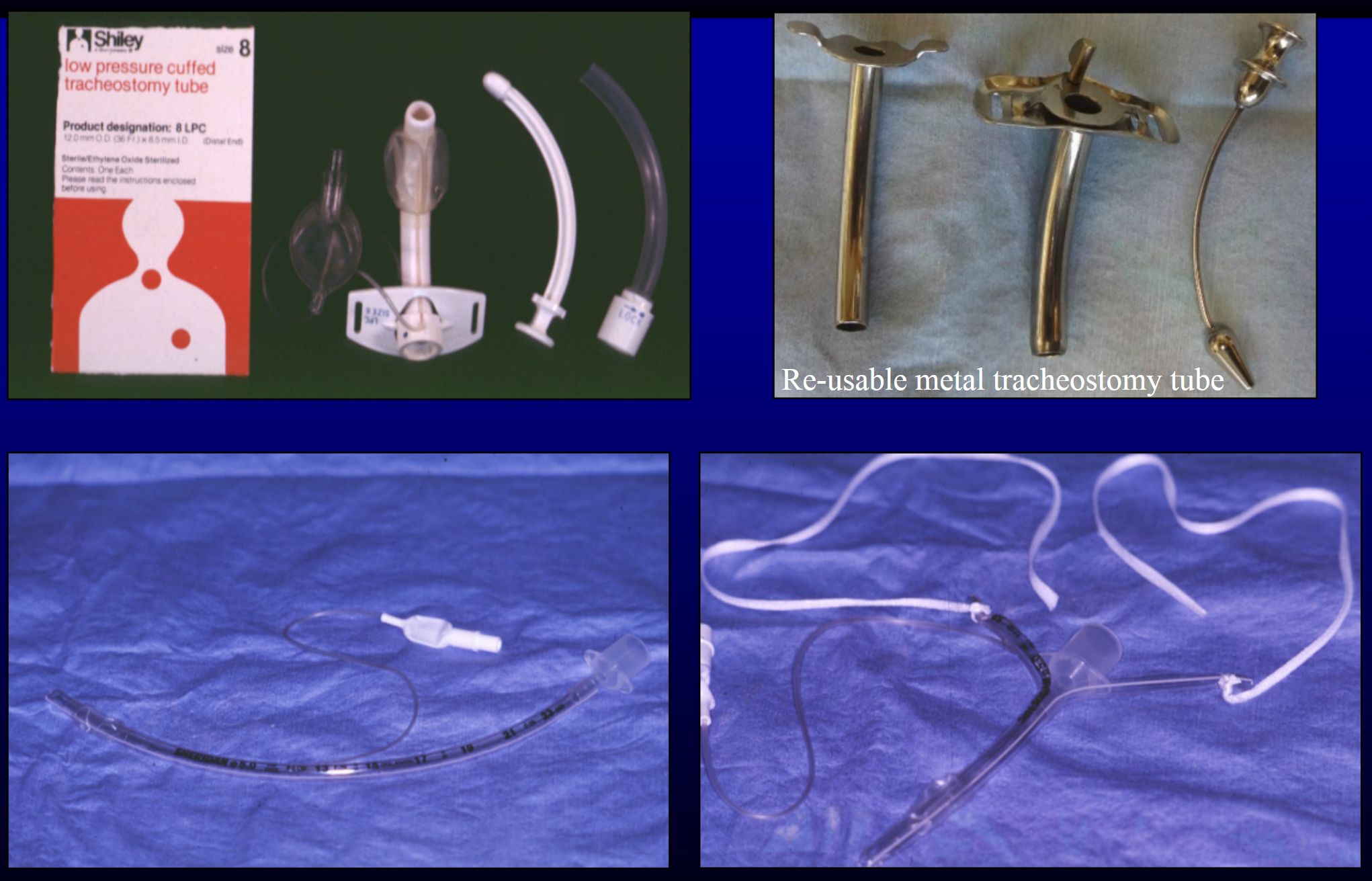
what are the indications of tube tracheostomy?
life-threatening upper airway obstruction
ventilatory assistance
removal of secretions and aspirated material
inhalation anesthesia for upper respiratory and intraoral surgery
what is a tube tracheostomy that is with or without inflatable cuff?
cuff needed for anesthesia and ventilatory assistance
tube without cuff preferred (safer) for simple maintenance of patent airway
tube tracheostomy with detachable inner tube
facilitates cleaning, suctioning
not available in small-sized tubes
what is a “home-made” tube for a tracheostomy?
fashioned from standard endotracheal tube
what is the prep for tube tracheostomy?
capture airway with endotracheal tube
prepare patient for controlled surgical approach
“slash” tracheostomy rarely necessary
dorsal recumbence
standard aseptic preparation of neck from chin to manubrium
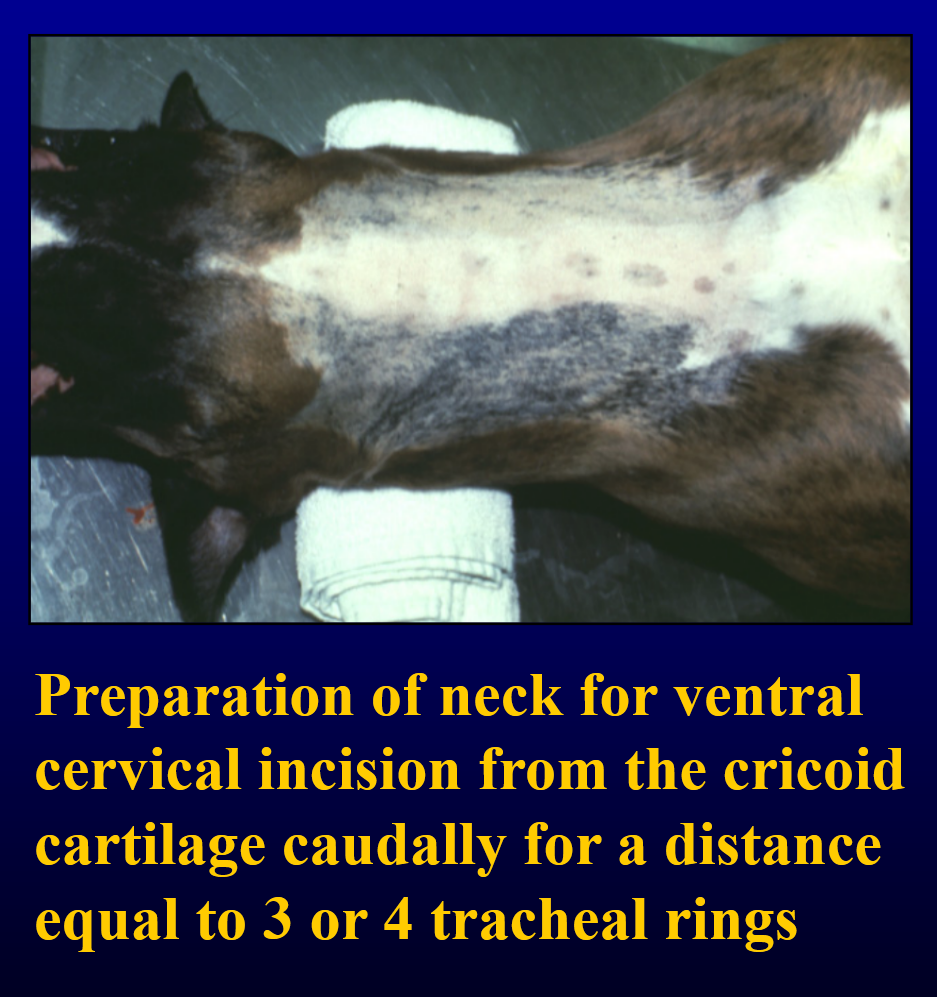
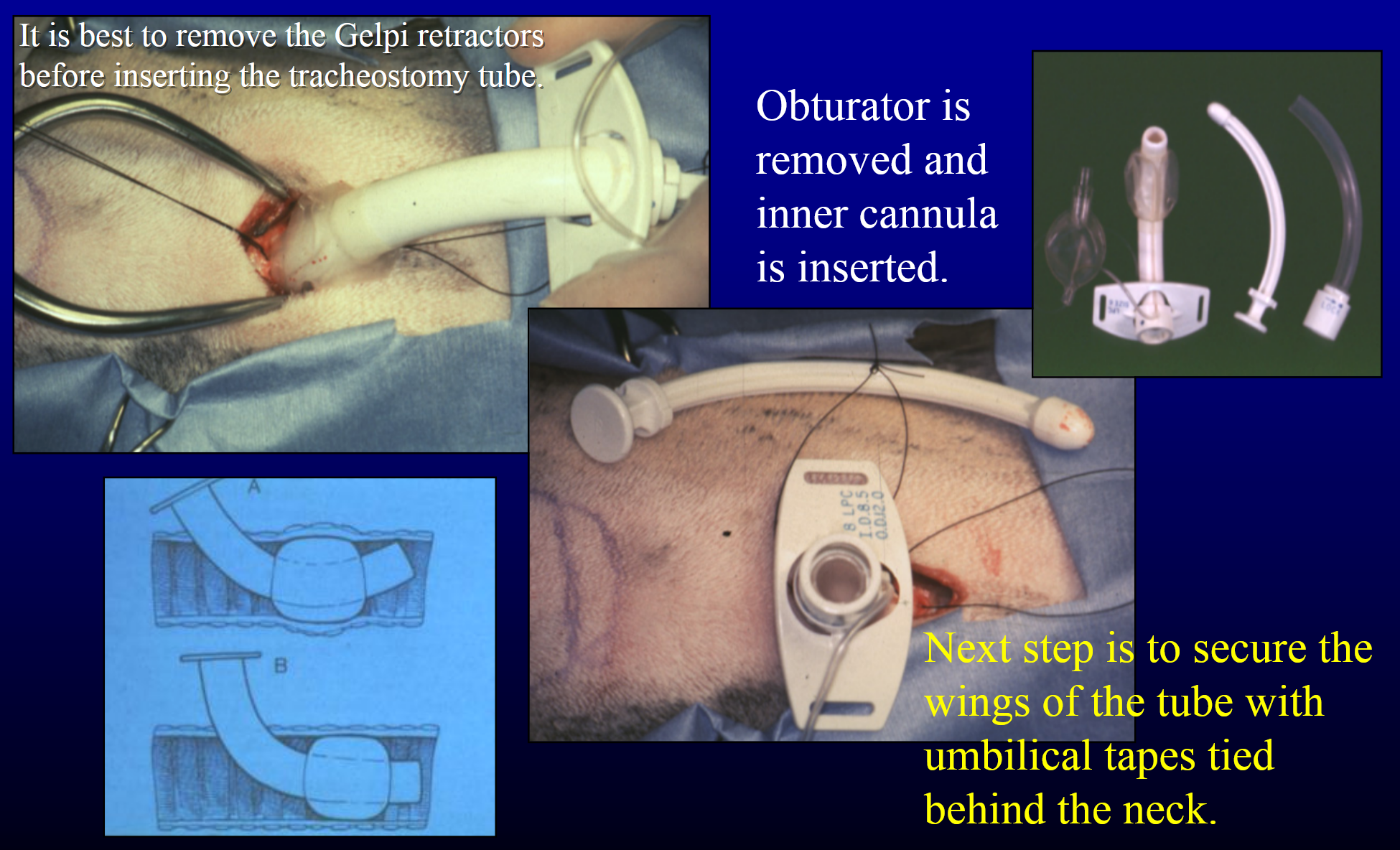
tube tracheostomy surgical technique
ventral midline incision from cricoid cartilage to about 3-4 cm caudally
separate sternohyoiedus muscles on midline
transverse interannular incision between tracheal rings 2 and 3
knotted stay sutures around rings 2 and 3
insert and secure tube with umbilical tapes tied behind the neck
tube tracheostomy skin incision
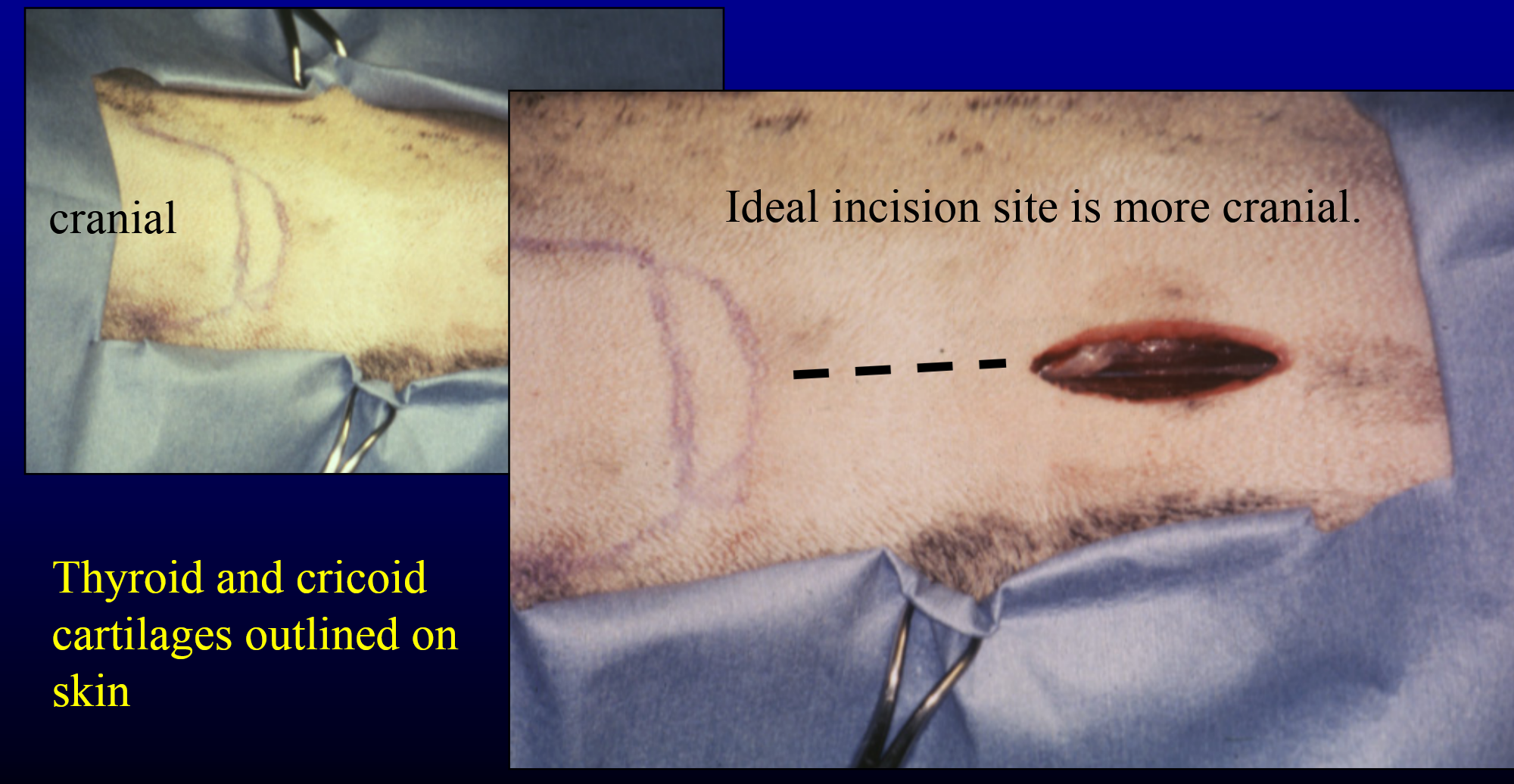
interannular incision
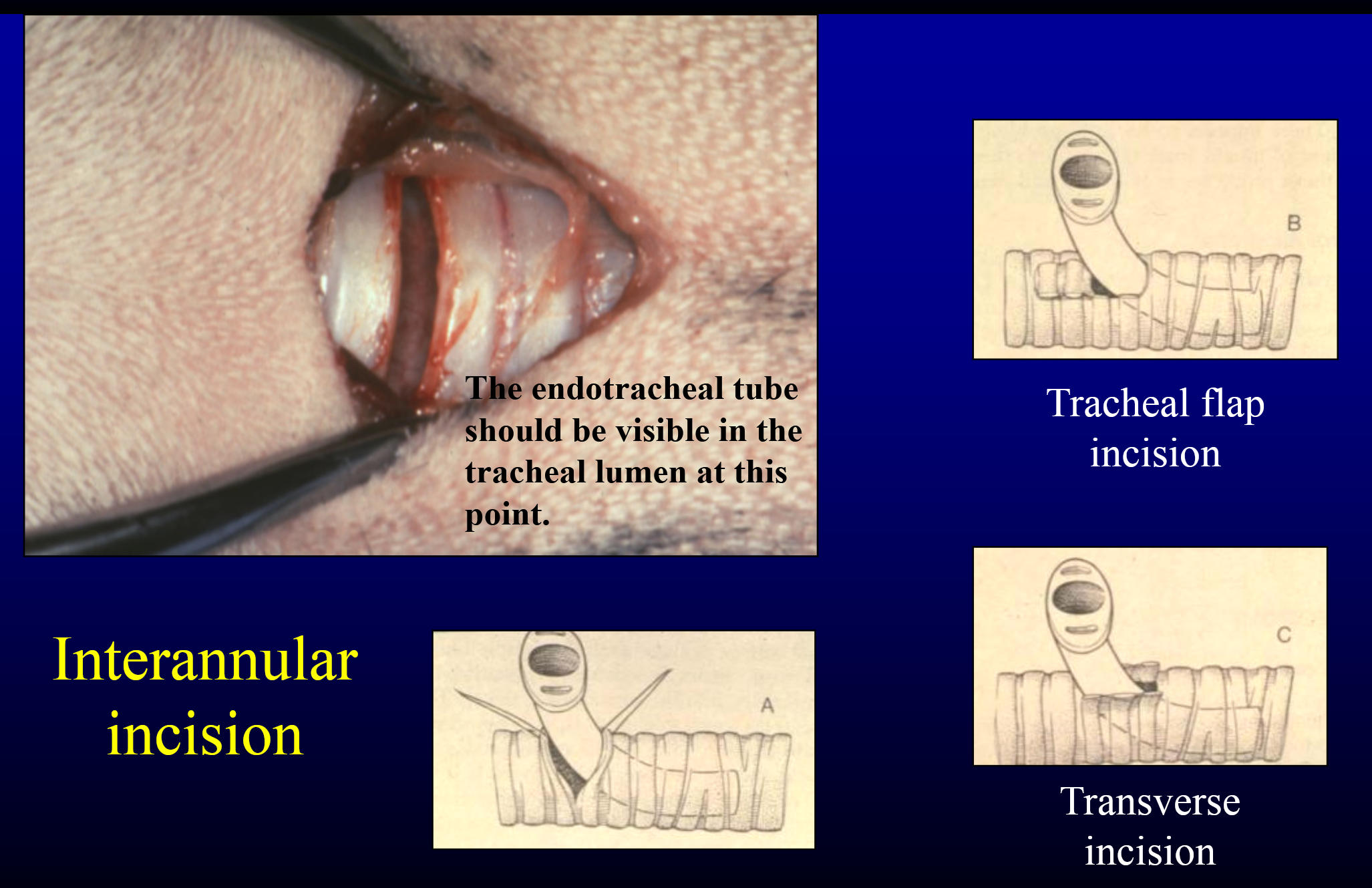
introduction of tracheostomy tube with aid of stay sutures
what are the 3 main tracheostomy tube care?
humidification = humified air and saline injection
frequent aseptic cleaning = q 1hr, sanitize materials (chlorhexidine), gloves, sterile supplies as much as is practical
airway suctioning = avoid mucosal injury
how is a tracheostomy tube removed?
removal after effective breathing around tube
allow wound to heal by second intention
what are the indications for permanent tracheostomy?
salvage procedure
untreatable upper airway obstruction
upper airway treatment failure
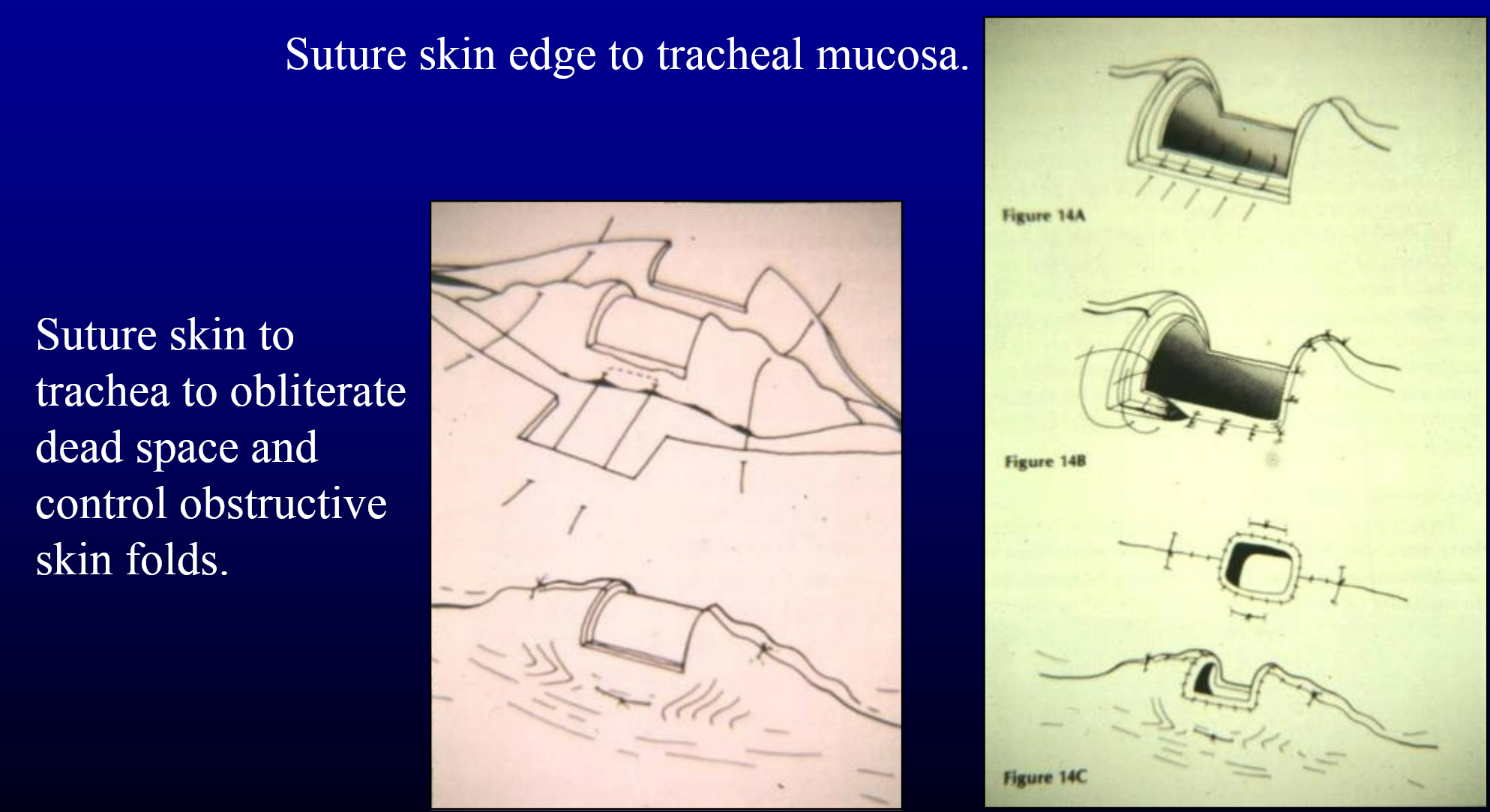
what is the surgical technique of permanent tracheostomy?
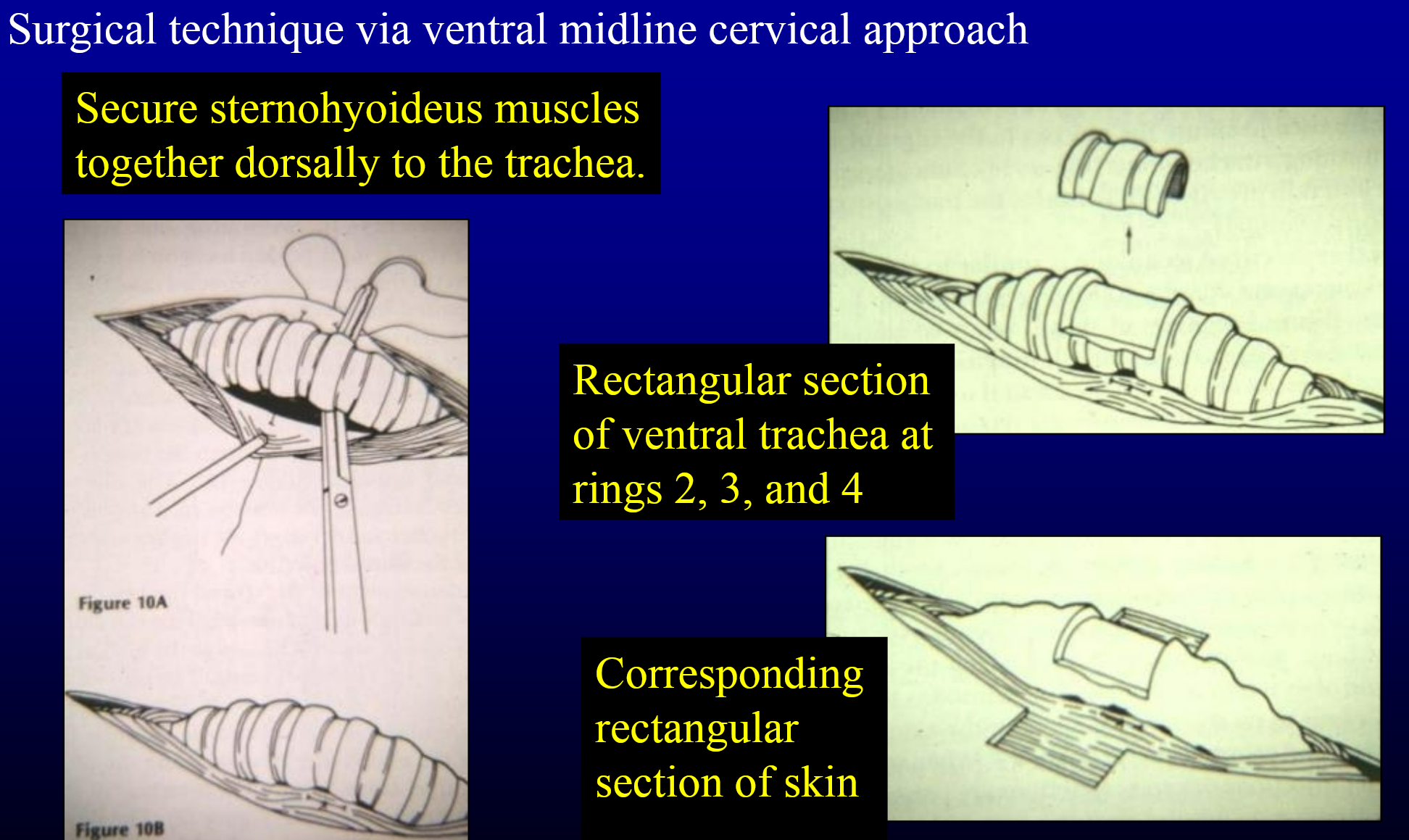
permanent tracheostomy suturing stoma
what is an alternative location for permanent tracheostomy?
cricotracheostomy
what is the long term care of a permanent tracheostomy?
maintenance of opening → clipping hair as needed
no swimming
protection from foreign bodies → plant material
can be surgically reversed if warranted → incise skin-mucosa junction and suture skin edges
what are the surgical conditions of the lungs?
pulmonary cyst
pulmonary bullae/blebs
pulmonary abscess
restrictive pleuritis
bronchiectasis
bronchial foreign bodies
lung laceration
lung lobe torsion
pulmonary neoplasia
what are pulmonary cysts, bullae, and blebs?
congential or acquired
may contain fluid or air
cysts are lined with
epithelium
what might cause spontaneous (idiopathic) pneumothorax?
bullae and bleds and a median sternotomy recommended
what is a bulla?
deep in lung, sometimes requiring attentive palpation to locate
what is a bleb?
located peripherally in the lung and is easily seen

what are pulmonary abscesses?
uncommon
can cause chronic debilitating disease
rupture could result in pneumothorax or pyothorax
what are pulmonary abscesses secondary to?
foreign body obstruction or migration
chronic lung infection
neoplastic disease
what is the medical treatment for pulmonary abscesses?
appropriate antibiotic therapy
pleural drainage if pyothorax
what is the surgical treatment of pulmonary abscesses?
if medical management ineffective
exploratory thoracotomy and (partial) lung lobectomy
what is restrictive pleuritis?
heavy fibrin deposition after trauma or inflammation of the pleura
sequela to chylothorax
restricts lung expansion
what is the surgical treatment of restrictive pleuritis?
lung decortication
poor results
bronchiectasis
congenital or acquired dilation of bronchi and bronchioles
contributes to recurrent respiratory infections
what is the surgical treatmnent for bronchiectasis?
lobectomy of affected lung lobes if only one or two lobes are involved
what might bronchial foreign bodies require?
may require lung lobectomy if foreign body cannot be removed endoscopically or if it migrates through lung
lung lacerations are usually
small and resolves spontaneously with aid of thoracic drainage
what are the causes of lung lacerations?
iatrogenic
thoracocentesis
thoracostomy tube
inadvertent cur during thoracotomy
rib fractures
penetrating trauma → often fatal
what are the indications for lung laceration surgical treatment?
uncontrollable or unresolving penumothorax
ongoing intrathoracic hemorrhage > 2ml/kg/hr
what are the techniques for surgical treatment for lung lacerations?
continuous inverting suture pattern → lembert
deep hemostatic mattress suture with simple continuous closure of laceration
partial or complete lobectomy
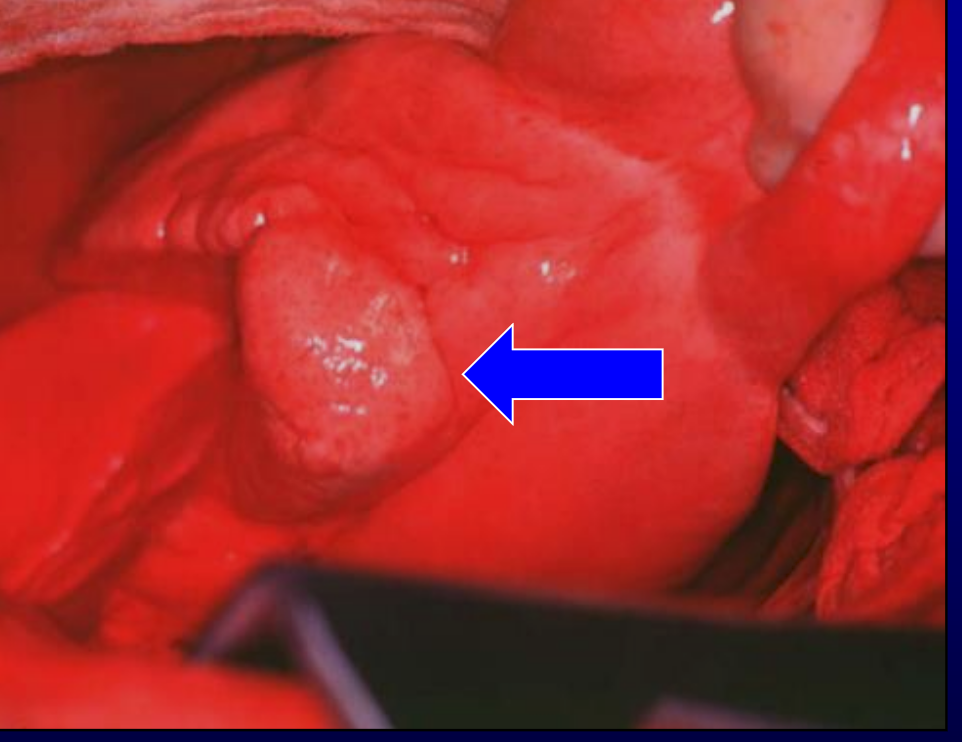
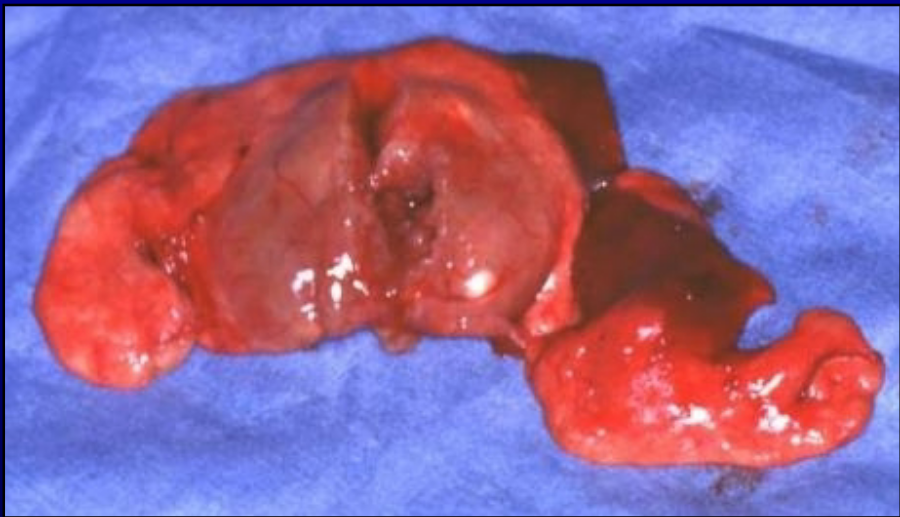
lung lobe torsion
uncommon
deep, narrow-chested dogs
right middle lobe most common → followed by right cranial and left cranial
congested, consolidated lobe
pleural effusion → serosanguinous or chylous
what is the treatment of a lung lobe torsion?
lobectomy → do not untwist
what form of pulmonary neoplasia is most common?
metastatic
T/F some survival benefit to pulmonary metastsectomy in dogs with less than 3 pulmonary metastatic osteosarcoma lesions
true
what is the most common primary pulmonary neoplasia?
pulmonary adenocarcinoma → sometimes amenable to excision
surgical lung biopsy is essentially the same as what?
partial lung lobectomy
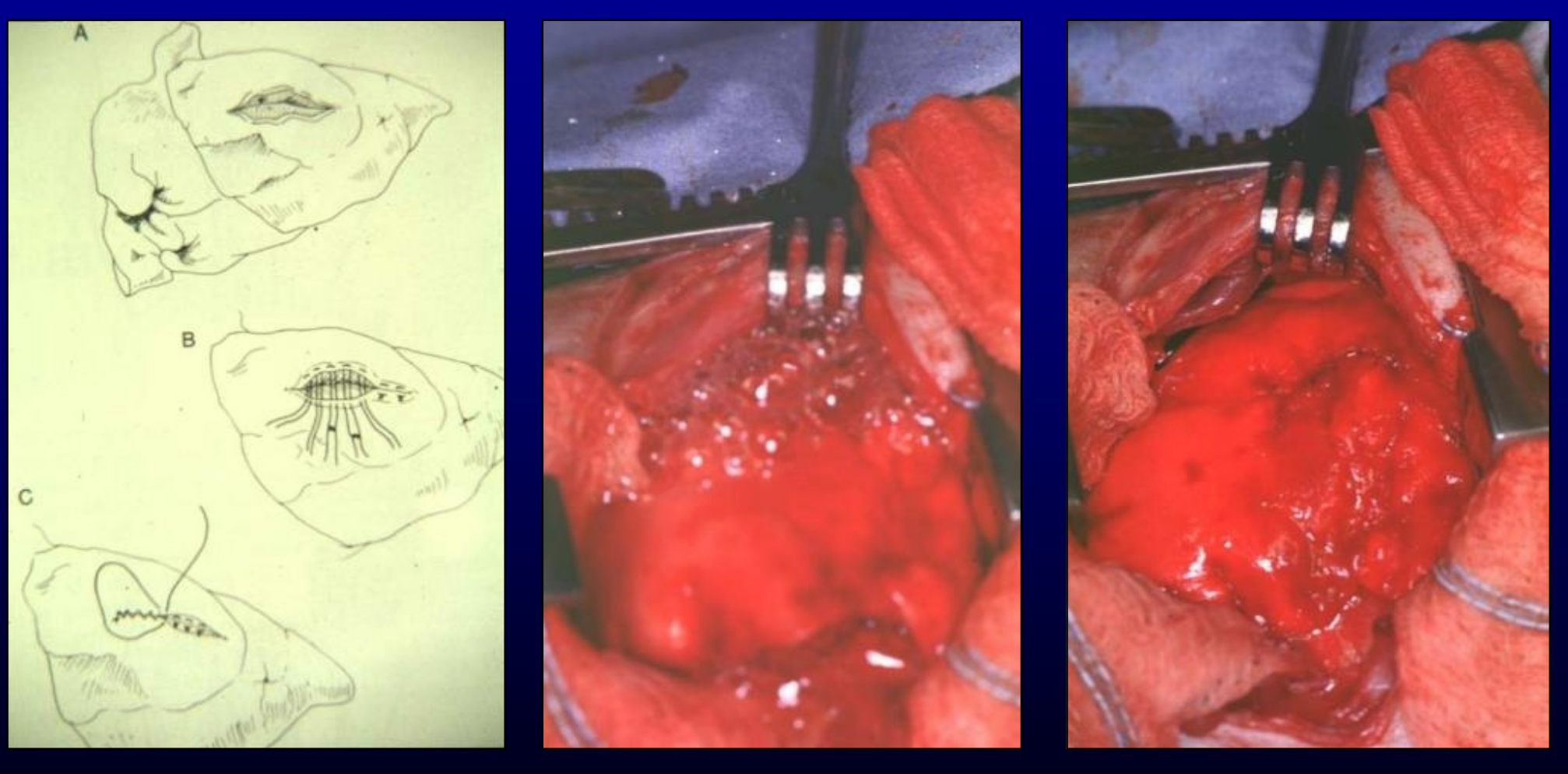
how is a partial lung lobectomy with sutures performed?
1) clamps proximal to lesions
2) continuous horizontal mattress pattern proximal to clamps
3) incision between clamps and horizontal mattress, or between clamps and lesion as illustrated
4) simple continuous oversew of incised edge
how is a complete pulmonary lobectomy performed?
dissect hilus to identify pulmonary artery, bronchus. and pulmonary
ligate/divide artery, then vein, then bronchus
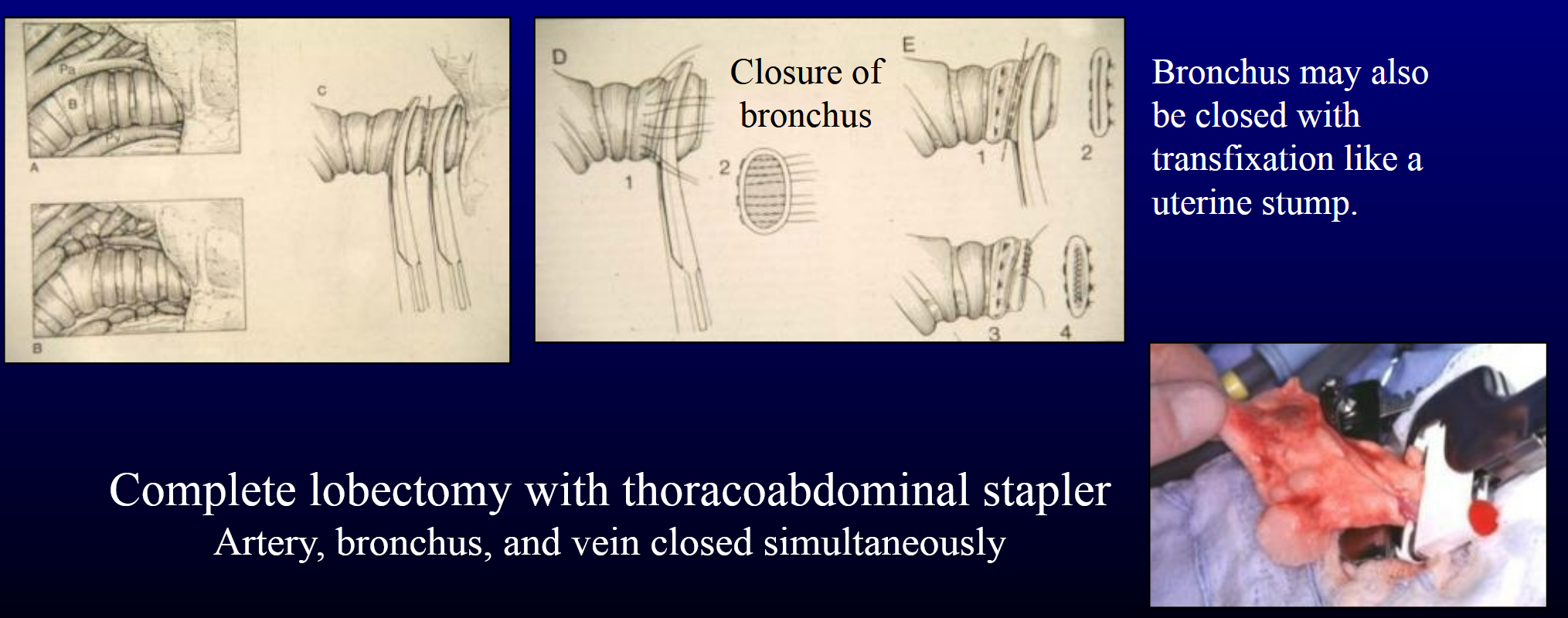
pneumonectomy
excision of entire lung on one side of thorax
can remove 50% of lung acutely → probably more if non-diseased lung already compensanting
technique similar to complete lobectomy → multuple lobectomies on one side
what are the indications for thoracostomy tube?
postoperative throacotomy → manage residual air and fluid
management of pneumothorax
management of pleural effusions
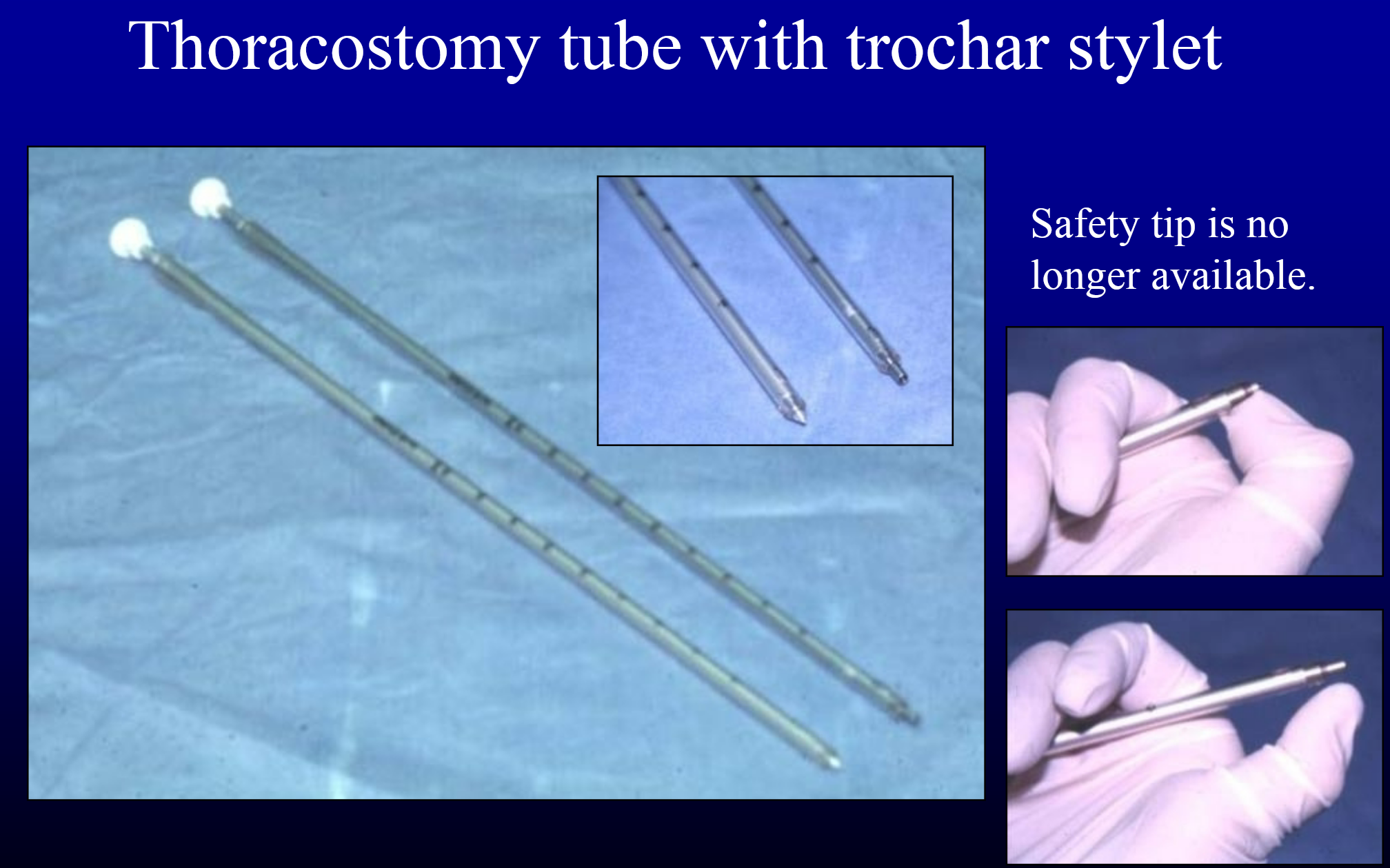
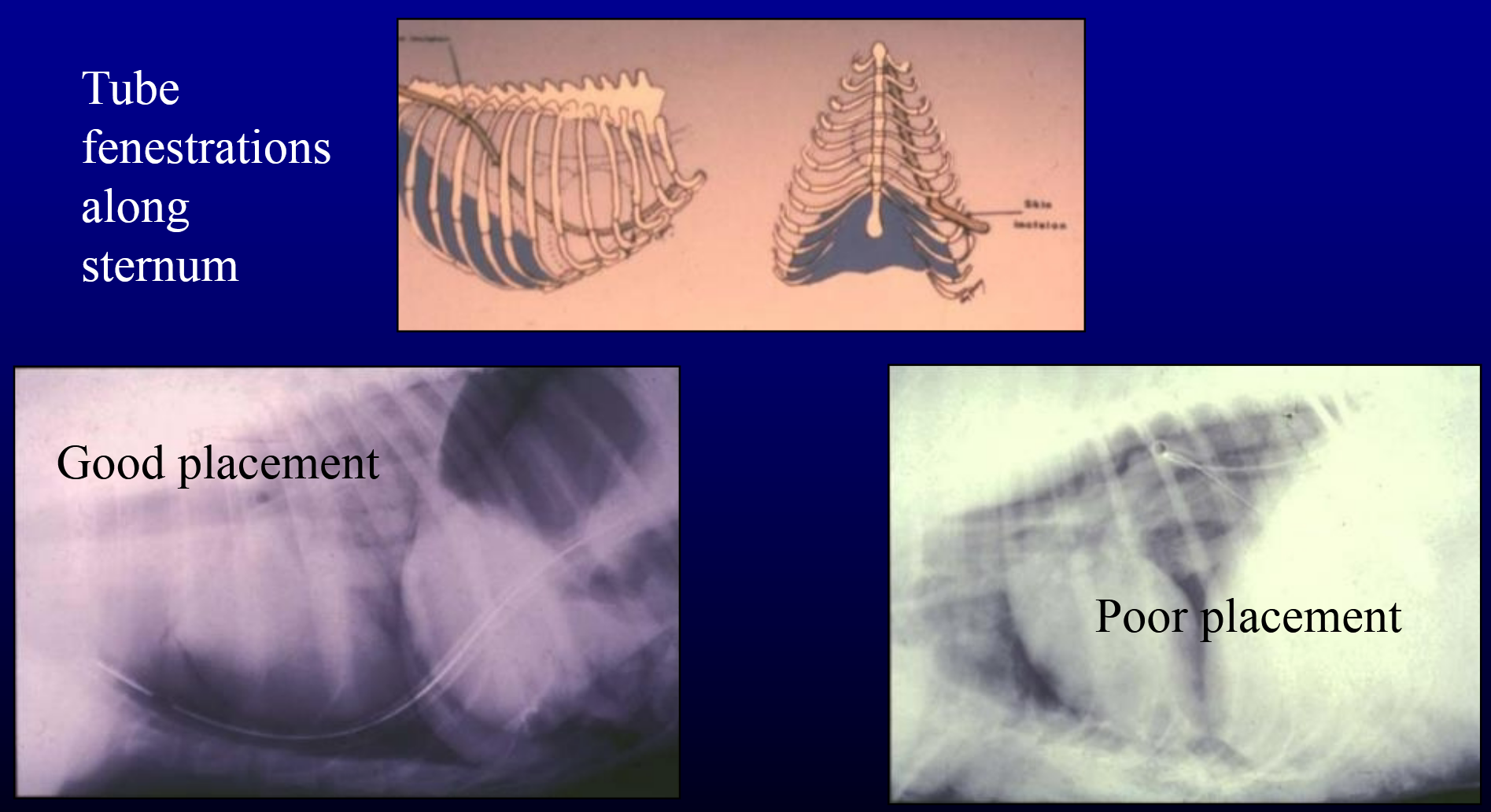
thoracostomy tube placement closed thorax
special tube with trochar stylet → alternative = tube tip in tips of hemostatic forceps
stab skin incision (as small as possible) → doral 1/3 of lateral thorax near 10th to 12th ICS
sub-latissimal tunnel → cranioventrally to 7th or 8th ICS at mid-thorax
controlled “thrust” into thorax → or puncture ICS with forceps before introducing tube
thoracostomy tube placement open thorax
placed at time of thoraotomy closure of thorax
trochar-type not necessary
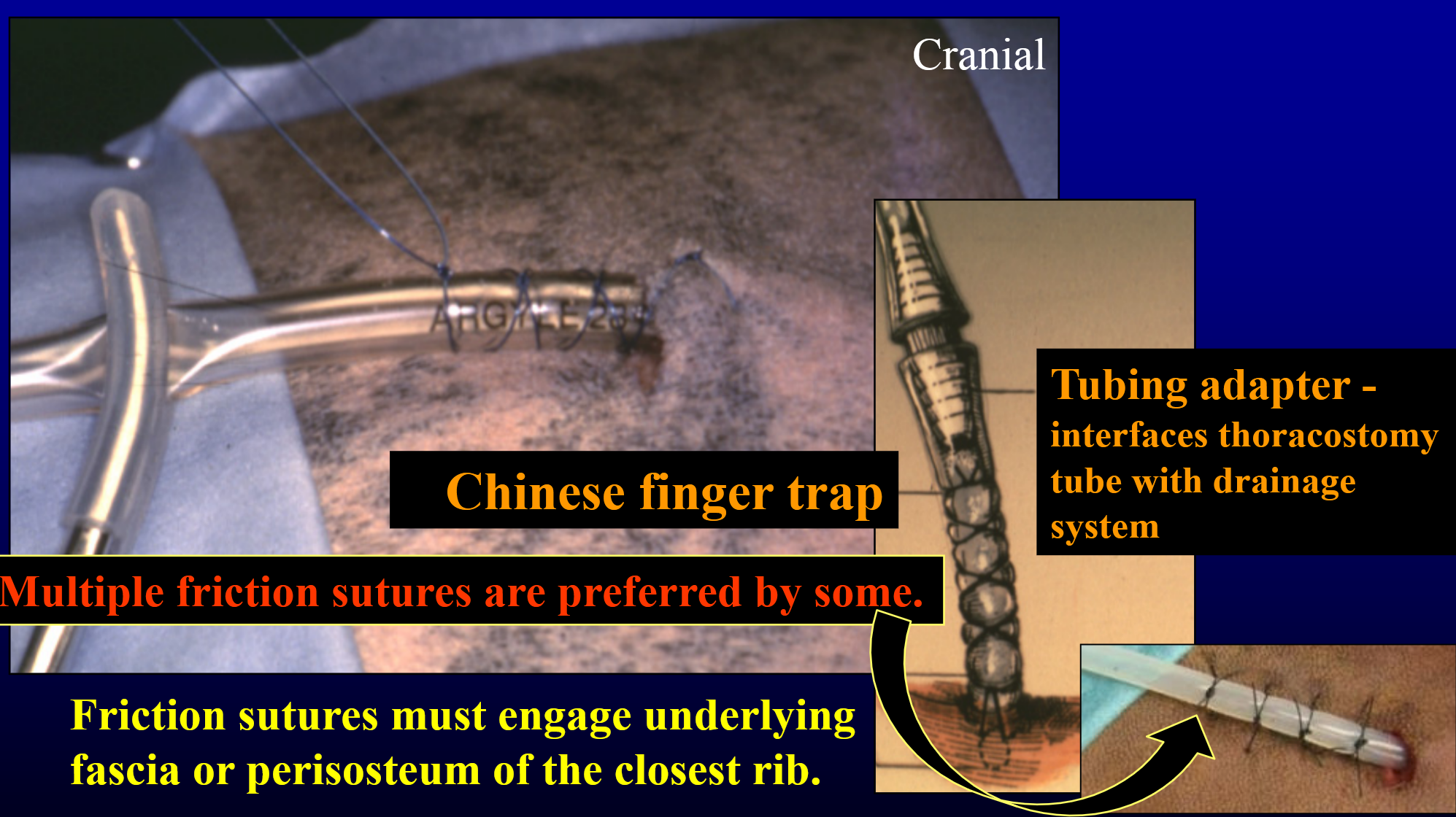
thoracostomy tube optimal placement
thoracostomy tube → securing the tube
what are the surgical approaches to the pleural space?
intercostal thoracotomy
rib osteotomy thoracotomy
rib pivot thoractomy
rib resection thoractomy
transternal thoracotomy
median sternotomy (or paramedian sternotomy)
transdiaphragmatic approach
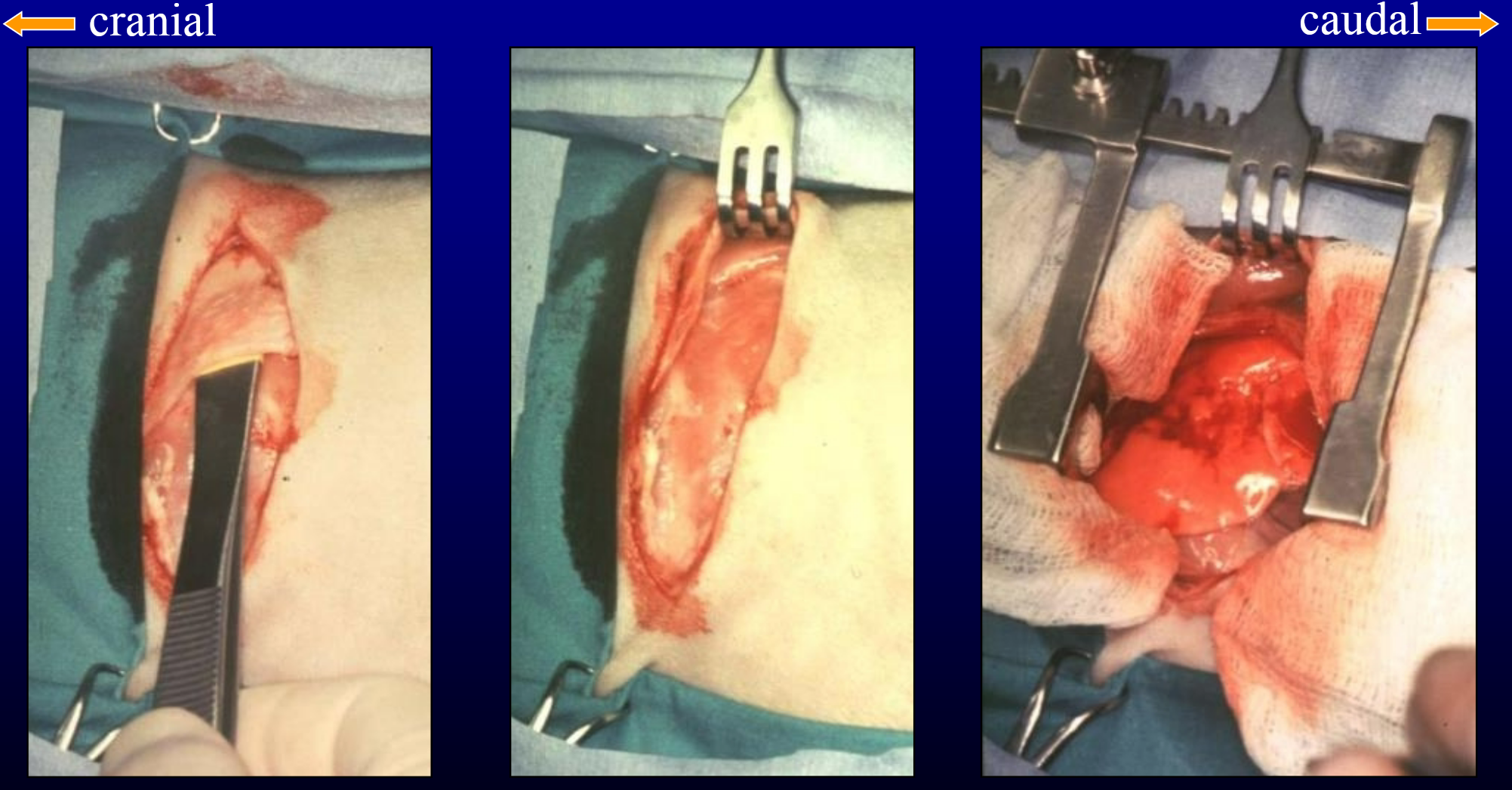
intercostal thoracotomy
preferred surgical approach because of simplicity
left or right, 3rd to 10th ICS
limited access → appropriate approach when surgically correctable abnormality is localized and defined
postoperative morbidity (lameness) can be minimized by retraction (rather than incision) of the latissimus dorsi muscle
left 4th ICS thoracotomy → latissimus dorsi muscle retraction
methods to increase exposure for intercostal thoracotomy
rib osteotomy
rib pivot
rib resection