NPB 101: Cardiovascular Physiology I
1/90
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
Three principle components that make up the circulatory system
heart (the pump)
blood vessels (pipes)
blood (fluid to be moved)
What is the circulatory system function impacted by?
endocrine system
nervous system
kidneys
Circulatory system functions
supply oxygen and nutrients
remove wastes
temperature regulation
distribute hormones
immuno-vigilance
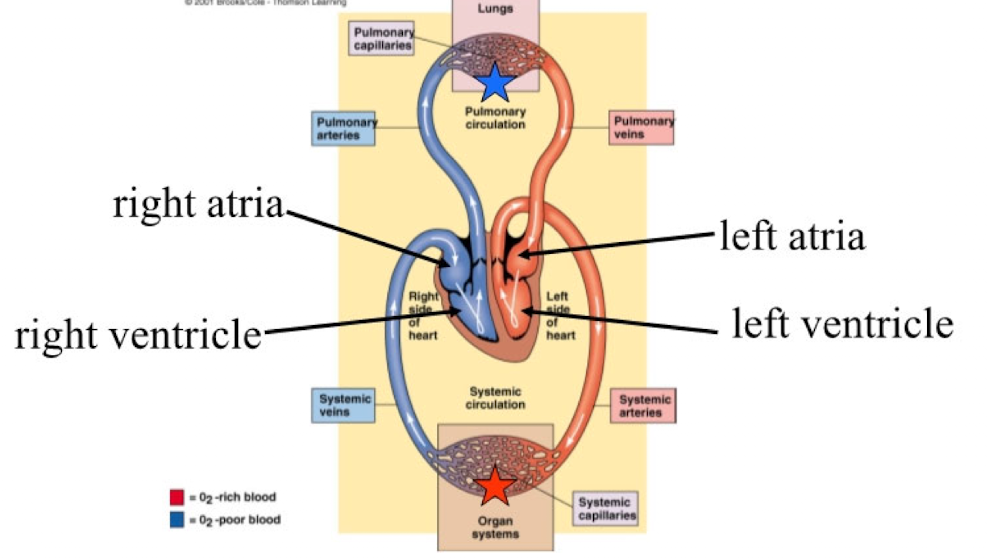
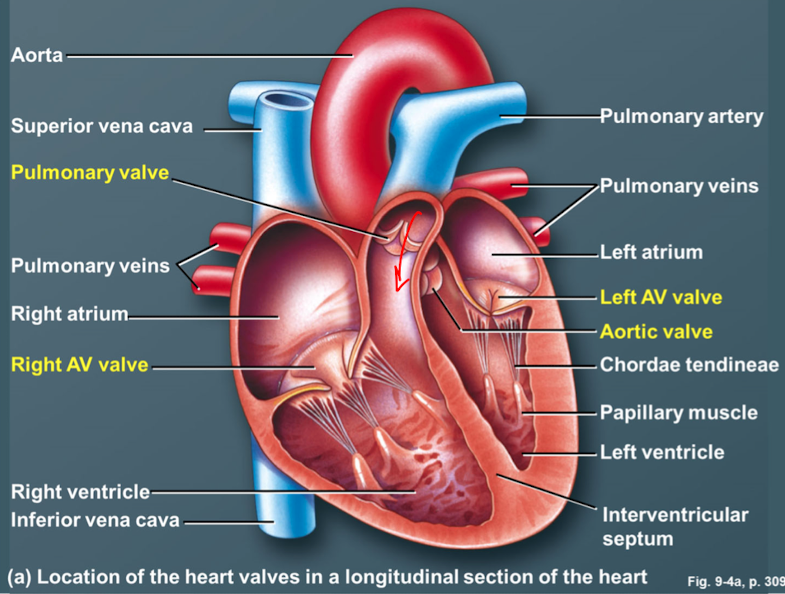
dual-pump system 4 chambers
left and right atria
pump oxygen-poor blood through the pulmonary circulation of the lungs
left and right ventricles
pump oxygen-rich blood through the systemic circulation to the body tissues
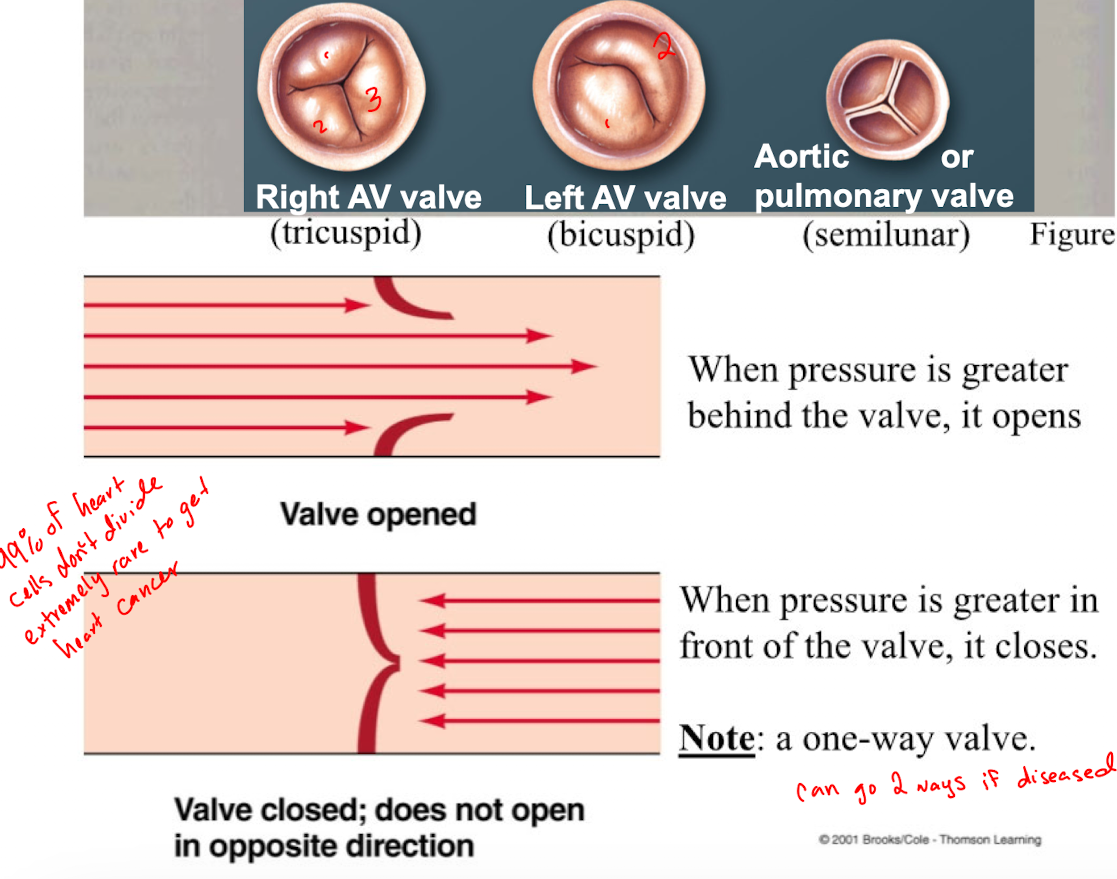
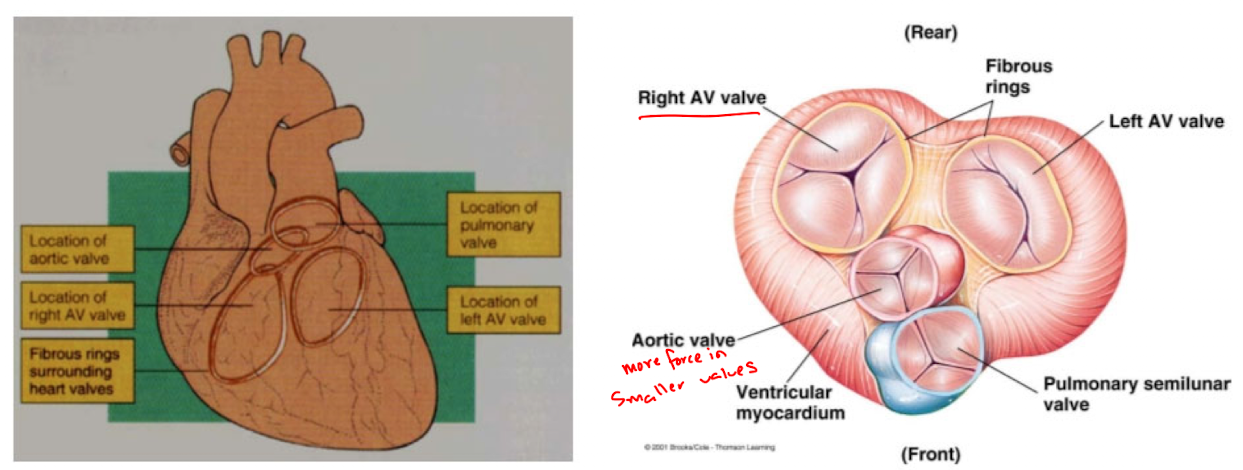
4 heart valves
right AV valve/tricuspid (r.a. → r.v.)
pulmonary/semilunar valve (r.v. → pulmonary artery)
left AV valve/ bicuspid/mitral (l.a. → l.v.)
aortic/semilunar valve (l.v. → aorta)
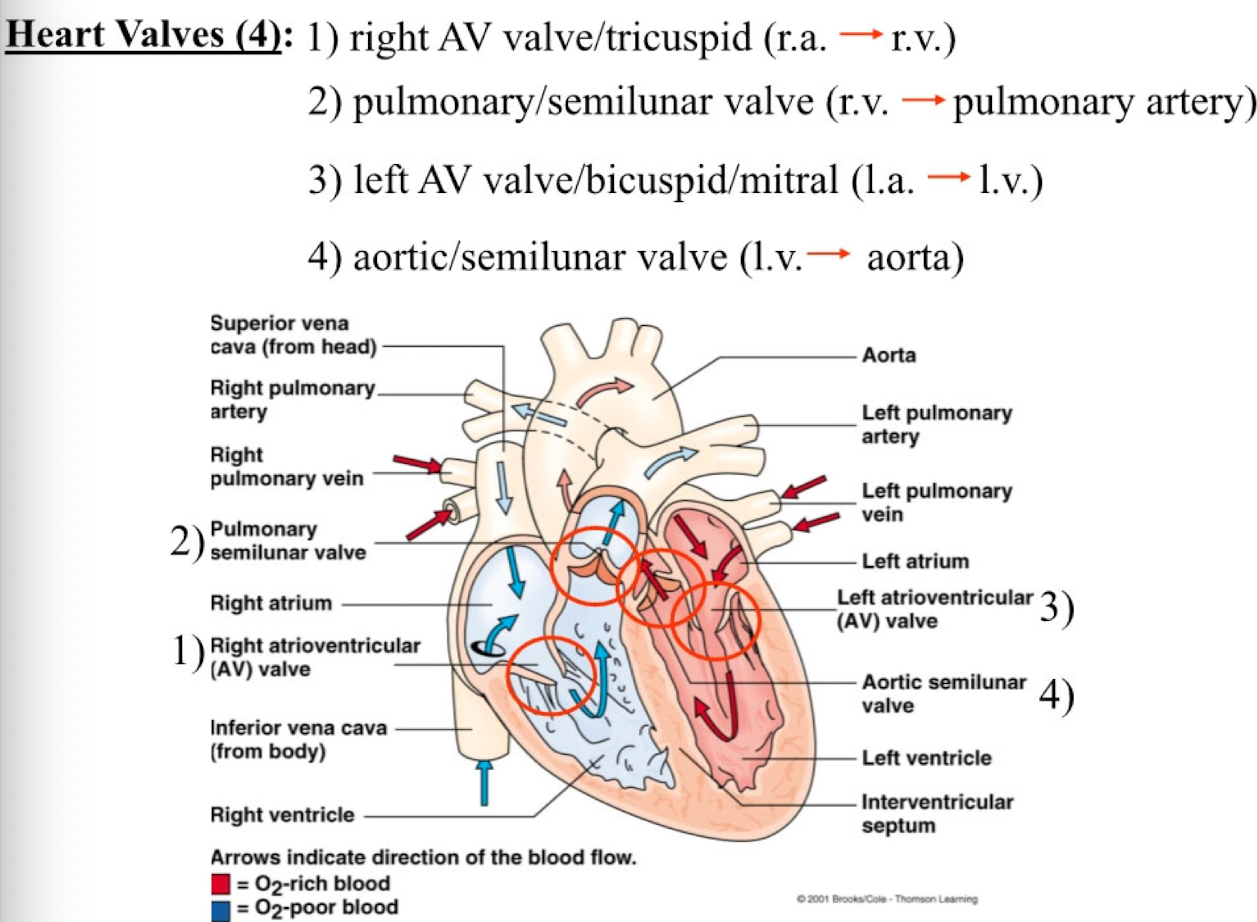
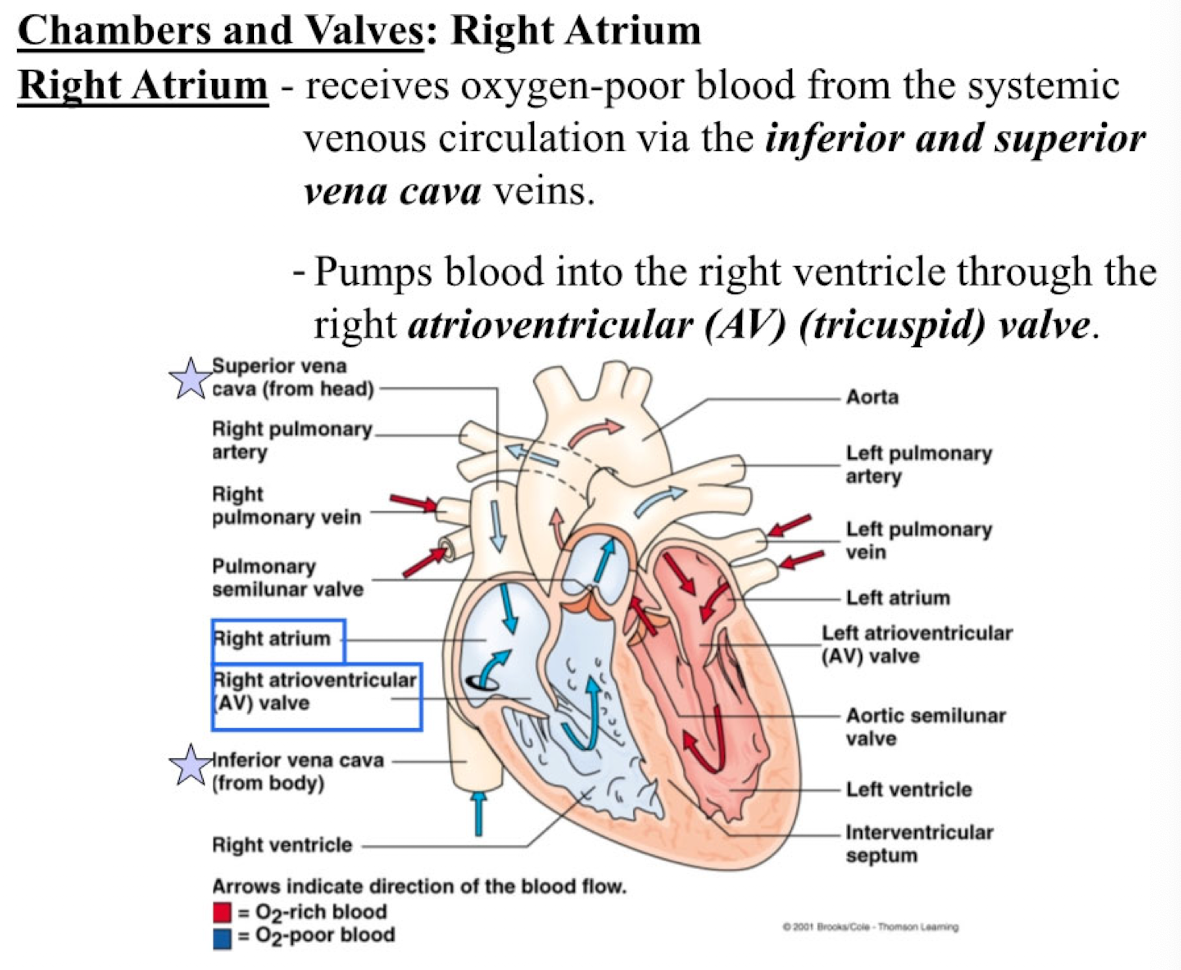
Right Atrium
receives oxygen-poor blood from the systemic venous circulation via the inferior and superior vena cava veins
pumps blood into the right ventricle through the right atrioventricular (AV) (tricuspid) valve
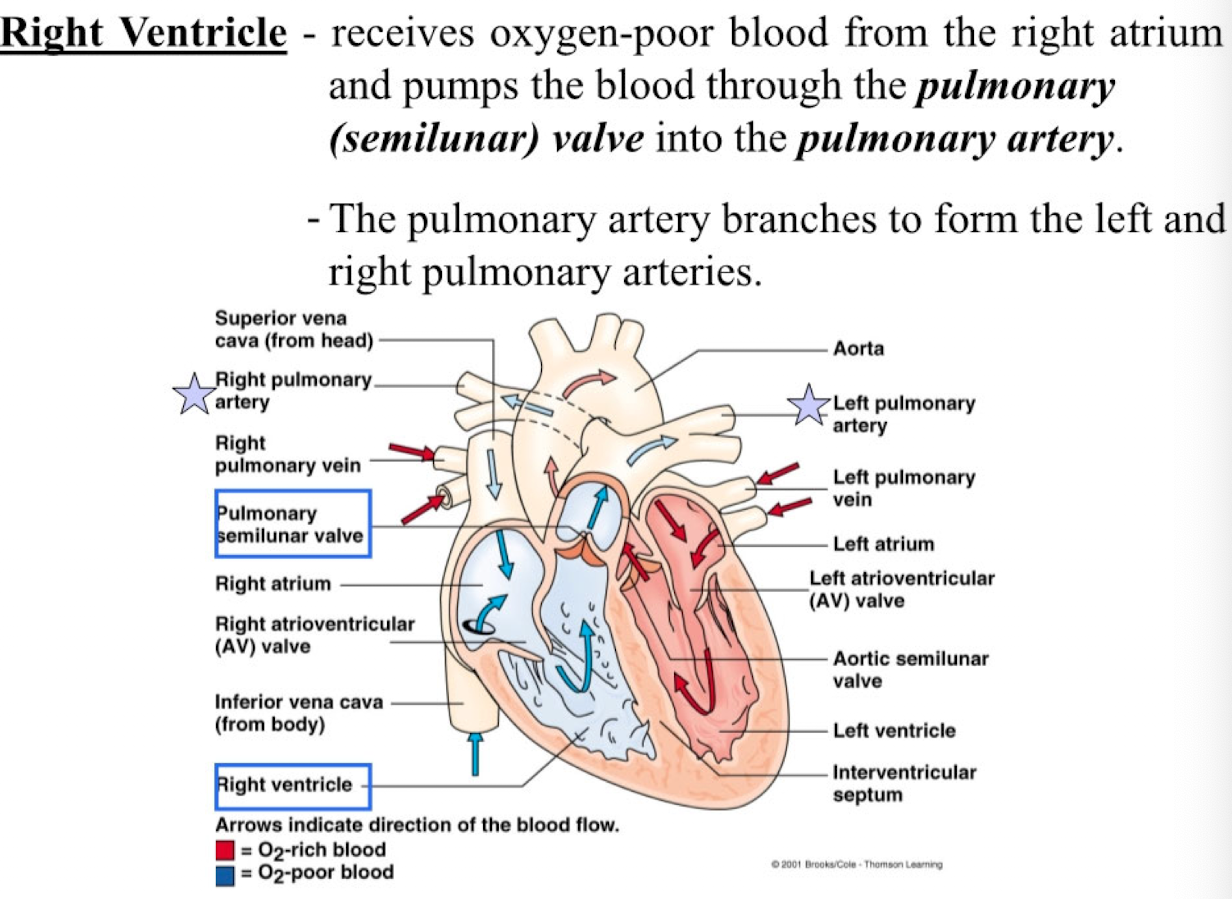
Right Ventricle
receives oxygen-poor blood from the right atrium and pumps the blood through the pulmonary (semilunar) valve into the pulmonary artery
the pulmonary artery branches to form the left and right pulmonary arteries
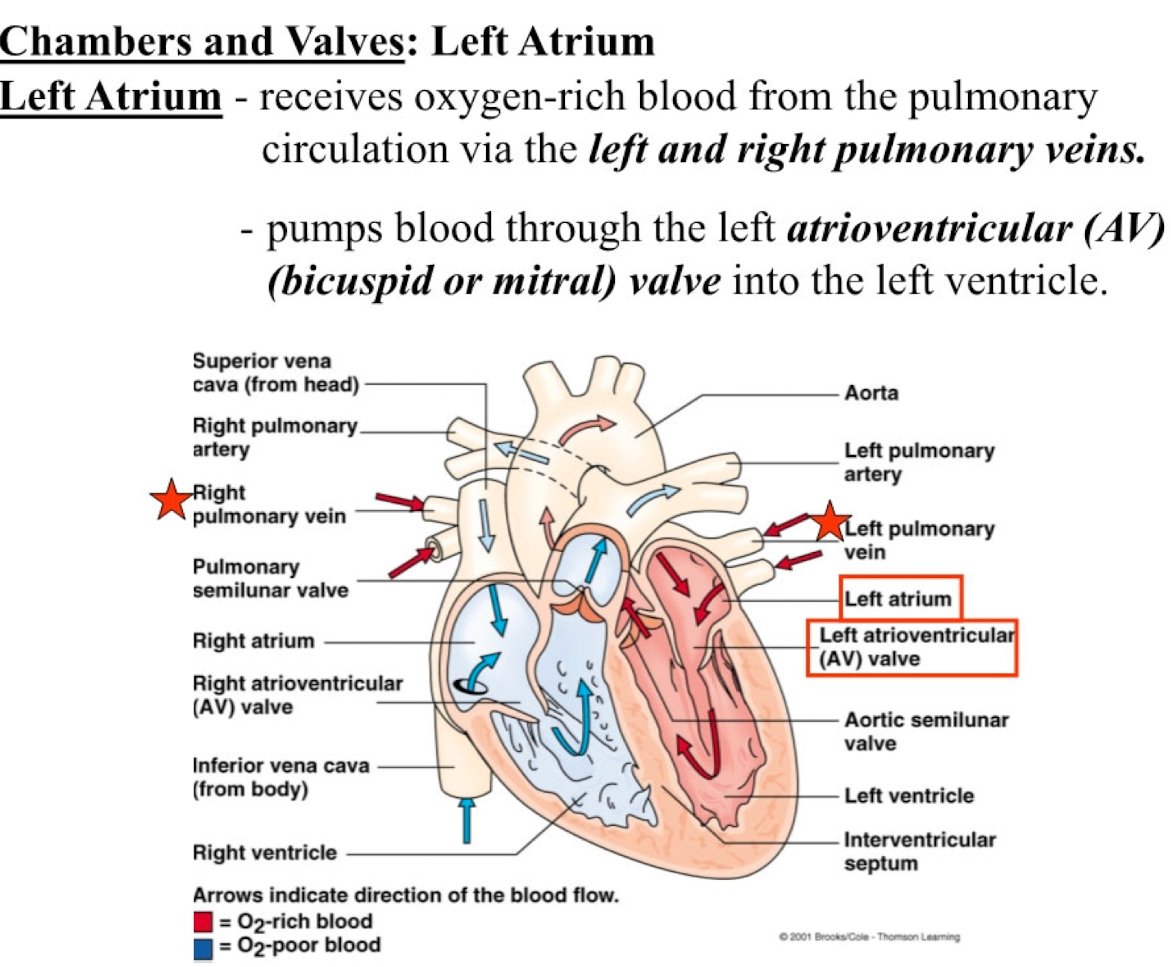
Left atrium
receives oxygen-rich blood from the pulmonary circulation via the left and right pulmonary veins
pumps blood through the left atrioventricular (AV) (bicuspid or mitral) valve into the left ventricle
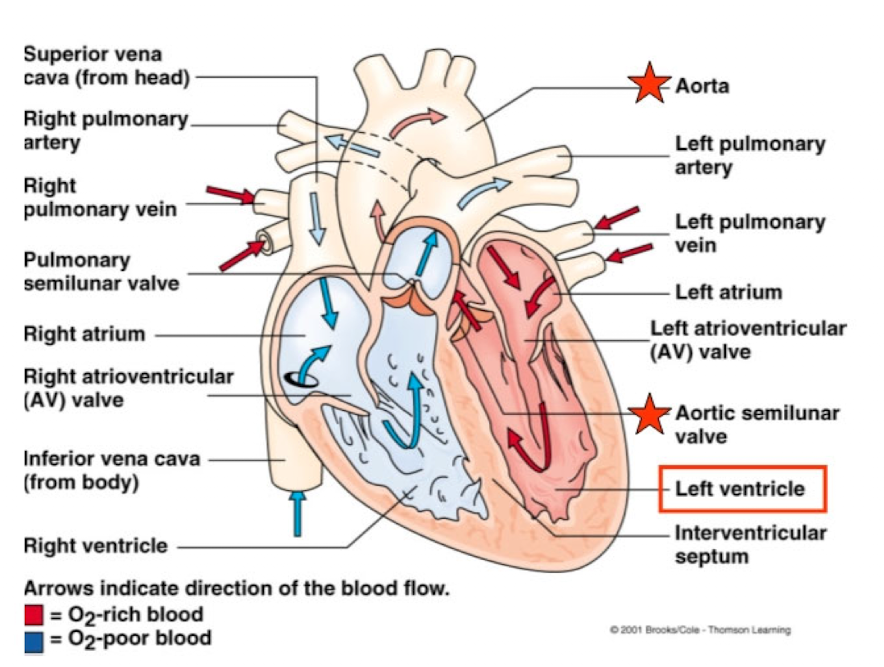
Left Ventricle
receives oxygen-rich blood from the left atrium and pumps this blood through the aortic (semilunar) valve into the aorta
Heart-Valve
ensure a one-way flow of blood
when pressure is greater behind the valve, it opens
When pressure is greater in front of the valve, it closes
Chordae Tendineae
tendons fibers attached to the inside edges of the AV valves and the interior base of the ventricles via papillary muscles
prevent the AV valves form everting during the pressure wave that occurs during ventricular contraction
There are ___ valves in the heart
4
Which one of these is NOT the name of a heart valve:
prolapse
T/F: Heart valve disease occurs only in those who are born with defects in their heart valves
False. Heart valve disease can be a product of age-related changes, infection, or other cardiovascular problems
Connective Tissue
Separates the atria from the ventricles and provides a rigid base for attachment of the heart valves and the cardiac muscle
A ring of dense fibrous connective tissue surrounds each other the valves of the heart
Name 3 heart walls
endocardium
myocardium
epicardium
Endocardium
thin layer of endothelial tissue lining the interior of each chamber
Myocardium and intercalated disks
middle layer of the heart wall, composed of cardiac muscle
connected end-to-end by intercalated disks where 2 types of contacts are formed: desmosomes and gap-junctions
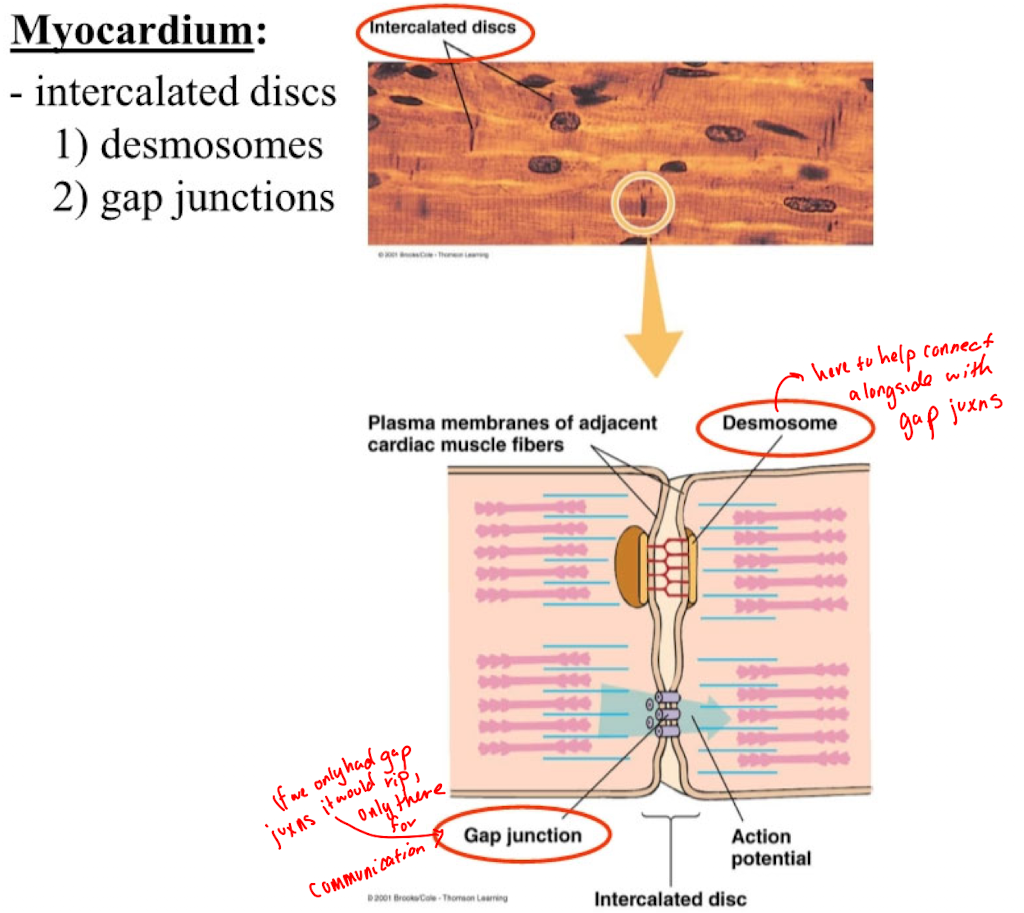
Desmosomes function in myocardium
mechanically hold the cells together
Gap junctions function in myocardium
provide paths of low resistance to the flow of electrical current between muscle cells
enable cardiac muscle to form a functional syncytium
Epicardium
thin external membrane covering th heart and is filled with a small volume of pericardial fluid
Autorhythmicity
Heart muscle capable of generating its own rhythmic electrical activity
Autorhythmic cells
initiate and conduct the action potentials that promote muscle contraction (pacemaker cells)
How does autorhythmicity occur?
Due to unique electrophysiological properties of a subset of specialized cardiac muscle cells that generate pacemaker activity
Pacemaker cells are grouped together into specialized regions called nodes that together control the rate and coordination of cardiac contraction
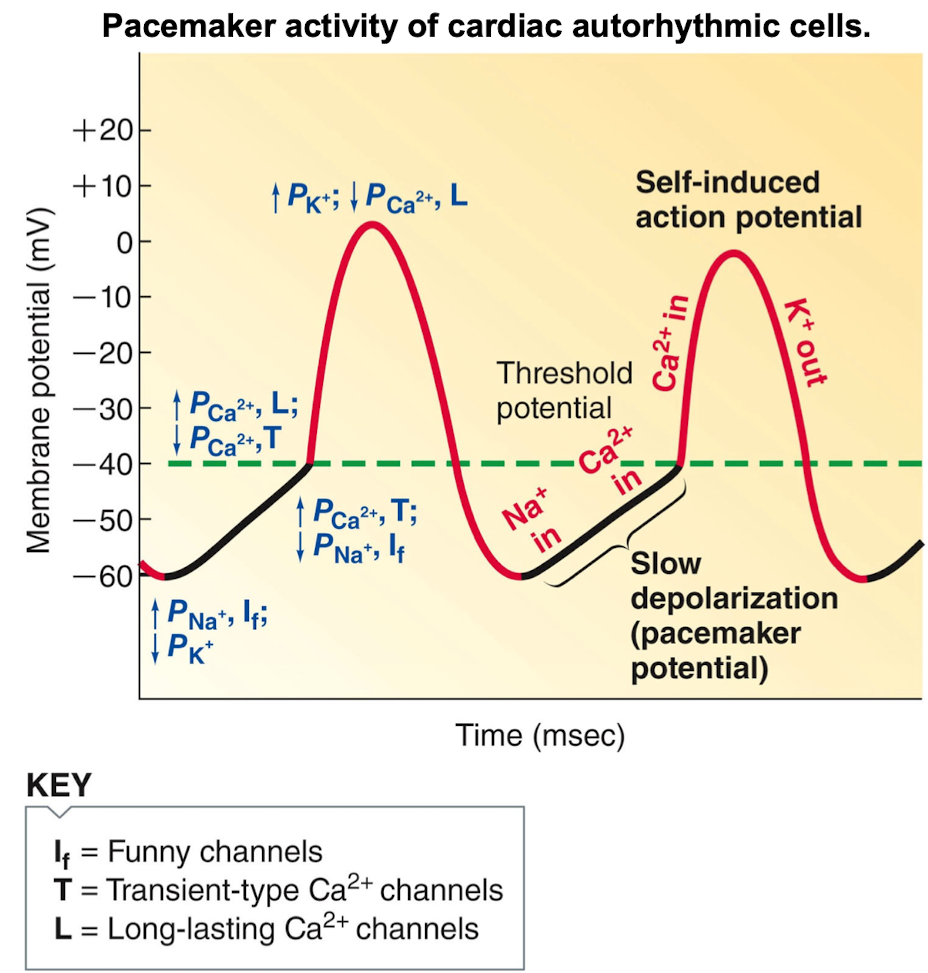
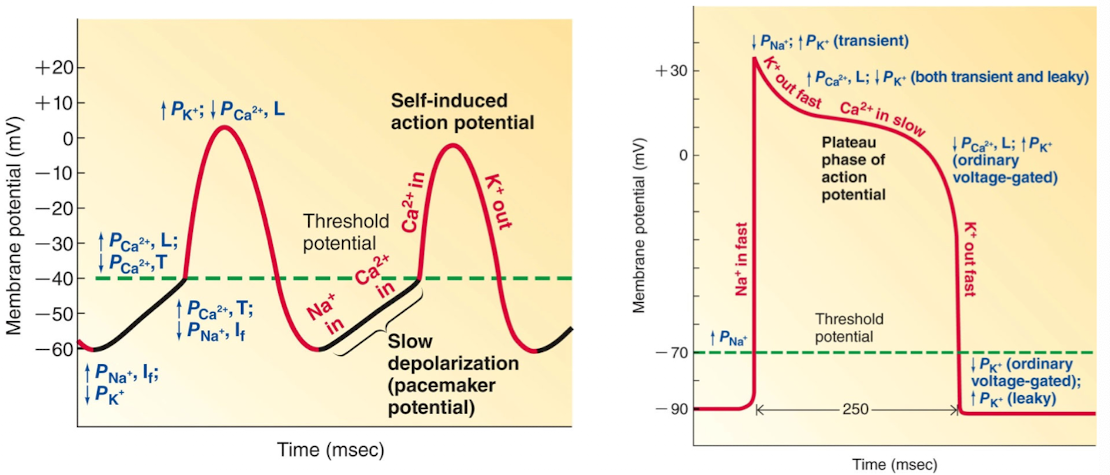
Pacemaker Activity
1% of cells are auto rhythmic and intrinsically initiate their own action potentials at a regular frequency
Controlled by pacemaker potentials
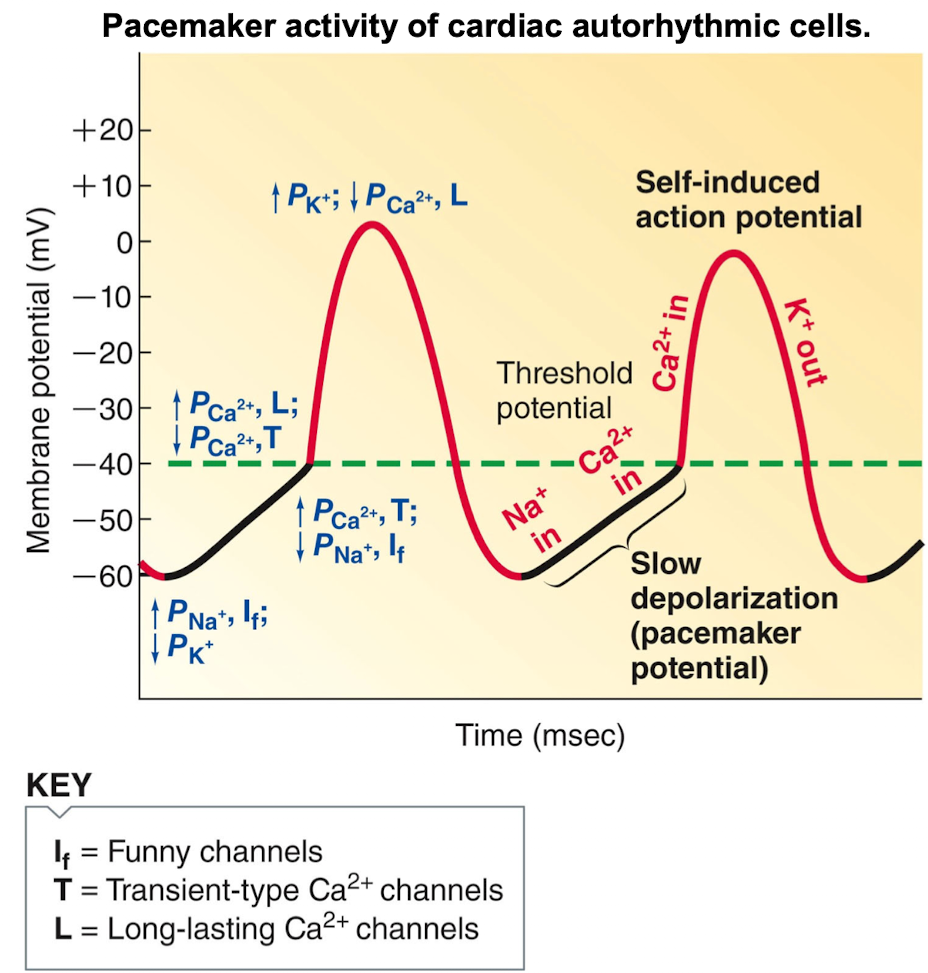
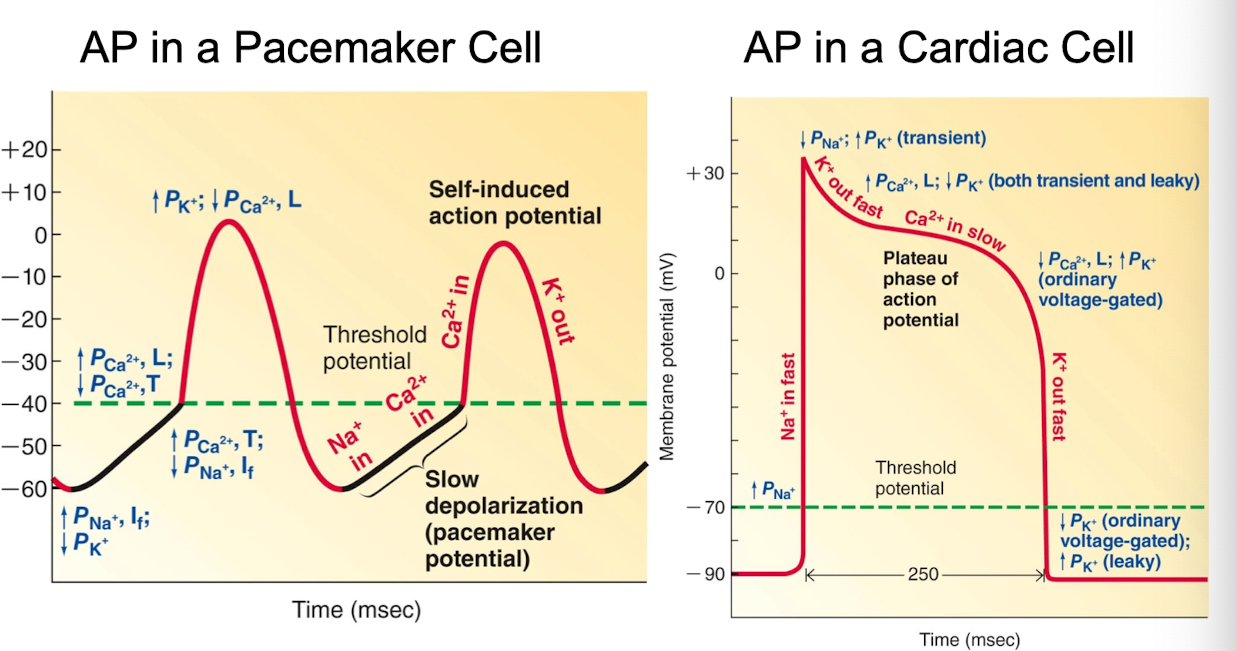
First half of the pacemaker potential is a result of…
simultaneous opening of unique funny channels which permits inward Na+ current, and closure of K+ channels, which reduces outward K+ current
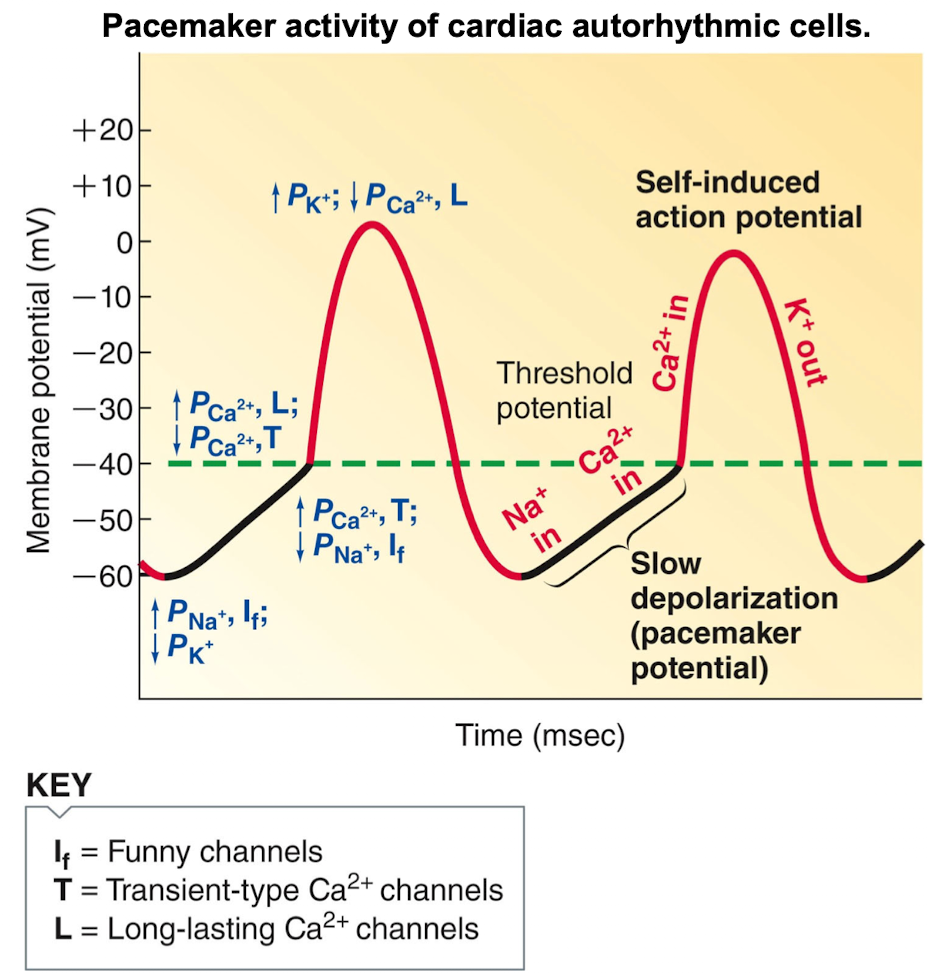
Second half of pacemaker potential is the result of …
opening of T-type (transient type) Ca++ channels
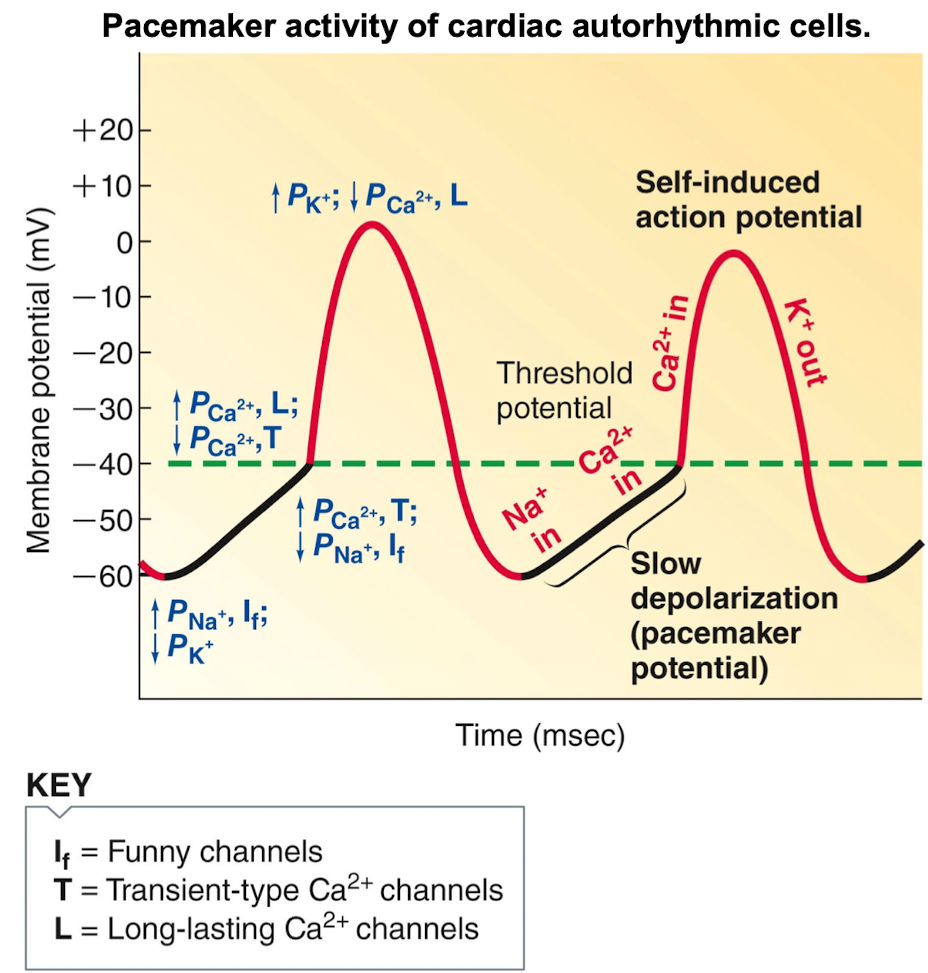
What happens once threshold is reached in pacemaker activity of cardiac autorhythmic cells
the rising phase of the action potential is the result of opening of L-type Ca++ channels, whereas the falling phase is the result of opening go K+ channels
Heart valve disease is often discovered during an exam when…
an echocardiogram is performed
The heart is ___-___, initiating it’s own rhythmic ___.
self-excitable; contractions
Contractile cells
99% of the cardiac muscle cells do the mechanical work of pumping
Nodes
specialized cardiac muscle cells capable of pacemaker activity are grouped together to form them
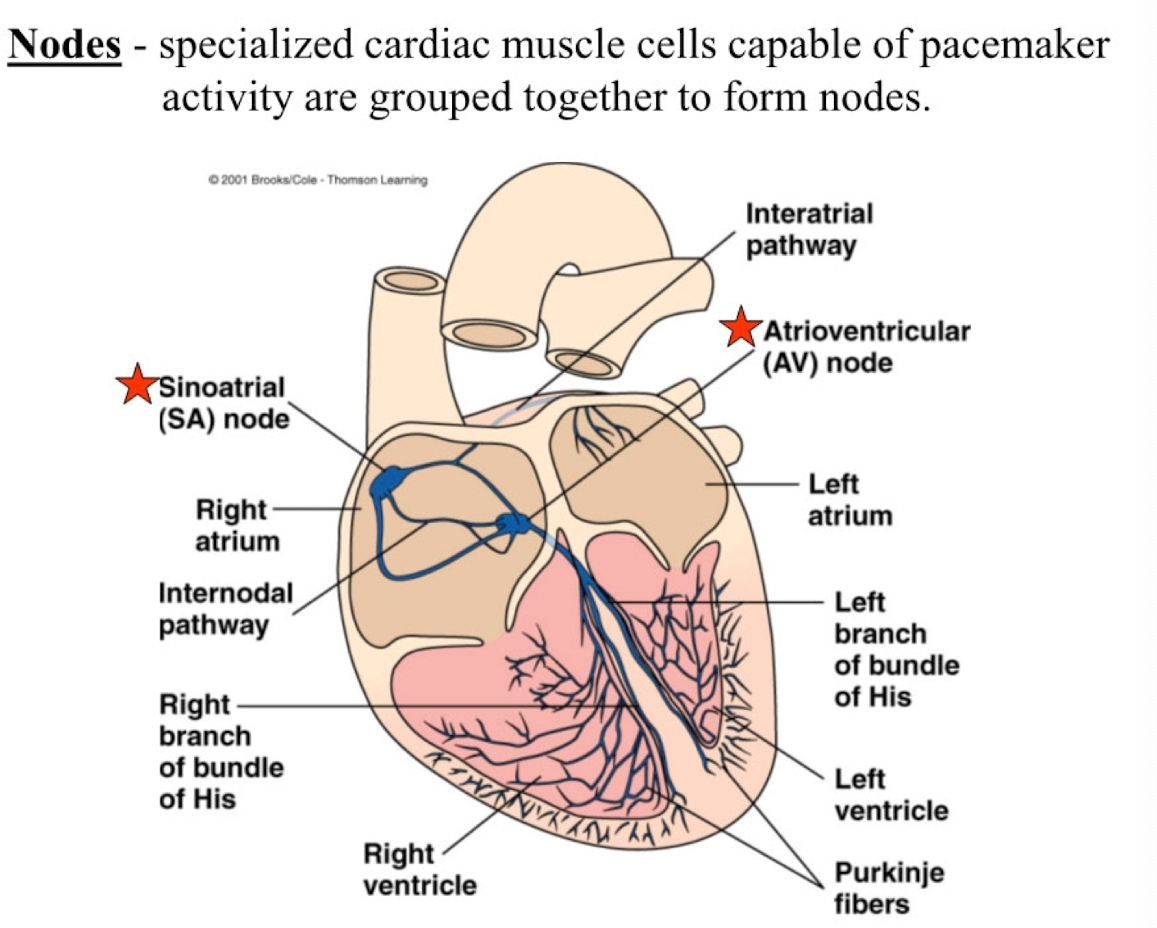
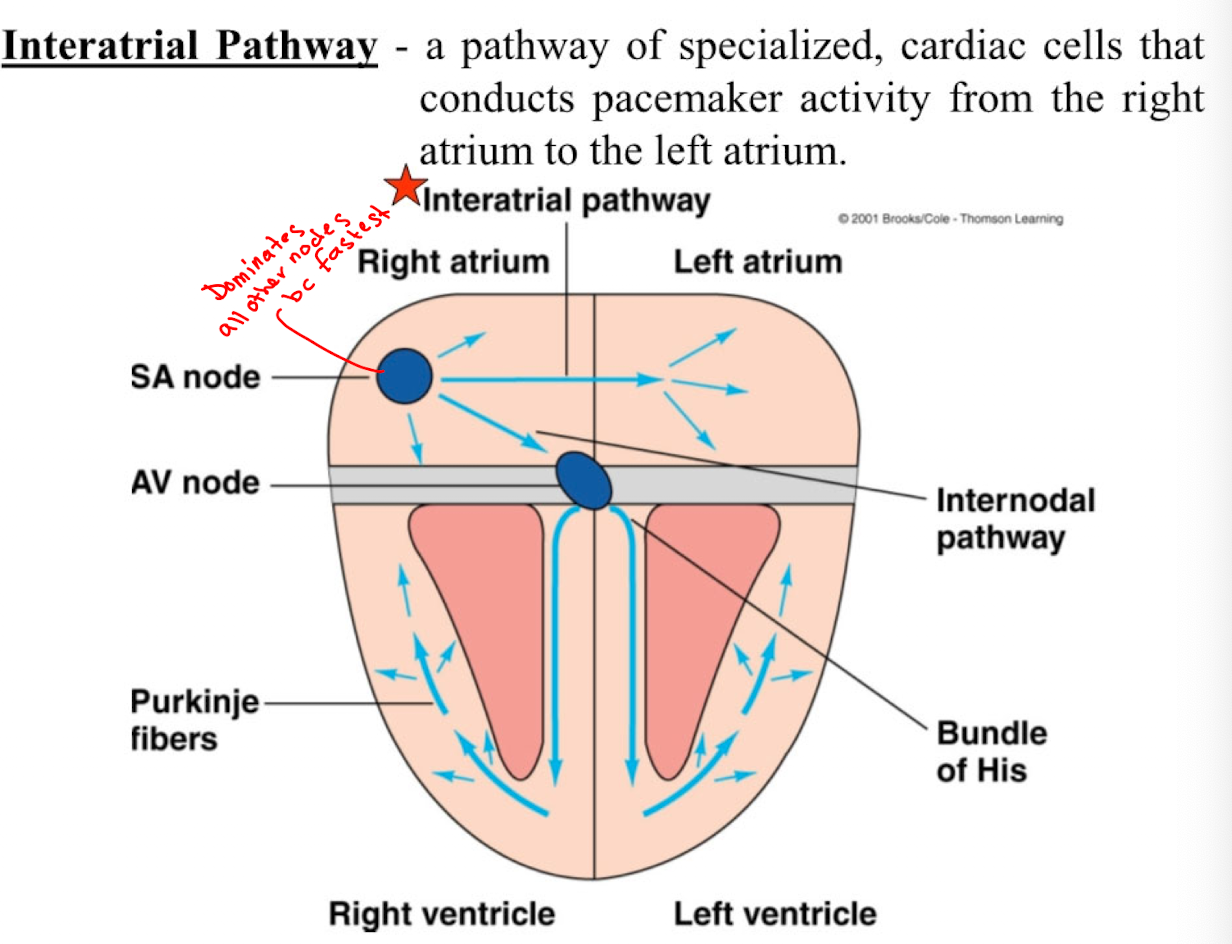
Sinoatrial (SA) Node
bundle of specialized cardiac pacemaker cells located in the wall of the right atrium near the opening of the superior vena cava
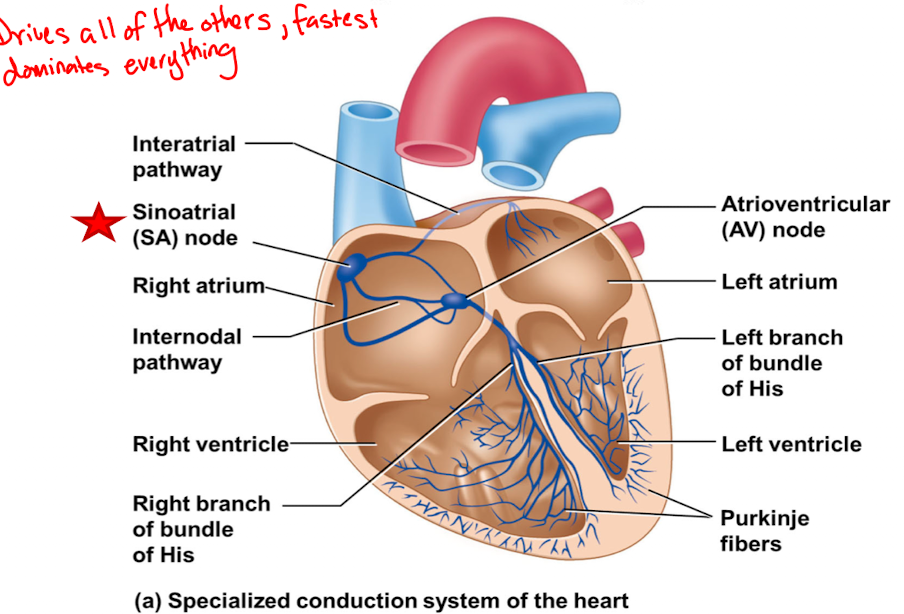
Sinoatrial (SA) Node Autorhythmicity
70 action potentials per minute and leads the activity of the other pacemaker structures in the heart (fastest)
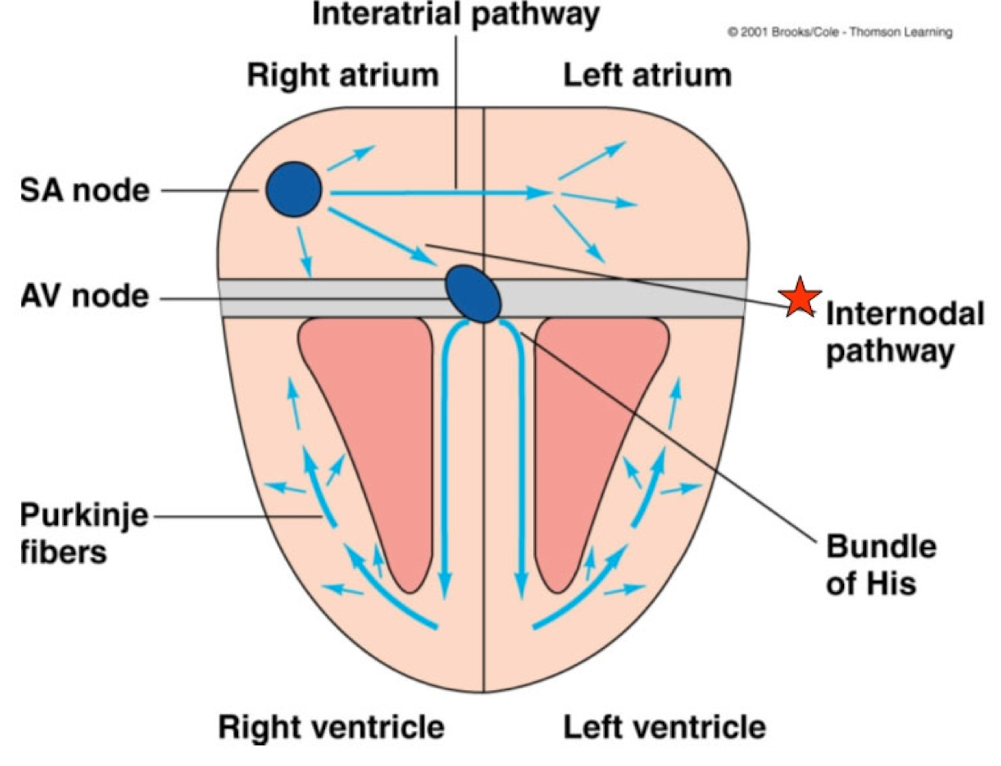
Atrioventricular (AV) Node
Bundle of specialized, cardiac pacemaker cells located at the base of the right atrium
Atrioventricular (AV) Node Autorhythmicity
50 action potentials per minute (with no SA node)
Under normal conditions, node follows faster SA node at 70 action potential per minute
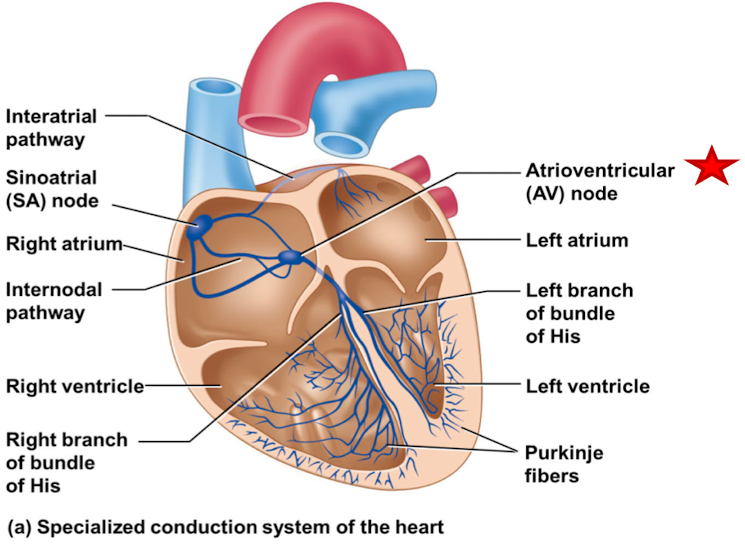
Bundle of His
tract of specialized, cardiac pacemaker cells that originates at the AV node and divides and projects into the left and right ventricles
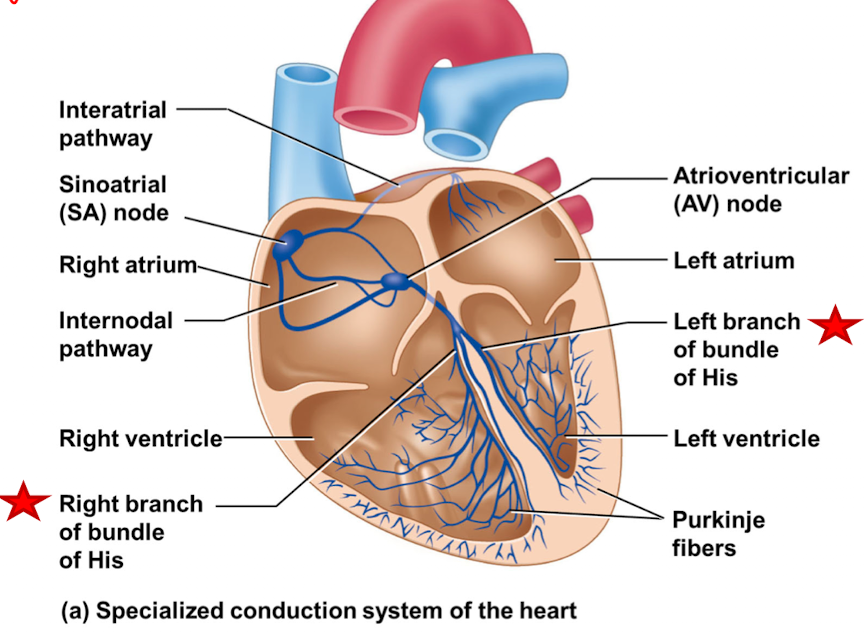
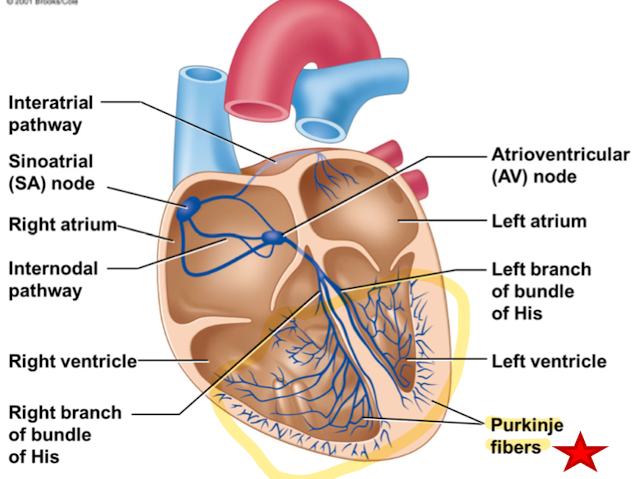
Purkinje Fibers
Small terminal fibers of specialized, cardiac pacemaker cells that extend from the bundle of His and spread throughout the ventricular myocardium
Purkinje Fibers Autorhymicity
30 action potentials per minute
Under normal conditions, they follow faster SA node (and AV node) at 70 action potentials per minute
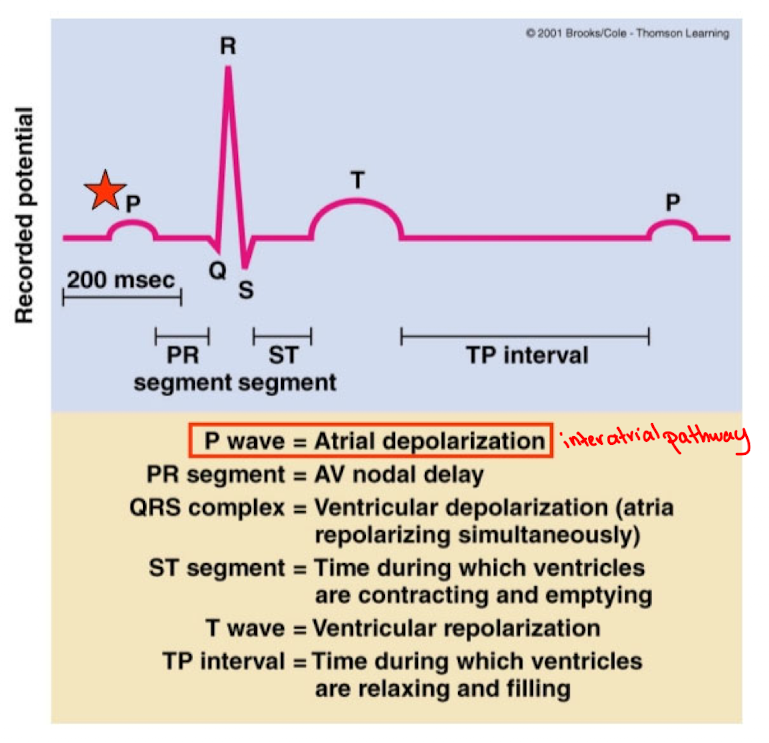
Interatrial Pathway
pathway of specialized, cardiac cells that conducts pacemaker activity from the right atrium to the left atrium
Internodal Pathway
pathway of specialized, cardiac cells that conducts pacemaker activity from the SA node to the AV node
AV Nodal Delay
Pacemaker activity is conducted relatively slowly through the AV node resulting in a delay of approximately 100 nm
Delay ensure ventricles contract after atrial contraction
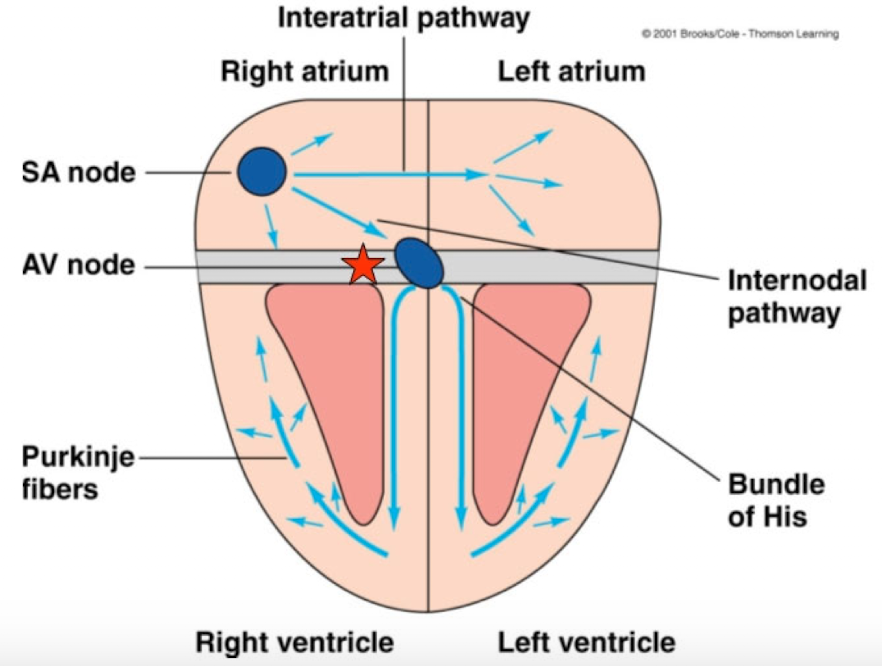
Choose the correct sequence of current flow though the heart wall:
SA node, AV node, AV bundle of His, right and left bundle branches, Purkinje fibers
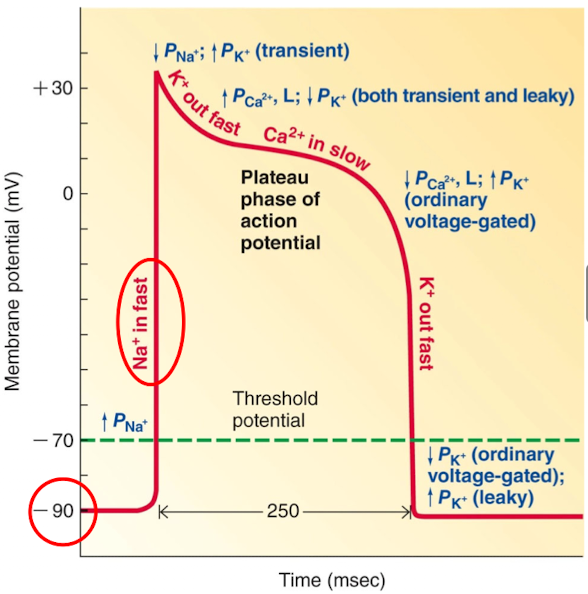
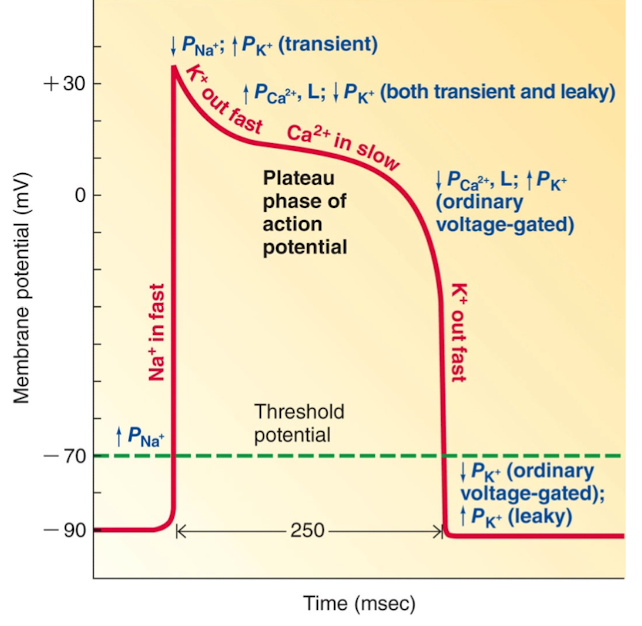
Action potential in contractile cardiac muscle cells
Action potential in cardiac contractile cells differs considerable from the action potential in cardiac autorhythmic cells
Very negative resting potential (-90mV) until excited
Rapid rising phase of the action potential in contractile cells is the result of Na+ entry on opening of fast Na+ channels at threshold
The early, brief repolarization after the potential reaches its peak is bc of limited K+ efflux on opening of transient K+ channels, coupled with inactivation
Plateau phase is result of slow Ca++ entry on opening of L-type Ca++ channels, couple with reduced K+ efflux on closure of several types of K+ channels
Rapid falling phase is the result of K+ efflux on opening of ordinary voltage-gated K+ channels, as in other excitable cells
Resting potential is maintained by opening of leaky K+ channels
AP in Pacemaker Cell vs AP in Cardiac Cell
During the spike of an action potential in a cardiac muscle cell
there is a rapid influx of Na+ into the cell
Excitation-Contraction Coupling of Cardiac Muscle
Mechanism of Ca++ entry into the cytosol is different from that in skeletal muscle cells
T-tubule membranes in cardiac muscle cells contain dyhydropyridine receptors that act as voltage-gated Ca++ channels. When an action potential invades the T-tubule membrane these channels open and allow Ca++ to flow into the cytosol
Ca++ entry triggers further release of Ca++ from the sarcoplasmic reticulum. These 2 sources of cytosolic Ca++ activate the power stroke of contraction
Unlike skeletal muscle cells, the number of activated cross-brides is proportional to the cytosolic Ca++ concentration
The cardiac cycle includes all of the following events except:
A. the movement of impulse from the SA node to all regions of the heart wall
B. The closing and opening of hearts valves during each heartbeat
C. the number of times the heart beats in one minute
D. the changes in pressure gradients in all chambers of the heart
E. the changes in blood volume in all chambers of the heart
C, the number of times the heart beats in one minute
Electrocardiogram
electrical currents generated by the coordinated action potentials of the heart muscle can reach the surface of the body and be detected as voltage differences btwn two points on the body surface
Record resulting from measuring these voltage changes is referred to as the electrocardiogram (ECG). Disturbances in heart function can be detected as changes in the ECG
Electrocardiogram Waveforms
P-wave
QRS complex
T-wave
PR Segment
P-wave
depolarization of the atria
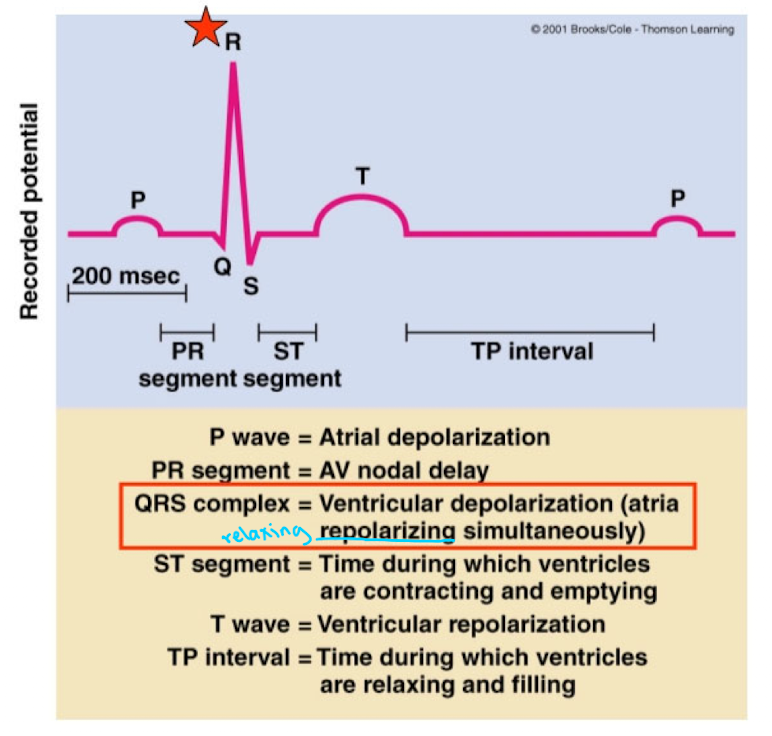
QRS complex
Ventricular depolarization (atria repolarizing simultaneously)
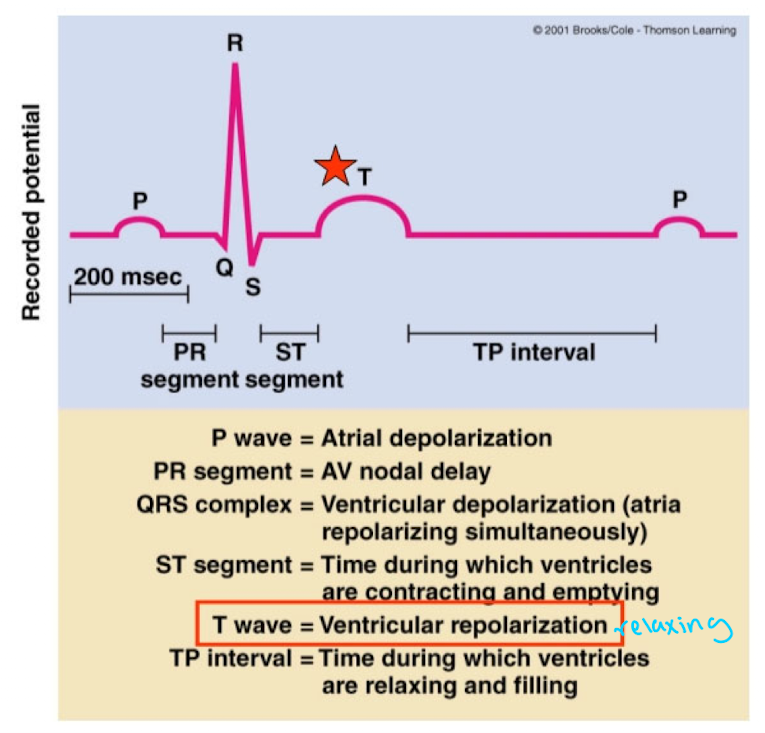
T-wave
Venticular repolarization
PR Segment
represents AV node delay
Abnormality in Heart Rate
Tachycardia - racing heart
If P, QRS, T is working a lot faster with no TP interval where ventricles will no longer fill, not enough oxygenated blood would pump through body
The P wave of the ECG represents:
atrial depolarization
Mechanical Events of the cardiac cycle
cardiac cycle consists of alternate periods of contraction and emptying (systole) and relocation and filling (diastole).
sequence of changes in pressure, volume, electrical activity and valve activity occur during each cycle
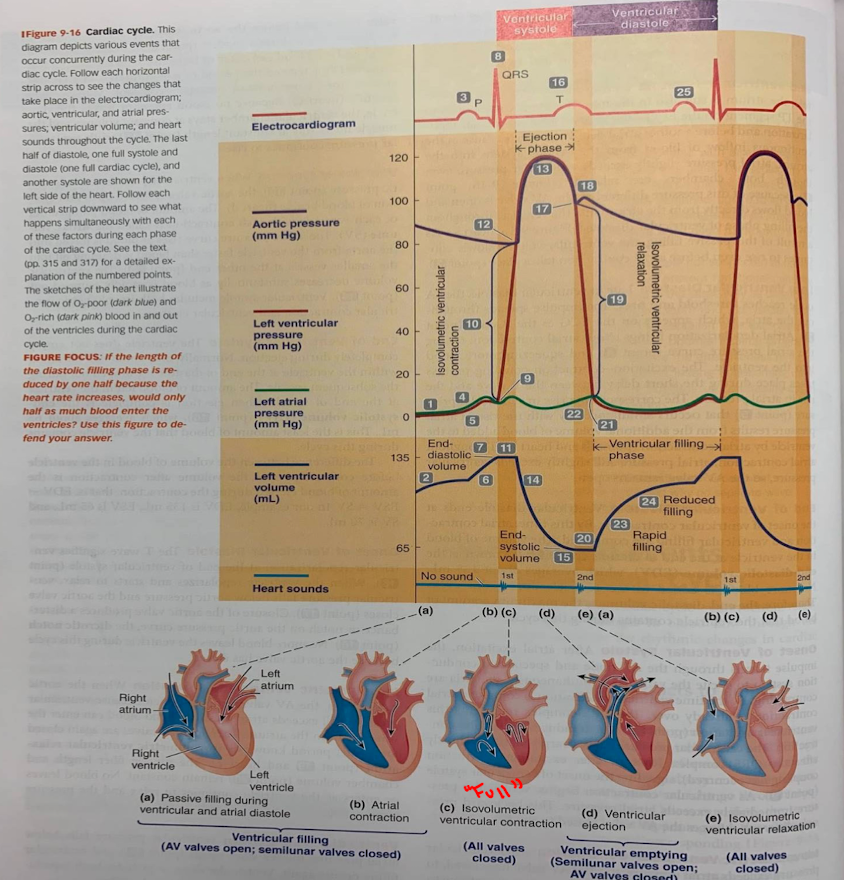
End-Diastolic Volume (mechanical events of cardiac cycle)
the volume of blood in the chamber at the end of diastole (relaxation/filling). Equivalent to the maximum amount of blood chamber will hold during the cycle
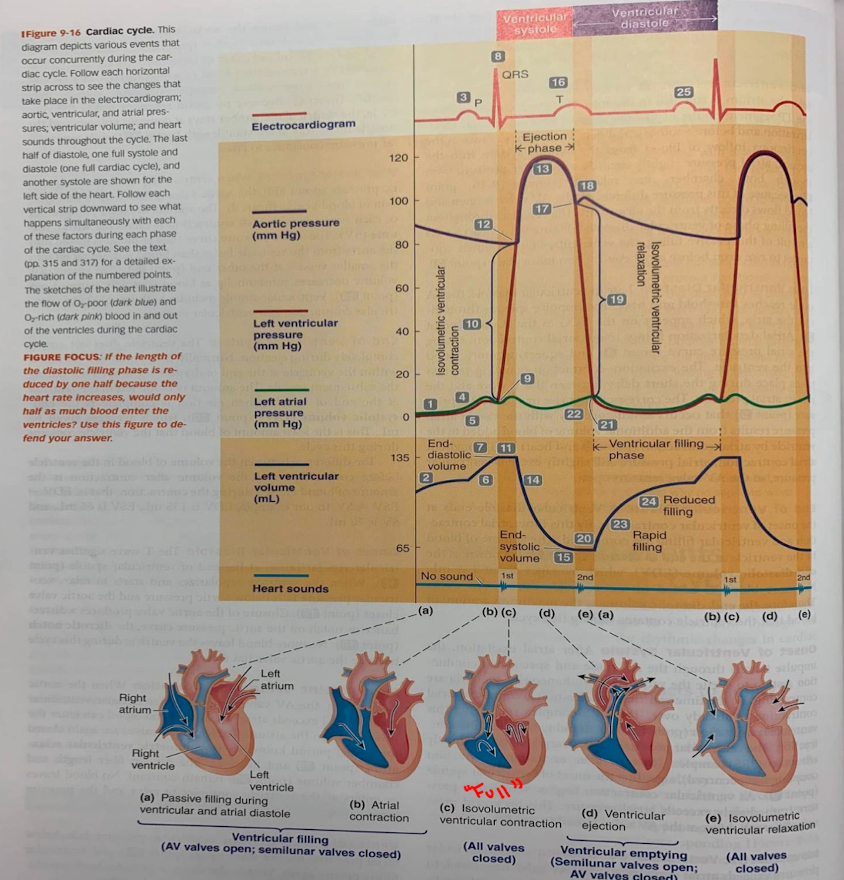
Isovolumetric Ventricular Contraction (mechanical events of the cardiac cycle)
Period of time during contraction when the chamber remains closed, and therefore no blood can enter or leave. Chamber pressure increases during this period
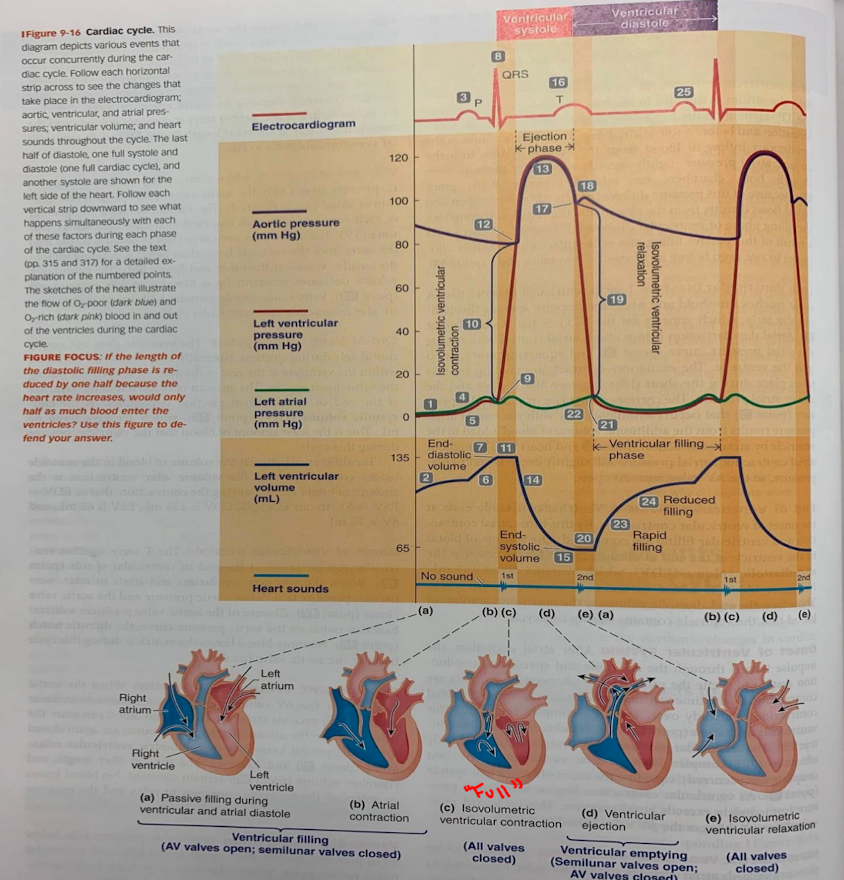
End-Systolic Volume (mechanical events of the cardiac cycle)
amount of blood remaining in the chamber at the end of systole (contraction/emptying) when ejection is complete
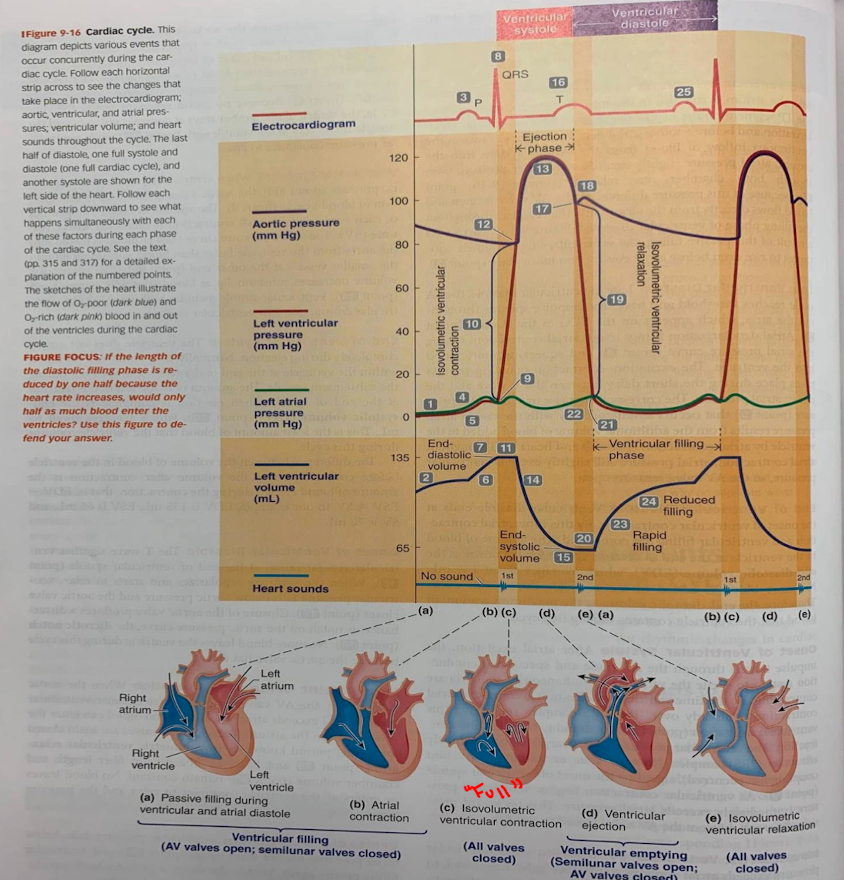
Stroke Volume (Mechanical Events of the Cardiac Cycle)
amount of blood pumped out of the chamber with each contraction. Equal to the end-diastolic volume minus the end-systolic volume
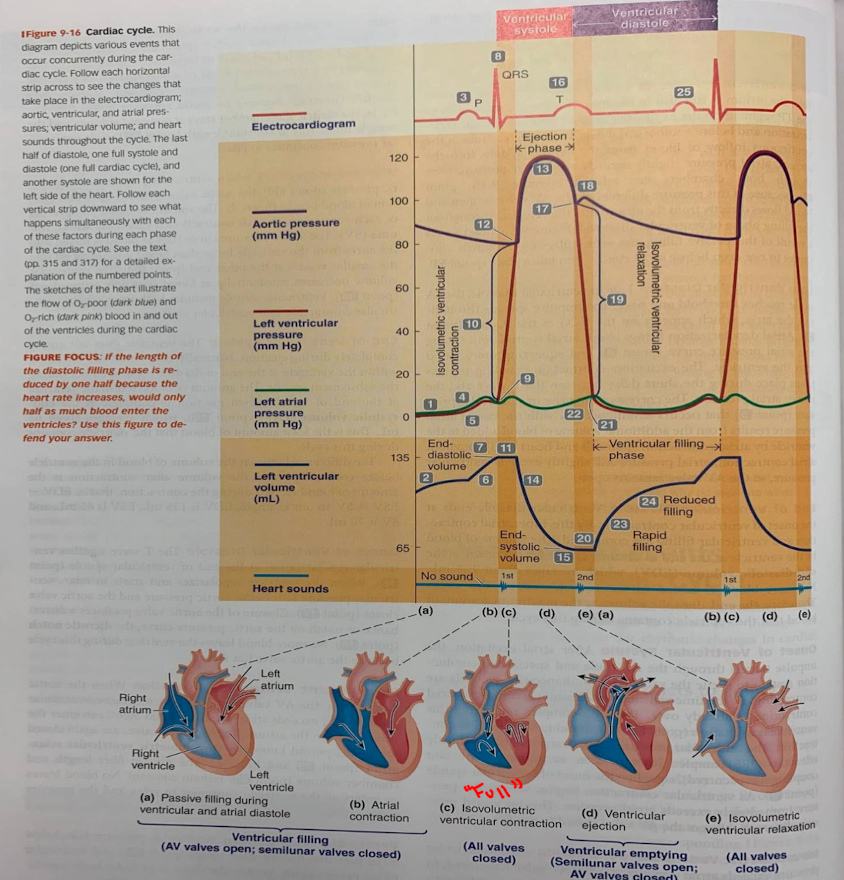
Isovolumetric Ventricular Relaxation (mechanical events of the cardiac cycle)
period of time during relaxation when the chamber remains closed, and therefore no blood can enter or leave. Chamber pressure decreases during this period
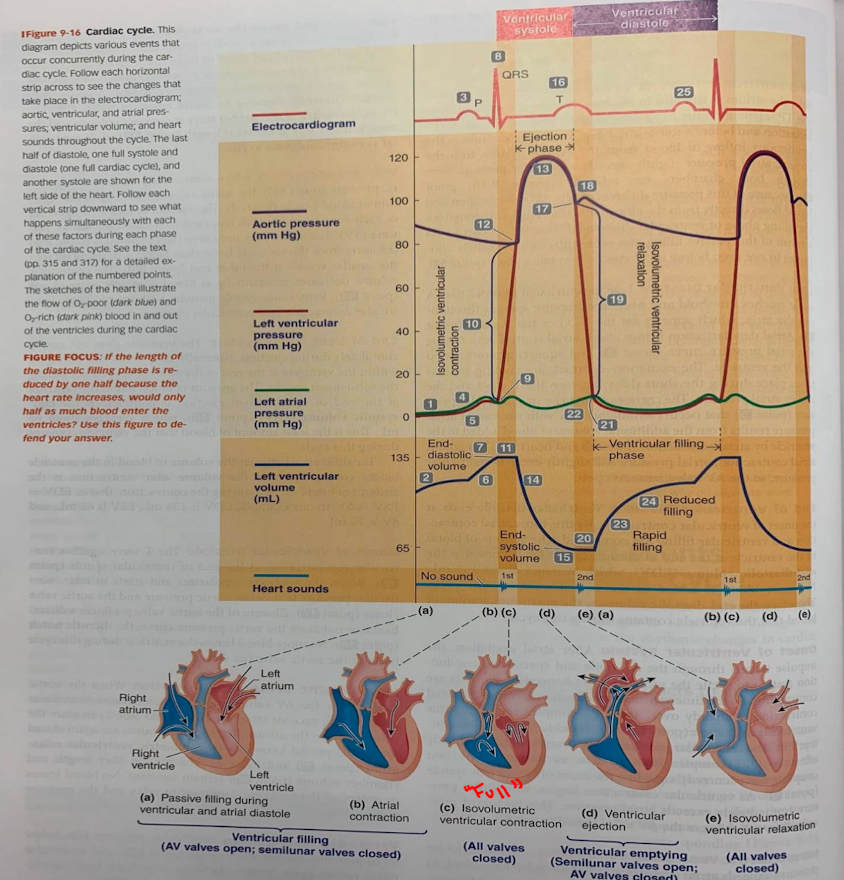
First heart sound
low-pitched, soft and relatively long sound associated with the closure of the AV valves.
Often referred to as a “lub
Second heart sound
high-pitched, sharp and relatively short sound associated with the closing of the semilunar valves.
Often referred to as a “dup”
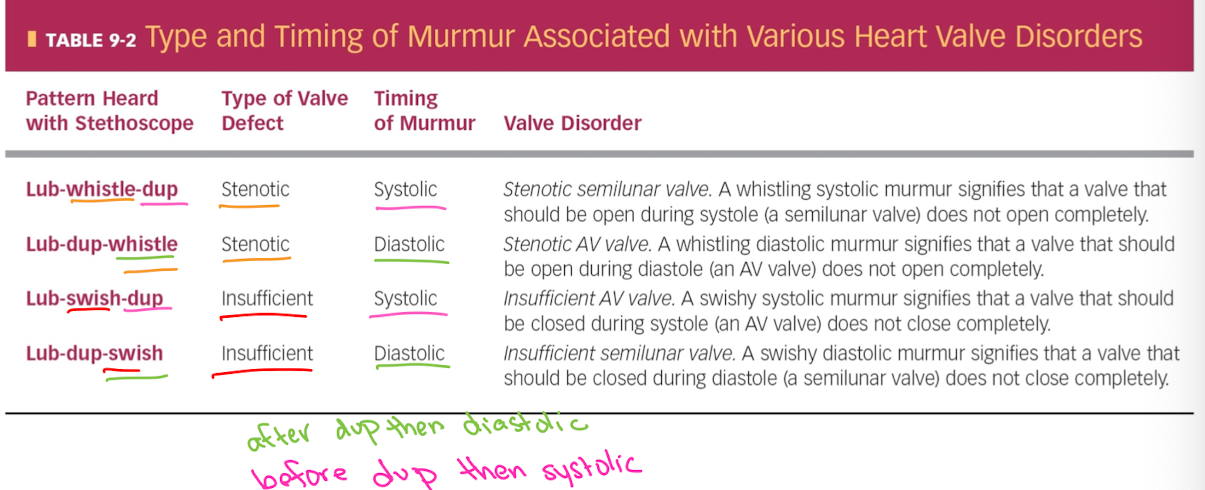
Murmurs
abnormal heart sounds, often associated with cardiac disease that are due to the turbulent flow of blood through malfunctioning valves
Stenotic Valve
stiff, narrow valve that does not open completely. Turbulent flow is induced bc blood must be forced through the valve at high velocity.
Produces an abnormal whistling sound
Insufficient Valve
Structurally damaged valve that does not close properly. Turbulence occurs when the blood flows backward through the valve and collides with blood moving in the opposite direction.
Produces an abnormal swishing sound
Rheumatic fever
an auto-immune disease triggered by streptococcal bacteria that leads to valvular stenosis and insufficiency
Type and Timing of Murmur Associated w/Various Heart Valve Disorders
Lub= AV valves closing
Dup = semilunar valves closing
Whistle = stenotic valve (forced blood at high velocity)
Swish = insufficient valve (back flow of blood)
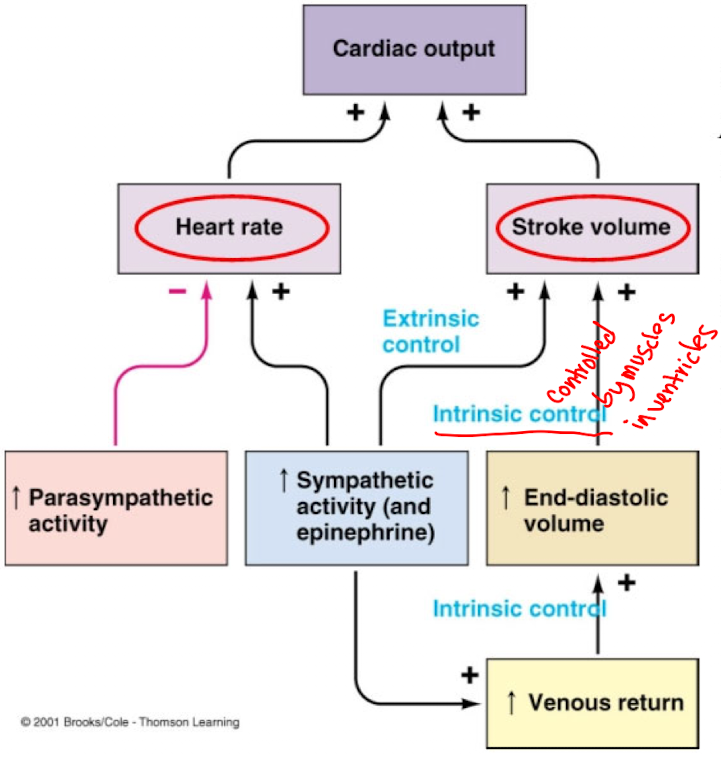
Regulation of Cardiac Output
Cardiac output is the volume of blood pumped by each ventricle per minute. Pulmonary volume is equivalent to the system volume
Determined by heart rate and stroke volume
C.O. = H.R. x S.V.
Ex. Avg heart rate is ~70bpm, avg stroke volume is ~70 mls.
C.O. = 70 × 70 = 4900mls.min = ~5liters/min
Heart rate
regulated by parasympathetic and sympathetic nervous system systems
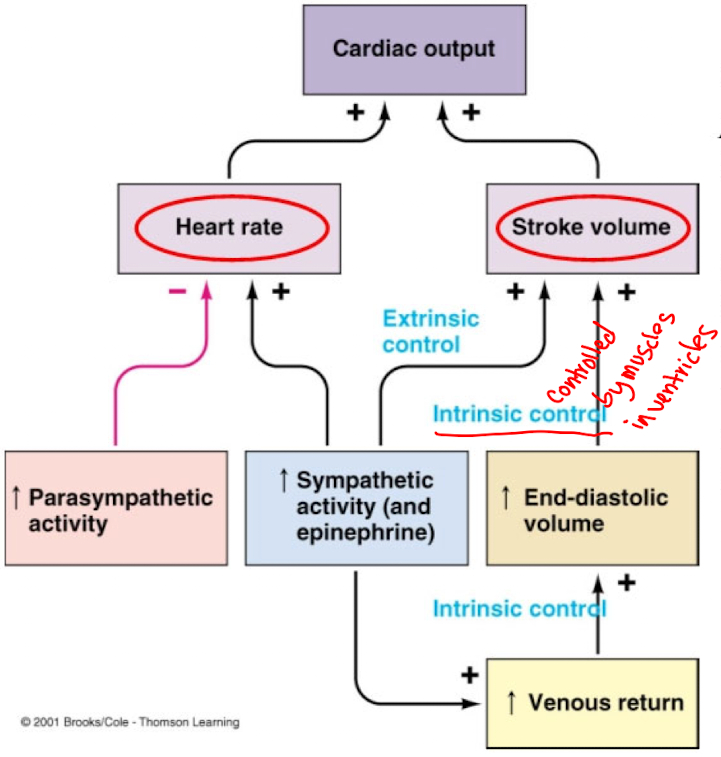
Stroke volume
regulated intrinsically by volume of venous blood returning to the ventricles, and extrinsically by the sympathetic nervous system
Heart Rate Regulation
Regulated primarily by autonomic influences that control the excitability of the SA node
Parasympathetic
supplied by the vagus nerve to the SA and AV nodes to the contractile cells of the atria. Very little parasympathetic innervation of the ventricles
What is parasympathetic input mediated by?
neurotransmitter Acetylcholine (ACh) through muscarinic receptors. ACh causes heart rate to decrease
Effects of Parasympathetic Release of Acetylcholine (ACH) on SA node
ACh increases the permeability of SA nodal cells to K+ by delaying the inactivation of K+ channels that occurs after an action potential.
Leads to greater hyperpolazarization of the SA nodal cells and slowing of the K+ component of the pacemaker potential
Effects of Parasympathetic Release of Acetylcholine (ACH) on AV Node
increases permeability of AV nodal cells to K+.
This reduces the excitability of AV node and further delays its response to the input arriving from the SA node
Effects of Parasympathetic Release of Acetylcholine (ACH) on Atrial Contractile Cells
shortens the duration of the cardiac fiber action potentials by reducing the Ca++ permeability during the plateau phase of the action potential
Less Ca++ enters the cells and strength of contraction is reduced
Sympathetic Influence on Heart Rate: Sympathetic and what is it mediated by
Nerves supply the aura (the SA and AV nodes) and richly innervate the ventricles
Input is mediated by the neurotransmitter Norepinephrine (NE) through beta-adrenergic receptors, causes the heart rate to increase
Sympathetic Influence on Heart Rate: SA Node
NE decreases permeability of SA nodal cells to K+ by accelerating the inactivation of K+ channels that occurs after an action potential.
Effect leads to less hyperpolarization of the SA nodal cells and an acceleration of the K+ component of the pacemaker potential
Sympathetic Influence on Heart Rate: AV Node
increases the conduction velocity of AV nodal cells, leading to a reduction of AV nodal delay by enhancing the slow increase in C++ permeability during the Ca++ phase of the pacemaker potential
Sympathetic Influence on Heart Rate: Bundle of His and Purkinje fibers
similar action to that occurring the AV node
Effects of Sympathetic Release of Norepinephrine:
Atrial and ventricular contractile cells
increases contractile strength by enhancing the Ca++ permeability during the plateau phase of the action potential. Therefore more Ca++ enters the cells and the strength of contraction is increased
Cardiac output is determined by …
heart rate and stroke volume
Name the 3 phases of cardiac cycle in the order:
mid-to-late diastole, ventricular systole, early diastole
Stroke Volume Regulation
Regulated extrinsically by neural control from the sympathetic nervous system and intrinsically by the volume of venous blood returning to the heart.
Both factors increase stroke volume by increasing the strength of contraction of the heart
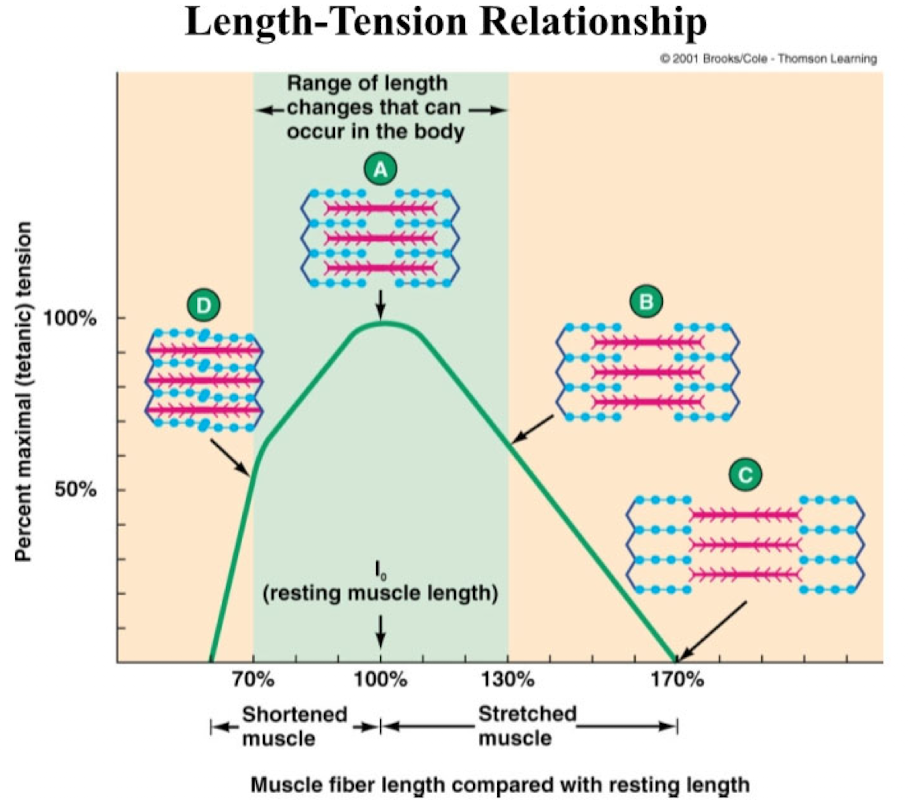
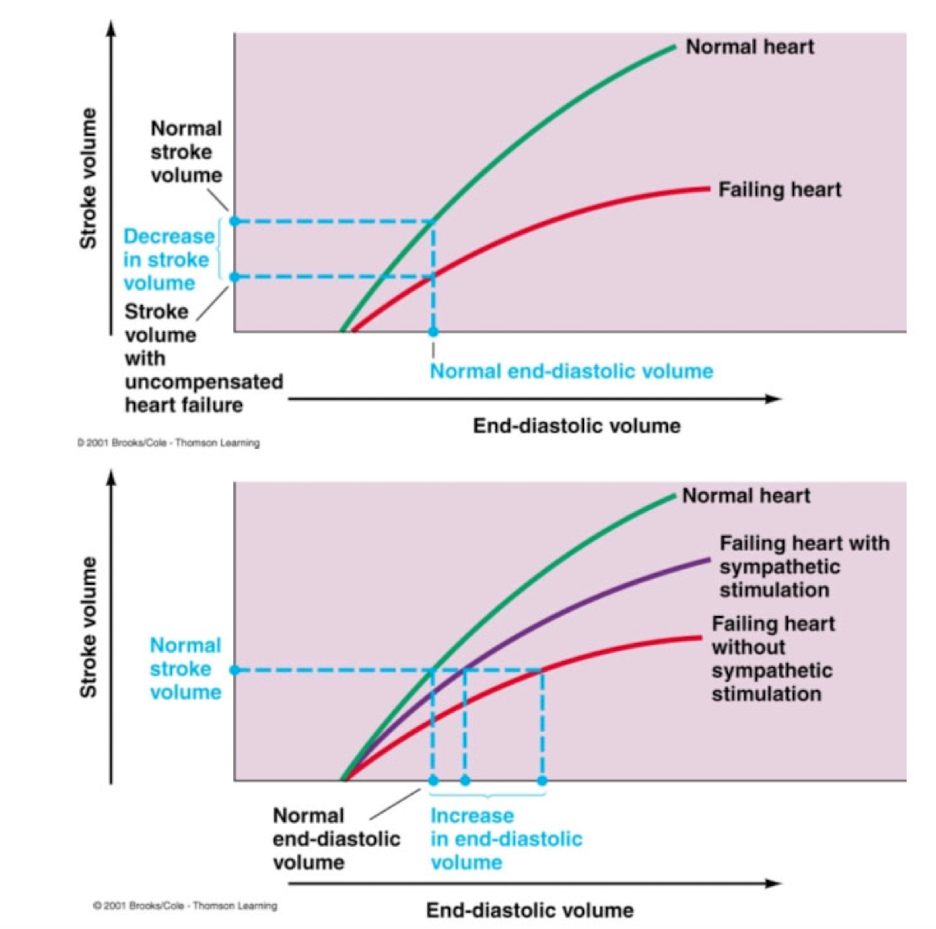
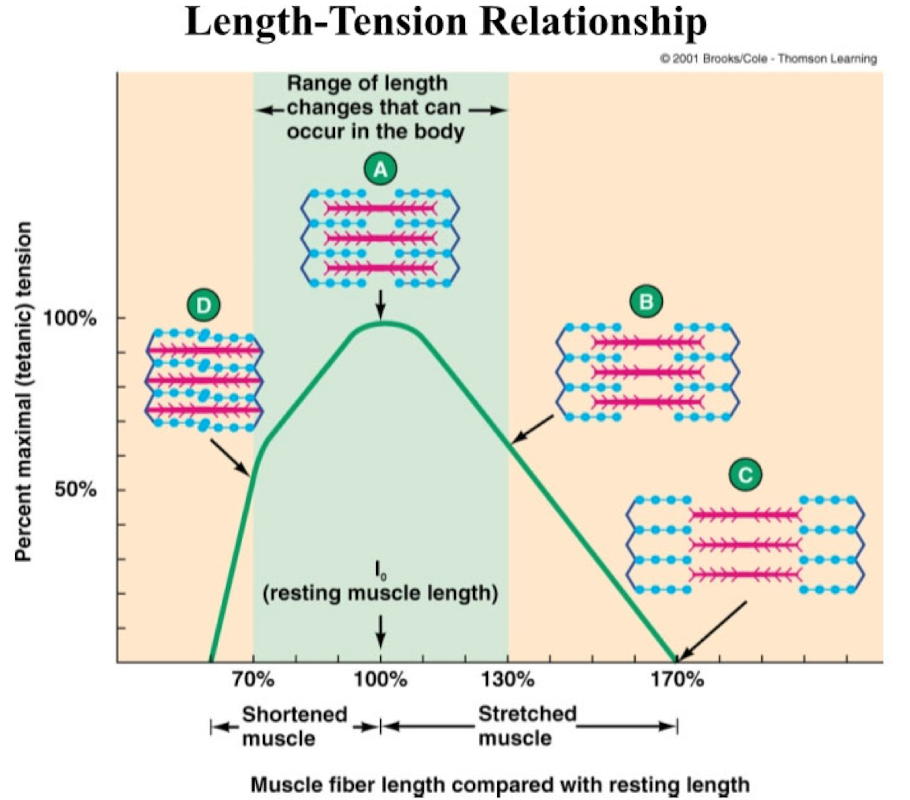
Intrinsic Control
Direct correlation between end-diastolic volume and stroke volume known as the Frank-Starling law of the heart.
Dependent on the length-tension relationship of cardiac muscle
Sympathetic Stimulation Shifts the Frank-Starling Curve to the Left
at a given end-diastolic volume, Increased Ca++ via sympathetic stimulation will increase the contractile force and SV of the heart
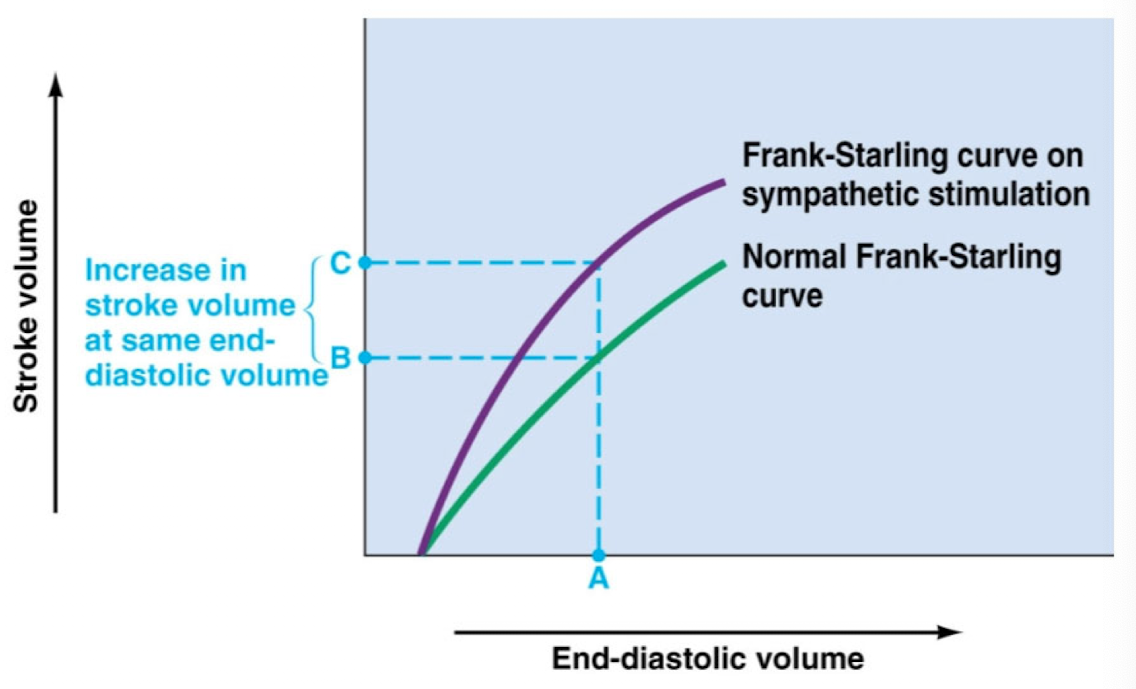
Heart Failure
Inability of cardiac output to meet the demands of the body
May occur in one or both ventricles leading to congestion of blood in the veins returning to the heart
Congestion results from …
damage to the heart muscle and/or prolonged pumping against increased arterial blood pressure (as might occur with a stenotic semilunar valve or chronic high blood pressure)
What is the end result of heart failure?
Decrease in cardiac contractility that shifts Frank Starling curve downward and to the right
Compensated for by increased sympathetic activity and increased blood volume due to retention of salt and water by the kidneys