Chapter 13: Lymphatic System And Immunity
5.0(1)
Card Sorting
1/132
Earn XP
Last updated 1:05 AM on 12/11/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
133 Terms
1
New cards
Enlist the Functions of the Lympathic System
1. Fluid balance
2. Lipid absorption
3. Defense
2. Lipid absorption
3. Defense
2
New cards
Lymphatic capillaries
-tiny, closed-ended vessels consisting of simple squamous epithelium
-more permeable than blood capillaries because they lack a basement membrane, and fluid moves easily into them
‑ joins to form larger lymphatic vessels
-more permeable than blood capillaries because they lack a basement membrane, and fluid moves easily into them
‑ joins to form larger lymphatic vessels
3
New cards
Lymphatic vessels
‑ resemble small veins
‑ have a beaded appearance because they have one-way valves that are similar to the valves of veins
‑ have a beaded appearance because they have one-way valves that are similar to the valves of veins
4
New cards
Factors that make compression of the Lymphatic vessels
1. contraction of surrounding skeletal muscle during activity
2. contraction of smooth muscle in the lymphatic vessel wall
3. pressure changes in the thorax during breathing
2. contraction of smooth muscle in the lymphatic vessel wall
3. pressure changes in the thorax during breathing
5
New cards
thoracic duct
where lymphatic vessels from the rest of the body enters; empties into the left subclavian vein
6
New cards
right lymphatic duct
lymphatic vessels from the right upper limb and the right half of the head, neck, and chest; empties into the right subclavian vein
7
New cards
Lymphatic Organs
include the tonsils, the lymph nodes, the spleen, and the thymus
8
New cards
Lymphatic tissue
characterized by housing many lymphocytes and other defense cells, such as macrophages
9
New cards
Tonsils
form a protective ring of lymphatic tissue around the openings between the nasal and oral cavities and the pharynx
10
New cards
Three groups of tonsils
palatine tonsils
pharyngeal tonsil
lingual tonsil
pharyngeal tonsil
lingual tonsil
11
New cards
palatine tonsils
located on each side of the posterior opening of the oral cavity; these are the ones usually referred to as “the tonsils.
12
New cards
pharyngeal tonsil
located near the internal opening of the nasal cavity
13
New cards
lingual tonsil
located on the posterior surface of the tongue
14
New cards
tonsillectomy
removal of the pharyngeal tonsils
15
New cards
adenoidectomy
removal of the palatine tonsil
16
New cards
Lymph Nodes
rounded structures, varying from the size of a small seed to that of a shelled almond
17
New cards
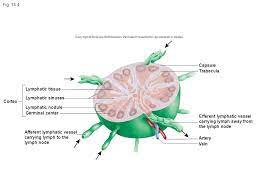
Parts if the Lymph node
Capsule
Trabeculae
Lymphatic nodules
Lymphatic sinuses
Germinal centers
Trabeculae
Lymphatic nodules
Lymphatic sinuses
Germinal centers
18
New cards
Three superficial aggregations of lymph nodes
• inguinal nodes in the groin
• axillary nodes in the axilla
• the cervical nodes in the neck
• axillary nodes in the axilla
• the cervical nodes in the neck
19
New cards
functions of lymph nodes
• activate the immune system
• remove pathogens from the lymph through the action of macrophages
• remove pathogens from the lymph through the action of macrophages
20
New cards
Spleen
‑ roughly the size of a clenched fist and is located in the left, superior corner of the abdominal cavity
‑ filters blood instead of lymph
‑ blood reservoir
‑ has an outer capsule of dense connective tissue and a small amount of smooth muscle
‑ filters blood instead of lymph
‑ blood reservoir
‑ has an outer capsule of dense connective tissue and a small amount of smooth muscle
21
New cards
Trabeculae
divide the spleen into small, interconnected compartments containing two specialized types of lymphatic tissue:
o white pulp
o red pulp
o white pulp
o red pulp
22
New cards
Splenectomy
removal of the spleen
23
New cards
Thymus
‑ a bilobed gland roughly triangular in shape
‑ located in the superior mediastinum
‑ site for the maturation of a class of lymphocytes called T cells
‑ surrounded by a thin connective tissue capsule
‑ located in the superior mediastinum
‑ site for the maturation of a class of lymphocytes called T cells
‑ surrounded by a thin connective tissue capsule
24
New cards
Lymph
the fluid that lympathic capillaries remove from the blood stream
25
New cards
Valves of lymphatic vessels
prevents backflow of lymph
26
New cards
Lacteals
found in the small intestine absorb lipids, which enter the thoracic duct.
27
New cards
Chyle
lymph containing lipids, enters the blood.
28
New cards
function of spleen
filters blood and is a site where lymphocytes
respond to infections
respond to infections
29
New cards
Lymphocytes
(pre-B and pre-T cells) originate from stem cells in the red bone marrow. The pre-B cells become mature B cells in the red bone marrow and are released into the blood. The pre-T cells enter the blood and migrate to the thymus
30
New cards
thymus
where pre-T cells derived from red bone
marrow increase in number and become mature T cells that are released into the blood.
marrow increase in number and become mature T cells that are released into the blood.
31
New cards
B cells and T cells
Populates all lymphatic tissues. These lymphocytes can remain in tissues or pass through them and return to the blood. B
cells and T cells can also respond to infections by dividing and increasing in number. Some of the newly formed cells enter the blood and circulate to other tissues.
cells and T cells can also respond to infections by dividing and increasing in number. Some of the newly formed cells enter the blood and circulate to other tissues.
32
New cards
Immunity
‑ the ability to resist damage from pathogens, such as microorganisms; harmful chemicals, such as toxins released by microorganisms; and internal threats, such as cancer cells
33
New cards
two immunity systems
• innate immunity (nonspecific resistance)
• adaptive immunity (specific immunity)
o specificity
o memory
• adaptive immunity (specific immunity)
o specificity
o memory
34
New cards
Physical Barriers
‑ prevent pathogens and chemicals from entering the body in two ways:
1. the skin and mucous membranes form barriers that prevent their entry
2. tears, saliva, and urine wash these substances from body surfaces
1. the skin and mucous membranes form barriers that prevent their entry
2. tears, saliva, and urine wash these substances from body surfaces
35
New cards
Chemical Mediators
‑ molecules responsible for many aspects of innate immunity.
‑ some chemicals on the surface of cells destroy pathogens or prevent their entry into the cells
• Complement
• Interferons
‑ some chemicals on the surface of cells destroy pathogens or prevent their entry into the cells
• Complement
• Interferons
36
New cards
White Blood Cells
‑ most important cellular components of immunity
‑ produced in red bone marrow and lymphatic tissue and released into the blood
‑ produced in red bone marrow and lymphatic tissue and released into the blood
37
New cards
Types of WBC
Phagocytic Cells = Neutrophils and Macrophages
Cells of Inflammation = Basophils, Mast cells, and Eosinophils
Natural Killer Cells
Cells of Inflammation = Basophils, Mast cells, and Eosinophils
Natural Killer Cells
38
New cards
Phagocytosis
ingestion and destruction of particles by cells called phagocytes
39
New cards
Neutrophils
small phagocytic WBC; usually the first WBC
to enter infected tissues from the blood in large numbers
to enter infected tissues from the blood in large numbers
40
New cards
Pus
an accumulation of fluid, dead neutrophils, and other cells at a site of infection
41
New cards
Macrophages
-are monocytes that leave the blood, enter tissues, and enlarge about fivefold
o mononuclear phagocytic system
o dust cells
o Kupffer cells
o microglia
o mononuclear phagocytic system
o dust cells
o Kupffer cells
o microglia
42
New cards
Basophils
derived from red bone marrow; motile WBCs that can leave the blood and enter infected tissues
43
New cards
Mast cells
derived from red bone marrow, are nonmotile cells in connective tissue, especially near capillaries
44
New cards
Eosinophils
participate in inflammation associated with allergies and asthma
45
New cards
Natural Killer Cells
‑ a type of lymphocyte produced in red bone marrow, and they account for up to 15% of lymphocytes
- recognize classes of cells, such as tumor cells or virus infected cells, in general, rather than specific tumor cells or cells infected by a specific virus
‑ do not exhibit memory response
- recognize classes of cells, such as tumor cells or virus infected cells, in general, rather than specific tumor cells or cells infected by a specific virus
‑ do not exhibit memory response
46
New cards
Inflammatory Response
Bacteria cause tissue damage that stimulates the release or activation of chemical mediators, such as histamine, prostaglandins, leukotrienes, complement, and kinins.
47
New cards
Local inflammation
an inflammatory response confined to a specific area of the body
48
New cards
Systemic inflammation
an inflammatory response that is generally distributed throughout the body
o Pyrogens
o Pyrogens
49
New cards
Antigens
-substances that stimulate adaptive immune responses; can be divided into two groups:
• Foreign antigens
• Self-antigens
o Autoimmune disease
• Foreign antigens
• Self-antigens
o Autoimmune disease
50
New cards
Adaptive immunity can be divided into
Antibody-mediated immunity &
Cell-mediated immunity
Cell-mediated immunity
51
New cards
Antibody-mediated immunity
involves a group of lymphocytes called B cells and proteins called antibodies, which are found in the plasma
o Antibodies
o Antibodies
52
New cards
Cell-mediated immunity
-involves the actions of a second type of lymphocyte, called T cells
o cytotoxic T cells
o helper T cells
o cytotoxic T cells
o helper T cells
53
New cards
Origin and Development of Lymphocytes
• Both B cells and T cells originate from stem cells in red
bone marrow.
• B cells are processed from pre-B cells in the red marrow.
• T cells are processed from pre-T cells in the thymus.
• Both B cells and T cells circulate to other lymphatic tissues,
such as lymph nodes.
bone marrow.
• B cells are processed from pre-B cells in the red marrow.
• T cells are processed from pre-T cells in the thymus.
• Both B cells and T cells circulate to other lymphatic tissues,
such as lymph nodes.
54
New cards
Ways of Activation and Multiplication of Lymphocytes
Antigen Recognition
Lymphocyte Proliferation
Lymphocyte Proliferation
55
New cards
Antigen Receptor
cell membrane proteins on the surfaces of lymphocytes
56
New cards
Lymphocyte Proliferation
-important process that generates the needed defense cells to protect the body
57
New cards
Proliferation of Helper T Cells
1. Antigen-presenting cells, such as macrophages, phagocytize, process, and display antigens on the cell’s surface.
2. The antigens are bound to MHC class II molecules, which present the processed antigen to the T-cell receptor of the helper T cell.
3. Costimulation results from interleukin-1, secreted by the macrophage, and the CD4 glycoprotein of the helper T cell.
4. Interleukin-1 stimulates the helper T cell to secrete interleukin-2 and to produce interleukin-2 receptors.
5. The helper T cell stimulates itself to divide when interleukin-2 binds to interleukin-2 receptors.
6. The “daughter” helper T cells resulting from this division can be stimulated to divide again if they are exposed to the same antigen that stimulated the “parent” helper T cell. This greatly increases the number of helper T cells.
7. The increased number of helper T cells can facilitate the activation of B cells or effector T cells.
2. The antigens are bound to MHC class II molecules, which present the processed antigen to the T-cell receptor of the helper T cell.
3. Costimulation results from interleukin-1, secreted by the macrophage, and the CD4 glycoprotein of the helper T cell.
4. Interleukin-1 stimulates the helper T cell to secrete interleukin-2 and to produce interleukin-2 receptors.
5. The helper T cell stimulates itself to divide when interleukin-2 binds to interleukin-2 receptors.
6. The “daughter” helper T cells resulting from this division can be stimulated to divide again if they are exposed to the same antigen that stimulated the “parent” helper T cell. This greatly increases the number of helper T cells.
7. The increased number of helper T cells can facilitate the activation of B cells or effector T cells.
58
New cards
Proliferation of B Cells
1. Before a B cell can be activated by a helper T cell, the B cell must phagocytize and process the same antigen that activated the helper T cell. The antigen binds to a B-cell receptor, and both the receptor and the antigen are taken into the cell by endocytosis.
2. The B cell uses an MHC class II molecule to present the processed antigen to the helper T cell.
3. The T-cell receptor binds to the MHC class II/antigen complex.
4. There is costimulation of the B cell by CD4 and other surface molecules.
5. There is costimulation by interleukins (cytokines) released from the helper T cell.
6. The B cell divides, the resulting daughter cells divide, and so on, eventually producing many cells that recognize the same antigen.
7. Many of the daughter cells differentiate to become plasma cells, which produce antibodies. Antibodies are part of the immune response that eliminates the antigen.
2. The B cell uses an MHC class II molecule to present the processed antigen to the helper T cell.
3. The T-cell receptor binds to the MHC class II/antigen complex.
4. There is costimulation of the B cell by CD4 and other surface molecules.
5. There is costimulation by interleukins (cytokines) released from the helper T cell.
6. The B cell divides, the resulting daughter cells divide, and so on, eventually producing many cells that recognize the same antigen.
7. Many of the daughter cells differentiate to become plasma cells, which produce antibodies. Antibodies are part of the immune response that eliminates the antigen.
59
New cards
Antibody-Mediated Immunity
effective against extracellular antigens, such as bacteria, viruses (when they are outside cells), and toxins
60
New cards
Antibodies
-proteins produced in response to an antigen. They are Y-shaped molecules consisting of four polypeptide chains: two identical heavy chains and two identical light chains
61
New cards
variable region
end of each “arm” of the antibody; part that combines with the antigen
62
New cards
Effects of Antibodies
• Antibodies directly affect antigens by inactivating the
antigens or by binding the antigens together.
• Antibodies indirectly affect antigens by activating other
mechanisms through the constant region of the antibody.
1. Inactivate the antigen
2. Bind antigens together
3. Activate the complement cascade. An antigen binds to an antibody. As a result, the antibody can activate complement proteins, which can produce inflammation, chemotaxis, and lysis.
4. Initiate the release of inflammatory chemicals. An antibody binds to a mast cell or a basophil. When an antigen binds to the antibody, it triggers the release of chemicals that cause inflammation.
5. Facilitate phagocytosis. An antibody binds to an antigen and then to a macrophage, which phagocytizes the antibody and antigen.
antigens or by binding the antigens together.
• Antibodies indirectly affect antigens by activating other
mechanisms through the constant region of the antibody.
1. Inactivate the antigen
2. Bind antigens together
3. Activate the complement cascade. An antigen binds to an antibody. As a result, the antibody can activate complement proteins, which can produce inflammation, chemotaxis, and lysis.
4. Initiate the release of inflammatory chemicals. An antibody binds to a mast cell or a basophil. When an antigen binds to the antibody, it triggers the release of chemicals that cause inflammation.
5. Facilitate phagocytosis. An antibody binds to an antigen and then to a macrophage, which phagocytizes the antibody and antigen.
63
New cards
Antibody Production
• primary response
• memory B cells
• secondary response/memory response
• memory B cells
• secondary response/memory response
64
New cards
Cell-Mediated Immunity
‑ a function of cytotoxic T cells and is most effective against microorganisms that live inside body cells; involved with allergic reactions, control of tumors, and graft rejection
65
New cards
Cytotoxic T cells have two main effects:
• When activated, cytotoxic T cells form many additional cytotoxic T cells, as well as memory T cells.
• The cytotoxic T cells release cytokines that promote the destruction of the antigen or cause the lysis of target cells, such as virally infected cells, tumor cells, or transplanted cells. The memory T cells are responsible for the secondary response.
• The cytotoxic T cells release cytokines that promote the destruction of the antigen or cause the lysis of target cells, such as virally infected cells, tumor cells, or transplanted cells. The memory T cells are responsible for the secondary response.
66
New cards
ACQUIRED IMMUNITY
• Natural
• Artificial
• Artificial
67
New cards
Active immunity
-immunity is provided by the individual’s own immune system
• active natural immunity
• active artificial immunity
• active natural immunity
• active artificial immunity
68
New cards
Passive immunity
-immunity is transferred from another person or an animal
• passive natural immunity
• passive artificial immunity
• passive natural immunity
• passive artificial immunity
69
New cards
Innate immunity
general response that does not improve with subsequent exposure
70
New cards
Adaptive immunity
- specific response that improves with
subsequent exposure; begins with a macrophage presenting
an antigen to a helper T cell
• Antibody-mediated immunity
• Cell-mediated immunity
subsequent exposure; begins with a macrophage presenting
an antigen to a helper T cell
• Antibody-mediated immunity
• Cell-mediated immunity
71
New cards
Immunotherapy
treats disease by altering immune system function or by directly attacking harmful cells
72
New cards
EFFECTS OF AGING ON THE LYMPHATIC SYSTEM AND
IMMUNITY
IMMUNITY
• Aging has little effect on the lymphatic system’s ability to remove fluid from tissues, absorb lipids from the digestive tract, or remove defective red blood cells from the blood.
• Decreased helper T-cell proliferation results in decreased antibody-mediated and cell-mediated immune responses.
• The primary and secondary antibody responses decrease with age.
• The ability to resist intracellular pathogens decreases with
age.
• Decreased helper T-cell proliferation results in decreased antibody-mediated and cell-mediated immune responses.
• The primary and secondary antibody responses decrease with age.
• The ability to resist intracellular pathogens decreases with
age.
73
New cards
DISEASES of lymphatic system
• Lymphedema
• Lymphoma
• Lymphoma
74
New cards
Immediate Allergic Reactions
• Asthma
• Anaphylaxis
• Anaphylaxis
75
New cards
Delayed Allergic Reactions
Symptoms occur in hours to days following exposure to the antigen because these types of reactions involve migration of T cells to the antigen, followed by release of cytokines
76
New cards
Immunodeficiencies
• Severe combined
immunodeficiency
(SCID)
• Acquired
immunodeficiency
syndrome (AIDS)
immunodeficiency
(SCID)
• Acquired
immunodeficiency
syndrome (AIDS)
77
New cards
pathogen
any substance or microorganism that causes disease or damage to the tissues of the body
78
New cards
Capsule
a dense connective tissue that surrounds each lymph node
79
New cards
Trabeculae
extensions of the capsule; subdivide a lymph node into compartments containing lymphatic tissue and lymphatic sinuses
80
New cards
Lymphatic nodules
lymphocytes and other cells that can form dense aggregations of tissue
81
New cards
Lymphatic sinuses
spaces between the lymphatic tissue that contain macrophages on a network of fibers
82
New cards
Germinal centers
lymphatic nodules containing the rapidly dividing lymphocytes; sites of lymphocyte production
83
New cards
white pulp
lymphatic tissue surrounding the arteries
within the spleen
within the spleen
84
New cards
red pulp
associated with the veins
85
New cards
trabeculae
divide each lobe into lobules
86
New cards
cortex
where lymphocytes are numerous and form dark-staining areas
87
New cards
medulla
lighter-staining, central portion of the lobules; fewer lymphocytea
88
New cards
Lymph nodes
filter lymph and are sites where lymphocytes respond to infections
89
New cards
innate immunity
body recognizes and destroys certain pathogens, but the response to them is the same each time the body is exposed
90
New cards
adaptive immunity
body recognizes and destroys pathogens, but the response to them improves each time the pathogen is encountered
91
New cards
specificity
the ability of adaptive immunity to recognize a particular substance
92
New cards
memory
the ability of adaptive immunity to “remember” previous encounters with a particular substance
93
New cards
Complement
a group of more than 20 proteins found in
plasma; can be activated by combining with foreign substances or antibodies; once activated, it can promote inflammation, phagocytosis, and lyse (rupture) bacterial cells
plasma; can be activated by combining with foreign substances or antibodies; once activated, it can promote inflammation, phagocytosis, and lyse (rupture) bacterial cells
94
New cards
Interferons
are proteins that protect the body against viral infections
95
New cards
chemotaxis
movement of WBC toward chemicals such as complement, leukotrienes, kinins, and histamine
96
New cards
mononuclear phagocytic system
formed by monocytes and macrophages because they are phagocytes with a single, unlobed nucleus
97
New cards
dust cells
lungs
98
New cards
Kupffer cells
liver
99
New cards
microglia
Central Nervous System (CNS)
100
New cards
Pyrogens
chemicals released by microorganisms, neutrophils, and other cells, stimulate fever production