Development II
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
39 Terms
development of vision from birth to 6 years (2)
•When a child is born their vision is very poor relative to an adults
•As long as development is not hindered by disease or other possible dysfunction (squints etc.) it gradually develops over the first 6 years of life.
when does visual acuity reach adult levels
Our acuity steadily improves approaching adult levels by ~4-5 years
roughly adult like by 5-6 years old
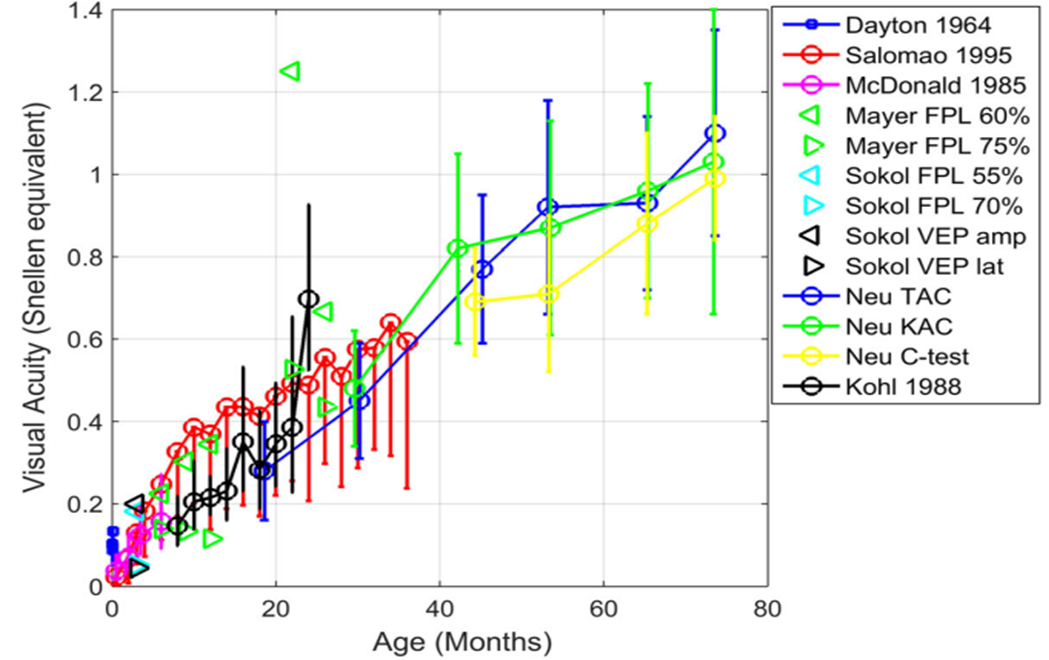
expected average VA based on age of children from 1 month - 4 years old
Age (months) | Test Distance (cm) | Mean Acuity (cycles/deg) | VA (Snellen approx) |
1 | 38 | 0.94 | 6/191 |
1.5 | 38 | 1.11 | 6/162 |
2.5 | 38 | 2.16 | 6/83 |
4 | 38 | 2.68 | 6/67 |
6 | 55 | 5.65 | 6/30 |
9 | 55 | 6.79 | 6/26 |
12 | 55 | 6.42 | 6/28 |
18 | 55 | 8.59 | 6/21 |
24 | 55 | 9.57 | 6/18 |
30 | 55 | 11.52 | 6/15 |
36 | 84 | 21.81 | 6/8 |
48 | 84 | 24.81 | 6/7 |
good to learn this table roughly for every 6 months - will be useful clinically
explain the problems that arise with measuring VA in children (3)
•Children’s acuity does however vary with the test, and cooperation of the child!
•The important thing is to have a rough idea of what it should be and compare the patient in your chair to suggested norms.
•Of extra importance – do both eyes see equally well - if they don’t - why is that
explain the contrast sensitivity function in children compared to adults and how it progresses over time (4)
In childhood contrast sensitivity is reduced compared to an adult, particularly at mid and high SFs
Contrast sensitivity shows a pronounced increase in the first two years of life
0-8 months - very significantly low CSF - as VA is very limited - cannot see high SFs
Immaturity of the retina (and cortex) in young children has been suggested as a reason for the differences
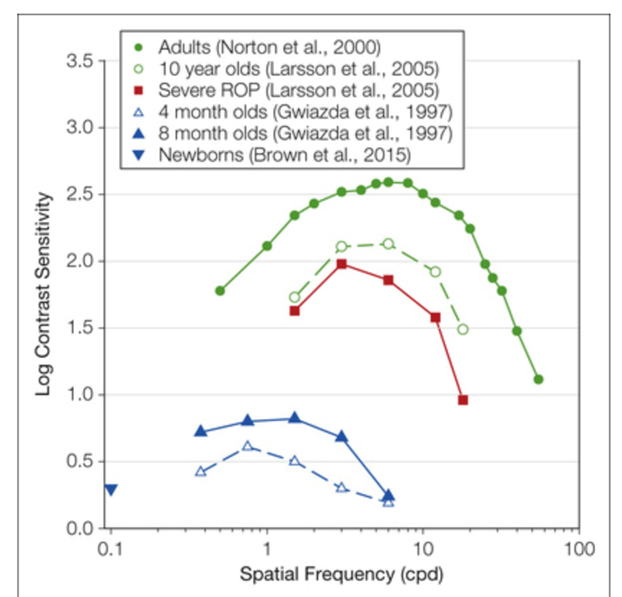
at what age does CSF reach adult levels
approximately 7-10 years
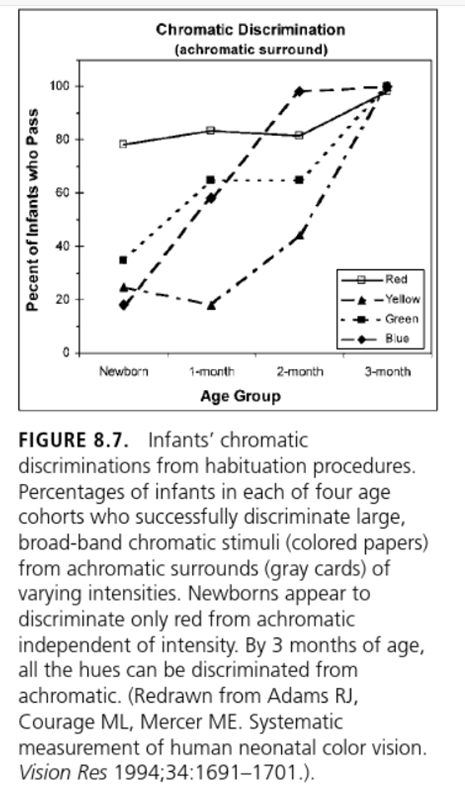
explain the development of colour vision from birth onwards (4)
•Colour vision at birth is poor.
•Studies suggest that newborn babies can discriminate red, but other colours aren’t reliably seen until about 2-3 months of age - which is why young babies like looking at B&W patterns
•It is suggested that a baby’s red-green colour pathway develops first, followed by the blue-yellow pathway a few months later. However, colours still need to be highly saturated to be detected.
•Discrimination of desaturated colours may not reach adult levels until late adolescence
explain the development of BV and stereopsis from birth onwards (3)
•Eye movement control has been shown to improve with age (and is better initially for static rather than kinetic stimuli).
•Sensitivity to retinal disparity (depth/responding to 3D stimuli) rapidly improves from about 12-16 weeks of age (and is not necessarily linked to eye alignment). It is thought that cortical development is the limiting factor in binocular function prior to this.
•Very young babies may exhibit exotropia which later disappears (after 6 months if not gone needs to be investigated), although the vast majority of children are born orthotropic.
describe the pattern of refractive error throughout childhood + what is the reason for this pattern (3)
Mean refractive error typically declines throughout childhood
start off hypermetropic - gradually become less hypermetropic as we age throughout early childhood years
this is due to emmetropisation
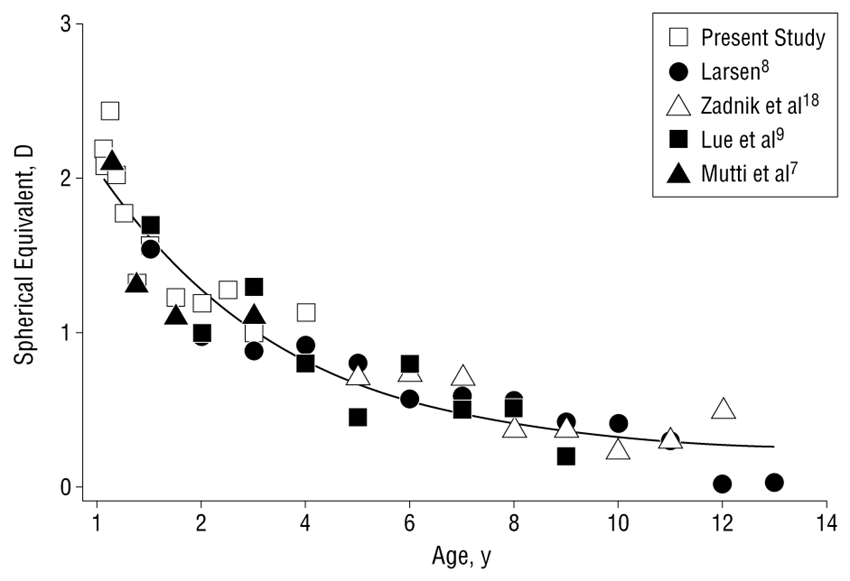
explain the term emmetropisaton (3)
In early childhood, the eye (through either a passive or active process) is attempting to reach emmetropia
It is growing in such a way that the combined optic power of the lens and cornea is tending towards a refractive error of 0.00DS (or low hyperopia)
SN: One of the biggest questions, is whether emmetropisation is a passive process guided by genetics, or whether it is influenced by environment
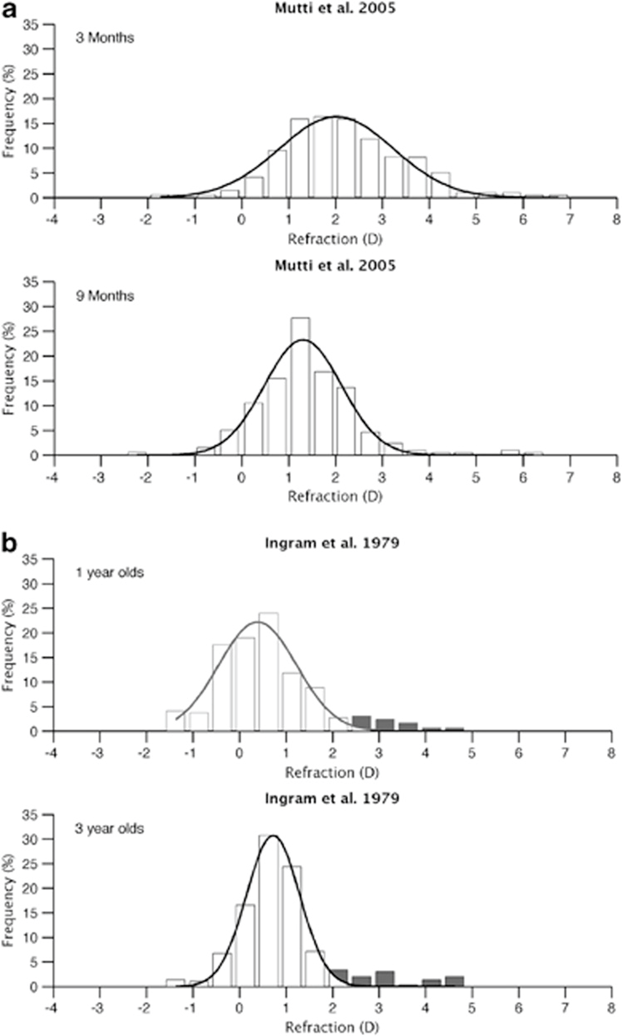
describe the shift in mean rx from birth to 3 years old (2)
•At birth the distribution is largely gaussian (normally distributed) with a mean refractive error of around +2.00DS
•By 3 years old the mean refractive error has shifted to around +0.75DS with a smaller standard deviation
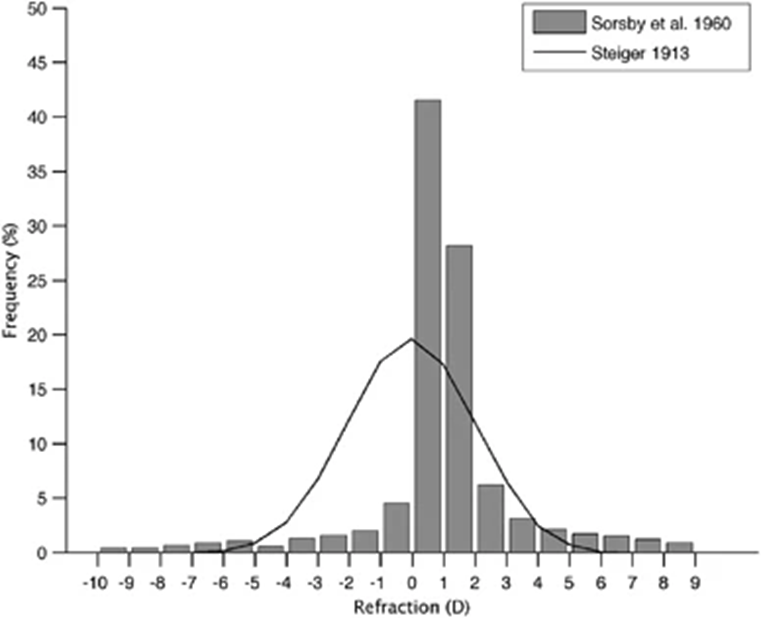
describe the distribution of rx in adults (in comparison to children/from birth) (2)
The distribution of refractive errors in adults shows a leptokurtotic distribution - (tall peak with more variation in the tails than a ‘normal distribution’)
there is a much greater distribution in the centre (0) as most people are emmetropic and then there are longer tails as more variation)
describe how eye growth was used to explain the theory of emmetropisation (3)
the eye grows from around 16.5mm at birth to 24mm as an adult – therefore there must be an increase in axial length
a study suggested that an increase of 0.35mm increases a myopic prescription by 1.00DS - so as the eye is growing it is becoming more myopic/less hypermetropic
however - this is not seen during early childhood! - and according to the above that = to 21D change - this is therefore NOT the reason for emmetropisation occurring
in terms of emmetropisation being a passive process - what does this mean and what are the 3 proposed mechanisms for this - explain each one
suggests that emmetropisation is a result of the natural growth and development of the eye – changes that could be said to be “pre-programmed”
1.Anterior chamber depth – this increases during childhood reaching adult levels by around 15 years. However, changes don’t appear to have a large role in changing refractive error.
2.Corneal power / curvature – data is equivocal in terms of the role it plays, some show a steepening of the radius of curvature whilst others show a flattening. Likely a very minor role compared to the…
3.Crystalline lens – this is thought to be largely responsible for the overall decrease in the refractive error as the eye grows/elongates. Research suggests that as the eye gets bigger it stretches the lens. This makes it thinner and reduces its dioptric power
explain the theory of emmetropisation being driven by an ACTIVE process (5)
emmetropisation is mediated by retinal blur - we can control this (with lenses)
Animal studies have used convex / concave lenses or form deprivation lenses during early life to simulate high refractive error / retinal blur
The eye deprived of clear visual input grows excessively becoming myopic
Interestingly if the goggles are removed the eye growth halts until the animal becomes emmetropic – suggests that myopic defocus is somehow “detected” and compensated for
High powered lenses of opposite powers (+ or -) can induce different types of retinal blur in each eye, and result in differing amounts of compensatory eye growth
why is understanding the theory of emmetropisation relevant in correcting and understanding rx in young children (3)
•It is important to consider possible barriers to emmetropisation – conditions that deprive eye completely of vision – eye becomes more myopic
•We should expect to see some degree of refractive error in very young children – as still tending to emmetropisation
•It is not always necessary to correct refractive errors in very young children (unless they have a strabismus etc.) – as we can disrupt emmetropisation – children may never become emmetropic (just monitor instead)
what else develops as well as emmetropisation that we have to consider
development of myopia !!!
By 2040 the global prevalence of myopia in children and teenagers is estimated to reach 36% (that’s 1 in 3), and is steadily rising
explain the factors that contribute to development of myopia in young children (5)
genetics
time spent doing near work
and possibly even exposure to sunlight/outdoors
The same retinal feedback mechanism that is thought to detect retinal blur and induce emmetropia (through a compensatory mechanism) is thought to be partly responsible for the development of myopia in young people
For example, when we focus on something close our accommodation system often demonstrates a small error (lag of accommodation), which causes hyperopic defocus on the retina (little bit of blur). This is thought to induce eye growth and ultimately myopia.
explain how correcting myopia can also contribute to myopic development (2)
Unfortunately, the concave lenses used to manage myopia (single vision lenses) also create peripheral hyperopic defocus, which is thought to contribute to myopia progression - exacerbates myopia
Strategies to overcome this and halt myopia progression are a major focus for research - CLs, different types of lens design, drops etc. - we cannot STOP myopia progression but can reduce it potentially
why is myopia development a problem (2)
px with myopia - particularly high myopia (as eye is longer than normal - stretching retina and other structures making them thinner and weaker
are at greater risk of conditions like: retinal detachment, glaucoma, AMD, choroidal neovascularisation etc.
describe the overall shift in rx from birth to early and late childhood depending on different factors (4)
in the early years of life we see this shift towards emmetropisation
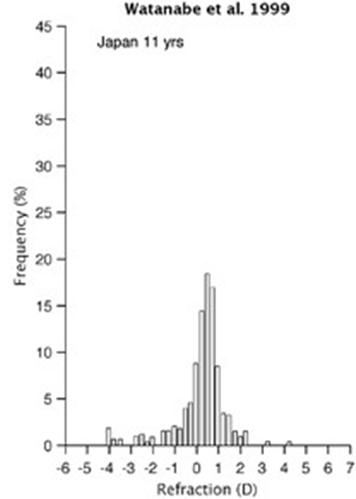
from around 6 years old we start to see changing distributions of refractive error depending on factors such as race/ethnicity/geographic location
For example, if we compare Australian children with Japanese children of the same age, there are more myopes in the Japanese cohort.
The prevalence of myopia can vary hugely from ~2% in 10 year old Norwegian children to ~55% in 10 year old Chinese children
describe the risk factors of myopia (4)
Children who spend more time outdoors (e.g. doing sports or outdoor activities) are less likely to develop myopia – mechanism not fully understood but could be linked to light increasing dopamine production (which may inhibit eye growth)
Children who perform prolonged near work (e.g. reading for >30mins continuously) or with a short working distance are more likely to become myopic (although some studies have found no link – so inconclusive?
Racial and ethnic differences in myopia prevalence exist – highest in east Asians (intense educational pressures?)
Hundreds of genes have now been associated with myopia, and these can be inherited. Having two parents with myopia is associated with a greater risk than one parent with myopia (which is a higher risk than no parents with myopia).
describe what amblyopia is (3)
Diminished visual acuity that does not result from any demonstrable anomaly of the eye or visual pathway and cannot be corrected with refractive correction”
poor vision resulting from a cortical visual impairment - inadequate stimulation of the visual system during the critical period of visual development
may be unilateral/bilateral
how do we clinically define amblyopia
a “two line” difference in acuity between the eyes – one eye is 6/6 and one eye is 6/9 or 6/12
prevalence of amblyopia
affects 1-3% of children in the UK
what is commonly / uncommonly associated with amblyopia in children
commonly associated with: heterotropia and/or uncorrected anisometropia (significant difference in rx between 2 eyes) in children and can have serious implications for their vision
uncommonly associated with: being caused by visual deprivation due to congenital cataract, ptosis etc…
explain what the critical period of visual development is in relation to amblyopia (4)
time period from birth to around 7-8 years old
during this time that the visual neurons in the brain are still ‘malleable’ (susceptible to change) - any problems during this period can be significant - Therefore the ‘critical period’ could be described as the time frame in which visual deprivation is effective in causing amblyopia
Beyond ~7-8 years old the visual system has matured, and is now in the state that it will remain in through adulthood. Visual deprivation after this age typically doesn’t have any detrimental effects on acuity
example: if someone got a cataract at 20 years old and it was removed after this their vision will be fine - however if a baby was born with a cataract as it is within this critical period time even after removal they will likely develop amblyopia
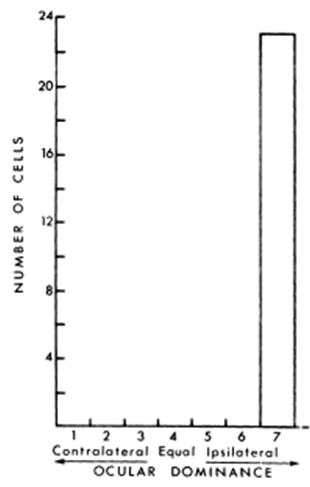
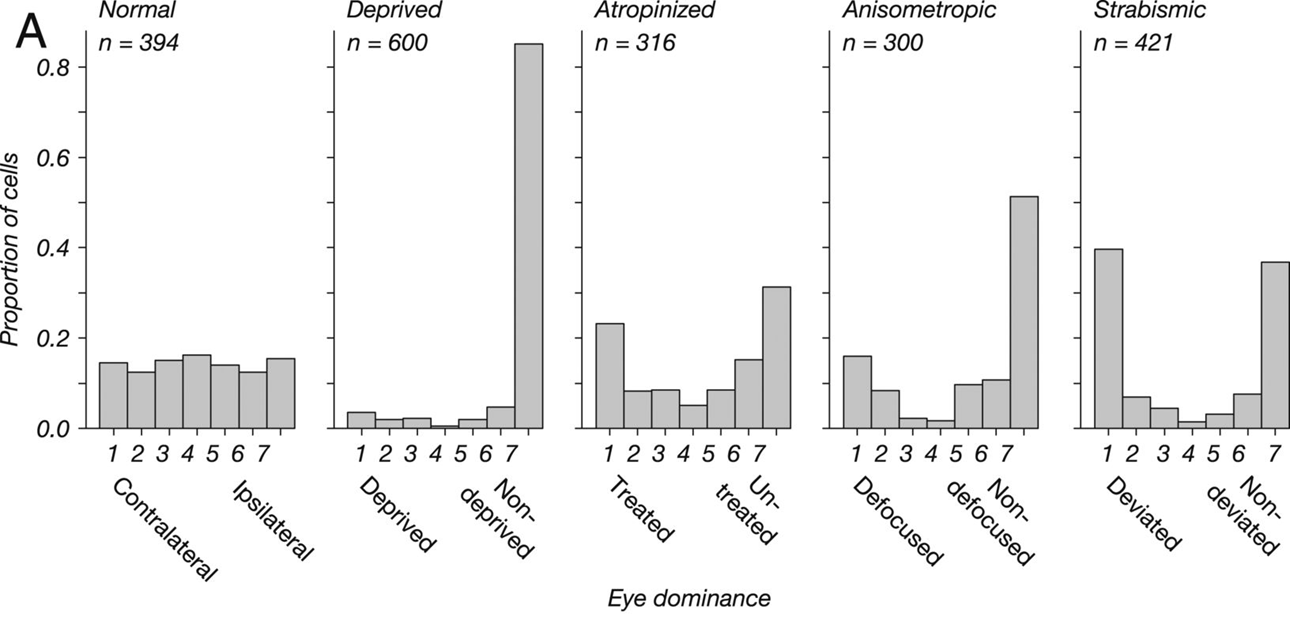
explain what ocular dominance columns are in relation to typical visual development (5)
this is a type of specialisation of cells in V1
it is the separation of neurons into ocular dominance columns – where each cell has a preference for input from one particular eye
This occurs because (in normal development) there is equal competition from both eyes for dominance – so both eyes become equally represented in the brain
Around 80% of neurons are “binocular”, leaving 20% to respond solely to input from one eye
Put simply, if a RE dominant cell receives a signal from the LE it will completely ignore it – there is no response, no change in firing rate.
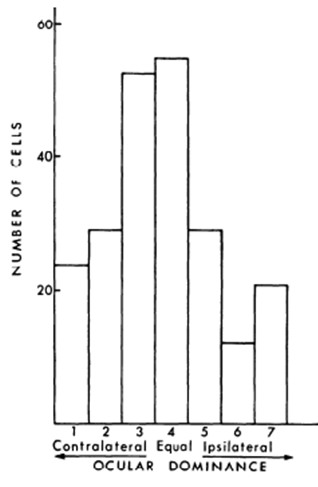
explain the effect of visual deprivation on ocular dominance columns (4)
depriving one eye of visual input at a young age causes physical changes in the brain
If an animal is deprived of sight in one eye from a young age (e.g. suturing the eyelid closed, or an occlusive contact lens) - the neurons undergo a change in function and begin to only respond to signals from the “good” eye (i.e. they are no longer binocular) - no longer any competition between 2 eyes and neurons for the other eye no longer develop
A loss of stereopsis is thought to follow
Shrinkage of ocular dominance columns is greatest when animals are monocularly deprived at a younger age - cataract at birth vs age 5 - worse case of amblyopia at birth, mild amblyopia at 5 years
why do strabismus and anisometropia cause amblyopia
they both cause a deprivation of some sort
Strabismus early in life leads to the inhibition of the signal from the deviated eye (suppression to prevent diplopia) - however dampens cellular response - like a form of monocular deprivation - so develop amblyopia
uncorrected anisometropia causes a type of deprivation in the affected eye (blurred retinal image results in little to no high spatial frequencies being seen) - differing amount of retinal blur on each retina - lose signal for brain to develop neurons for specialisation - so develop amblyopia
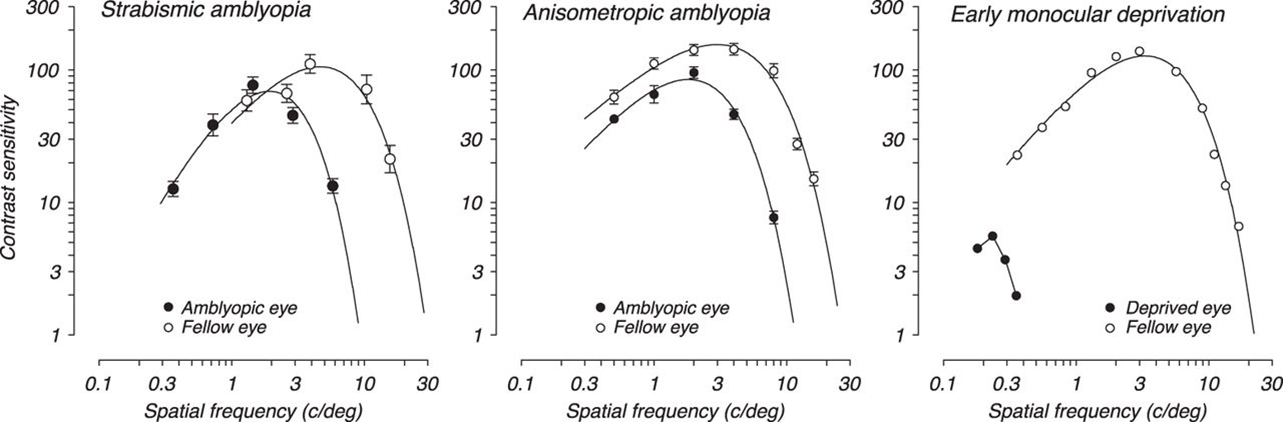
compare the effects of strabismic amblyopia vs anisometropic amblyopia (and mixed)
anisometropic amblyopes not only had reduced acuity but also poorer contrast sensitivity
whereas strabismic amblyopes showed only reduced acuity
Mixed amblyopes had the poorest functional vision.
summarize the causes of amblyopia
Resulting in suppression (due to a difficulty fusing, or rivalry), followed by amblyopia:
Strabismus (heterotropia) - will not be picked up unless tested in an eye examination
Uncorrected refractive error:
Anisometropia
High Rx - blurry retinal image
Astigmatism (meridional)
types of stimulus deprivation:
Congenital cataract
Ptosis
Corneal scar(trauma)
explain how the age of the child affects amblyopia developing following visual deprivation (3)
The younger the child, the more quickly amblyopia develops following visual deprivation
Roughly speaking, the age of the child tells you how many weeks of deprivation would cause amblyopia (up to the age of 5 years), for example:
A 1 year old child would develop amblyopia after one week of visual deprivation
A 4 year old child would develop amblyopia after four weeks of visual deprivation
The longer the period of deprivation, the more dense the amblyopia
clinically what do we need to be aware of with amblyopia (3)
•When testing young children you must always be on the lookout for amblyopia
•If detected, it is vital to try and establish the cause
Treatment (reversal?) of amblyopia is really only possible until the child is ~7 years old, so it is a time critical condition - brain has matured and also the fact that some children will not want to wear an eye patch etc.
how do we treat amblyopia
eye patch - covering up the good eye
px has to wear for a few hours of the day
successful treatment leads to 6/12 vision, 6/6 if lucky and strict motivation to the regime
what tests make up our clinical investigation/diagnosis of amblyopia (5)
Case history and observation - look for clues. Do they have a heterotropia? Significant anisometropia? Ptosis? Media opacities? Family history?
Cover test – is there a heterotropia (strabismus?)
Retinoscopy – is there significant anisometropia or a high Rx?
Ophthalmoscopy – there should be no other obvious cause of poor vision - amblyopic eye should look healthy
Pinhole – confirm that visual acuity doesn’t improve (reduces aberrations and can therefore indicate if there is residual uncorrected refractive error) - pinhole shouldn’t improve vision if px has amblyopia
SN: if you do suspect/know that a px has amblyopia do not ignore the affected eye - problems can still develop in this eye
explain the use of neutral density filter in investigating amblyopia
Neutral density filter – acuity is normally diminished when a neutral density filter is introduced, yet in amblyopia acuity remains similar to without the filter

what is the crowding effect (2)
Patients with amblyopia typically perform better on single letters rather than when reading the whole chart (or a single letter flanked by bars)
Letters surrounded by other letters or bars are more ‘crowded’


explain the relevance of the crowding effect to amblyopia investigation (3)
Px with amblyopia – do worse on a crowded chart than charts with a single letter - measuring VA on a single letter chart will underestimate vision loss in amblyopia
so we need to always use a crowded chart when testing vision in children especially – as can miss the amblyopia
SN: The crowding effect is less pronounced in anisometropic amblyopes, and more obvious in strabismic amblyopes