Weakness - Lower Motor Neurons
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
What parts of the body are considered to be part of the LMN pathway?
Ventral roots
Plexi
Peripheral nerve
Neuromuscular junction
Muscle
Do nerve roots exit the spinal cord at the level it leaves the cord?
Not always - in the lower spinal cord nerve roots descend past the termination of the spinal cord as part of the cauda equina.
Symptoms of a lesion in the cauda equina
Bilateral paralysis
Sensory loss
LMN signs
Loss of bladder / bowel function
Cauda equina syndrome
Compression of the cauda equina. This is a surgical emergency - if it is not decompressed quickly there is a threat of permanent paralysis.
Where are common places for nerve roots to be compressed?
The spaces between where nerves exit the spinal canal.
Radiculopathy
Compression of a nerve root
What are some common causes of radiculopathy?
A prolapsed intervertebral disc
Facet joint hypertrophy
Spondylolisthesis
Radiculitis
Symptoms of radiculopathy
Pain radiating down nerve
Dermatomal sensory loss +/- weakness in the site
LMN signs upon examination
Provocative manouevers elicit characteristic pain
Areflexia in an effected territory
LMN signs
Areflexia
Wasting
Lower Motor Neuron (LMN)
The efferent neuron of the peripheral nervous system (PNS) that connects the central nervous system (CNS) with the muscle to be innervated.
What are the symptoms of a plexus lesion?
The pattern of weakness does not conform to an individual root territory, nor peripheral nerve.
What is a serious condition that can lead to compression of the brachial plexus?
Pancoast tumour - an apical lung tumour that can invade lower segments of the brachial plexus.
Neurological symptoms of a Pancoast tumour
Weakness and wasting of the intrinsic hand muscles. This may the first sign of their cancer.
Typically any pain will be worse at night.
What can cause peripheral nerve lesions?
Compression
Inflammation
Tumours
And more
Mononeuropathy
Lesion affecting a single peripheral nerve.
Symptoms of a peripheral nerve lesion
Loss of function in the region supplied by the specific nerve
Usually sensory +/- motor features, though it may only have motor only features too
Saturday night palsy
Radial nerve palsy - can be more common in people who have been drunk the night before as they may fall asleep with their arm over the back of a chair and compress the nerve.
Carpal tunnel syndrome
Compression of the median nerve at the carpal tunnel
What time of day is the pain for carpal tunnel syndrome worse?
Typically night
How is carpal tunnel syndrome treated?
Surgery can be performed if it is serious, and if not serious, a splint is used.
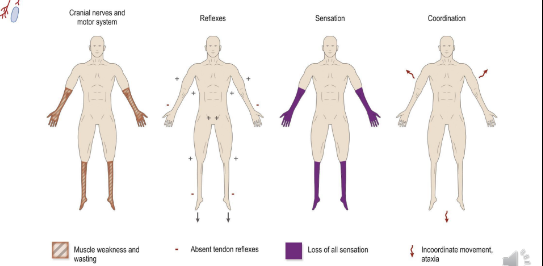
Polyneuropathy
Lesions affecting multiple nerves in multiple limbs (+/- cranial nerves).
What is the typical presentation of polyneuropathy?
Various patterns exist, but in general the longest nerves are damaged first creating a ‘glove and stocking’ sensory loss pattern (distal weakness)
Reflexes diminished / absent
Chronically, the condition can cause muscle wasting, and sometimes fasciculations
What can cause chronic polyneuropathy?
Toxic metabolic diseases
Diabetes
Chemotherapy
Alcoholism
Autoimmune disorders
Neuromuscular Junction (NMJ)
The synapse between motor neuron and muscle.
Typical presentation of issues at the NMJ
Sensation is normal
Reflexes are unaffected
Fatiguable weakness (sustained exertion on bedside testing causes decreasing power)
Symptoms may be worse at the end of the day (diurnal pattern)
Weakness affects:
Proximal muscles (eg. shoulders, hip girdle)
Ocular muscles (diplopia/gaze palsy, ptosis)
Bulbar muscles (dysarthria, dysphagia, loss of airway tone)
Neck muscles (head drop)
What causes fatiguable weakness
The NMJ runs out of acetylcholine.
What are some more common NMJ diseases?
Myasthenia Gravis
Lambert-Eaton syndrome
Myasthenia Gravis (MG)
An autoimmune condition that causes destruction of acetylcholine receptors at the NMJ. This results in fatiguable weakness in muscles under voluntary.
Typical presentation of MG
Ptosis (droopy eyelids), worsening upon sustained upgaze
Proximal muscle weakness, worse on sustained exertion
Intermittent double vision
Slurred speech
Difficult chewing and swallowing
Symptoms worse at the end of the day (diurnal)
Lambert-Eaton syndrome
An autoimmune syndrome that causes the destruction of calcium channels that facilitate the release of acetylcholine into the synaptic cleft.
How is MG treated?
Pyridostigmine (acetylcholinesterase)
Immunosuppression (steroids, azathioprine, IVIg)
Supportive measures (eg. feeding tubes, rehabilitation)
In some cases, surgery: association with thymoma (paraneoplastic disorder)
Avoid certain drugs which may worsen the disorder (e.g. gentamicin)
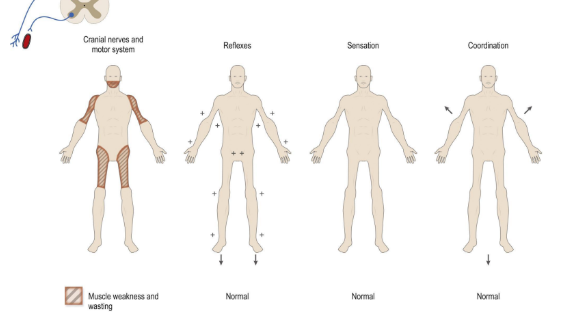
Myopathy
A general term referring to any disease that affects the muscles that control voluntary movement in the body.
Typical presentation of myopathy
Many different patterns exist
General pattern is proximal weakness (might cause difficulty getting up from a chair for example)
Fatiguability is not seen
Reflexes are generally preserved
Sensation is normal
Characteristic regions of atrophy (or hypertrophy)
Contractures
Pain
Dysmorphic features
Does hypertrophy mean muscles are stronger?
No, despite growth, they are often weak.
Polymyositis
Autoimmune disorder causing muscle inflammation. It can sometimes be associated with underlying cancer (paraneoplastic phenomenon).
What investigations might be performed on someone with polymyositis
Creatine Kinase test (will be elevated)
Muscle biopsy (will show invading lymphoid cells and inflammation)
How is polymyositis treated?
Immunosuppression: steroids, azathioprine/methotrexate, IVIg
Supportive measures: physiotherapy, OT, SLT
Screen for underlying cancer - and treat if present
Is MND a LMN disease?
No, it is a mixed upper and lower MN disease.
Typical presentation of MND
Mix of UMN and LMN and bulbar features affecting multiple regions
Gradual, insidious progression over months
Motor Neuron Disease (MND)
Motor neurone disease (MND) is a rare condition that progressively damages parts of the nervous system. This leads to muscle weakness, often with visible wasting. There is no cure, and it is unfortunately rapidly fatal.
What is the most common form of MND?
Amyotrophic lateral sclerosis
MND causes degeneration where?
In the descending corticospinal pathways, anterior horns, and peripheral motor nerves.