Chronic Kidney Disease and Dialysis
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
13 Terms
Kidney Functions
Regulate fluid volume and acid-base balance → ultrafiltrate produced at 125ml/ min
Excrete nitrogenous waste
Synthesize Erythropoietin (to produce RBCs) and 1,25-dihydroxycholecalciferol (active vit D) and renin
Metabolizes drugs
Target organ for parathormone and aldosterone
Chronic Kidney Disease (CKD)
Define
Stages
Define: Progressive loss of kidney function that persists for more or equal to 3 months → from direct damage to nephrons
Stage Classifications:
Stage 1: Normal or slightly decreased GFR associated with some kidney damage
Stage 2: Mildly decreased GFR
Stage 3: Moderately decreased GF to 50% of normal renal function\
Stage 4: Severely decreased GFR
Stage 5: Renal failure; More than 75% of renal function loss
What problems develop due to Renal failure
Azotemia: due to buildup of nitrogen compounds such as urea → not detectable yet
Use BUN test to detect
Uremia: urea in blood due to inability of kidneys to concentrate and filter sodium → decreased urine output, fluid overload
Hypertension due to urine output drop and NaCl retention
Hyperlipidemia, atherosclerosis and arterial hypertension, congestive heart failure
Insulin resistance
Metabolic Acidosis → sepsis
Hematologic abnormalities: anemia, leukocyte dysfunction and platelet dysfunction and coagulopathy
Impaired immunity
Renal osteodystrophy → no vit D synthesized → causes reduced intestinal absorption of calcium → leads to low serum calcium and increased serum phosphate → PTH increases
Secondary parathyroidism → decreased osteoblast activity and increased bone remodeling→ osteomalacia, osteitis fibrosa, osteosclerosis
What are the primary etiologic diseases that can cause CKF?
Diabetes
Hypertension
Chronic glomerulonephritis
Polycystic kidney disease
Pathophysiology of CKD
Various diseases can affect different segments of the nephron but eventually the entire nephron is lost and cannot be replaced
Early renal failure is usually asymptomatic due to compensatory hypertrophy of remaining nephrons
There might be underlying azotemia
Sodium pump loses effectiveness and sodium is excrete, polyuria occurs
As disease progresses, the compensatory mechanisms become overwhelmed, then signs and symptoms such as uremia appear
Clinical presentation
Few until Stage 3
Malaise, fatigue, headaches, nausea, loss of appetite and weight loss
Further progression →
Leg cramps, insomnia, nocturia, anemia (lethargy and dizziness)
Skin:
Hyperpigmentation (brown-yellow) due to retention of carotene-like pigments normally excreted by the kidney
Whitish coating on skin of trunk and arms is urea crystals left when perspiration evaporates→ “uremic frost”

Bone pain
Gastrointestinal: anorexia, nausea, vomiting, generalized gastroenteritis, peptic ulcer disease, malnutrition and diarrhea (from uremic syndrome)
Neurologic: mental slowness, depression, psychosis, peripheral neuropathy, muscular hyperactivity
Hemorrhagic episodes: occult GI bleeding, mucous membrane bleeding, skin manifestations, skin ecchymoses/petechiae, purpura
CV manifestations: congestive heart failure, hypertension, pericarditis
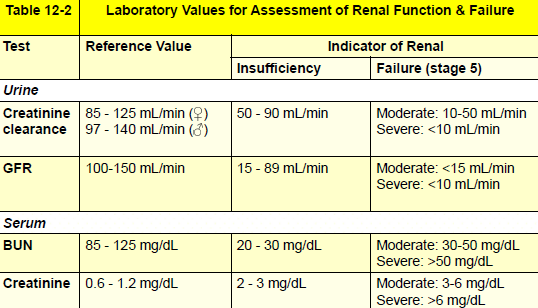
CKD Laboratory tests
GFR: Overall kidney function
Not detected until 20mL /minute
Urinalysis
Special emphasis on specific gravity
Principal marker of kidney damage is persistent protein in urine
BUN: Not as specific as creatinine clearance or serum creatinine level
Not detected until over 20mg/dL
Serum creatinine: Measure of muscle breakdown & filtration capacity of nephrons
Creatinine clearance: Proportional to the glomerular filtration and tubular excretion rates in a 24-hour urine collection
Not detected until 20mL/min
Serum electrolytes involved in acid-base regulation
Protein electrophoresis
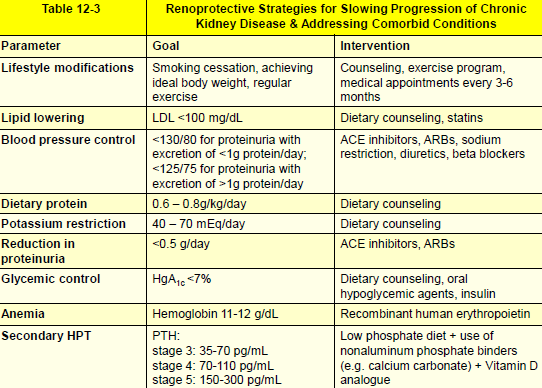
Medical management for each Stage of CKD
Stage 1&2:
Decrease retention of nitrogenous waste
Low-protein diet
Control fluid and electrolyte imbalances
Maintain fluid, sodium and potassium intake
Correct and control comorbid conditions such as diabetes, htn, chf and hyperparathyroidism
Adjust drug dosage: increase if drug does not bind strongly to protein (may be cleared by hemodialysis), decrease if GFR is below 60 (both antibiotics and analgesics but not anesthetics), single dose diazepines
Provide tx day after dialysis or at least 6 hrs after
Avoid bp cuff on arm with shunt
Avoid narcotics
Stage 3:
Manage anemia, malnutrition, bone disease
Stage 4
Care by nephrologist recommended and begin preparation for renal replacement therapy
Stage 5
Start dialysis and consider if eligible for renal transplant
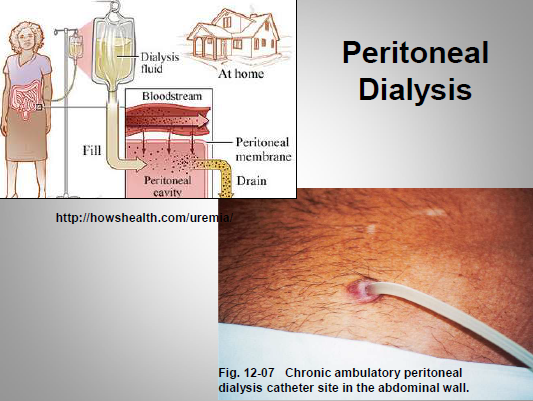
Dialysis
Define
Types: proas and Cons of each
Define: A medical procedure that artificially filters blood necessary when the number of nephrons diminishes to the point that azotemia is uncontrollable
Types
Peritoneal: hypertonic solution instilled into the peritoneal cavity through a permanent catheter and eventually the solution and urea are drawn out
Can be continuous at night or manually 4-5 times a day
Pros: low initial cost, ease of performance, reduced disease transmission and no need for anticoagulants
Cons: Frequent sessions needed due to lesser effectiveness, risk of peritonitis, common development of abdominal hernias
Hemodialysis: Method of choice, permanent surgically-created arteriovenous graft or fistula to which patients are plugged into and machine filters blood
Pros: only needed every 2-3 days
Cons: Heparin anticoagulant needed, still provides only about 15% of normal function → anemia, amyloidosis, improper calcium (m tetany and high PTH);
Increased risk of infection (HBV and HCV)
Staph aureus infection of fistula that can result in sepsis
Risk of antibiotic resistant infections
Bleeding tendencies due to anticoagulant and mechanical destruction by machine
Dental management of Patients with CKD
General considerations:
Monitor bp before and during tx
Alterations in drug dosages may be needed
May be taking large doses of corticosteroids so ensure they take them before tx to avoid adrenal crises
For invasive procedures, screen for bleeding disorders, obtain platelet count, hematocrit and hemoglobin to assess anemia
Anticoagulants may be needed: topical thrombin, microfibrillar collagen or systemic agents such as desmopressin
Antianxiety agents need little modifications: nitrous oxide and diazepam
Intravenous sedation: hematocrit or hemoglobin should be measured to ensure adequate oxygenation
CNS depressant drugs such as barbiturates and narcotics should be avoided in pts with uremia due to bbb not being intact and sedation may be excessive
Stage 3 and below: can be treated i an outpatient setting, conservative medical care and well controlled disease
Stage 4 or Higher: consult with physician first
Defer tx if uncontrolled disease or comorbidity
Consult with physician to assess if they need antibiotics after surgical procedure
CKD Oral manifestations
Mucosal anemia (oral pallor)
Red-orange discoloration due to carotene-like pigment deposition
Salivary flow may be diminished → causing xerostomia and parotid infections
Candidiasis

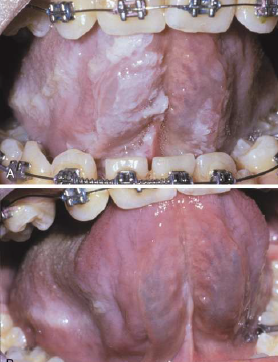
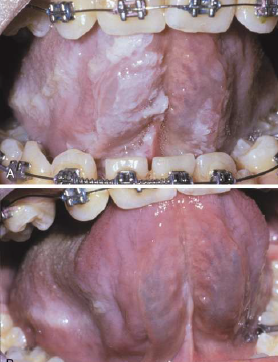
Uremic Stomatitis: adherent white plaques on buccal mucosa, tongue, floor of the mouth
Altered pH due to high urea, ammoniac/urine breath odor
Altered or metallic taste: bleeding tendency in labial, buccal, soft palate, tongue margins and gingival bleeding
Poor oral hygiene, gingivitis and periodontal disease in pt over stage 3
Increased incidence of lesions: ulcers, lichen planus, lichenoid-like lesions, hairy tongue, hairy leukoplakia, pyogenic granulomas
Osseous changes in Triad: loss of lamina dura, demineralized bone (ground glass appearance), localized radiolucent jaw lesions (central giant cell granulomas from secondary hyperthyroidism)
If ESRD begins at an early age: enamel hypoplasia, tooth erosion from vomiting, red-brown discoloration of enamel, slight delay on eruption, pulp narrowing, caries
CKD Secondary Hyperparathyroidism Oral manifestations
Dental abnormalities: widened pulp chamber, developmental defects, eruption alteration, weak teeth,
Brown tumor
Loss of bone density
Soft tissue calcification