Lecture 4 -2 Bipolar Disorders and suicide
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
61 Terms
Bipolar disorder Symptoms
Unlike those experiencing depression, people in a state of mania typically experience dramatic and inappropriate rises in mood
Emotional symptoms in bipolar disorder
Motivational symptoms in bipolar disorder
Behavioral symptoms in bipolar disorder
Cognitive symptoms in bipolar disorder
Physical symptoms in bipolar disorder
Diagnosing bipolar disorders
Two kinds of bipolar disorder (DSM-5)
Bipolar I disorder
Bipolar II disorder
Worldwide, 1 to 2.6 percent of all adults have bipolar disorder at any given time: 4 percent have it at some point in life
No gender differences, but higher rates in low-income populations
Manic episode
For 1 week or more, person displays a continually abnormal, inflated, unrestrained, or irritable mood as well as continually heightened energy or activity, for most of every day
Person also experiences at least three of the following symptoms for Manic episode
Grandiosity or overblown self-esteem
Reduced sleep need
Rapidly shifting ideas or the sense that one’s thoughts are moving very fast
Attention pulled in many directions
Heightened activity or agitated movements
Excessive pursuit of risky and potentially problematic activities
Bipolar I disorder
Occurrence of a manic episode
Hypomanic or major depressive episodes may precede or follow the manic episode
Bipolar II disorder
Presence or history of major depressive episode(s)
Presence or history of hypomanic episode(s)
No history of a manic episode
Cyclothymic disorder (DSM-5)
Numerous periods of hypomanic symptoms and mild depression symptoms
Symptoms continue for two or more years, with normal moods for days or weeks in between
No gender differences
May evolve into bipolar I or bipolar II
What Causes Bipolar Disorders?
Throughout the first half of the twentieth century, the search for the cause of bipolar disorders made little progress.
More recently, biological research has produced some promising clues
These insights have come from research into neurotransmitter activity, ion activity, brain structure, and genetic factors
Biological research and perspectives - Neurotransmitter activity
Mania may be related to high norepinephrine activity along with a low level of serotonin activity (“permissive theory”)
Biological research and perspectives - Ion activity
Improper transport of ions back and forth between the outside and the inside of a neuron’s membrane
Biological research and perspectives -Brain structure
Brain imaging and postmortem studies have identified a number of abnormal brain structures in people with bipolar disorder —in particular, the basal ganglia and cerebellum
Not clear what role such structural abnormalities play
Genetic factors
Many theorists believe that people inherit a biological predisposition to develop bipolar disorders
Family pedigree studies
Molecular biology techniques
Treatments for Bipolar Disorders
Before 1970, treatments for people with bipolar disorders were largely ineffective
In 1970, FDA approved the use of lithium
Mood-stabilizing (antibipolar) drugs were later developed
Lithium
Very effective in treating bipolar disorders and mania
Determining the correct dosage for a given patient is a delicate process
Too low = no effect
Too high = lithium intoxication (poisoning)
Other mood stabilizers
Some patients respond better to other drugs or to combinations of drugs
Effectiveness of lithium and other mood stabilizers
More than 60 percent of patients with mania improve on these medications
Most individuals experience fewer new episodes while on the drugs
These drugs may help prevent symptoms from developing
Mood stabilizers also help those with bipolar disorder overcome their depressive episodes, albeit to a lesser degree
Adjunctive psychotherapy
Psychotherapy or mood stabilizing alone is rarely helpful for persons with bipolar disorder
Individual, group, or family therapy is often used as an adjunct to lithium (or other medication-based) therapy
Adjunctive therapy improves a variety of client behaviors, especially in those persons with a cyclothymic disorder
Unipolar depression factors
Biological abnormalities
Positive reinforcement reduction • Negative thinking
Perception of helplessness
Life stress
Sociocultural influences
Bipolar depression factors
• Biological abnormalities
Inherited
Stress triggered
What are
the one-year prevalence
female-to-male ratio
typical age at onset
prevalence among first-degree relatives
percentage receiving treatment for Major Depressive Disorder?
Prevalence: 8.0%
Female-to-Male Ratio: 2:1
Typical Age at Onset: 18−29 years
Prevalence Among First-Degree Relatives: Elevated
Percentage Receiving Treatment: 50%
What are
the one-year prevalence
female-to-male ratio
typical age at onset
prevalence among first-degree relatives
percentage receiving treatment for Persistent Depressive Disorder (with dysthymic syndrome)?
Prevalence: 1.5−5.0%
Female-to-Male Ratio: Between 3:2 and 2:1
Typical Age at Onset: 10−25 years
Prevalence Among First-Degree Relatives: Elevated,
Percentage Receiving Treatment: 62%
What are
the one-year prevalence
female-to-male ratio
typical age at onset
prevalence among first-degree relatives
percentage receiving treatment for Bipolar I Disorder?
Prevalence: 1.6%
Female-to-Male Ratio: 1:1
Typical Age at Onset: 15−44 years
Prevalence Among First-Degree Relatives: Elevated
Percentage Receiving Treatment: 49%
What are
the one-year prevalence
female-to-male ratio
typical age at onset
prevalence among first-degree relatives
percentage receiving treatment for Bipolar II Disorder?
Prevalence: 1.0%
Female-to-Male Ratio: 1:1
Typical Age at Onset: 15−44 years
Prevalence Among First-Degree Relatives: Elevated
Percentage Receiving Treatment: 49%
What are
the one-year prevalence
female-to-male ratio
typical age at onset
prevalence among first-degree relatives
percentage receiving treatment for Cyclothymic Disorder?
Prevalence: 0.4%
Female-to-Male Ratio: 1:1
Typical Age at Onset: 15−25 years
Prevalence Among First-Degree Relatives: Elevated
Percentage Receiving Treatment: Unknown
Suicide
Suicide is one of the leading causes of death in the world
Approximately 1 million people die by suicide each year worldwide, including more than 42,000 in the United States
Classification
Not officially classified as a mental disorder in DSM-5
Suicidal behavior disorder has been proposed for the next revision
Definition of Suicide
Self-inflicted death in which one makes intentional, direct, and conscious effort to end one’s life
Intentional death
Death seeker
Death initiator
Death ignorer
Death darer
Non-suicidal self-injury
The deliberate, self-directed damage to body tissue without suicidal intent and for purposes not socially or culturally sanctioned.
Increases capability for suicide, which increases the risk later in life
Suicide rates vary
Country to country
Gender and marital status
Race and ethnicity
Social environment
Religious devoutness (not exclusively affiliation)
Underreporting may exist
Common triggers
Stressful events
Mood and thought changes
Alcohol and other drug use
Mental disorders
Modeling
Stressful events and situations for suicide = Immediate stressors
Loss of loved one through death, divorce, or rejection
Loss of job or significant financial loss
Natural disasters
Stressful events and situations for suicide = Long-term stressors
Social isolation
Serious illness
Abusive or repressive environment
Occupational stress
Mood and thought changes
Many suicide attempts are preceded by changes in mood and shifts in thinking patterns
Hopelessness
Sadness, anxiety, tension, frustration, shame
Psychache
Dichotomous thinking
Alcohol and other drug use
70 percent of suicide at tempters drink alcohol just before the act
One-fourth of these people are legally intoxicated
Use of other kinds of drugs may have similar ties to suicide, particularly in teens and young adults
Mental disorders
The majority of suicide attempters have a psychological disorder
Unipolar or bipolar depression (70 percent)
Chronic alcoholism (20 percent)
Schizophrenia (10 percent)
• Risk increases with multiple disorders
Other psychological disorders to triggers a suicide
Posttraumatic stress disorder (PTSD)
Panic disorder
Substance use disorder
Often in conjunction with schizophrenia or borderline personality disorder
Modeling: Contagion of suicide
A suicidal act appears to serve as a model for other such acts, especially among teens
Common models
Family members and friend
Celebrities
Highly publicized cases
Coworkers and colleagues
Interpersonal-psychological theory (Joiner et al.)
Perceptions related to desire for suicide
Perceived burdensomeness
Thwarted belongingness
Psychological ability to carry out suicide (capability for suicide)
Important to examine variables collectively
Biological view of Suicide
Genetics
Early twin studies port to genetic links to suicide
Brain development
Low serotonin activity and abnormalities in depression-related brain circuits contribute to suicide
Both aid in the production of aggressive feelings and impulsive behavior
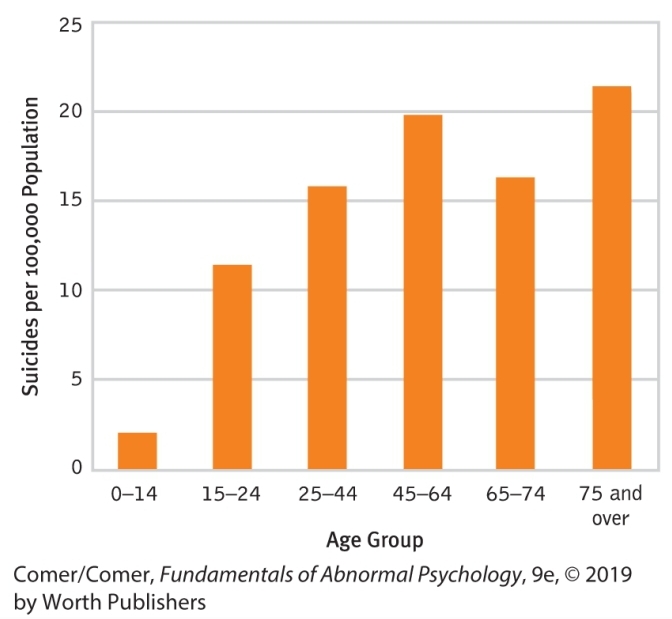
Is Suicide Linked to Age?
Children - Suicide
Suicide is infrequent among children
Suicide by very young is often preceded by behavioral struggles
Many child suicides appear to be based on a clear understanding of death and a clear wish to die
Adolescents - Suicide
Suicidal actions become much more common after the age of 13
About 8 of every 100,000 U.S. teenagers commit suicide yearly
12 percent have persistent suicidal thoughts
4 to 8 percent make suicide attempts
Teenage suicide links
Developmental stress of adolescence
Long- and short-term stressors, especially among LGBTQ teens
Clinical depression, low self-esteem, hopelessness
Anger, impulsiveness, alcohol or drug problems
Internet and in-person modeling
Factors linked to suicide attempts for Adolescents
Competition for jobs, college position, academic and athletic honors
Weakening family ties
Availability of alcohol/drugs
Mass media
Far more teens attempt suicide than succeed
Ratio may be as high as 200:1
The Elderly - suicide
U.S. elderly are most likely to commit suicide and most successful
Contributory factors of suicide in Elderly
Illness
Loss of close friends and relatives
Loss of control over one's life
Loss of social status
Treatments after suicide attempts
Medical care
Appropriate follow-up with psychotherapy or drug therapy
Therapies for Suicide.
Psychodynamic
Drug therapy
Group and family therapies
Cognitive - behavioural therapy
Mindfulness - based
Dialectical Behaviour
Therapy goals after suicide attempts
Keep the patient alive
Reduce psychological pain
Achievement of nonsuicidal state of mind and a sense of hope
Development of better ways of stress management
Suicide prevention
Prevention programs and crisis hotlines
Staffed by professionals or paraprofessionals
Offered through various modalities
Suicide prevention goals for initial contact
Establishing a positive relationship
Understanding and clarifying the problem
Assessing suicide potential
Assessing and mobilizing the caller's resources
Formulating a plan
Longer-term prevention of Surcide
Referral
Therapy
Reduction of access to common suicide means
Do suicide prevention programs work?
Assessment of program effectiveness is difficult
Variety of program types, variables, and confounds
Mixed results
• Accurate suicide risk assessment is elusive
Newer assessment approaches for suicide prevention programs
Nonverbal behaviors
Psychophysiological measures
Brain scans
Self-Injury Implicit Association Test
Following the break-up with his girlfriend, Eduard (27) has been feeling down for the past week, complaining that he has difficulties concentrating, is unable to sleep but feels nonetheless tired, feels agitated, and has been gaining some weight. He does not, however, have a history of mania. According to the DSM-5, Eduard would classify for the following diagnosis:
No disorder