Periodontolo'gy- CH. 7 Mucogingival deformities and conditions around teeth
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
62 Terms
Define mucogingival
The portion of the oral mucosa that covers the alveolar process including gingiva and alveolar mucosa
Define mucogingival deformity and condition
Any type of defect that is associated with a deviation of normal anatomic/morphologic relationship between the gingiva and the alveolar mucosa
Which age range is susceptible to mucogingival deformities?
All age groups
T/F Mucogingival deformities can affect a tooth or implant
True
T/F Mucogingival deformities can occur within the presence or absence of periodontitis
True
Name 6 mucogingival deformities and conditions:
Gingival/Soft tissue recession
Lack of keratinized gingiva
Decreased vestibular depth
Aberrant frenum/muscle position
Gingival excess
Abnormal color
Mucogingival deformities can affect what aspects of the tooth or periodontium
-form
-function
-esthetics
Most common type of mucogingival deformity?
-gingival/soft tissue recession
T/F Variations in periodontal anatomy which have no clinical significance are considered within the spectrum of normal findings and are commonly found
True
-not all variations of anatomy are considered abnormal
Define Normal mucogingival condition
the absence of diseased state-Ex. absence of recession, gingivitis, periodontitis
Name 3 examples of normal mucogingival conditions due to the fact that they are commonly found in the absence of underlying disease. These conditions are typically due to developmental reasons.
-Lack of keratinized tissue
-Decreased vestibular depth
-Aberrant frenum
T/F Periodontal health is impossible to maintain with proper oral hygiene measures and Periodontal treatment in the presence of a mucogingival deformity/ condition
False, It can be maintained
Define periodontal biotype/phenotype
describes features of the periodontium such as gingival thickness, gingival width, and shape of dental crown that are influenced by genetic and environmental factors
What are three descriptions that your periodontal biotype defines?
-Gingival biotype
-Bone morphology
-Tooth dimension
Define gingival biotype
describes gingival thickness and width of keratinized tissue
Define bone morphology
describes the thickness of the buccal bony plate
T/F There is no correlation between certain types of periodontal biotypes and certain mucogingival deformities/conditions
False, there is a strong correlation
Name the three periodontal biotype categories that one may be categorized as
-Thin-scalloped gingival biotype
-Thick-scalloped gingival biotype
-Thick-flat gingival biotype
What are the 6 characteristics of a thin-scalloped gingival biotype?
-triangular shaped crown
-thin, delicate soft tissue (transparent)
-thin alveolar bone
-narrow zone of keratinized tissue
-scalloped gingival margin
-greater tendency for onset and progression of mucogingival deformity and trauma
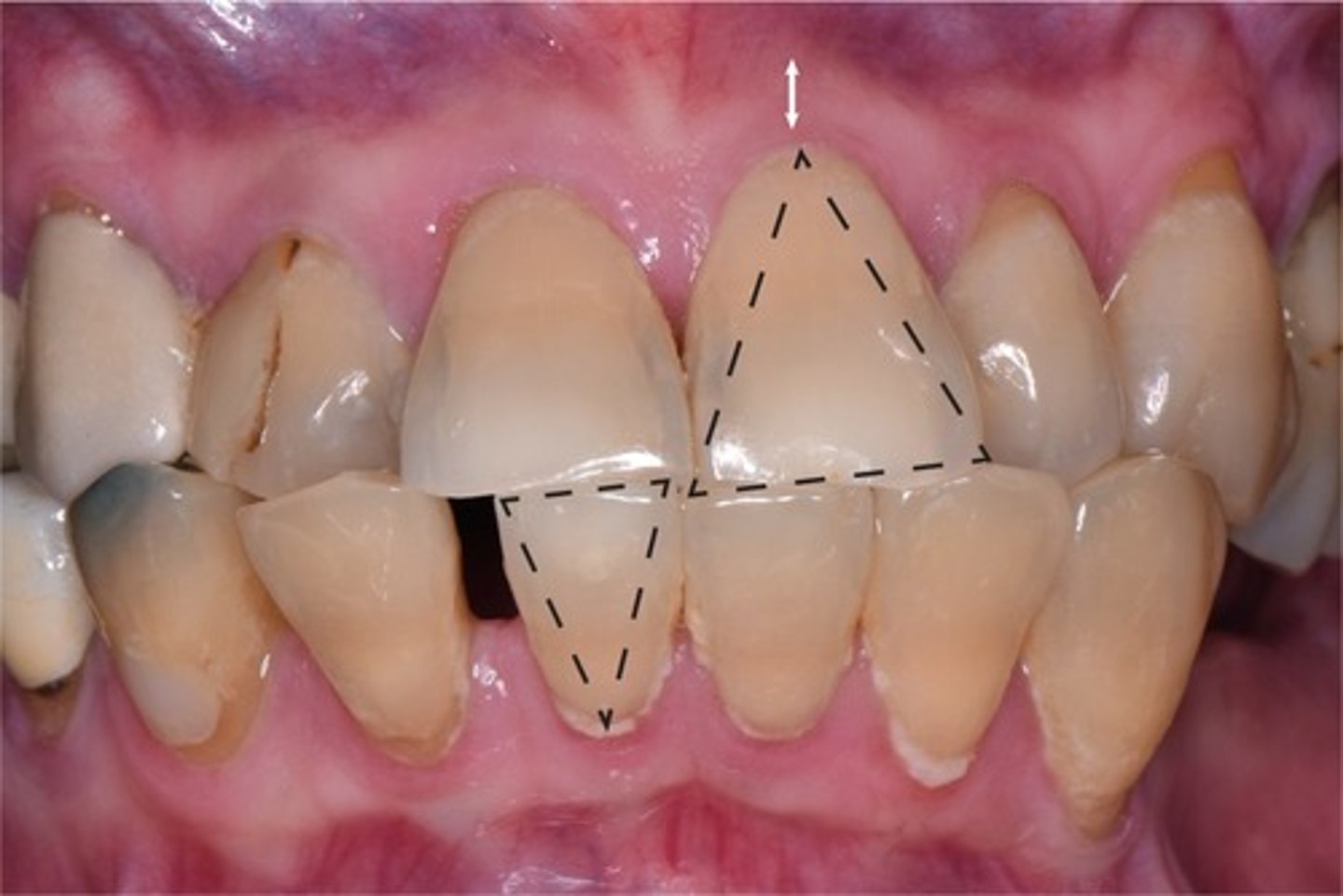
What are the 6 characteristics of a thick-scalloped gingival biotype?
-triangular shaped crown
-Thick, fibrotic gingiva
-thin bone
-narrow to moderate zone of keratinized tissue
-scalloped margin
-prone to development of mucogingival deformity and trauma
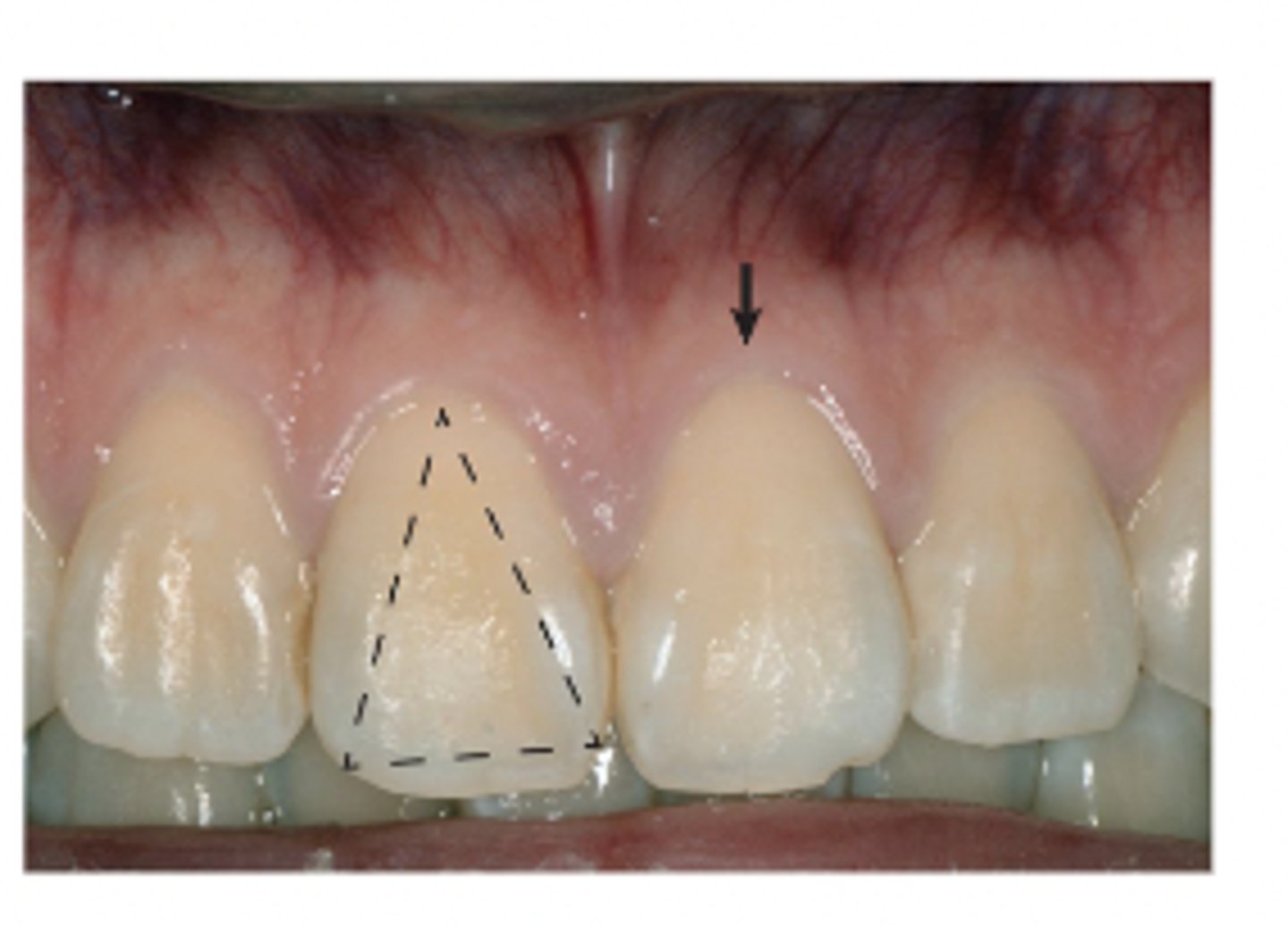
What are the 6 characteristics of a thick-flat gingival biotype?
-Wide, square shaped crown
-thick, dense, and fibrotic tissue
-thick bone
-Wide band of keratinized tissue
-flat margin contour
-More resilient and less susceptible to inflammation, trauma, and deformities (optimal for periodontal health)
Key difference in thin vs. thick scalloped crown shape?
Thick scalloped is not as friable and delicate as thin biotype
T/F Periodontal biotype can vary among different teeth within the SAME person/mouth?
True
Why is it important to assess and identify the different phenotypes within a patients mouth? (3)
-assess for risk and/or progression of mucogingival deformities
-allows time to possibly mitigate (prevent) or preempt (stall) the development
-implement life style changes to minimize risk
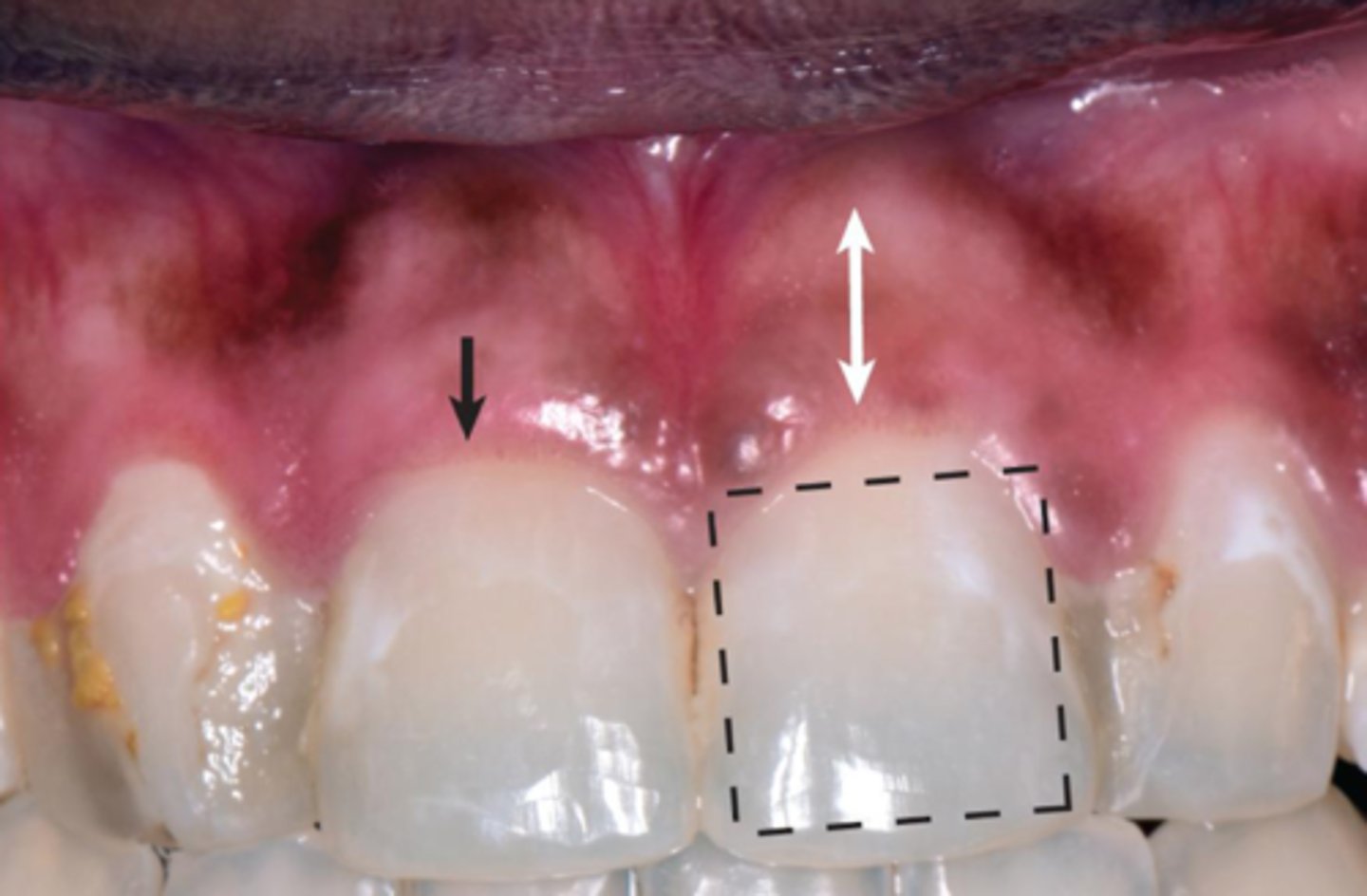
Define gingival recession
movement of gingival margin apically to the CEJ
What is the most common mucogingival deformity?
gingival recession
Gingival recession can affect any age group however the likely hood of it happening increase/decreases with age
Increases
What corresponds with the attachment loss that exposes the root surface to the oral enviorment?
gingival recession
Name three issues that gingival recession can be associated with:
-esthetically unpleasing
-dentin hypersensitivity
-carious or non carious cervical lesions (ex. abrasion)
Name 5 risk factors for gingival recession?
-Thin tissue biotype
-Narrow band of keratinized tissue
-Reduced thickness of bone (due to abnormal tooth position)
-Mechanical trauma
-Orthodontics
How can you determine if tissue is thick or thin?
Insert probe into sulcus:
-if you can see the probe through the tissue it is thin
-If you cannot see the probe it is thick
Tissue that is considered thin is less than or equal to how many millimeters?
1
Tissue that is considered thick is greater than how many millimeters?
1
Keratinized tissue zone includes what structures? Measured from where to where?
-free and attached gingiva
-Measured from margin to mucogingival junction
Why is a broad band of keratinized tissue desired?
-offered greater resistance to recession
Which biotypes are susceptible to recession? Why?
-thick and thin scalloped biotypes
-have less resistance to mechanical forces due to lack of keratinized tissue
What is the desired amount of keratinized tissue and gingiva for periodontal health?
-2mm of keratinized tissue
-1mm of keratinized gingiva
T/F There is a minimum amount of keratinized tissue needed to prevent attachment loss when optimum biofilm control is present
False, there is no minimum of keratinized tissue is required for health if optimal biofilm control is present
How can mechanical trauma promote recession?
Ex.
-improper brushing technique
-aggressive brushing
-use of hard bristled toothbrush
How is orthodontics a risk factor for gum recession?
If it results in the movement in a buccal or facial direction
What is the miller classification system based on?
level of gingival margin with respect to mucogingival junction and underlying alveolar bone
How many categories are in the miller classification system?
4
Class 1 of miller classification system?
-Marginal tissue that does not extend to mucogingival junction (MGJ)
-100% of root coverage can be anticipated
-Interdental papilla still present
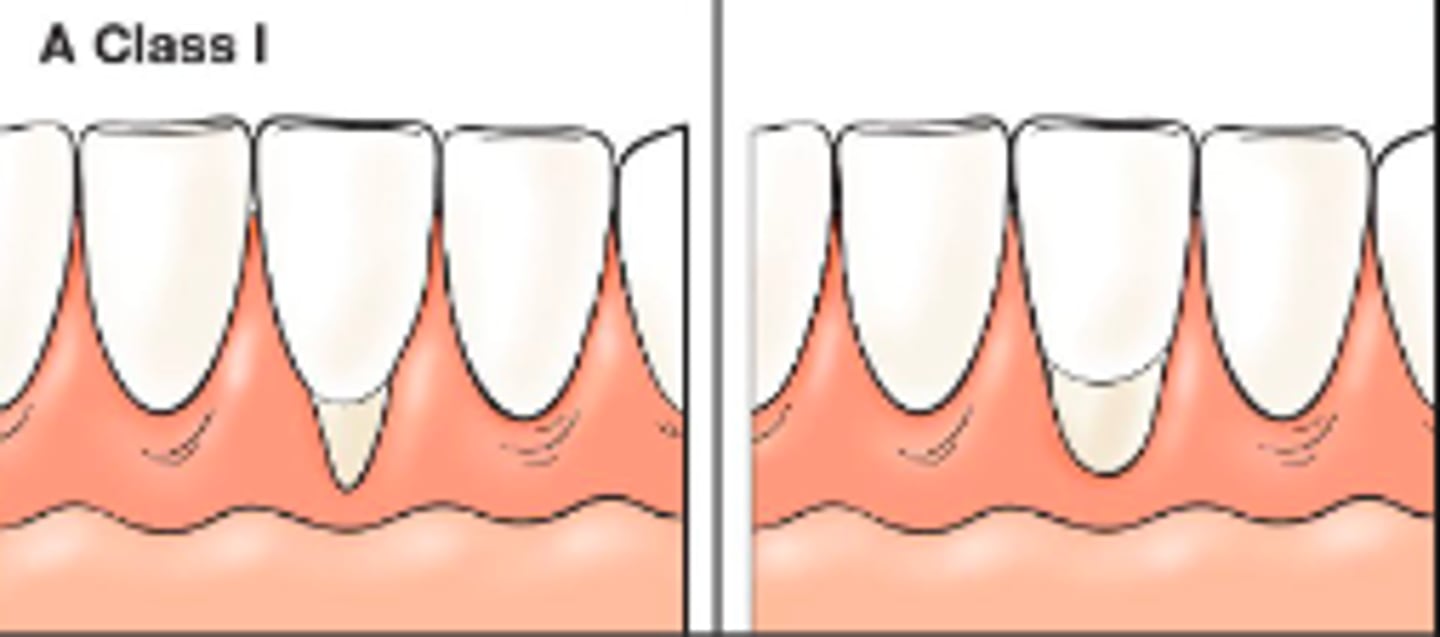
Class 2 of miller classification system?
-Marginal tissue recession that extends to or beyond MGJ
-Interdental papilla still present
-100% root coverage can be anticipated

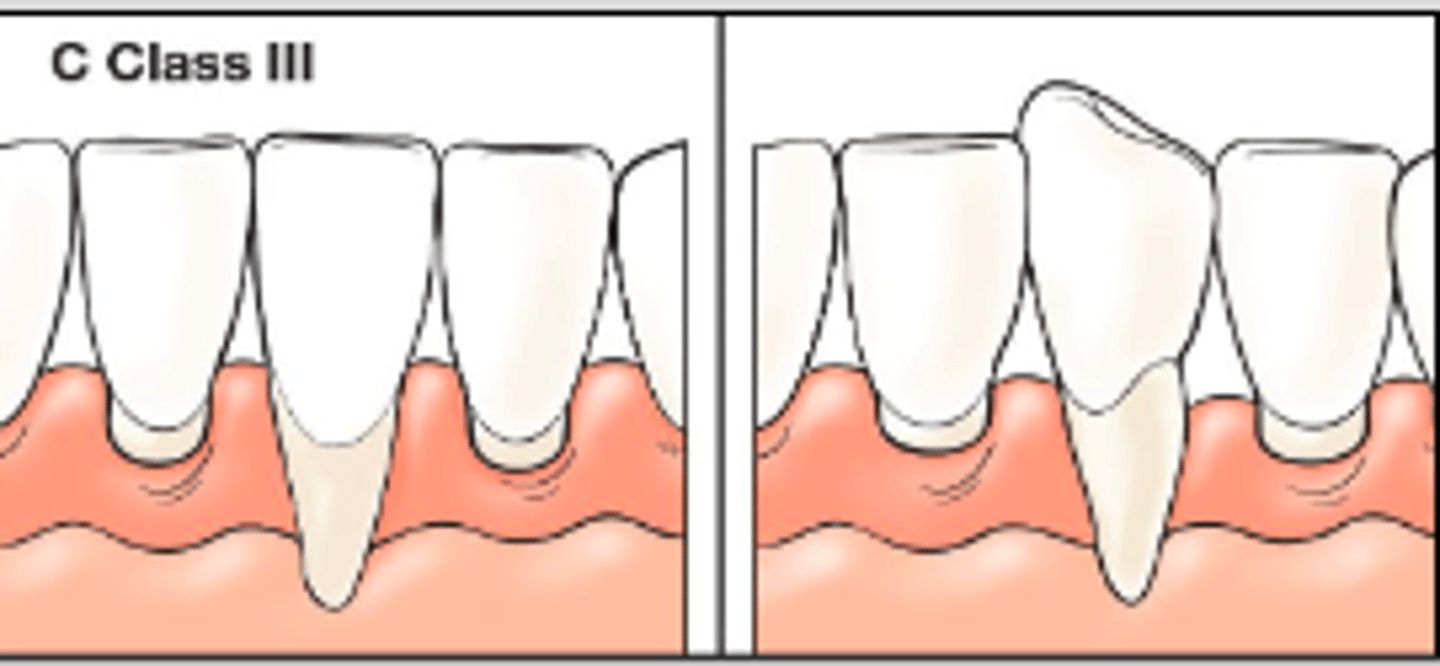
Class 3 of miller classification system?
-Marginal tissue recession that extends to or below the MGJ
-interdental bone or soft tissue loss and/or mispositioning of teeth
-Partial root coverage
Class 4 of miller classification system?
-Marginal tissue recession that extends beyond MGJ
-may have mispositioned tooth
-severe loss of interdental bone and papilla to level corresponding to apical extent of marginal tissue recession
-No root coverage anticipated
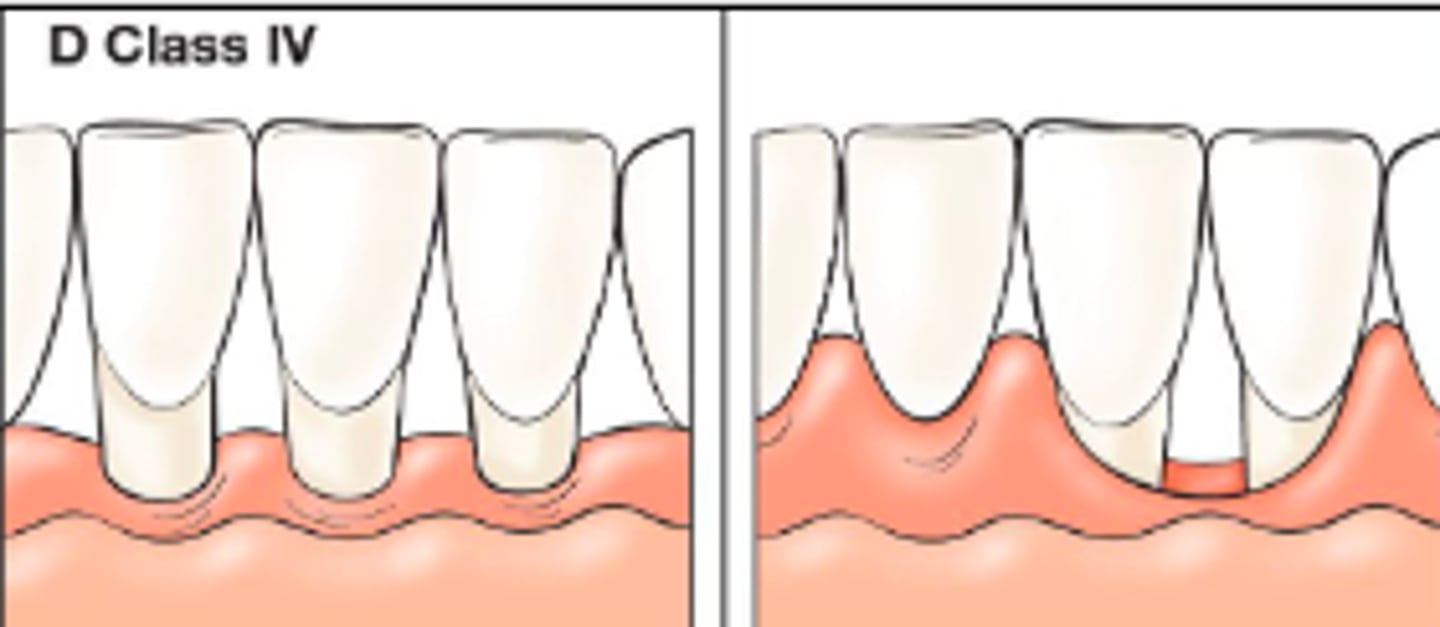
3 critics of the miller classification system?
-hard to identify exact location of apical extent from MGJ to differentiate class 1 from 2
-Does not define amount of interdental bone/tissue to differentiate class 3 from 4
-Not reliable and has never been tested in a clinical setting
What is the Cairo classification system?
Newer classification system for gingival recession
What is the Cairo classification system based on?
clinical attachment level measurement at buccal and interproximal sites
Why is the Cairo classification system preferred over millers? (2)
-uses objective identifiable criteria
-more reliable
How many types of recession are in Cairo classification system?
3
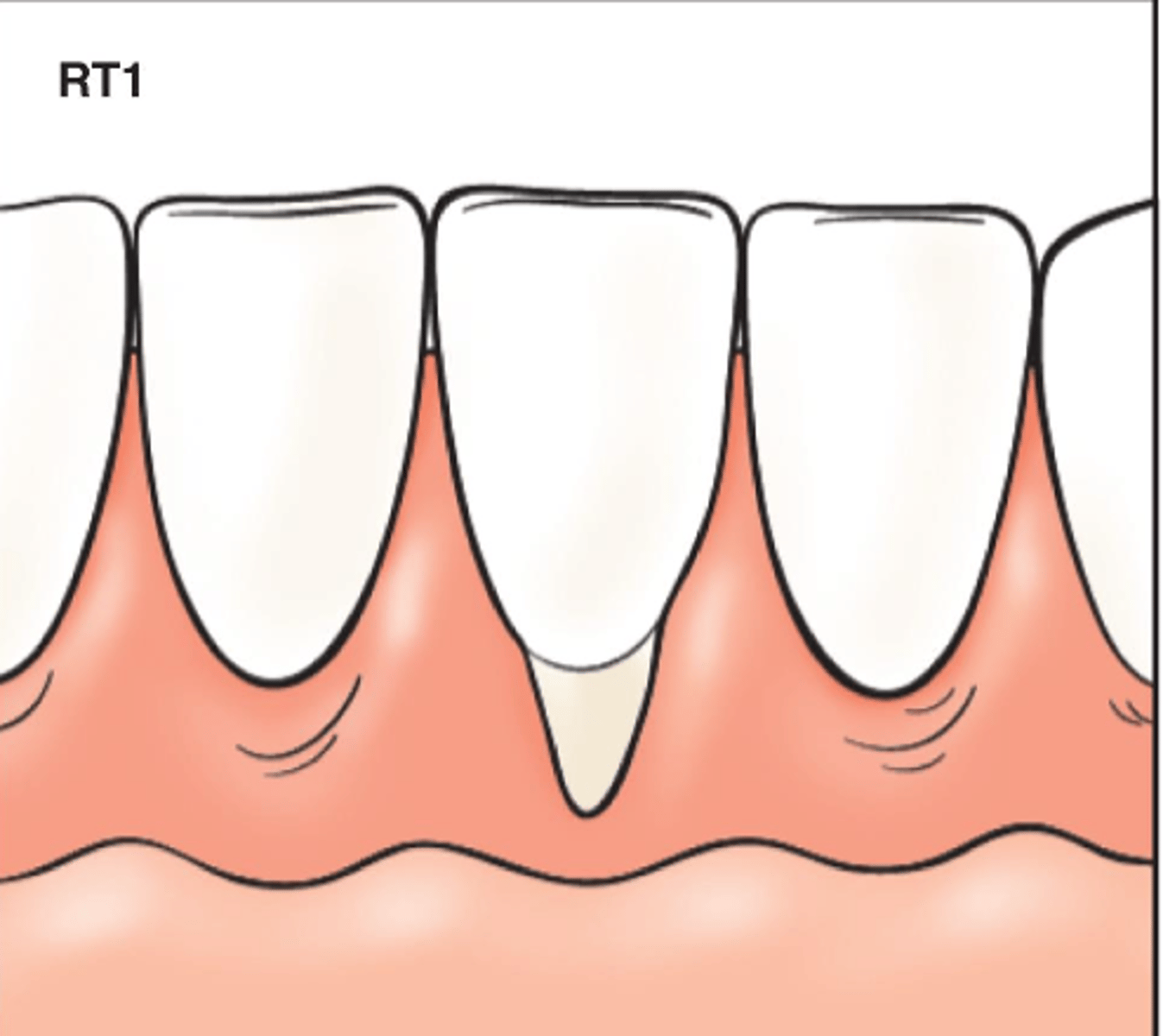
Recession type 1 (RT1) of Cairo classification system?
-Gingival recession with no loss of interproximal attachment
-interproximal CEJ is not visible
-Most likely due to traumatic toothbrushing
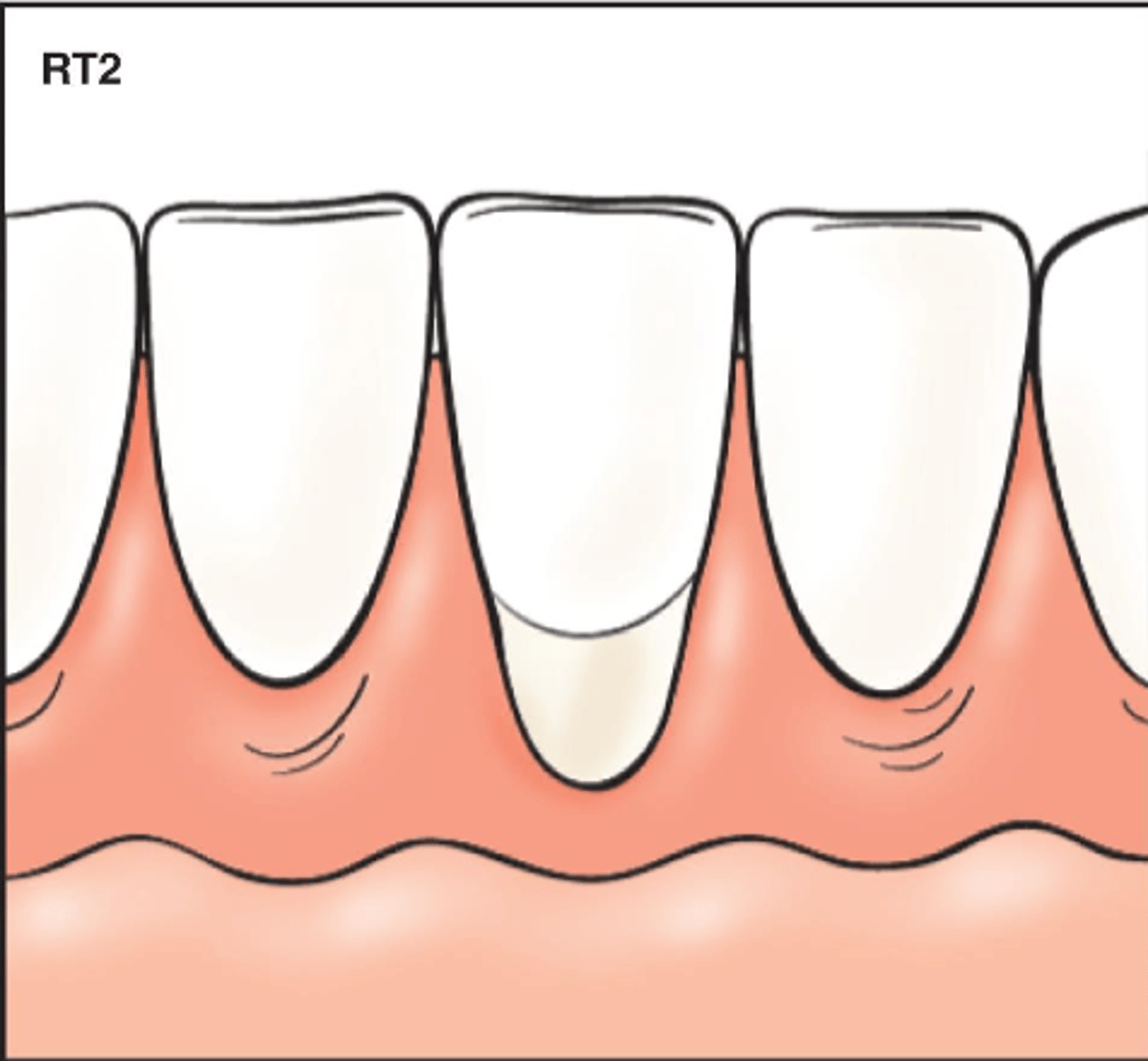
Recession type 2 (RT2) of Cairo classification system?
-Gingival recession with loss of interproximal attachment
-Amount of interproximal attachment loss is less than or equal to buccal attachment loss
-most likely associated with periodontitis induced horizontal bone loss
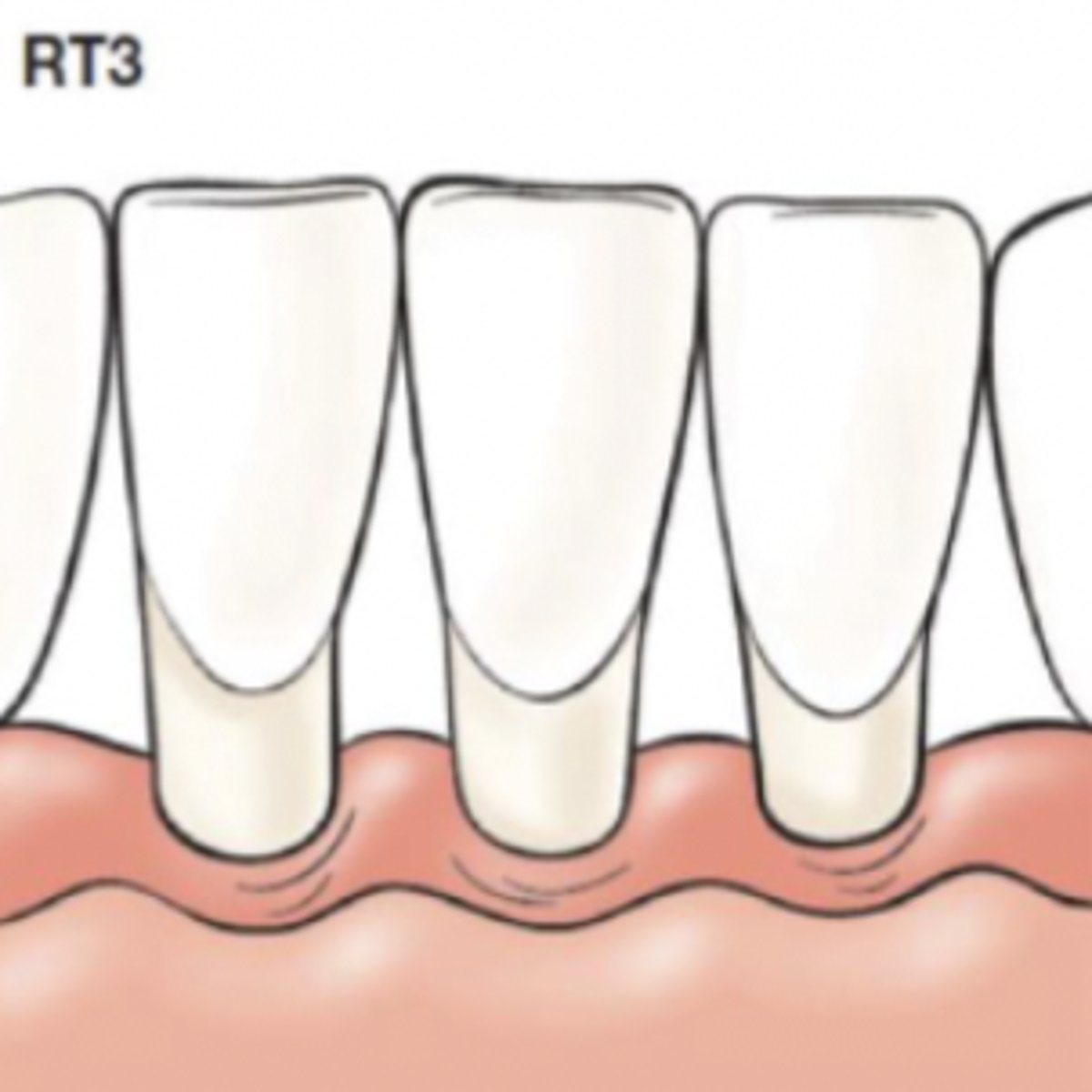
Recession type 3 (RT3) of Cairo classification system?
-Gingival recession with loss of interproximal attachment
-Amount of interproximal attachment loss is greater than buccal attachment loss
-most likely associated with periodontitis but more severe interproximal attachment loss or an interproximal infrabony defect
In Cairo classification system, how is interproximal attachment loss measured?
From interproximal CEJ to apical end of sulcus/pocket
In Cairo classification system how is buccal attachment loss measured?
From buccal CEJ to apical end of buccal sulcus/pocket
What factors must a clinician consider when treating gingival recession? (3)
-Severity/extent of symptoms
-Tissue biotype
-patient specific risk factors (ex. caries risk, periodontal disease risk, esthetic conerns)
What are 2 options of gingival recession treatment?
-Monitor the recession with no treatment
-Restorative/ Surgical measures
When may surgical intervention be necessary? (5) What will the surgery achieve? (2)
-Thin tissue biotype, dentin hypersensitivity, esthetic issues, root caries, severe plaque induced gingival inflammation
-Increased gingival thickness and thicker keratinized zone
When may surgical intervention of gingival recession not be required? (2)
-progression of recession arrests early on
-gingiva on tooth appears stable and healthy
-especially if patient is able to exercise proper plaque control and limit mechanical trauma
If a patient has any one of the following, surgical intervention is needed:
A)Thin gingival tissue
B) Gingival recession
C) Probing depths beyond the MGJ
D)Absence/Reduction in keratinized tissue
E) None of the above
E- Surgical warranty is not granted based solely on the presence of any of the options, it has to do with multiple factors
T/F If recession is halted, evidence suggests that it will not impact the long-term survival of the affected tooth
true, if the patient performs proper plaque control