Unit 6A: Gastrointestinal (GI) Function
1/110
Earn XP
Description and Tags
58 slides
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
111 Terms
what is digestion in the GI system
breaking down macromolecules (nutrients) into forms that CAN be transported across epithelium
what are the 4 functions of the GI system
digestion
absorption
secretion
motility
what is absorption in the GI system
actually transporting nutrients, water, ions, vitamins across epithelium
what is needed to accomplish digestion and absorption
secretion and motility
what is secretion
releasing enzymes into the gut lumen
what is motility
keeping the gut contents moving
what happens if the protective barriers in the GI tract break down alongside macromolecules
peptic, duodenal ulcers
Peptic ulcers = open sores on the lining of the stomach
duodenal ulcers = ulcers specifically in the duodenum
what are some things that provide protection from pathogens in the GI tract? why is this important in the GI tract specifically
important bc GI lining is largest area of contact btwn internal and external environment
mediated by…
epithelial barrier
mucus
digestive enzymes
acid
Gut Associated Lymphoid Tissue (GALT)
needs to react to pathogens but not to “foreign” proteins associated w food
what are some important considerations the GI tract specifically has to abide by
needs to digest macromolecules but not itself
needs to allow entry of digested nuts but not pathogens
needs to maintain balance btwn water input/output (balance btwn secretion and absorption)
what is gut associated lymphoid tissue (GALT)
note: also called mucosa lymphoid tissue
part of immune system that works in the GI tract → acts as kinder, gentler immune system
needs to react to pathogens but not foreign proteins associated w food
explain water balance in the GI tract
fluid input = fluid ingested + secretions from body
(~9L / day = 2L ingested + all the rest are secretions)
fluid output (removed from lumen) = fluid absorbed + fluid excreted (in feces) (~9L)
fluid input = fluid output
when is food considered to be “in” your body
Food isnt really "in” your body until it crosses your gut epithelium
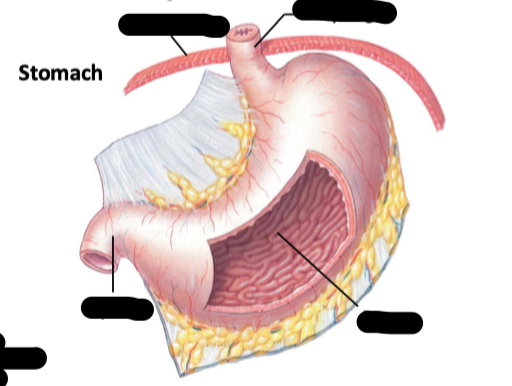
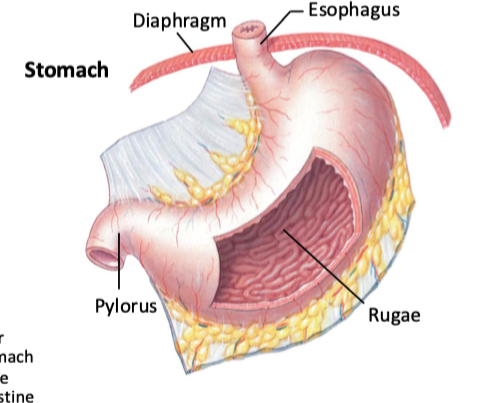
what are rugae
characteristic folds on the inner lining of the stomach
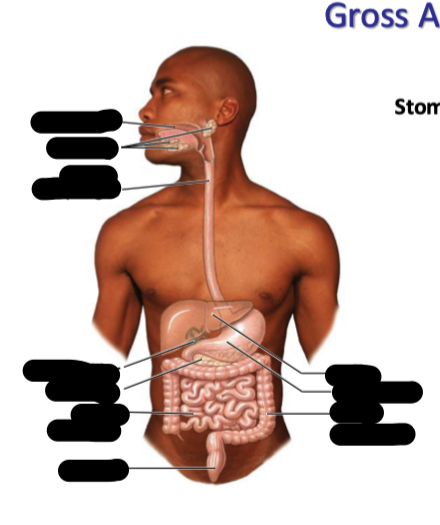
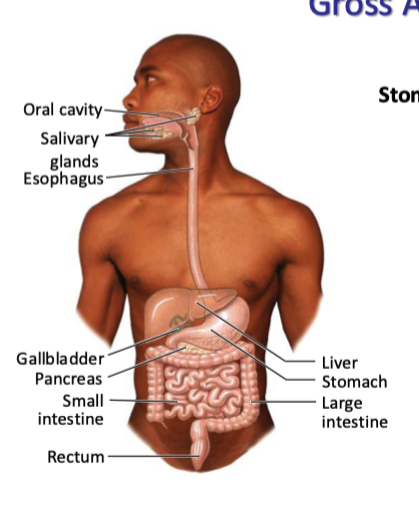
where does food go after exiting the stomach (explain all the following steps)
into the small intestine
duodenum → jejunum → ileum
into large intestine
colon → rectum
what are mucosal surfaces
the inner lining of certain passages and organs in the body that are exposed to the external environment (eg in the GI tract, back of eyes, vagina, etc)
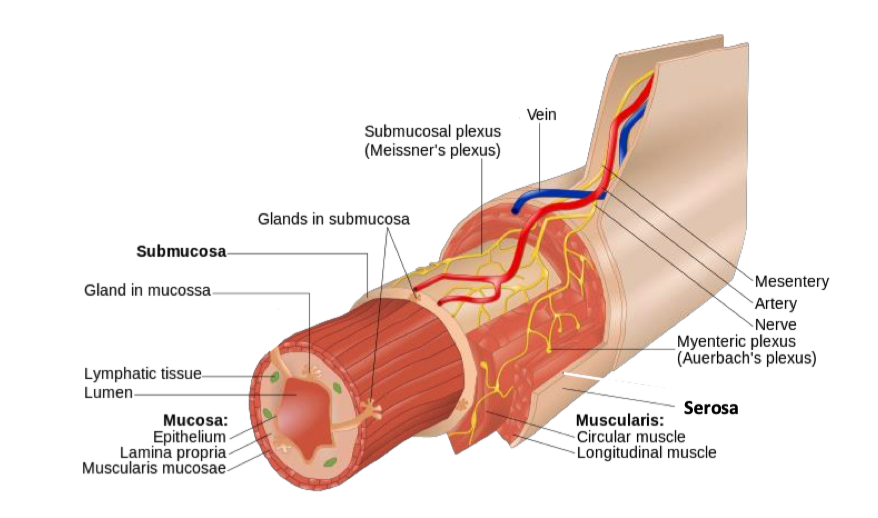
what are the 4 main components of mucosal surfaces
mucosa
inner lining
submucosa
some deeper glands protrude from here
smooth muscle layers
serosa
like bag holding everything tg
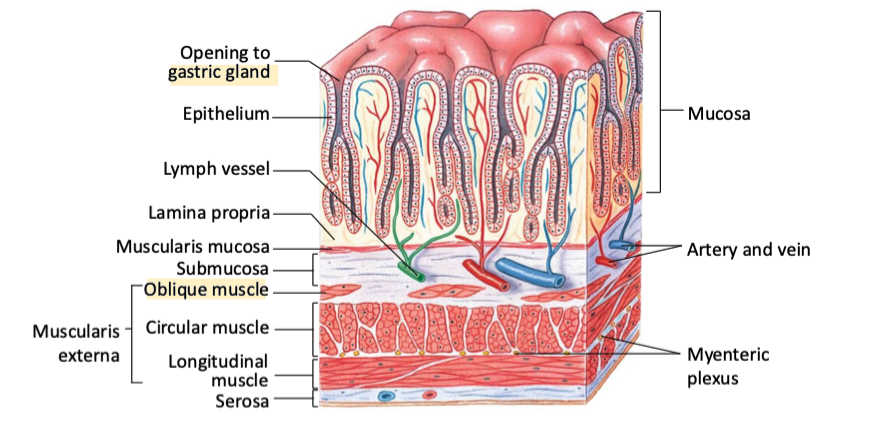
what are the 3 things the mucosa comprised of? explain them
Epithelial layer: The top layer of cells that can absorb or secrete substances.
Lamina propria: layer of connective tissue underneath
supports epithelium.
where a lot of secretory glands are
Muscularis Mucosa: thin layer of smooth muscle found at the base of the mucosa → just below lamina propria.
Moves the mucosa gently to enhance contact with contents (like food or air).
Helps expel glandular secretions.
Maintains the tone of the mucosal layer
epithelial layer, then connective tissue, then thin smooth muscle layer
what is the submucosa comprised of
the submucosa itself is connective tissue but it contains
Meissner’s (submucosal) plexus
provides outtermost innervation for GI tract
connective tissue containing nerves
what are the smooth muscle layers comprised of? explain them
Circular muscle
Myenteric (Auerbach’s) plexus
runs btwn these 2 sets of muscles
Longitudinal Muscle
2 types of muscle and nerves between
what is the serosa
epithelial tissue
outlines intestines
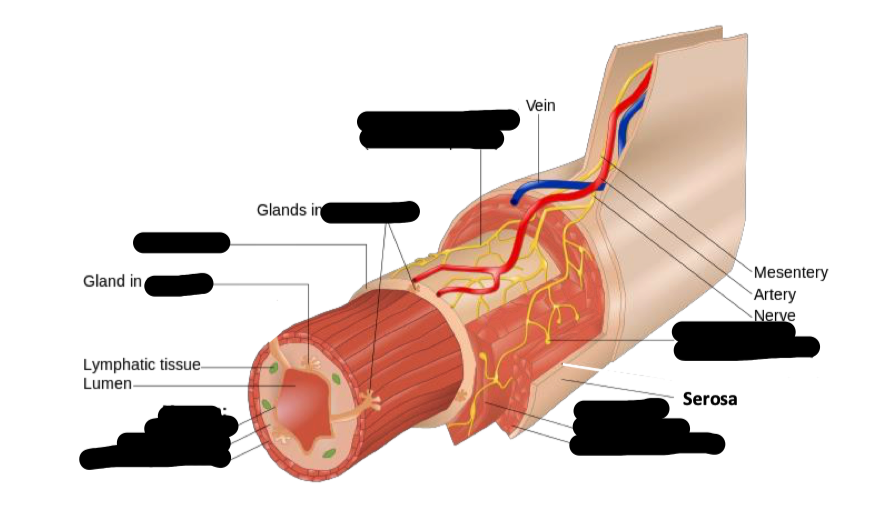
submucosa
myenteric plexus
muscularis
serosa
mucosa
what are the 3 main structures the stomach has compared to the intestines? why are those differences there
stomachs in addition to circular and longitudinal muscle in their smooth muscle layers, they also have oblique (diagonal) muscles
bc the stomach is a bag not a tube → has to contract in more dimentions
stomachs have gastric glands → deep epithelial grooves → for exocrine secretions
rugae
allow stomach to expand / contract as needed w varying amounts of food → inc SA of the stomach → aids in digestion
smooth out as the stomach expands
what are 3 notable structures in the small intestine that are not within the stomach? what does each do
plica → permanent, crescent-shaped folds of the mucous membrane → increase SA for nutrient absorption
do NOT smoothen out like rugae in stomach
Villi (and microvilli) → tiny, finger-like projections → further inc SA of intestine → facilitate absorption of nutrients into the bloodstream
Payer’s patches → only obvious evidence of immune system cells in small intestine
patches of immune cells → more numerous at far end of small intest (far away from stomach)
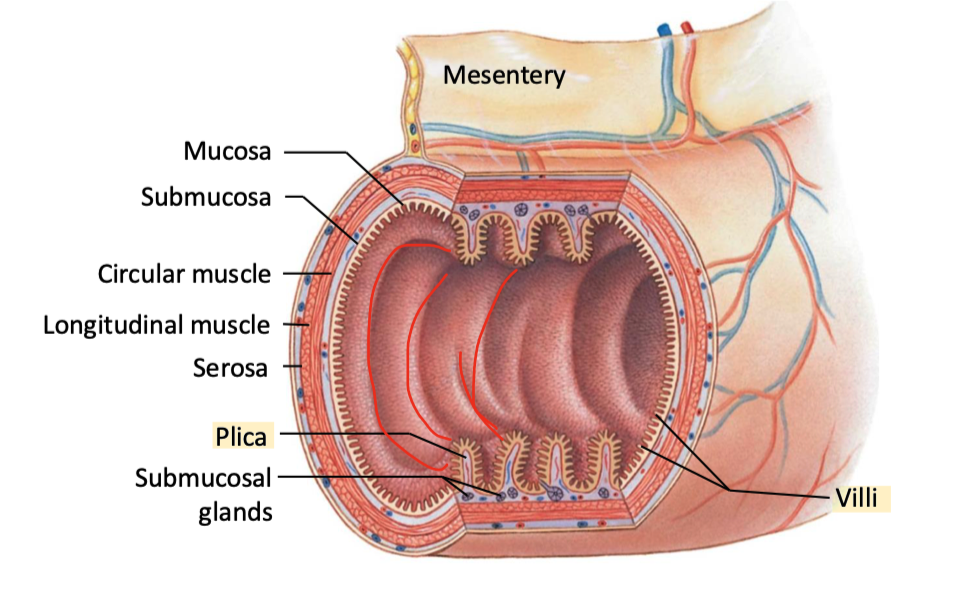
what are the 3 ways the intestines inc their SA
plica
villli
made of epithelial cells
microvilli
on epithelial cells that make up the villi
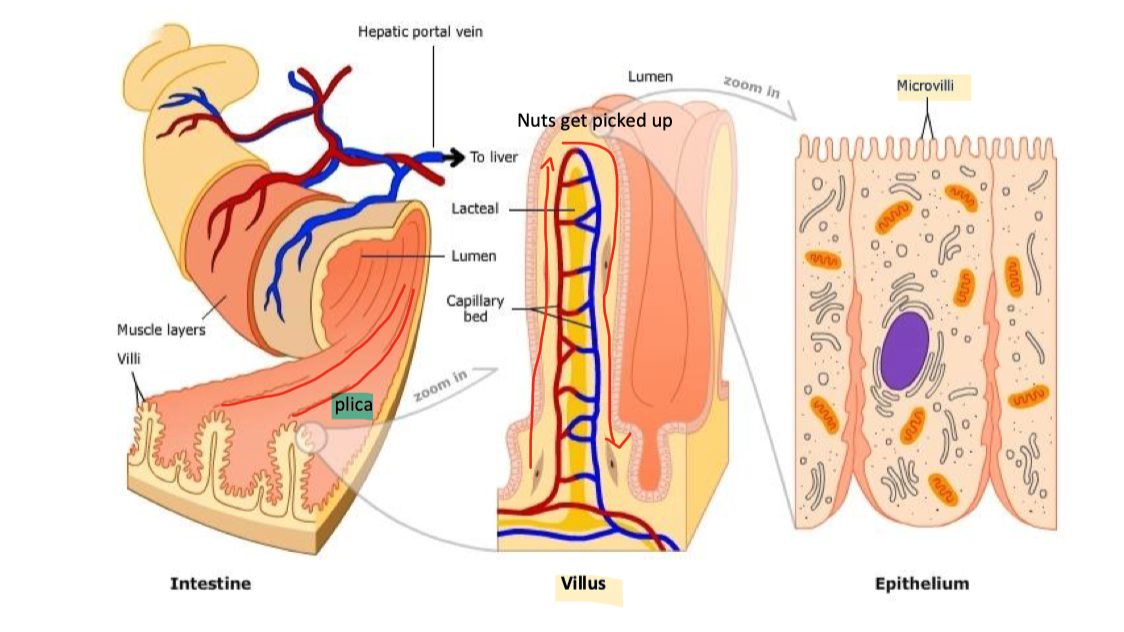
what is the brush border in the small intestines
the densely packed, microvilli-covered surface of absorptive epithelial cells (enterocytes)
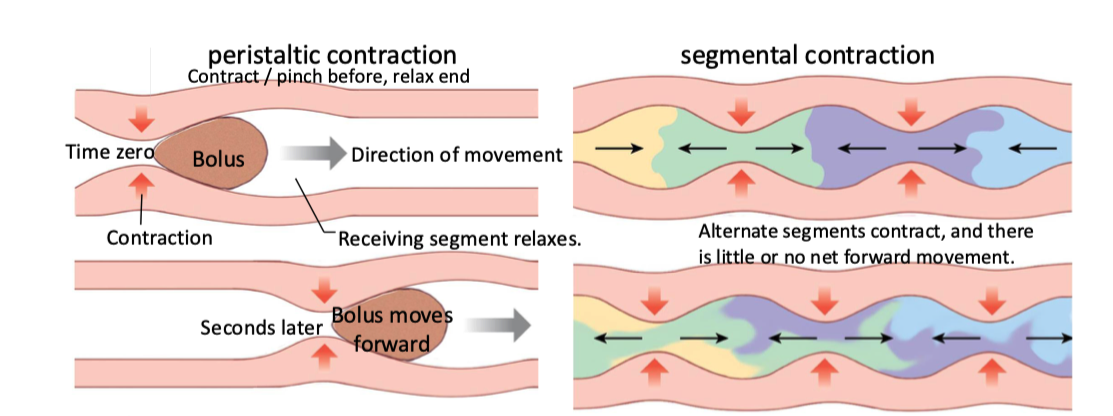
what are peristalsis and segmental contractions? explain them
the 2 main patterns of contraction in gut motility
peristalsis → moving food from mouth to anus
segmental contractions → mixing / churning
maximizes exposure to digestive enzymes and epithelium
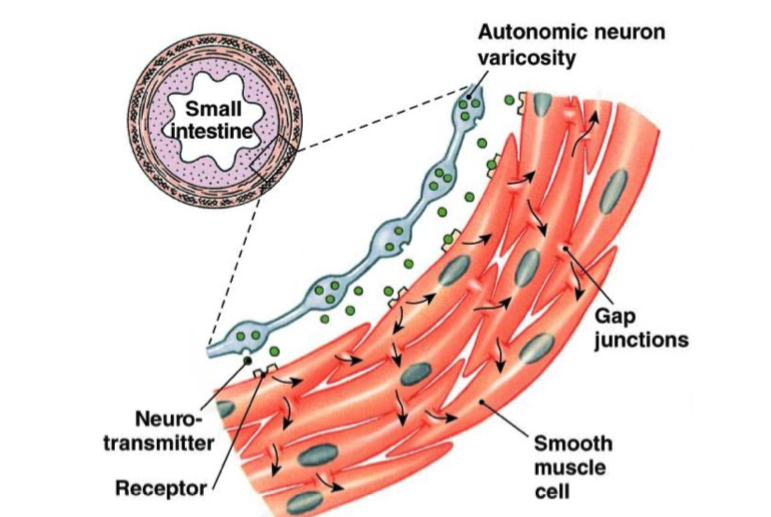
explain single-unit smooth muscle. where are they commonly located
smooth muscle all connected by gap junctions → fxs as a single unit → easier for single waves of depolarization to travel
most common in walls of GI tract, urinary tracts, and blood vessels
which areas of the gut are tonically active
smooth muscle sphincters
prevent food from moving backwards
eg btwn esophagus n stomach, anus and external environment, etc
stay contracted for minutes to hours
which ares of the gut undergo phasic contractions
posterior stomach, small intestine
stay contracted for a few seconds
explain gut motility in the small intestine between meals
fasted state:
migrating motor complexes sweep slowly down tract (~90 mins from stomach → large intest)
electrical complexes that sweep and slowly move things down
note: NOT peristaltic contractions
supposed to b clearing out residual things in small intest and prepare for next mean
explain gut motility in the small intestine during/after meals
peristaltic and segmental contractions
what determines the force and duration of muscle contraction
force = amplitude
duration = frequency
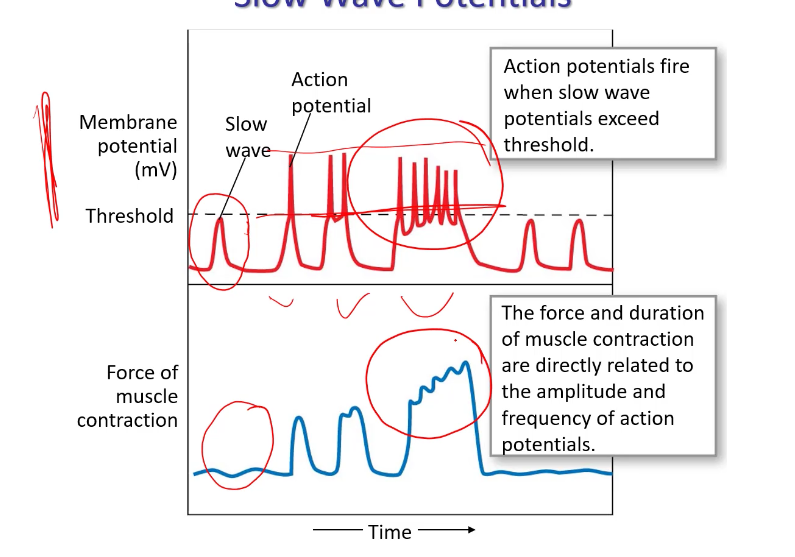
what are the amplitude and duration of contraction influenced by
neurotransmitters (autonomic input)
hormones
paracrine factors
what are slow wave contractions in gut smooth muscle similar to
pacemaker potentials in cardiac tissue → BUT much less frequent and do not necessarily reach threshold
explain slow wave contractions in gut smooth muscle
below threshold → no contraction
above → V-gated Ca+ channels open, action pots, contraction
t/f: slow wave frequency varies in diff regions of tract? explain why or why not
true → set by pacemaker cells between smooth muscle layers
eg more frequent in duodenum than stomach
what are the interstitial cells of cajal
specialized cells in the gastrointestinal (GI) tract → act as pacemakers → generate electrical slow waves that regulate gut motility
explain the secretion of water and ions in the GI tract
ions mostly are excreted via mem transporters
water follows via osmotic gradient
water and ions can also pass between cells (paracellular) in some regions
explain acid secretion by parietal cells
as H+ is secreted from the apical side, bicarb (from CO2 + OH-) is absorbed into blood
H+ (acid) gets pumped into lumen of stomach in exchange for K+
AT SAME TIME Bicarb gets pumped into blood in exchange for Cl- (which then diffuses into stomach lumen to make HCl with H+)
Overall:
hydrogens and Cl pushed out into stomach lumen
HCO3- goes into blood
note: this happens in gastric glands
explain the alkaline tide
temporary increase in blood pH (making it more alkaline)
occurs after a meal, especially one that stimulates gastric acid secretion
bc bicarb goes into blood (inc pH)
and H+ and Cl- goes into stomach (dec pH)
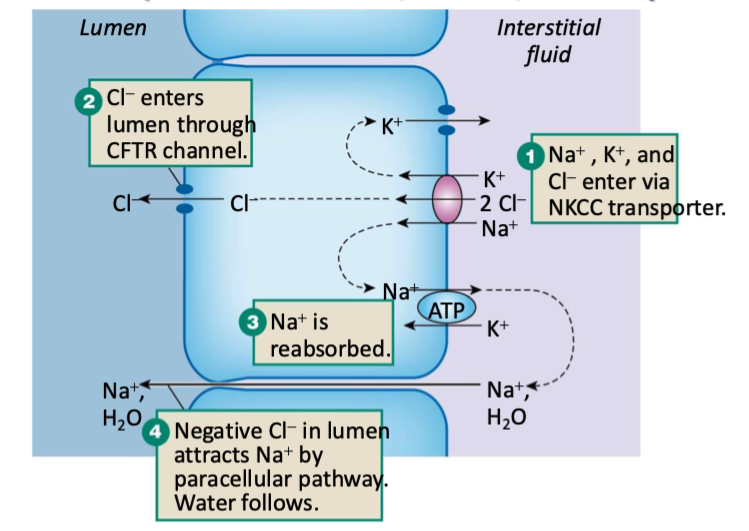
explain how salt (NaCl) is secreted in the small intestine, colon, and salivary glands
Via Crypt Cells
Na, K, and Cl enter the epithelial cells via NKCC transporters
Cl- enters lumen through CFTR channel
this is the driving force
Na and K go back into interstitial fluid
Na+ is reabsorbed (pumped back into interstitial fluid)
K+ diffuses through ion channel back into interstitial fluid
Negative Cl- in lumen attracts Na+ by paracellular pathway
Na+ goes through paracellular pathway and water gets dragged along with it
Na, Cl, (making NaCl) and water are now in the intestinal lumen
Creates intestinal saline that mixes w mucus
which cells secrete mucus
goblet cells
explain why bicarb is secreted from the pancreas into duodenum
pancreatic ducts secrete bicarb into duodenum to neutralize acid from stomach
Stomach makes acid -> dumps extremely acidic contents into top of small intestine -> enzymes in small intest cannot work in high acidic conditions -> needs to b quickly neutralized -> duct cells dumb bicarb on them to minimize acidity
what are acinar cells
cells in the pancreas that secrete digestive enzymes
explain pancreatic bicarb secretion on the cellular level? what is the driving force
bicarb is secreted via apical Cl-/HCO3 antiporter
Cl enters pancreatic duct cell / duodenal cell via basolateral NKCC transporter and leaves via apical CFTR channel
Luminal Cl then reenters the cell via Cl/HCO3 antiporter
bc chloride is the driving force, this is referred to as a chloride shift mechanism
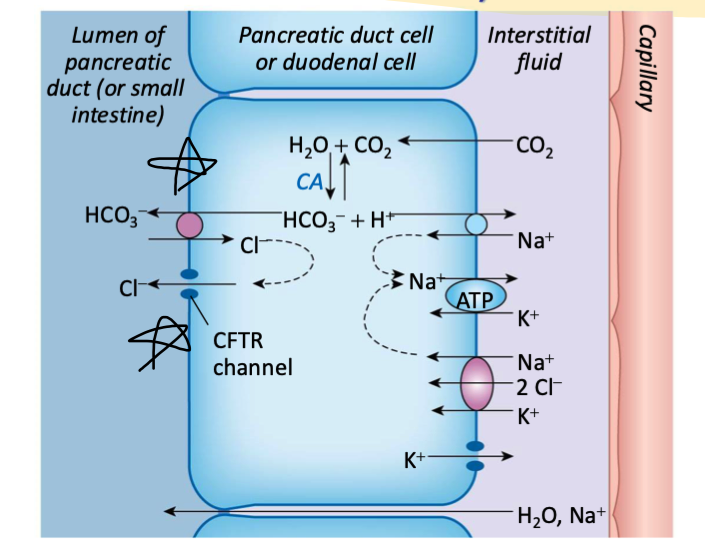
what is needed in excess for pancreatic bicarb production
requires a lot of carbonic anhydrase so a lot of bicarb is produced
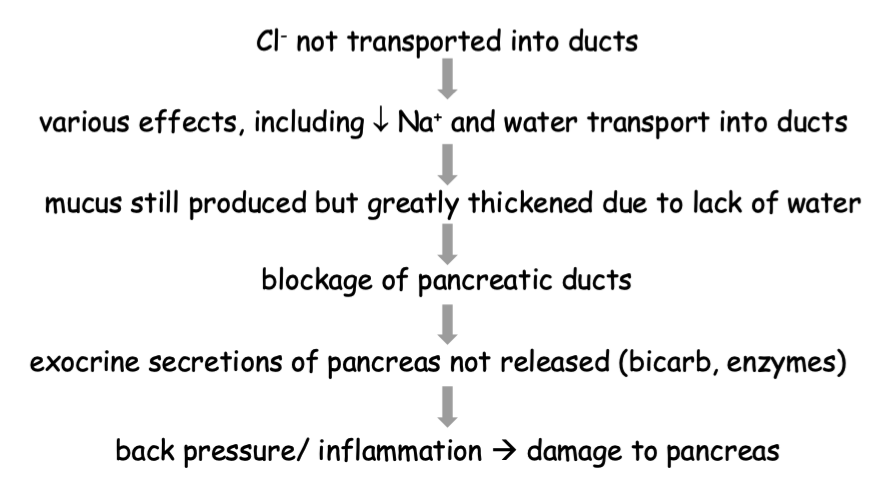
explain what cystic fibrosis is
mutation in the gene that encodes for CFTR channel in pancreatic cells that secrete bicarb
leads to deficits in Cl (and water) transport
named for changes in the pancreas
creates fluid-filled cysts and fibrosis (scarring)
without it, the luminal Cl levels will stay low and it can’t be antiported back into the pancreatic duct cells and push bicarb back
would taking a pill that replaced secreted molecules in the pancreas/small intestine help with cystic fibrosis
yes → would include bicarb and help neutralize HCl from stomach
explain how and what secretes enzymes
secreted by either exocrine glands (eg pancreas, salivary) or epithelial cells lining stomach and small intestine
synthesized by rough ER, packaged by golgi into vesicles, stored in cell under signal for release by exocytosis
wht are “brush border” enzymes
enzymes that remain linked to apical mems by protein or lipid “stalks”
what are zymogens
inactive precursors for enzymes → enzymes are often released as these inactive precursors to prevent auto-digestion (enzymes digesting/breaking down things on their way to their targets)
what types of stimulation typically regulates secretion → sympathetic or parasympathetic
parasympathetic stimulation (through vagus nerve)
what is mucus primarily made of
“mucins” → mixture of glycoproteins
what types of cells produce mucus
exocrine cells
serous cells in salivary glands
mucous cells in stomach
goblet cells in intestine
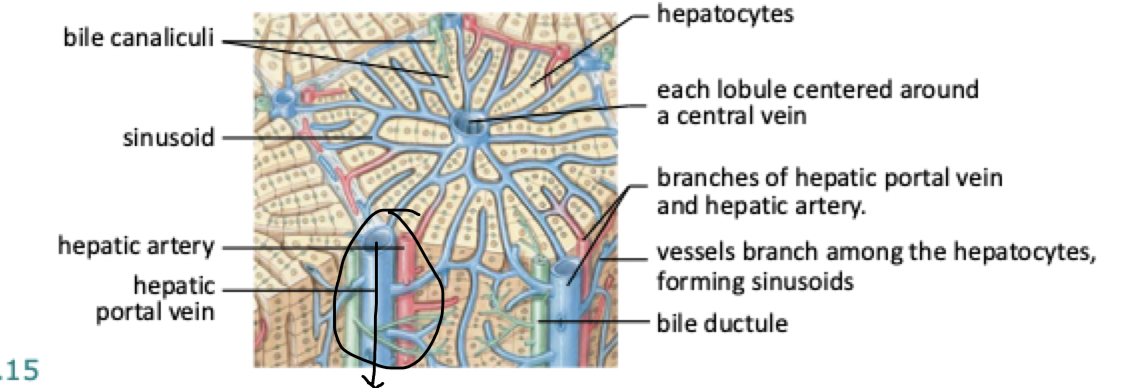
what is the hepatic lobule? what shape are they
the functional unit of the liver
hexagonal in shape
blood and bile flow through it
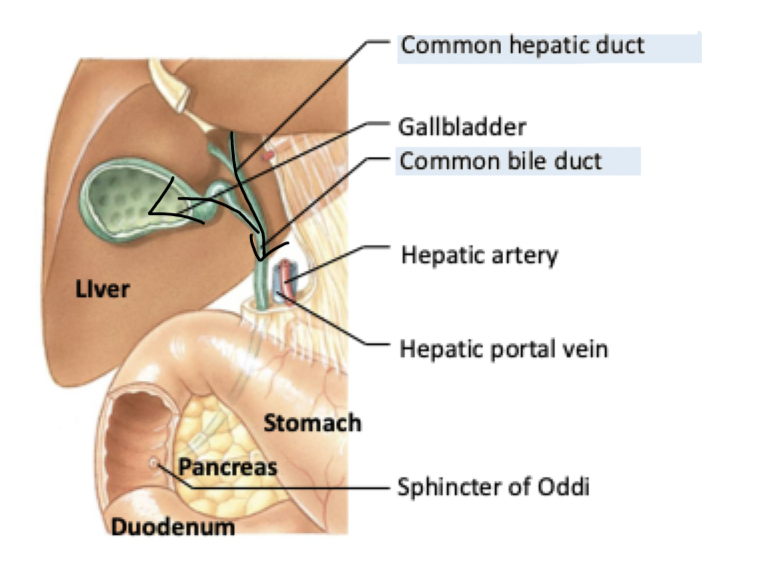
explain how bile flows from the liver to the digestive tract (how it is secreted)
note:
bile ductules
gall bladder
common hepatic duct
sphincter of Oddi
duodenum
common bile duct
bile canaliculi
hepatocytes
in hepatic lobule
Hepatocytes (liver cells arranged around central vein) → secrete bile into →
Bile canaliculi (tiny channels btwn hepatocytes where bile is secreted - collect bile and carry it in opposite direction of blood flow (away from central vein) → drain into →
Bile ductules (receive bile from canaliculi and lead to larger ducts outside of lobule)→ merge into →
Common hepatic duct
From here, bile can take two paths:
Stored in gall bladder
Or go directly through common bile duct to small intestine
Common bile duct passes through the sphincter of Oddi and empties bile into the duodenum (the first part of the small intestine)
what are xenobiotics
foreign substances
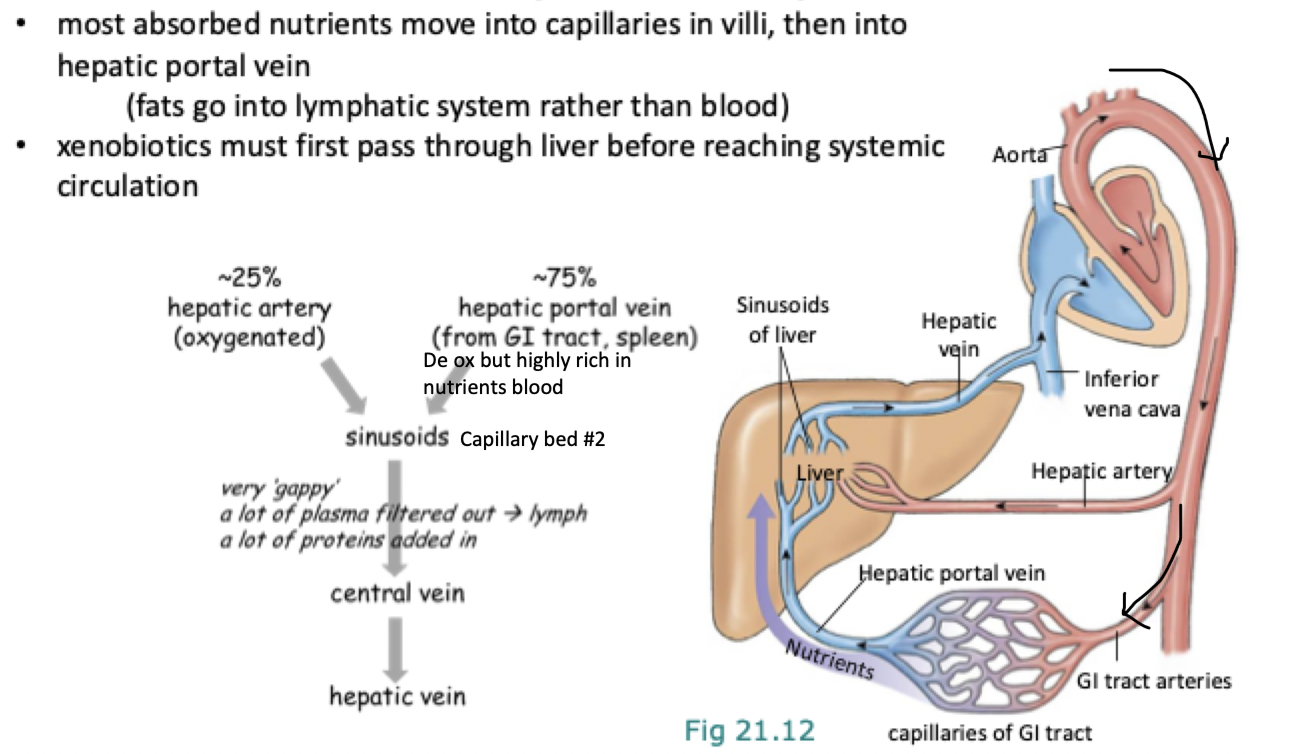
what does the hepatic portal system do
ensures most nutrients and xenobiotics (foreign substances) absorbed in the GI tract are processed by liver before they enter general circulation
xenobiotics (eg drugs and toxins) are detoxified by the liver BEFORE reaching systemic circulation
where does blood flow through the hepatic portal system
1. Absorption in the GI Tract:
Nutrients from digested food are absorbed through the capillaries in the intestinal villi.
nuts enter hepatic portal vein → carries de oxy blood from GI tract and spleen to liver (high in nuts, low in O2)
Note: Fats are exception—they enter the lymphatic system instead of the blood.
2. Hepatic Portal Vein (~75% of Liver Blood Flow):
Carries nutrient-rich, deoxygenated blood from the GI tract and spleen to the liver.
Hepatic Artery (~25% of Liver Blood Flow) (another place blood comes into liver from) :
Carries oxygen-rich blood from the aorta to the liver.
3. Sinusoids of Liver:
Blood from the hepatic artery and portal vein mix here.
Sinusoids are leaky capillaries that allow for the exchange of substances between the blood and hepatocytes (liver cells).
The liver can filter toxins, process nutrients, and add plasma proteins here.
4. Central Vein → Hepatic Vein → Inferior Vena Cava:
After processing, blood drains into central veins, then into the hepatic veins, and finally enters the inferior vena cava to return to the heart.
what are the 3 key components of bile
bile salts (facilitate fat digestion)
bile pigments (eg bilirubin from hemoglobin breakdown)
cholesterol
how do we still feel the effects of drugs if they are filtered at the liver
Drugs come into liver and detox can happen, liver can completely break it down and dump it into duodenum to end up in feces BUT then body wouldn’t feel many effects -> usually some of it exits via hepatic portal vein and into circulation so there are systemic effects
what is bilirubin and where does it go
Bilirubin -> breakdown of RBCs goes into speeel, makes Hb, makes bilirubin -> goes into liver and is sent out with bile into feces
Colour of bilirubin is most of the reason why feces are the colour they are
t/f: the liver builds proteins or contributes to circulating AA pool that rest of body can use
true
what are some of the main substances that go into the liver from the GI tract (through hepatic portal vein)
bilirubin
nutrients
drugs / foreign substances
what are some of the main substances that go into the liver from the peripheral tissues (hepatic artery)
bilirubin
nuts
hormone and drug metabolites
what gets secreted by the bile duct of the liver and into the duodenum
bile salts
bilirubin
what gets secreted into the hepatic vein by the liver and into the peripheral tissues
glucose
plasma proteins
t/f: the liver makes glucose
true → oscillates between creating glucose and glycogen
what is bilirubin responsible for
the normal colour of feces
normal colour of urine
what are some indicators of injury / pathology related to bilirubin
yellow phase of bruises (blood pools and cant get bilirubin filtered out)
yellow pigmentation in jaundice (hyperbilirubinemia)
what kinds pf proceses is digestion a combination of? why and where does that occur
combination of mechanical and enzymatic processes
occurs in mouth, stomach, small intestine
chewing and churning exposes more SA to enzymes
emulsification (combination) via bile exposes more SA for lipid digestion
where does most absorption occur
in the small intestine
t/f: digestion and absorption are directly regulated (explain why or why not)
false → influenced by motility and secretion, which are regulated by hormones, NS, and. local mechanisms
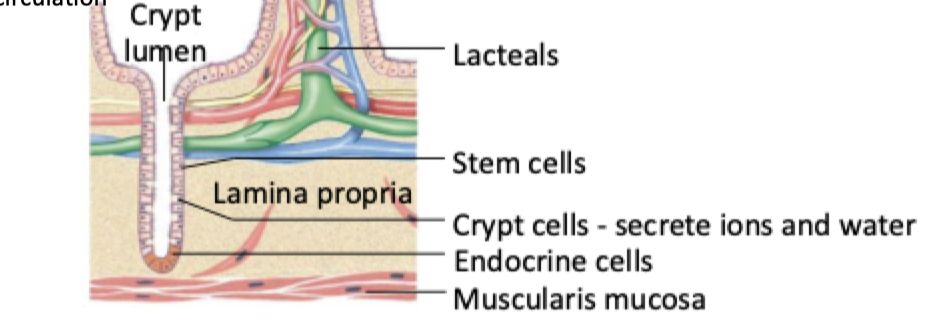
explain absorption in the small intestine
goes from the gut lumen → the apical mem → into epithelial cell (called enterocyte) → through basolateral mem → into lamina propria → into either the capillaries or lymph
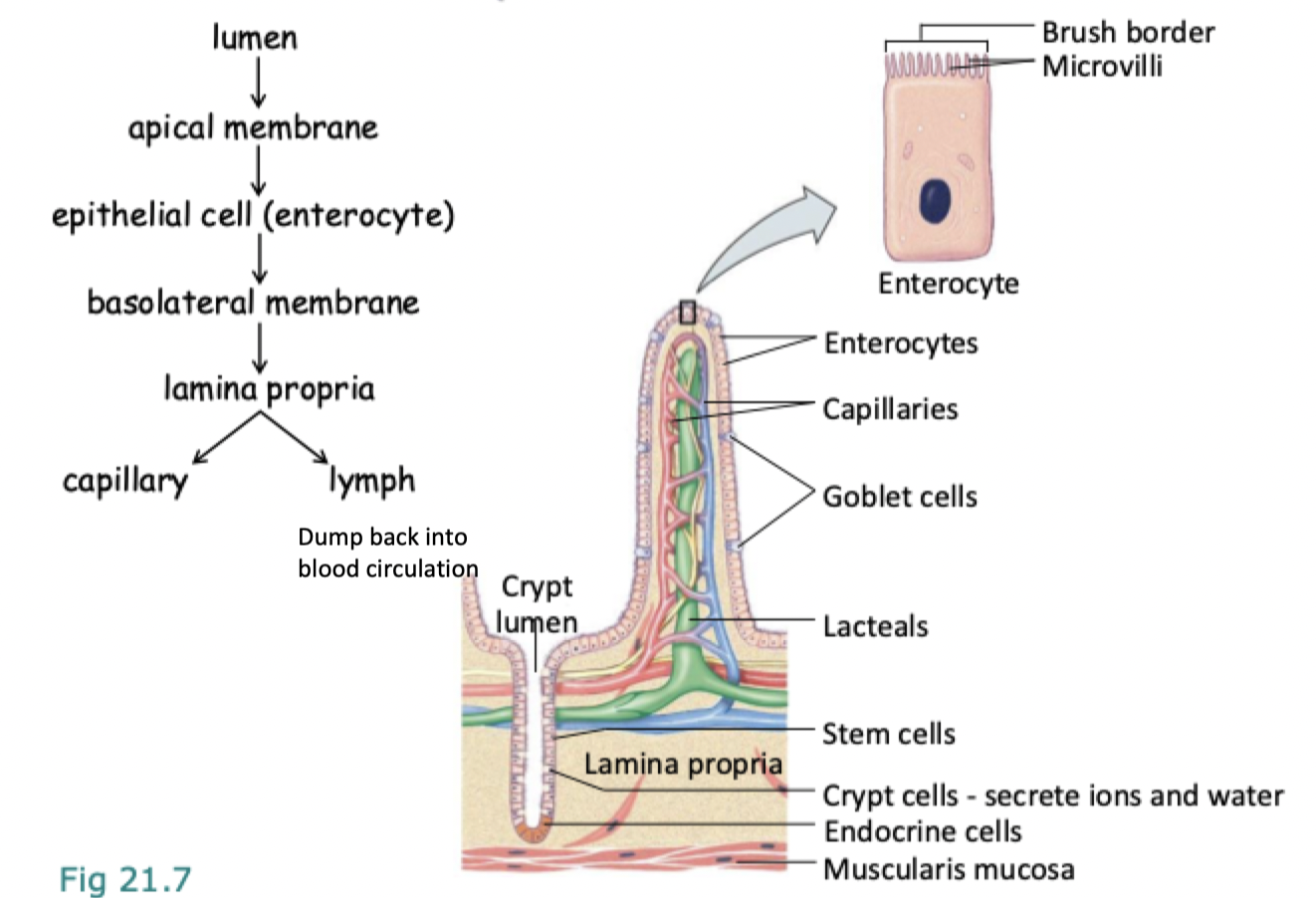
where are enterocytes located
on microvilli
where are crypt cells located
in the lamina propria
how much of our caloric intake consists of carbs
around half
mostly starch and sucrose
how do artificial sweeteners work
trick body into activating their “sweet” receptors but don’t get broken down into monosaccharides to enter enteroctes on microvilli -> just excreted
what are some examples of glucose polymers
starch and glycogen
what are some examples of dissacharides
maltose, sucrose, lactose
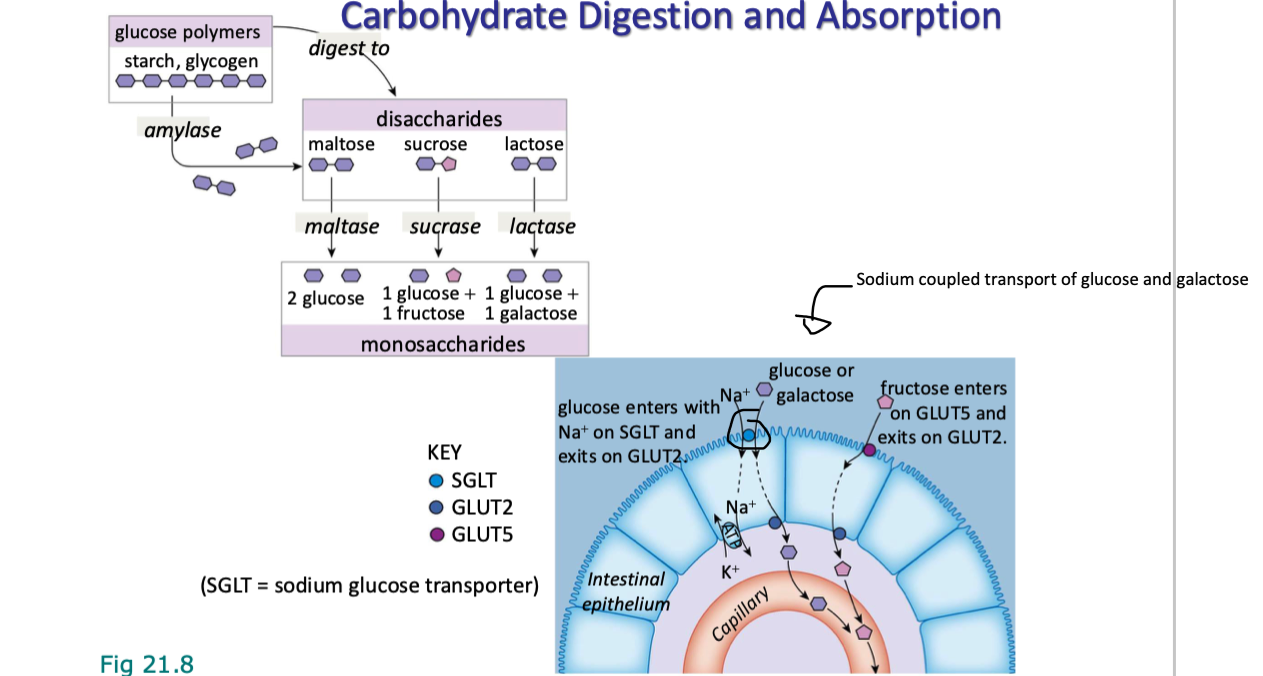
which monosaccharides do maltose, sucrose, and lactose digest into? which enzyme(s) are used?
Maltose | Maltase | Glucose + Glucose |
Sucrose | Sucrase | Glucose + Fructose |
Lactose | Lactase | Glucose + Galactose |
explain how carbohydrates are digested and absorbed
starches and disaccharides are broken down and how the resulting monosaccharides are absorbed by intestinal epithelial cells
Digestion:
glucose polymers (eg. starch, glycogen) broken down by amylase (from pancreas and saliva
amylase converts them into disaccharides (maltose, sucrose, lactose)
disaccharides are broken down by its specific brush border enzyme (ie lactase, maltase, sucrase) into monosaccharides
Absorption:
Glucose and Galactose
work like in kidneys
enter apical mem of epithelial cells in small intest via SGLT (sodium glucose transporter) using Na+ cotransport
exit basalateral mem into bloodstream via GLUT2 (facilitated diffusion)
Fructose
enters apical mem via GLUT5 (facilitated diffusion)
exits via GLUT2 just like (glucose and galactose)
what are endopeptidases
proteases (break down proteins) in the middle (make them smaller chunks)
what are some exs of endopeptidases
pepsin (from stomach)
trypsin and chymotrypsin (from pancreas)
what are exopeptidases
cleaves peptide bonds at the end of a protein or peptide chain, releasing single amino acids, dipeptides, or tripeptides
what does it mean when an enzyme has “ogen” at the end of it
it means the enzyme is a zymogen (in its inactive form)
explain protein digestion and what its products are
stomach:
HCl in stomach denatures proteins
stomach endopeptidases can then break them down (eg pepsin in stomach)
Small Intestine:
pancreatic endopeptidases (trypsin, chymotrypsin) break them down further
exopeptidases from brush border and pancreas digest terminal peptide bonds to release individual AAs
produces free AAs, di and tri peptides
explain protein absorption
di and tri peptides are cotransported w H+ into enterocytes
di and tripeptides → enter through H+ cotransport
broken down into individual AAs by intracellular peptidases
AA → enter through Na+ cotransport
all intracellular AAs now enter blood through antiport with Na+
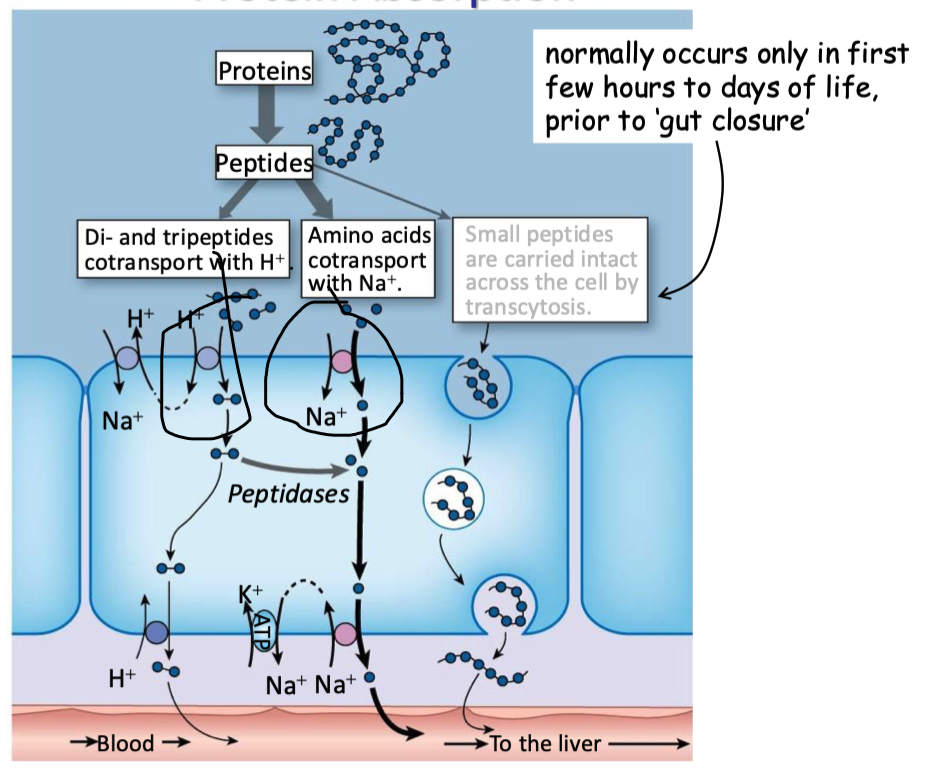
when are proteins carried in tact across the cell (transcytosis)
only for first few hours/days of human life
where are most of our fat calories from
triglycerides
explain what makes digestion of fats in the stomach unique
HCl in stomach is polar → can’t dissolve fats (like-dissolves-like)
leave stomach as large droplers mixed with aqueous chyme (other stuff digested in stomach that stuck to it)
low SA available to interact w enzymes
what helps break down fats
broken down into smaller particles through action of bile salts
what are bile salts all derivates of
cholesterol → just all have diff side chains
t/f: bile salts are amphipathic
true
explain what happens to fats when they enter the duodenum
small intestine senses fats enter it → release hormone called cholecystokinin (CCK)
causes the gallbladder to secrete bile produced by the liver → contains bile salts
hydrophobic parts → conduct emulsification → coat the large lipids and break them down
higher surface area to volume ratio, meaning → more SA for digestive enzymes to work on
Pancreatic lipases (digestive enzymes originating from the pancreas) break down triglycerides into free fatty acids and monoglycerides
bile salts can actually inhibit lipase (make it harder to bind) → co-enzyme called colipase is secreted by pancreas w lipase → binds to lipase and fat droplets, anchoring them together even when bile salts are present
all fats (except for cholesterol) are digested into smaller components
broken-down fats, now monoglycerides free fatty acids, and phospholipids, alongside bile salts form micelles
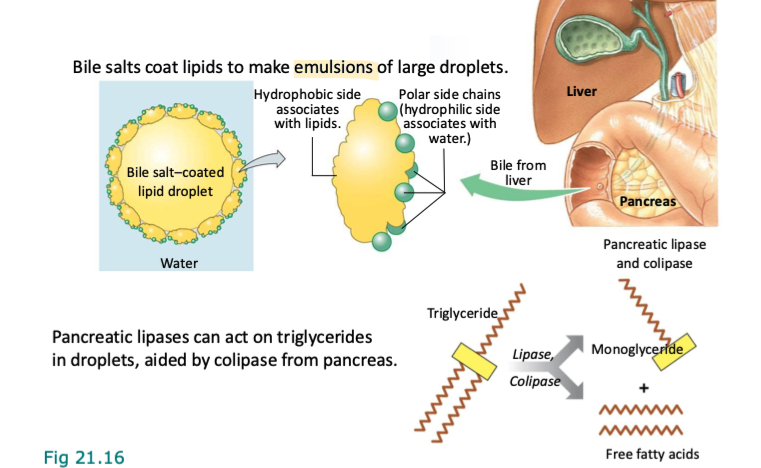
explain how micelles are arranged
cholesterol molecules and free fatty acids, along with hydrophobic pieces of the other molecules (like the phospholipids) located inwards, and the hydrophilic pieces pointing outwards
what are micelles used for
used to transport the digested fats through the watery environment of the small intestine until they reach enterocyte