Cardiopulmonary Anatomy & Physiology Chapter 19: Electrocardiogram and Cardiac Arrythmias in Adults
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
58 Terms
myocardial cells
working or mechanical cells responsible for contraction
pacemaker cells
specialized cell of the electrical conduction system that spontaneously generates and conducts impulses
Automaticity
the ability of pacemaker cells to initiate an electrical impulse without being stimulated by another source
Excitability (irritability)
ability of cardiac muscle cells to respond to an outside stimulus
Conductivity
ability of a cardiac cell to receive an electrical stimulus and conduct that impulse to an adjacent cardiac cell
Contractility
the ability of cardiac cells to shorten, causing cardiac muscle contraction in response to an electrical stimulus
antiarrhythmic drugs
medications used to correct irregular heartbeats; either slows down or speeds up heart beat
arryhthmia/dysrhythmia
an irregular heartbeat or abnormal sinus rhythm
Electrocardiogram (ECG)
voltmeter that records electrical voltages (potentials) generated by depolarization of heart muscle
ECG leads
electrodes places on the skin and attached to a specialized voltmeter (ECG)
-Conduction disturbances
-The electrical effects of medications and electrolytes
-the presence of ischemic damage
name 3 important things the ECG can inform us about
FALSE: the ECG provides electrical information about the heart, NOT mechanical information
True or False: The ECG can provide information about the mechanical (contractile) condition of the myocardium.
Bipolar limb leads
(Leads I,II,III) leads composed of two opposite polarity electrodes
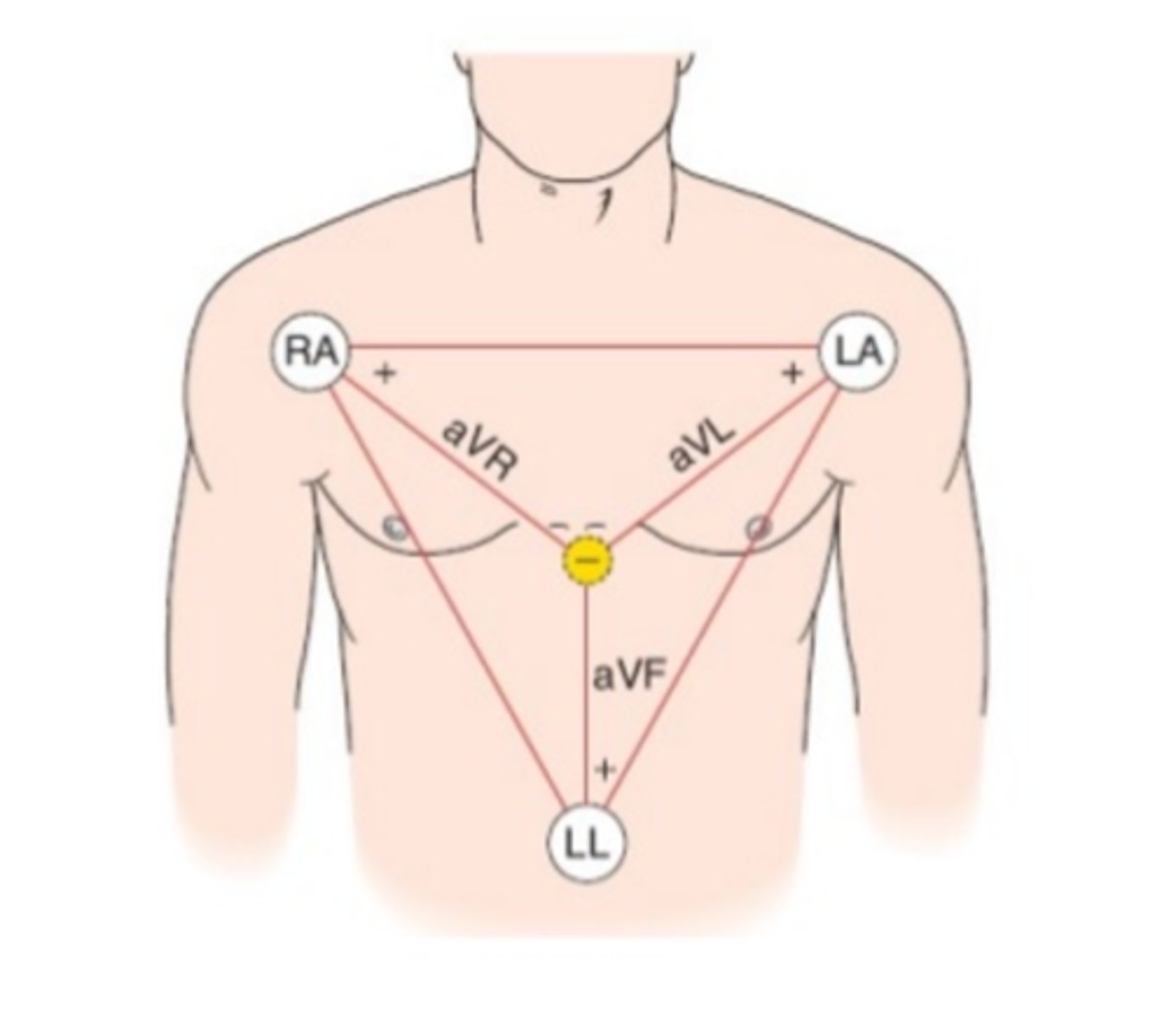
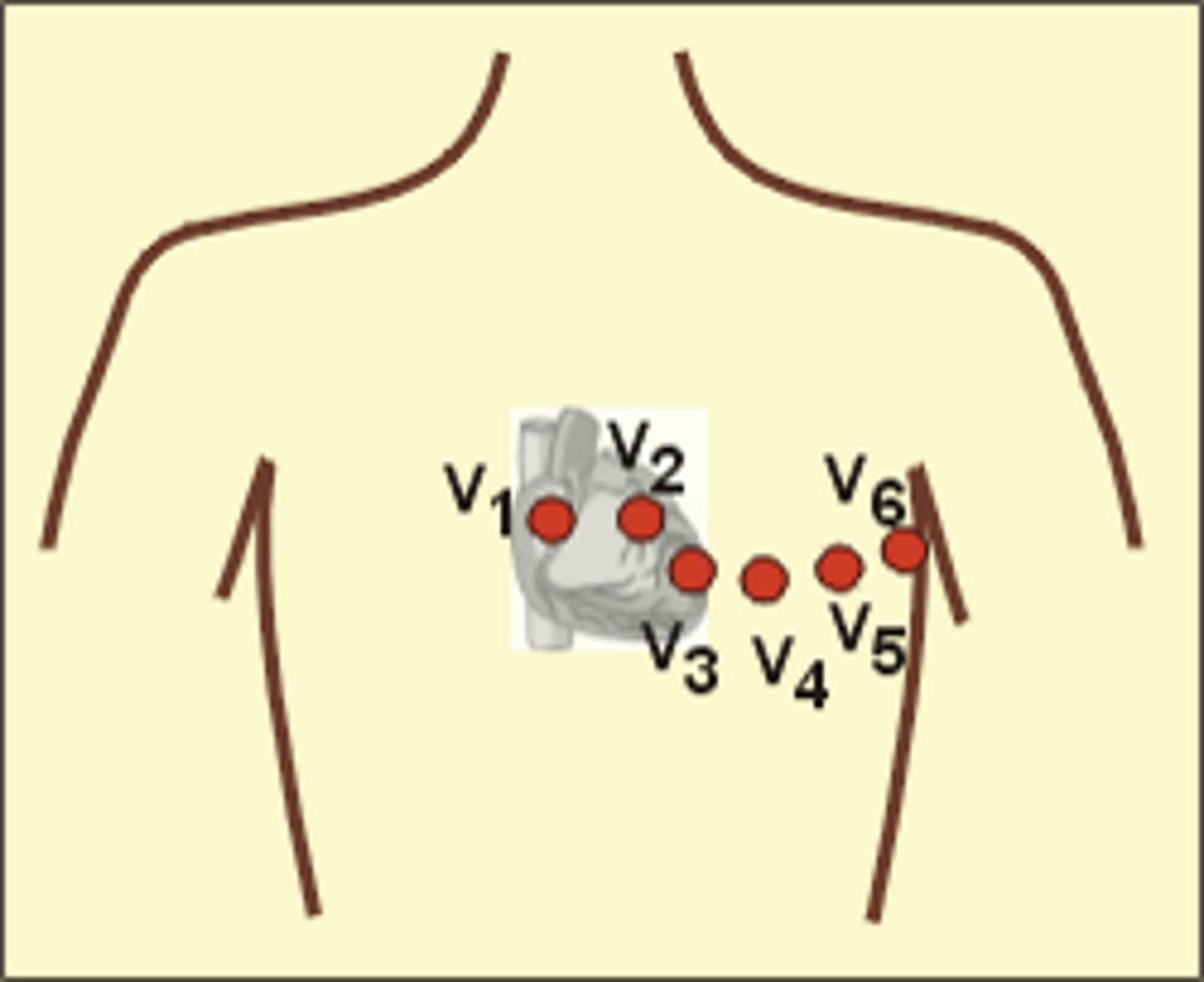
Precordial Chest Leads
(Leads v1-v6) Leads placed on a horizontal plane through the chest; consisting of six positive unipolar electrodes on the surface of the chest
P-wave
part of the ECG that represents depolarization of the atria (atrial systole)

QRS complex
part of the ECG that represents ventricular depolarization
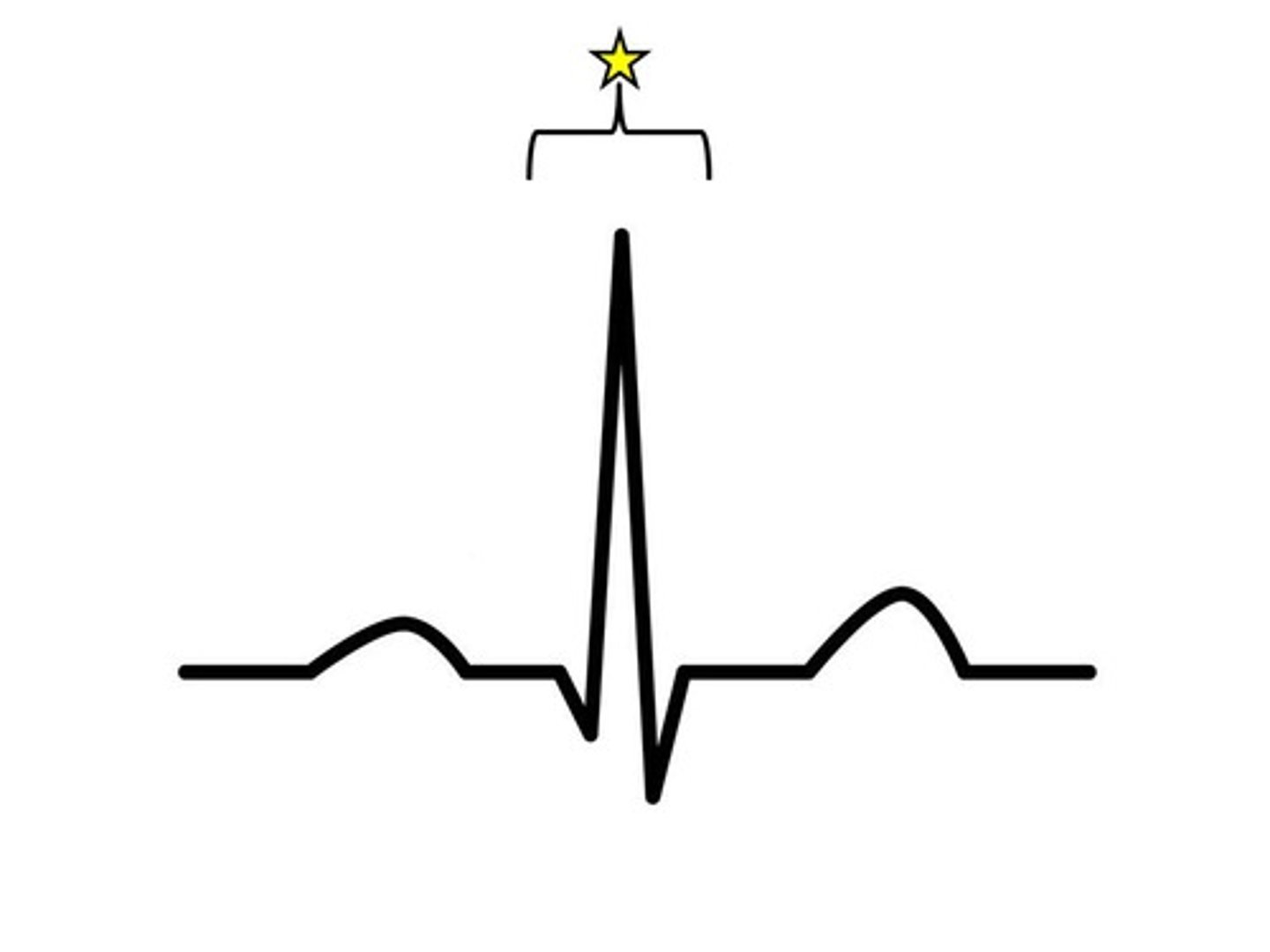
T-wave
part of the ECG that represents ventricular repolarization
ECG graph paper
a grid permitting time management along the horizontal lines, and voltage measurement along the vertical lines
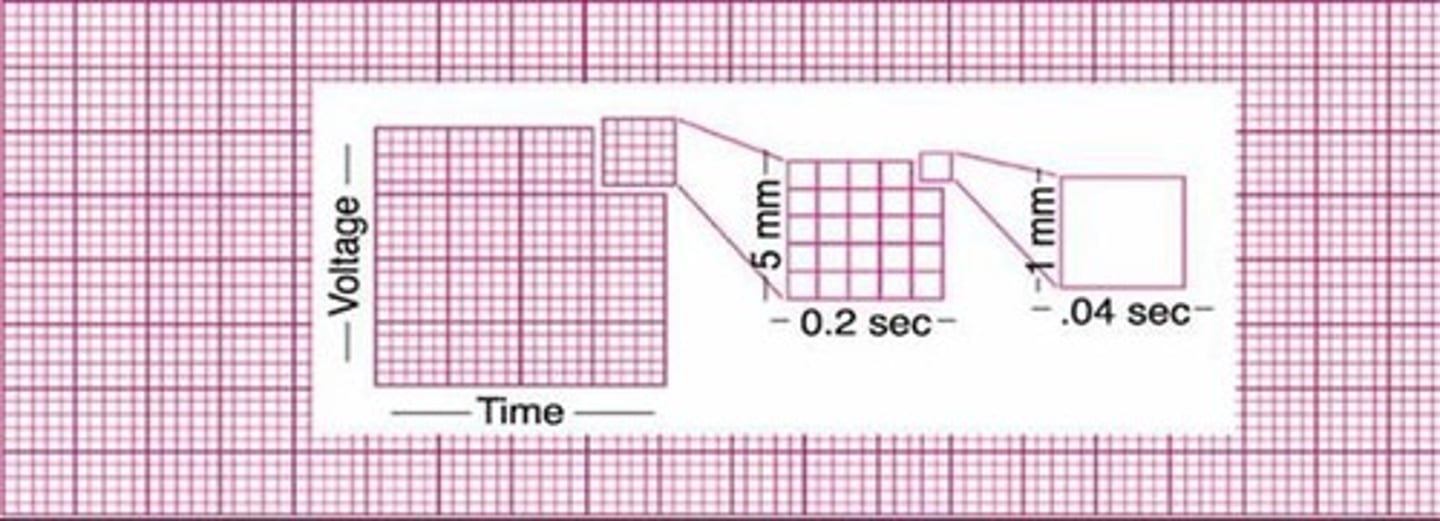
count each R-wave and multiply by 10
how does one calculate heart rate on ECG graph paper?
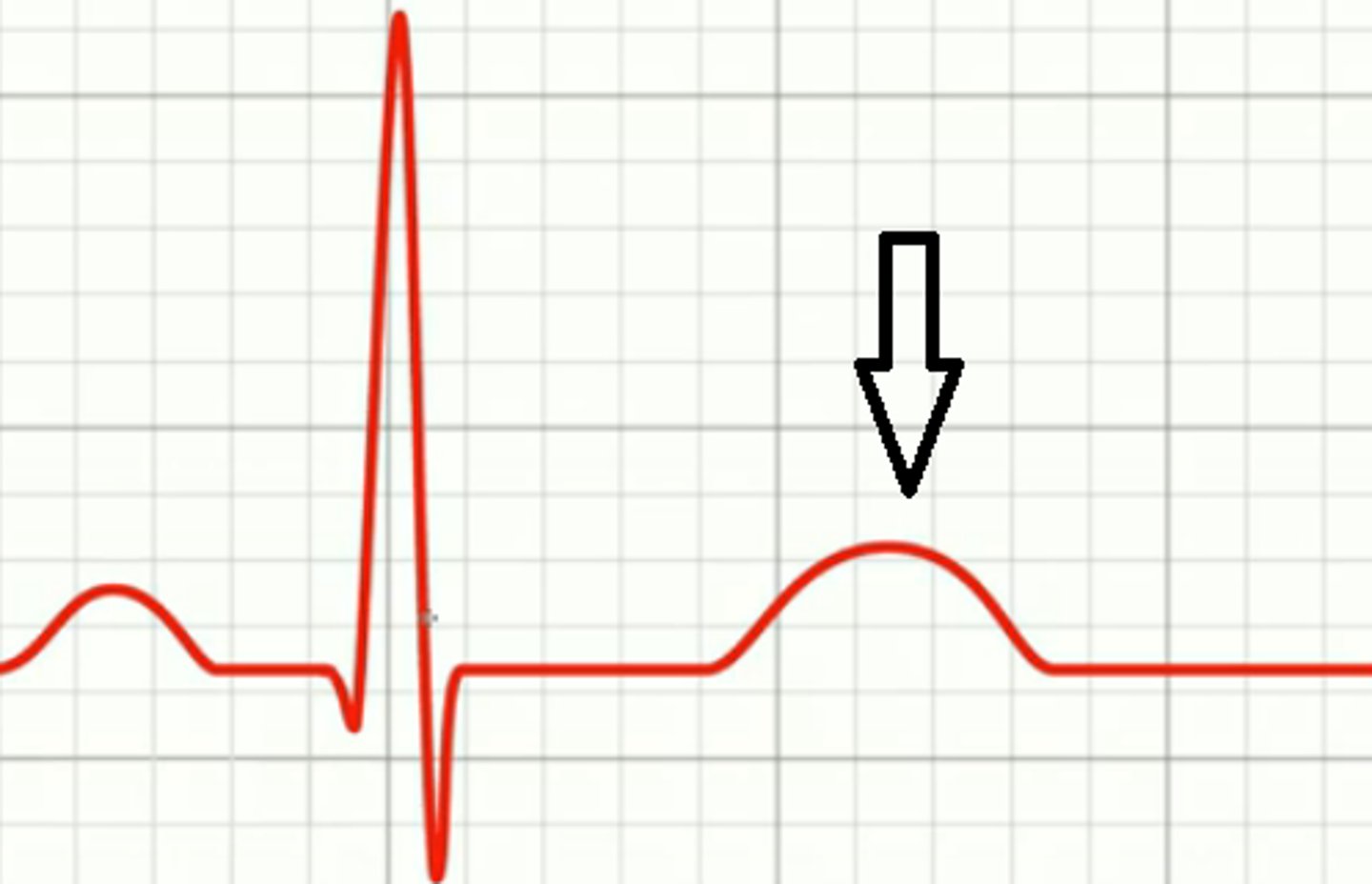
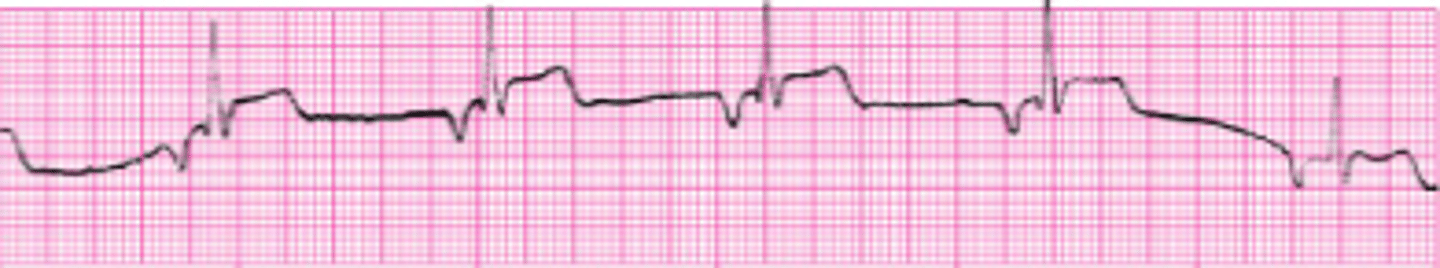
myocardial injury/infarction
what does an elevated ST segment indicate?

6 seconds
how many seconds long is an ECG graph paper strip?
absolute refractory period
from the beginning of the QRS complex to the middle of the T-wave; no outside stimulus can cause the cells to depolarize.
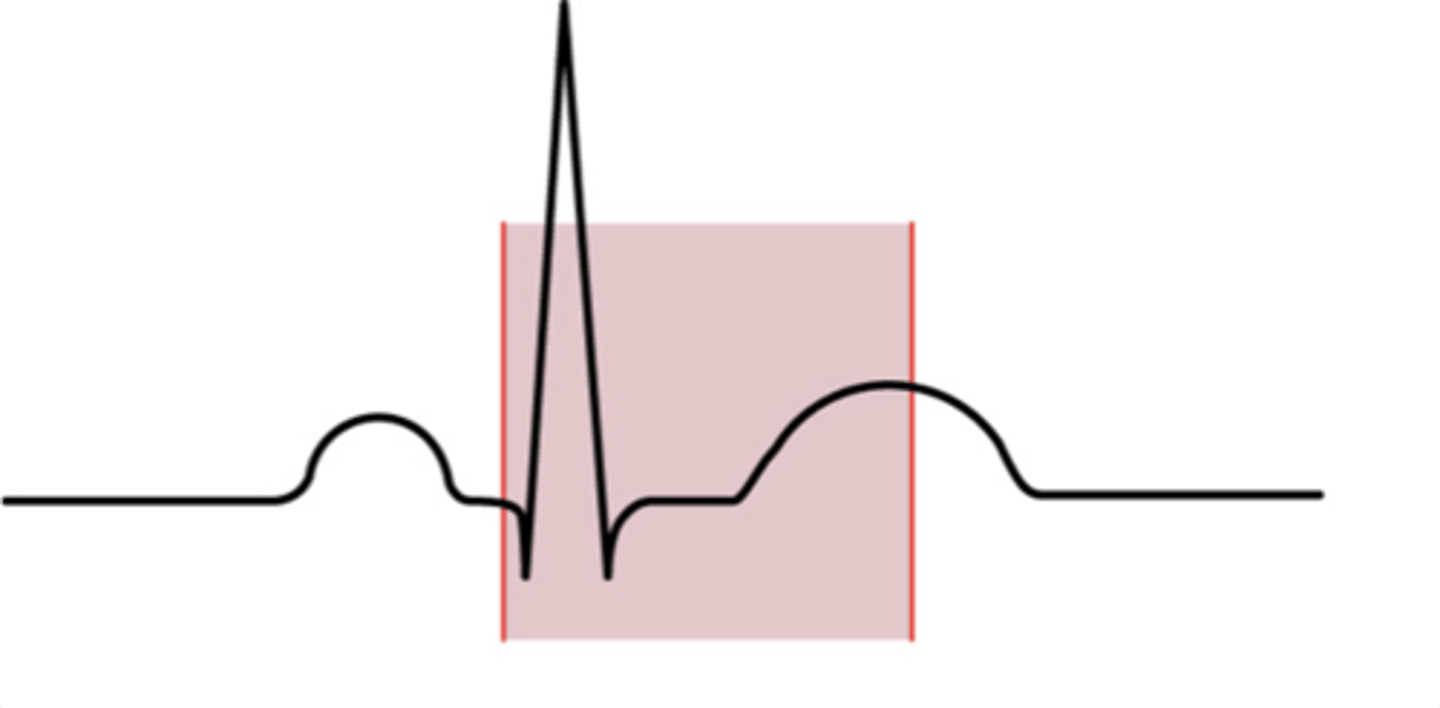
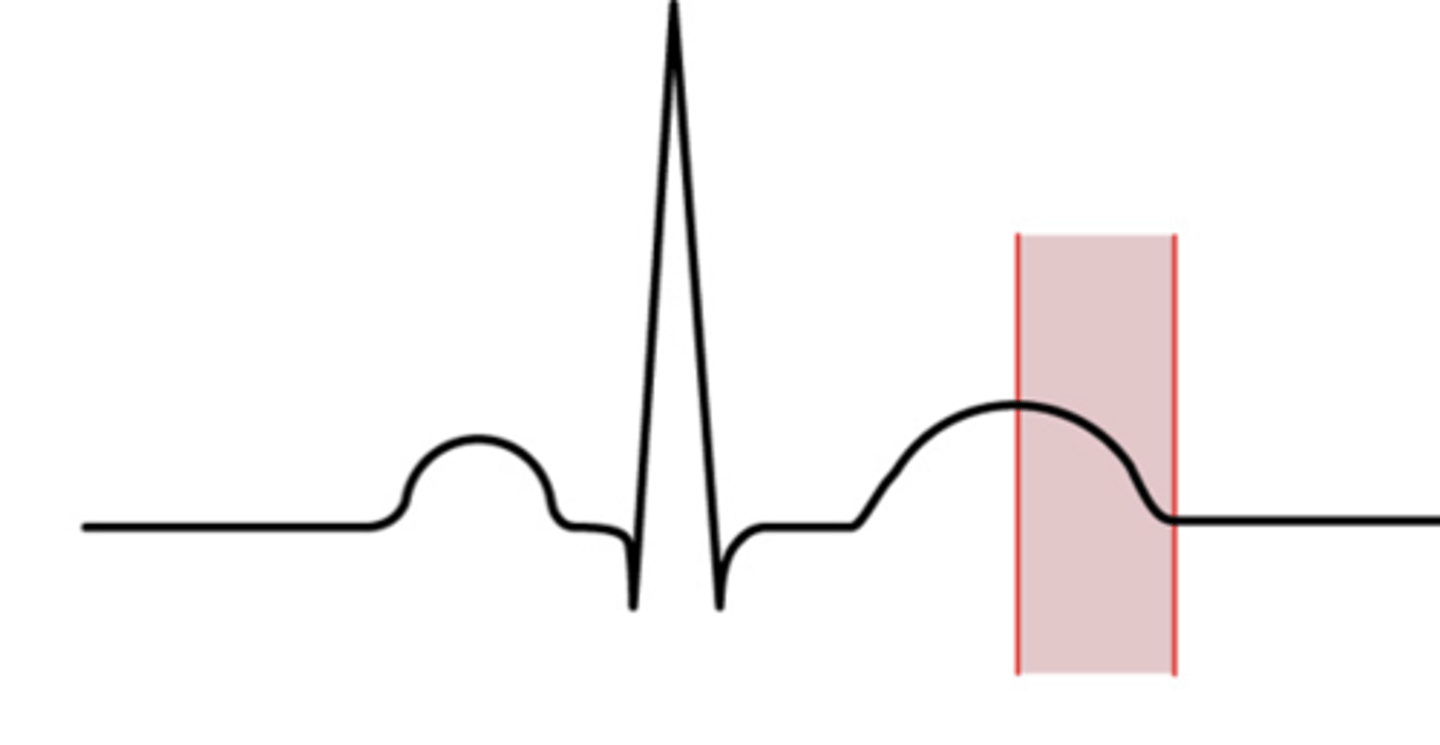
relative refractory period
from the middle of the T-wave to the end of the T-wave; A strong enough outside stimulus can initiate depolarization of the only partially recharged cells.
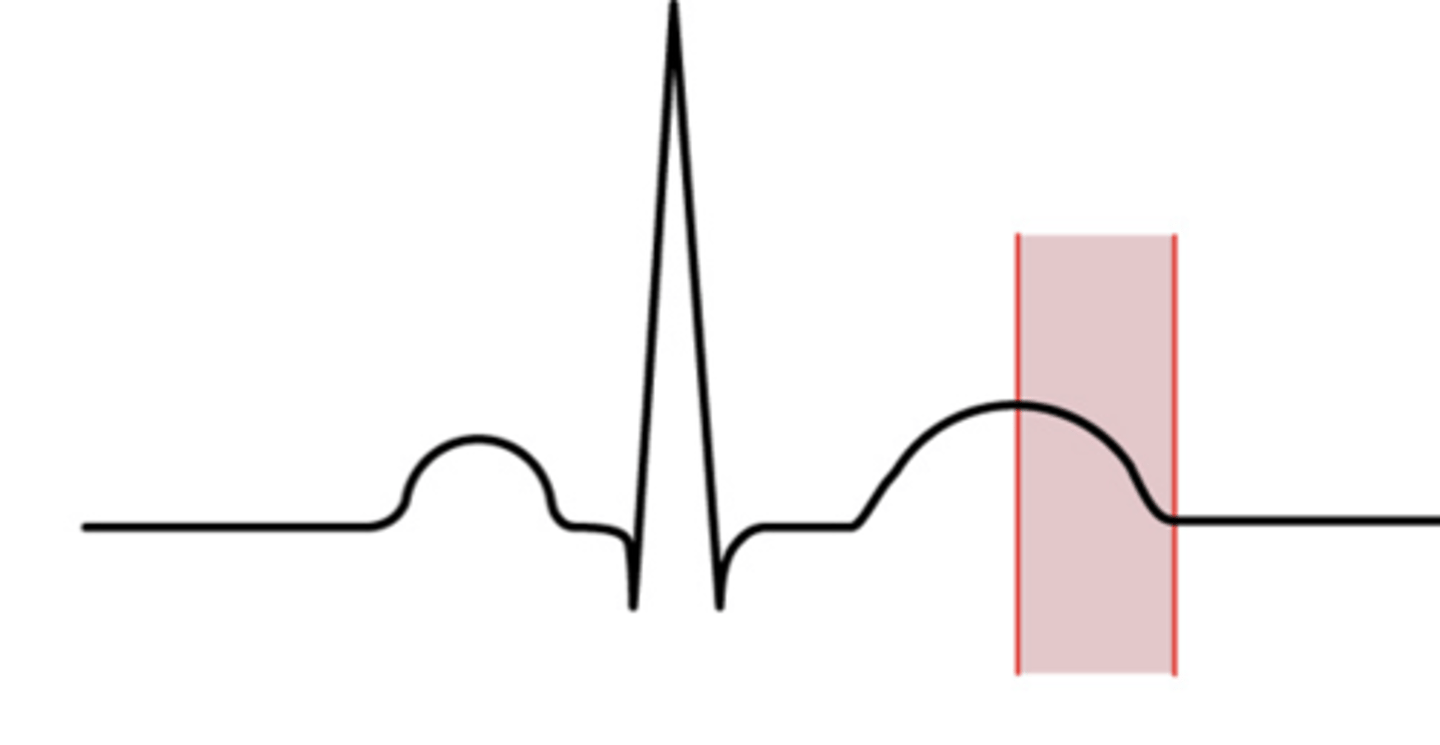
It is a dangerous period that can possibly cause a lethal arrhythmia.
what is the significance of the relative refractory period?
60-100 beats/minute
what is the rate of a Normal Sinus Rhythm?
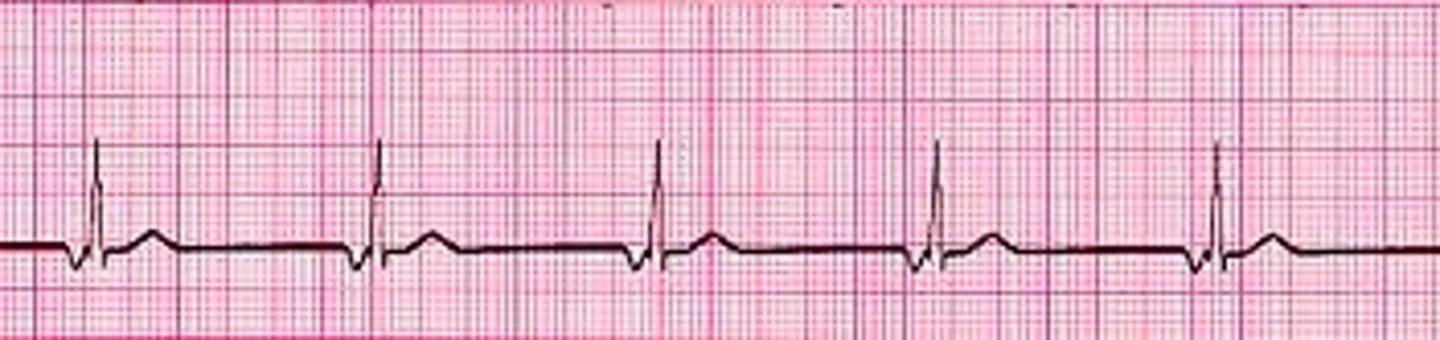
Sinus Bradycardia
how would we define a sinus rhythm less than 60 beats/minute?
-oxygen administration
-atropine (parasympatholytic)
name 2 ways to treat sinus bradycardia
Sinus tachycardia; Beta blocker drugs (sympatholytic)
how would we define a sinus rhythm greater 100 beats/minute? how would we treat that condition?
Sinus Arrythmia
when the SA node fires irregularly, this is called...
1. P-P interval is consistent
2. R-R interval is consistent
name two determining factors of a Normal Sinus Rhythm

1:1; Each QRS Complex should be preceded by 1 P-wave
in a Normal Sinus Rhythm, how what should the P-Wave to QRS Complex ratio be?
Premature Atrial Contraction (PAC)
and ectopic focus that originates outside of the SA node in the atria will cause...
Supraventricular Arrhythmia
an ectopic focus located above the ventricles will cause...
Atrial Flutter
this is caused by a single ectopic focus above the AV node with electrical impulses at a rapid rate; Produces F-waves (saw-tooth pattern) that replace the P-Waves

Atrial Fibrillation (A-Fib)
This arrhythmia is caused by multiple randomly/chaotic firing ectopic atrial foci; Causes atrial "quivering" (no pumping)
Reduces ventricular filling by 20% due to loss of atrial kick
how does atrial fibrillation affect ventricular filling?
Stroke (due to pooling of blood in the left atrium)
Name the risk of left atrium fibrillation
pulmonary embolism (due to pooling of blood in the right atrium)
Name the risk of right atrium fibrillation
Junctional Arrythmia
Supraventricular arrythmia where the SA node is blocked or fails to fire so the AV node assumes the role of pacemaker
an inverted (upside-down) P-Wave
name a key identifier of a Junctional Arrhythmia on an ECG
40-60 beats/min
what is the AV nodes pacemaker rate?
True
True or False: Ventricular Arrythmias are considered more dangerous that Supraventricular Arrhythmias
20-40 beats/minute
what is the pacemaker rate of the Purkinje Fibers?
the ventricles
cells in which part of the heart are considered the least efficient pacemakers?
premature ventricular contraction (PVC)
this arrhythmia is caused by an ectopic focus arising from the ventricles below the Bundle of His, where the QRS (of the ectopic focus) is not preceded by a P-Wave
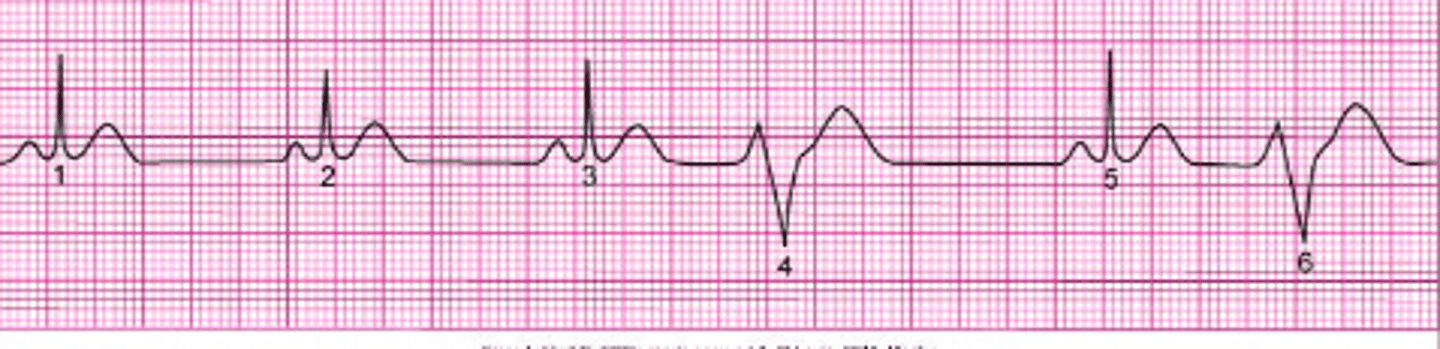
-QRS (of ectopic focus) not preceded by P-Wave
-Compensatory Pause
name two identifying factors of a Premature Ventricular Contraction
Unifocal PVC
a PVC in one area of the ventricle is called...
Multifocal PVCs
a PVC in different areas of the ventricle is called...
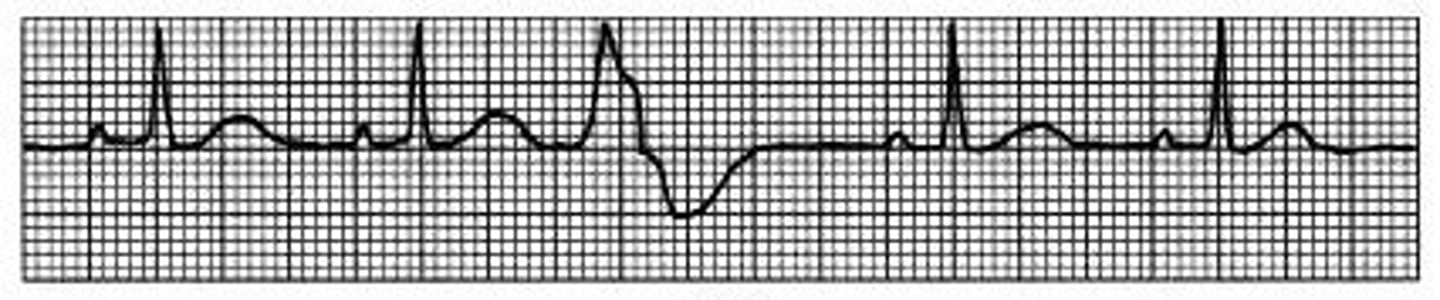
Ventricular Tachycardia (VT)
this arrhythmia is characterized by "successive runs of PVCs," and is lethal
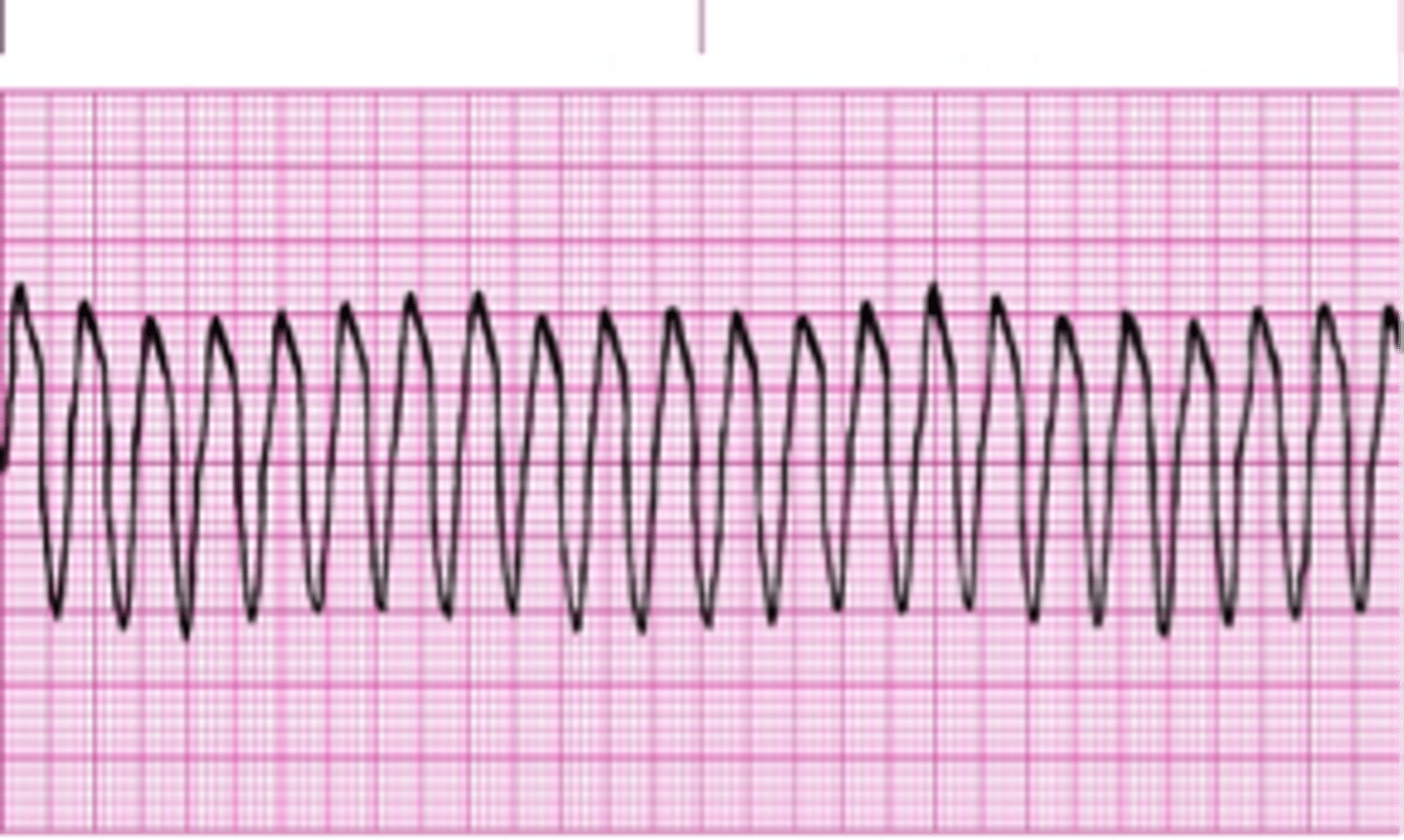
Immediate defibrillation
how do we treat ventricular tachycardia?

high chance of progression to ventricular fibrillation
why is ventricular tachycardia considered lethal?
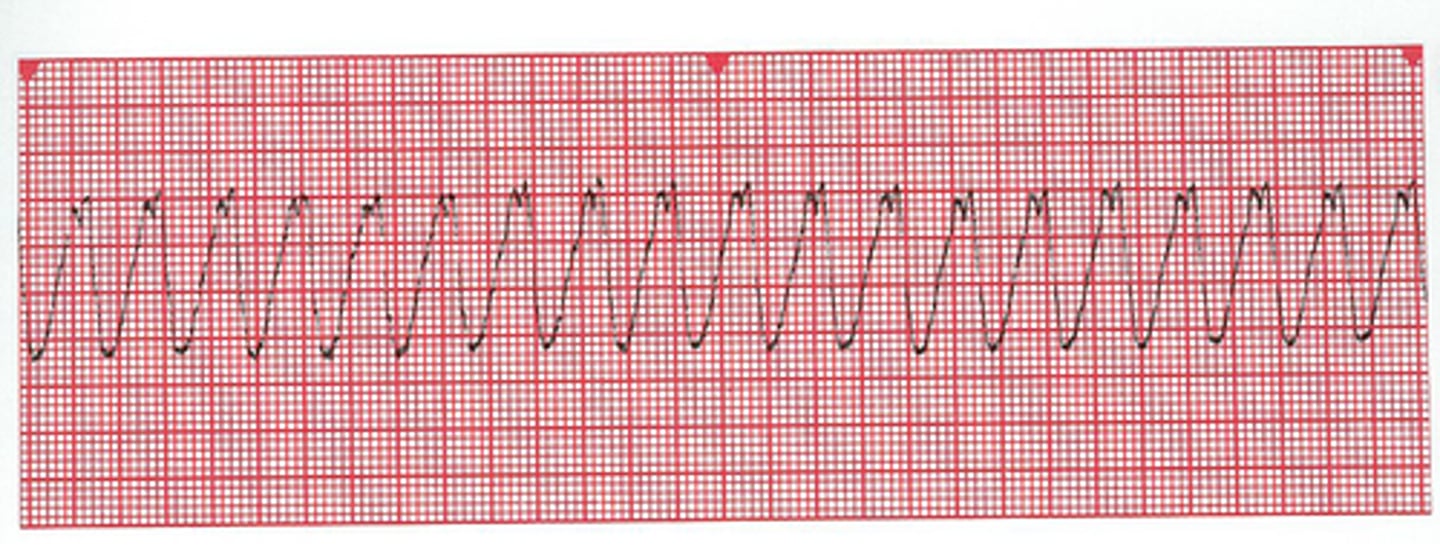
Ventricular Fibrillation (VF)
most lethal arrhythmia; nonfunctional ventricles that quiver with no pumping activity

there's no recognizable waves or complexes
how can you identify ventricular fibrillation on an ECG?
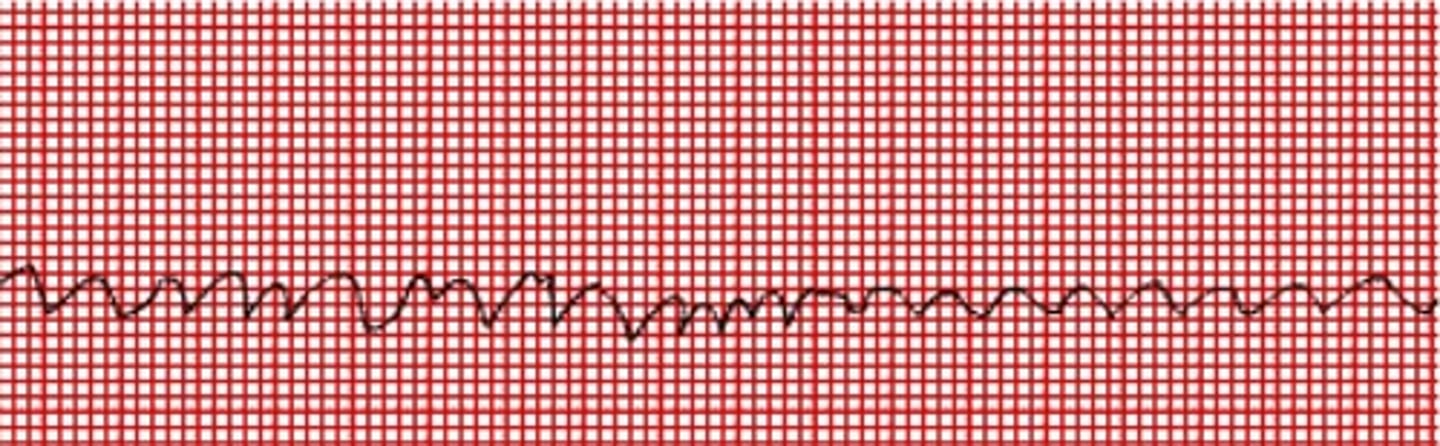
Asystole
"not a rhythm;" Absence of all cardiac electrical activity, represented by a flat line; indicative of clinical death.

myocardial infarction
what is the major cause of asystole
Pulseless Electrical Activity (PEA)
when there is electrical activity but the heart does not contract, this is called...
Second Degree Heart Block AKA Type I (Wenckebach) Heart Block
heart block where the PR segment gradually lengthens until the QRS fails to appear (non-conducted P-Wave)

Third Degree Heart Block
heart block where none of the SA nodal impulses (P-Waves) transmit to the ventricles; no relation between P and QRS waves
