Respiratory System
5.0(2)
Card Sorting
1/55
Earn XP
Description and Tags
Last updated 7:02 PM on 2/21/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
56 Terms
1
New cards
Cellular respiration
Automatic flow of material from an area of
* High concentration → low concentration
* Requires no energy
* Diffusion through lungs=Humans
* High concentration → low concentration
* Requires no energy
* Diffusion through lungs=Humans
2
New cards
Function of the Respiratory system
* ventilation
* gas exchange
* regulation of blood pH
* gas exchange
* regulation of blood pH
3
New cards
Simple Diffusion
* Passive transport
* Works based on a gradient system from high to low concentration
* Directly through the phospholipid bilayer from area of high concentration to low concentration
* Non-polar and lipid-soluble substances
* Ex. CO2, O2, fat soluble vitamins
* Body oxygen are close to the site of diffusion-less distance is less time (quicker)
* Shorter distance=more effective
* Blood is a carrier
* High volume of oxygen travels through blood and blood vessels
* Lung facilitates bulk flow, amount of surface area
* Works based on a gradient system from high to low concentration
* Directly through the phospholipid bilayer from area of high concentration to low concentration
* Non-polar and lipid-soluble substances
* Ex. CO2, O2, fat soluble vitamins
* Body oxygen are close to the site of diffusion-less distance is less time (quicker)
* Shorter distance=more effective
* Blood is a carrier
* High volume of oxygen travels through blood and blood vessels
* Lung facilitates bulk flow, amount of surface area
4
New cards
Conducting Zone
* No diffusion
* Area from nose all the way to the bronchioles
* Responsible for bringing air in
* Nostrils, nasal cavity, pharynx, larynx and trachea
* Area from nose all the way to the bronchioles
* Responsible for bringing air in
* Nostrils, nasal cavity, pharynx, larynx and trachea
5
New cards
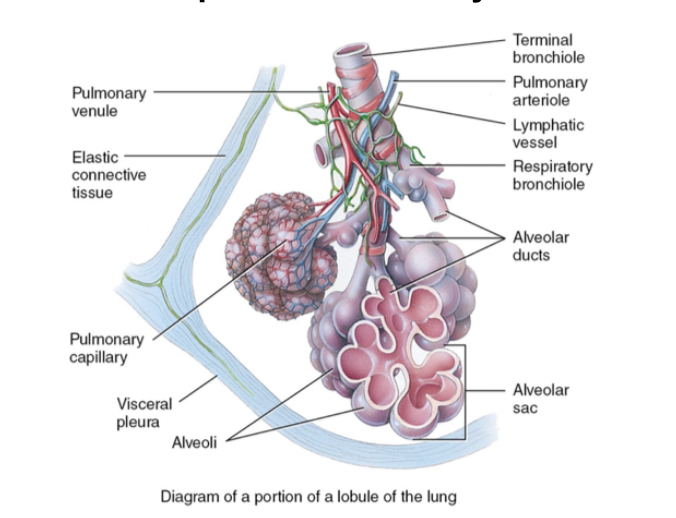
Respiratory Zone
* Where diffusion occurs
* Alveolar duct to alveoli
* Responsible for absorbing air or exchange of gas
* Respiratory bronchioles, alveolar ducts, alveolar sacs, cluster alveoli
* Alveolar duct to alveoli
* Responsible for absorbing air or exchange of gas
* Respiratory bronchioles, alveolar ducts, alveolar sacs, cluster alveoli
6
New cards
Upper Respiratory Tract
Outside of thorax (nose, pharynx, larynx, nasal cavity)
7
New cards
Lower Respiratory Tract
Within the thorax (trachea (windpipe), bronchi, bronchioles, alveoli, lungs)
8
New cards
Apex
Superior Point of Lung
9
New cards
Base
Surface of lung resting on diaphragm
10
New cards
Hilium
Entry and exit point of primary bronchi
11
New cards
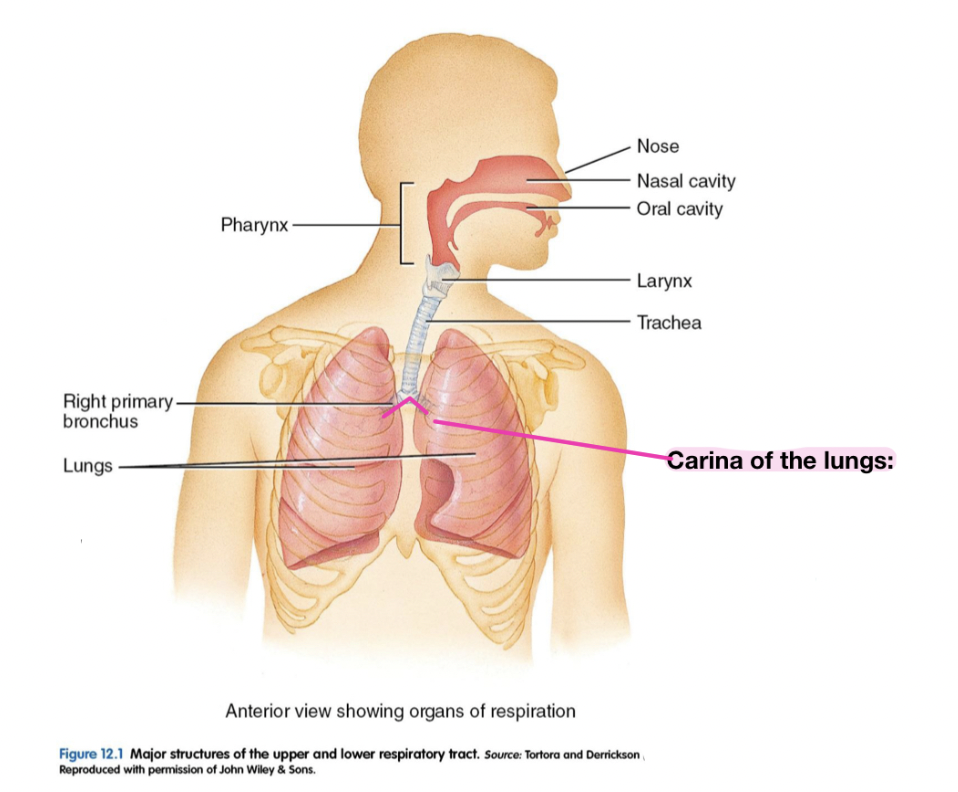
Hilium of lung vs Carina of Lung
%%**Carina of Lung:**%% Trachea bifurcates within the primary bronchi (the “V”)
\
%%**Hilium of the Lung:**%% Supporting structures enter the lung (primary, secondary bronchi, entering the lung pulmonary veins and arteries entering the lung)
\
%%**Hilium of the Lung:**%% Supporting structures enter the lung (primary, secondary bronchi, entering the lung pulmonary veins and arteries entering the lung)
12
New cards
Fissures
Narrow division separating the lungs into lobes
13
New cards
Cardiac Impression
Concavity in which the heart rests
14
New cards
Superficial to deep
1. Parietal pleura
2. Pleural cavity
3. Visceral pleura
4. Lung tissue
15
New cards
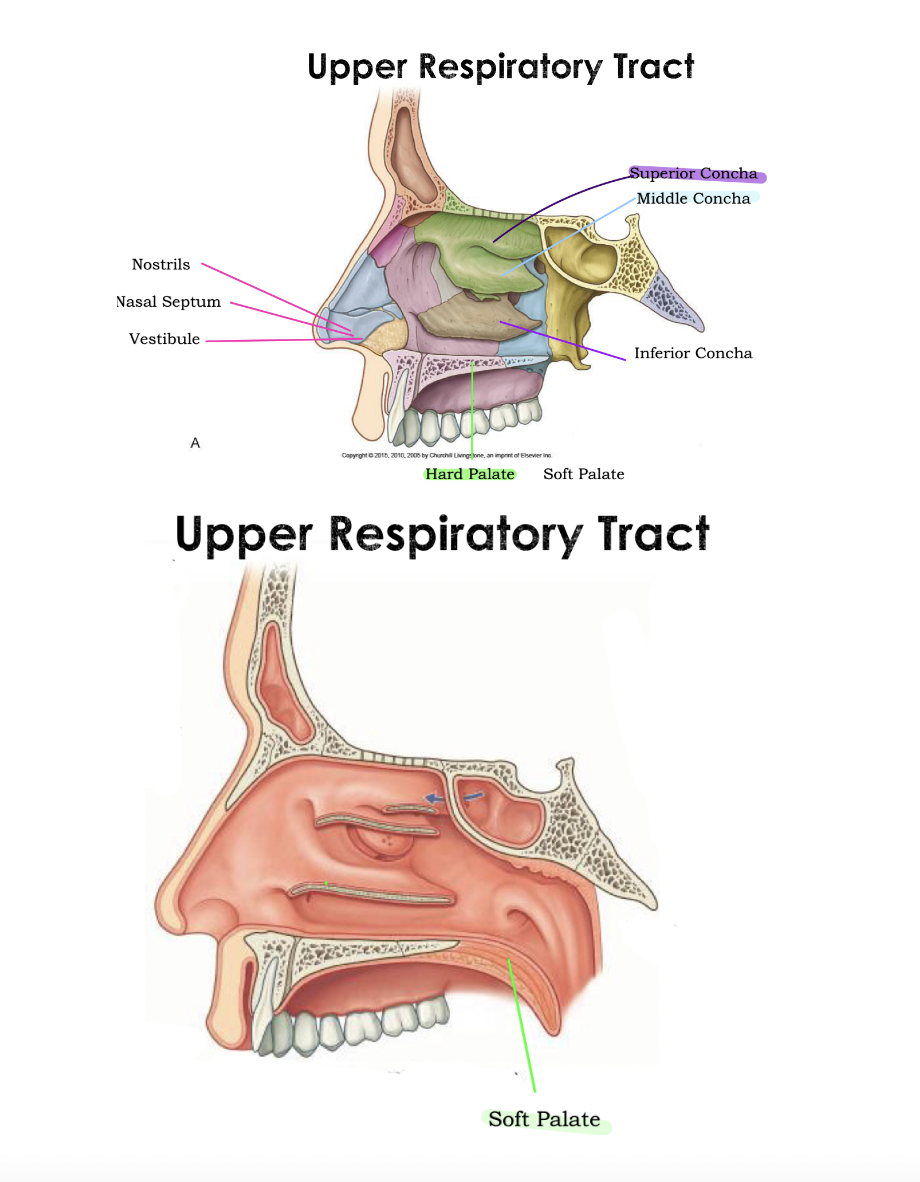
Upper Respiratory Tract
* **Pharynx:** Where the nasal and oral cavity connect
Divided into 3 regions
* ==**Nasopharynx:**== Behind the nose, Connects the nasal cavity to the oropharynx and is separated from the oral cavity by soft palpate.
\- Leads to auditory (eustachian tubes)
* ==**Oropharynx:**== Behind oral cavity, Sits behind the soft palate and upper border of the epiglottis and posterior to the oral cavity and tongue and found immediately with Laryngopharynx
\- Passageway for food, drinks and air
* ==**Laryngopharynx:**== Behind larynx and underneath oropharynx, terminates at the level of the cricoid cartilage by becoming continuous with the esophagus.
\- Passageway for food, drinks and air
Divided into 3 regions
* ==**Nasopharynx:**== Behind the nose, Connects the nasal cavity to the oropharynx and is separated from the oral cavity by soft palpate.
\- Leads to auditory (eustachian tubes)
* ==**Oropharynx:**== Behind oral cavity, Sits behind the soft palate and upper border of the epiglottis and posterior to the oral cavity and tongue and found immediately with Laryngopharynx
\- Passageway for food, drinks and air
* ==**Laryngopharynx:**== Behind larynx and underneath oropharynx, terminates at the level of the cricoid cartilage by becoming continuous with the esophagus.
\- Passageway for food, drinks and air
16
New cards
Pharynx
Five tonsils:
* Mouth open: 2 Palatine, Lingual pharyngeal or adenoid tonsils
* Lined with non-keratinized stratified squamous epithelium
* Nasal cavity is separated by the septum (cartilage and vomer bone)
* Air will enter through the nostrils, move towards the nasals cavity (divide into septum), most towards the pharynx and then towards the trachea
* @@**Nasal vestibule:**@@ Nose hair
\
@@**Concha role:**@@ Air more turbulent + more surface area cause air to become moist and warm
\- Lined with mucuous membrane made from pseudostratified ciliated columnar epithelium which contain capillaries and goblet cells
\-Blood flows through the capillaries warms the passing airs while mucous moistens
\-Mucus covered cut particles are propelled by the cilia towards the pharynx, where they can be swallowed or expectorated
* Mouth open: 2 Palatine, Lingual pharyngeal or adenoid tonsils
* Lined with non-keratinized stratified squamous epithelium
* Nasal cavity is separated by the septum (cartilage and vomer bone)
* Air will enter through the nostrils, move towards the nasals cavity (divide into septum), most towards the pharynx and then towards the trachea
* @@**Nasal vestibule:**@@ Nose hair
\
@@**Concha role:**@@ Air more turbulent + more surface area cause air to become moist and warm
\- Lined with mucuous membrane made from pseudostratified ciliated columnar epithelium which contain capillaries and goblet cells
\-Blood flows through the capillaries warms the passing airs while mucous moistens
\-Mucus covered cut particles are propelled by the cilia towards the pharynx, where they can be swallowed or expectorated
17
New cards
Soft Palate
Blocking of nasal cavity, prevents food from entering nasal cavity
18
New cards
Hard Palate
Forms with palatine bones, maxillae
19
New cards
Tonsils
Lymph nodules and part of defense system
20
New cards
Crypts
Epithelial lining of their surface which has deep folds
21
New cards
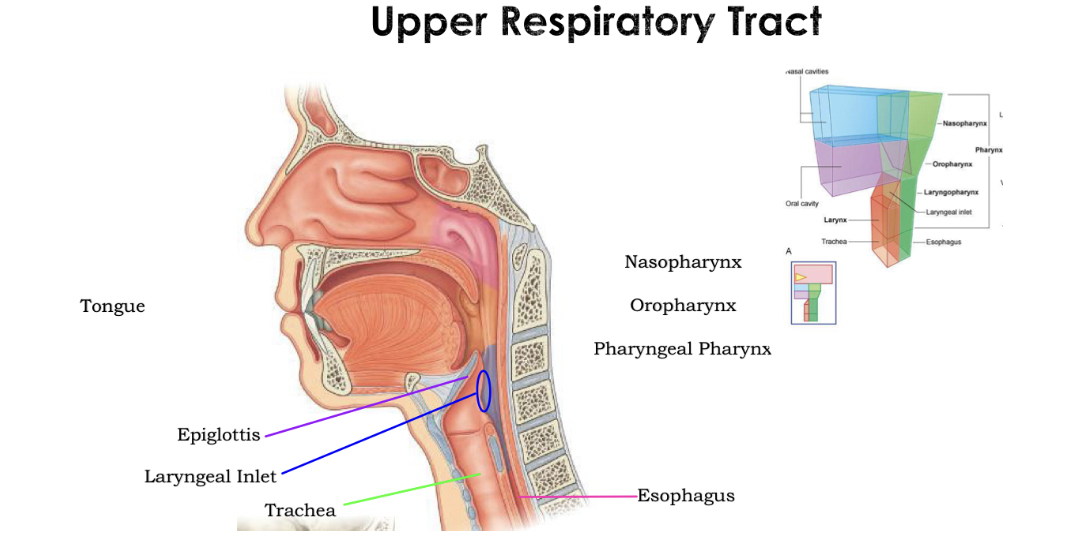
Upper Respiratory diagram
* Around the soft palate the oral cavity to the nasal cavity
* ^^**Large area=**^^Tongue
* Superior to the tongue=Hard and soft palate
* ^^**Door**^^=Epiglottis (automatically closes when swallowing food byt stays open when breathing)
* ^^**Laryngeal inlet**^^=Producing area of epiglottis (blue area)
* ^^**Anterior to the esophagus**^^=Trachea
* ^^**Large area=**^^Tongue
* Superior to the tongue=Hard and soft palate
* ^^**Door**^^=Epiglottis (automatically closes when swallowing food byt stays open when breathing)
* ^^**Laryngeal inlet**^^=Producing area of epiglottis (blue area)
* ^^**Anterior to the esophagus**^^=Trachea
22
New cards
Contents of the thoracic cavity
* Heart
* Lungs
* Distal trachea
* Esophagus
* Lungs
* Distal trachea
* Esophagus
23
New cards
Thorax: Container
* Bony cage formed by the vertical column, ribs and sternum
* Intercostal spaces- contain intercostal muscles, veins, arteries and nerves
* Provides attachment point for many muscles (upper limb, neck, abdomen, and back)
* Functional importance in respiration: resists negative pressure
* Protects thoracic cavity
* Intercostal spaces- contain intercostal muscles, veins, arteries and nerves
* Provides attachment point for many muscles (upper limb, neck, abdomen, and back)
* Functional importance in respiration: resists negative pressure
* Protects thoracic cavity
24
New cards
Thorax
* 12 pairs of ribs
* 12 pairs of costal cartilages
* 12 thoracic vertebrae (and intervertebral disks) The sternum (manubrium of the sternum, body of sternum, Xiphoid process)
* 12 pairs of costal cartilages
* 12 thoracic vertebrae (and intervertebral disks) The sternum (manubrium of the sternum, body of sternum, Xiphoid process)
25
New cards
3 Major cavities
* **Right pulmonary cavity:** Houses right lung
* **Mediastinum:** Houses heart and great vessels
* **Left pulmonary cavity:** Houses left lung
\
* **Mediastinum:** Houses heart and great vessels
* **Left pulmonary cavity:** Houses left lung
\
26
New cards
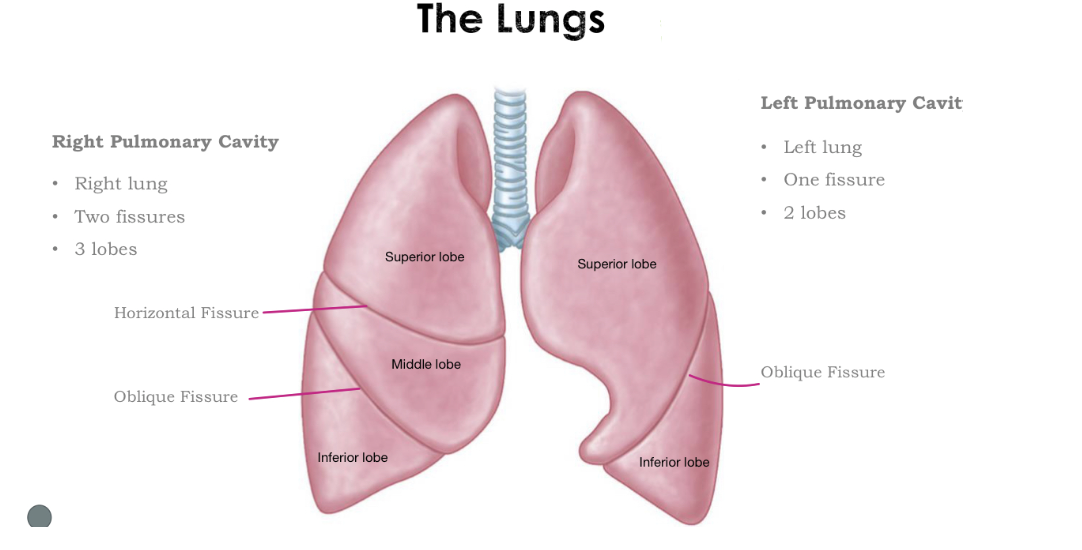
The Lungs
**Right side:**
__**3 lobes:**__ **Superior, middle, and inferior**
* **Two fissures:** Oblique and Horizontal
* **Right lung**
\
^^**Left side:**^^
**2 lobes:** Superior and inferior
* **One fissure:** Oblique Fissure
* **Left lung**
__**3 lobes:**__ **Superior, middle, and inferior**
* **Two fissures:** Oblique and Horizontal
* **Right lung**
\
^^**Left side:**^^
**2 lobes:** Superior and inferior
* **One fissure:** Oblique Fissure
* **Left lung**
27
New cards
Pulmonary Pleurae
Invagination of the lungs
* The lungs are covered by a 2 layer of pleurae (outermost layer, the parietal pleura, and inner layer that directly covers the lung, the visceral pleura) through a process known as invagination
* The lungs invaginate into the pleura from the medial aspect, thus the visceral layer meets the parietal layer at the roots of the lungs
* The lungs are covered by a 2 layer of pleurae (outermost layer, the parietal pleura, and inner layer that directly covers the lung, the visceral pleura) through a process known as invagination
* The lungs invaginate into the pleura from the medial aspect, thus the visceral layer meets the parietal layer at the roots of the lungs
28
New cards
2 layers of Pulmonary Pleurae
1. **Parietal**
2. **Visceral (touches the lung)**
\
* The **fluid-filled** space between the parietal pleura and visceral pleura is known as the __**pleural cavity**__
* __**Function:**__ Friction/Lubricant and adhesion/surface tension
* Medial to lateral=Invagination
* Superior to inferior=Invagination of the heart
* Pleural cavity: Space between the visceral and parietal
* Lung needs to expand and shrink
* When there is negative pressure, we need a lubricant and adhesioin to create a frictionless environment
29
New cards
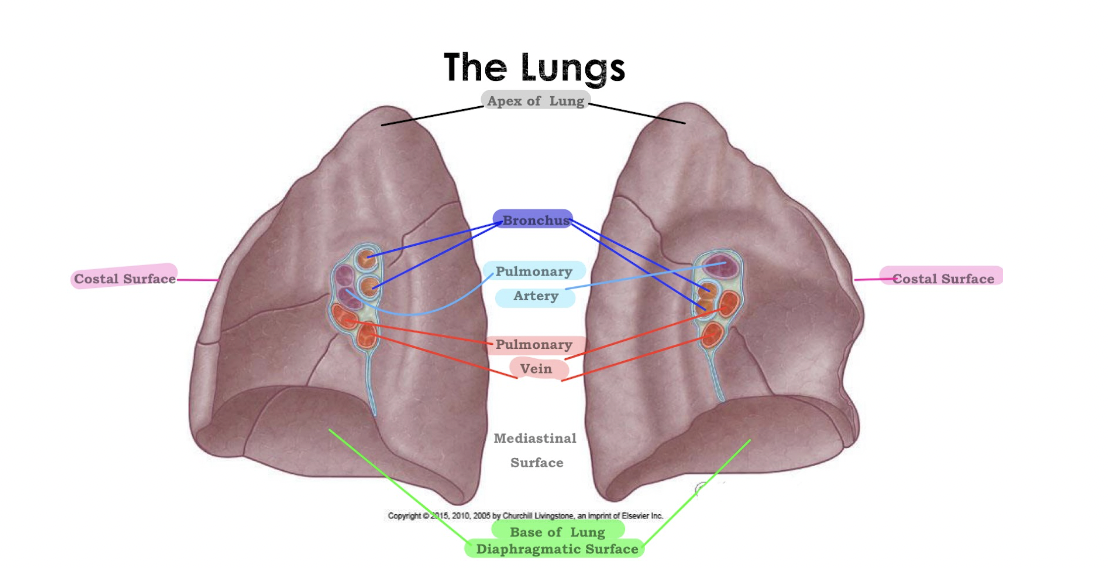
The Lungs
30
New cards
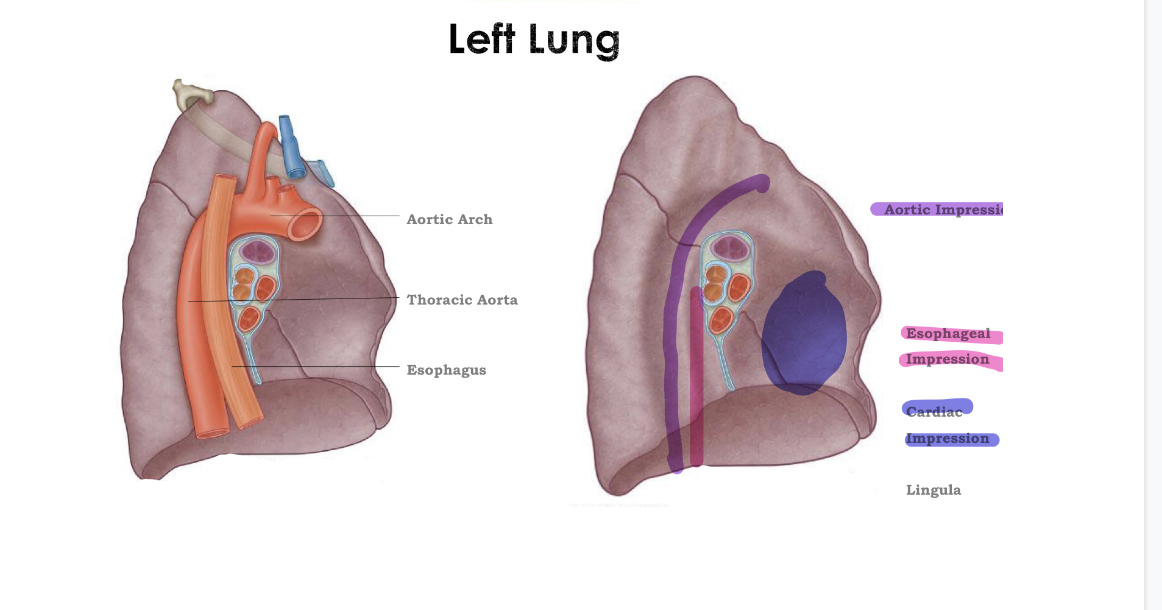
Left Lung
31
New cards
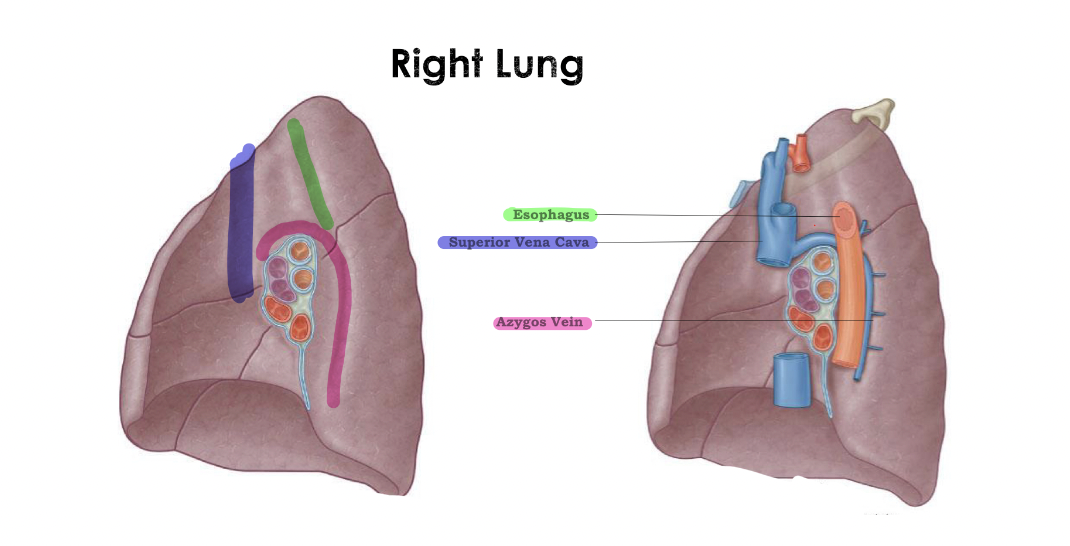
Right Lung
\
32
New cards
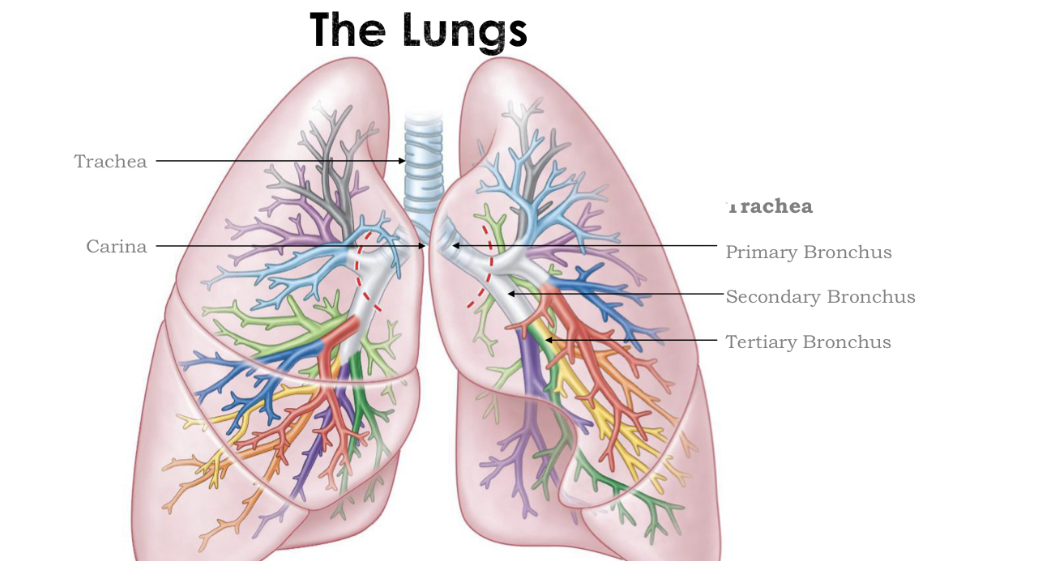
The Lungs
* __***Lower respiratory Tract (within the tract): Lungs, Larynx, Trachea and Right/Left primary bronchi***__
* **Larynx:** Voicebox and connects the trachea and laryngopharynx
* 3 single pieces: __***Thyroid cartilage***__ (adams apple), __***epiglottis***__ (leaf shape of elastic cartilage attached to the top of the larynx), __***cricoid cartilage***__ (Protect vocal chords)
* **Function of epiglottis:** Protect airway from food and water
\- When it comes to swallowing, epiglottis blocks entry to the larynx and food/liquids are diverted toward the esophagus
* **First division:** Primary bronchus
* **Secondary division:** Secondary bronchus
* **Tertiary division:** Tertiary bronchus
* **Larynx:** Voicebox and connects the trachea and laryngopharynx
* 3 single pieces: __***Thyroid cartilage***__ (adams apple), __***epiglottis***__ (leaf shape of elastic cartilage attached to the top of the larynx), __***cricoid cartilage***__ (Protect vocal chords)
* **Function of epiglottis:** Protect airway from food and water
\- When it comes to swallowing, epiglottis blocks entry to the larynx and food/liquids are diverted toward the esophagus
* **First division:** Primary bronchus
* **Secondary division:** Secondary bronchus
* **Tertiary division:** Tertiary bronchus
33
New cards
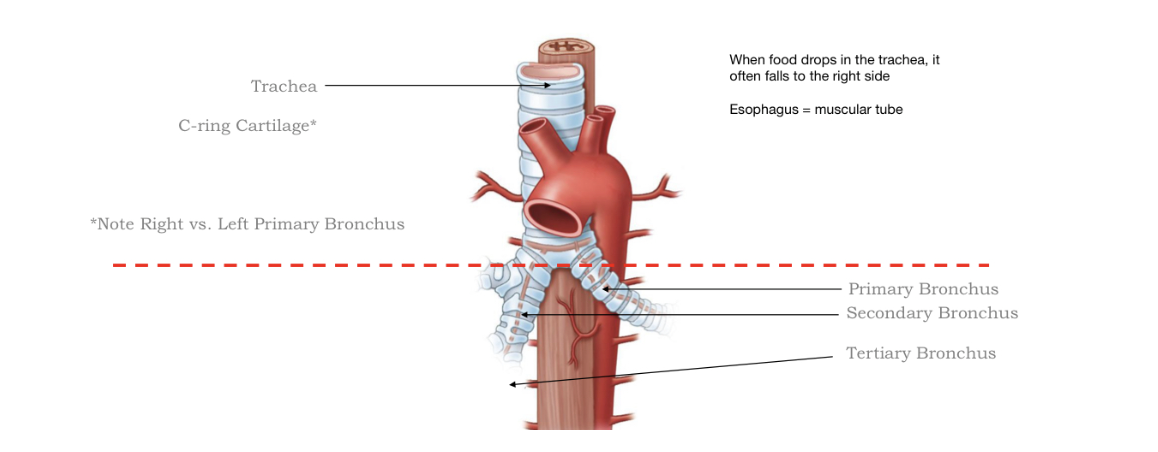
Trachea
* Tubular vessel that carries air from the larynx down towards the lungs
* Lined with pesudostratified ciliated columnar epithelium
* **C-ring cartilage:** Prevents the trachea from collapsing from negative pressure, wont be able to suck air in
* Trachealis muscle=Posterior aspect
* Lined with pesudostratified ciliated columnar epithelium
* **C-ring cartilage:** Prevents the trachea from collapsing from negative pressure, wont be able to suck air in
* Trachealis muscle=Posterior aspect
34
New cards
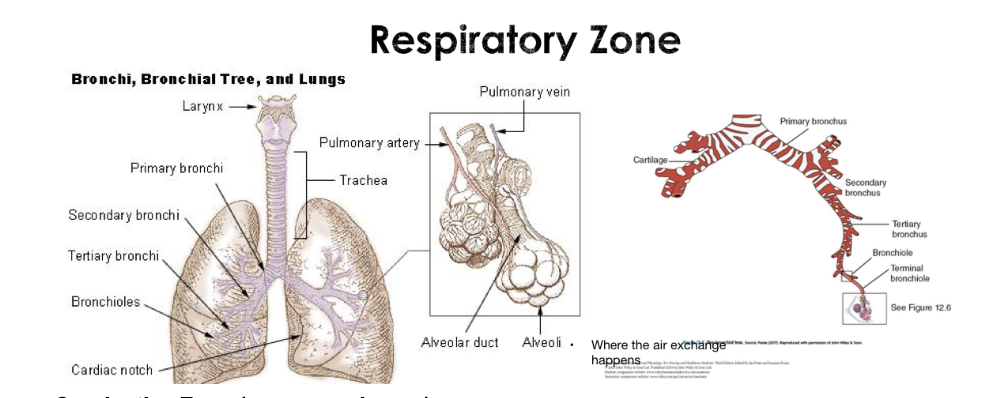
Respiratory Zone
@@**Respiratory Zone (gas exchange)**@@
* Bronchioles —> Alveoli
\
@@**Conductive zone (no gas exchange)**@@
* Mouth/nose —> Trachea —> Larynx —> Bronchi
* Humidifies, warm, and filters air
* Bronchioles —> Alveoli
\
@@**Conductive zone (no gas exchange)**@@
* Mouth/nose —> Trachea —> Larynx —> Bronchi
* Humidifies, warm, and filters air
35
New cards
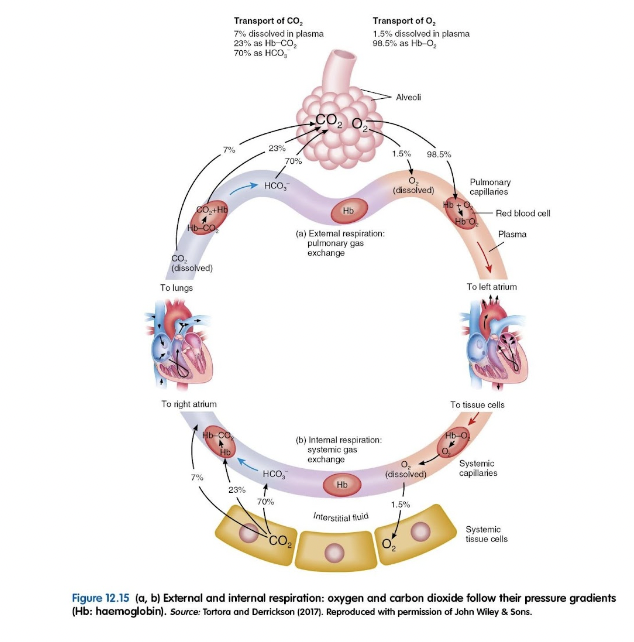
Respiration
* Process by which oxygen and carbon dioxide are exchanged between the atmosphere and body cells
\
==__**4 Distinct Phases**__==
1. **Pulmonary ventilation:** How air gets in/out of lungs
2. **External respiration:** Oxygen diffuses from the lungs to the bloodstream and how carbon dioxide diffused from blood and to the lungs
3. **Transport of gasses:** Oxygen and Carbon dioxide are transported between the lungs and body tissue
4. **Internal respiration:** How oxygen is delivered to and carbon dioxide from body cells
\
==__**4 Distinct Phases**__==
1. **Pulmonary ventilation:** How air gets in/out of lungs
2. **External respiration:** Oxygen diffuses from the lungs to the bloodstream and how carbon dioxide diffused from blood and to the lungs
3. **Transport of gasses:** Oxygen and Carbon dioxide are transported between the lungs and body tissue
4. **Internal respiration:** How oxygen is delivered to and carbon dioxide from body cells
36
New cards
Mechanics of Breathing Pulmonary Ventilation
* Lungs dont have muscles to expand they open up and expand because of the negative pressure
* When the diaphragm contracts, it flattens out, causes larger volume of the thoracic cavity which allows for more room for the lungs
* Thoracic walls lifts up, diaphragm drops down
\
* When the diaphragm contracts, it flattens out, causes larger volume of the thoracic cavity which allows for more room for the lungs
* Thoracic walls lifts up, diaphragm drops down
\
37
New cards
Inspiration
* Diaphragm
* External intercostal muscles
* They contract and bring air in
* As diaphram contracts it flattens out and increases the volume within the thoracic cavity
* The two muscles listed above job is to increase the thoracic cavity volume
* External intercostal muscles
* They contract and bring air in
* As diaphram contracts it flattens out and increases the volume within the thoracic cavity
* The two muscles listed above job is to increase the thoracic cavity volume
38
New cards
Exhalation
* Passive: No muscles
* Forced: Internal intercostal muscles and abdominal muscles
* Forced: Internal intercostal muscles and abdominal muscles
39
New cards
Pulmonary ventilation
Deliver of oxygen into and expulsion of carbon dioxide and water out of the lungs
40
New cards
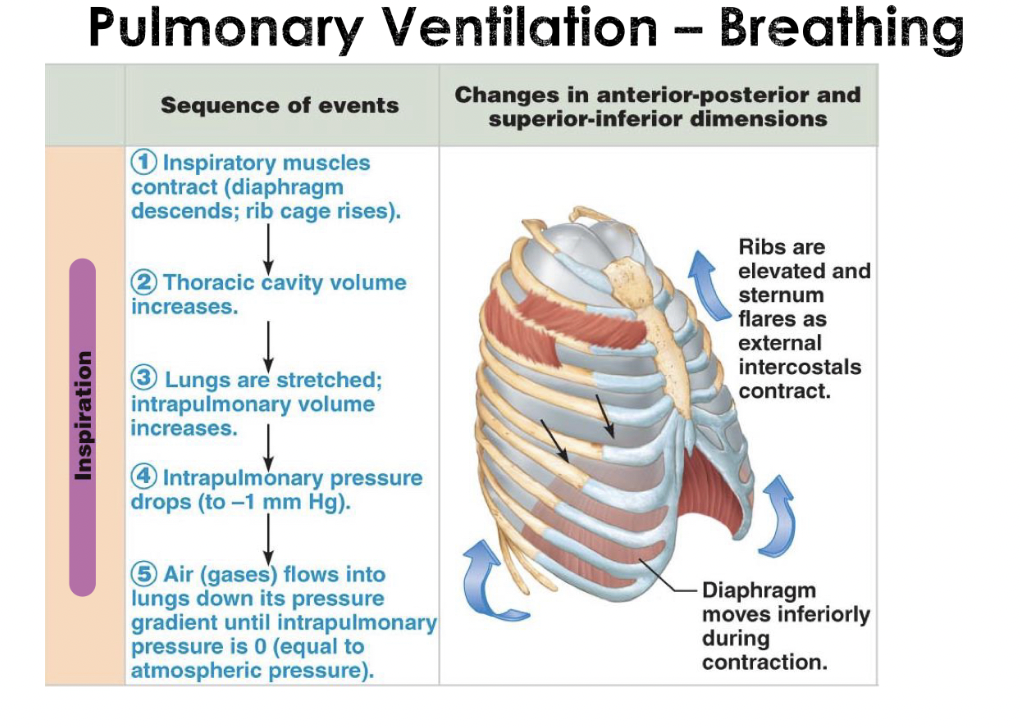
Pulmonary Ventilation- Breathing Inspiration
* During inhalation, air pressure in the atmosphere is higher than in the lungs, so air flows into the lungs.
41
New cards
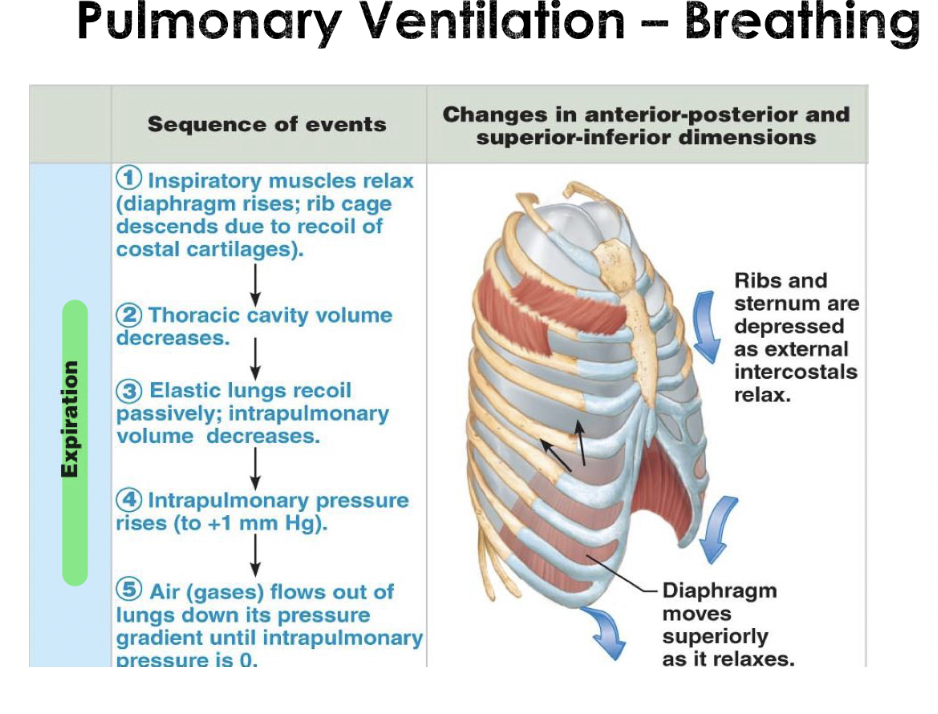
Pulmonary Ventilation Breathing Expiration
* Decreasing the volume of the lungs will increase the air pressure in the lungs, and air flows out. During exhalation, the lungs revert back to their original size, pressure in the lungs rises compared to atmospheric pressure and air moves out.
42
New cards
External Respiration Pulmonary Gas Exchange
* Exchange of oxygen and carbon dioxide between the air in our alveoli and blood in our pulmonary circulation
\
^^**Alveoli**^^
* Consists of one single layer of epithelia
* Composed of simple squamous epithelium
* Where gas exchange occurs
^^**External Respiration**^^
* Bringing air close to the blood vessels
* Simple diffusion taking place based from concentration gradients
* From higher concentration to lower concentration
\
^^**Alveoli**^^
* Consists of one single layer of epithelia
* Composed of simple squamous epithelium
* Where gas exchange occurs
^^**External Respiration**^^
* Bringing air close to the blood vessels
* Simple diffusion taking place based from concentration gradients
* From higher concentration to lower concentration
43
New cards
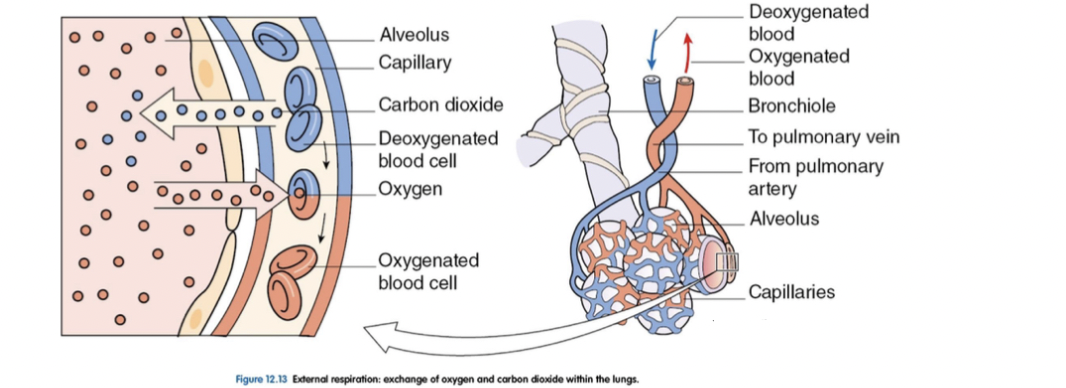
External Respiration Pulmonary Gas Exchange
* Describes both the bulk flow of air into and out of the lungs and the transfer of oxygen and carbon dioxide into the bloodstream through diffusion
* Occurs beyond the respiratory bronchioles diffusion of oxygen from alveoli into pulmonary circulation
* oxygen diffuses across the respiratory membrane from the alveolus to the capillary, whereas carbon dioxide diffuses out the capillary into the alveolus
* Pulmonary Arteries (in blue): Bringing back deoxygenated blood that interacts with the lungs
* Pulmonary Veins (in red): Brings back the oxygenated blood
* Capillary beds: Close to the single layers squamous cells
* Occurs beyond the respiratory bronchioles diffusion of oxygen from alveoli into pulmonary circulation
* oxygen diffuses across the respiratory membrane from the alveolus to the capillary, whereas carbon dioxide diffuses out the capillary into the alveolus
* Pulmonary Arteries (in blue): Bringing back deoxygenated blood that interacts with the lungs
* Pulmonary Veins (in red): Brings back the oxygenated blood
* Capillary beds: Close to the single layers squamous cells
44
New cards
Oxygen
* In the atmosphere there is 21%
* Blood within the capillaries is not going to have the same concentration level because it is coming back from the heart
* No oxygenated, will have higher cardioxide than low oxygen
* Oxygen from the alveolus will diffuse into the capillaries because theres a lower concentration gradient of oxygen within the capillaries directly
* Will be brought back to the heart into the left atrium
* Blood within the capillaries is not going to have the same concentration level because it is coming back from the heart
* No oxygenated, will have higher cardioxide than low oxygen
* Oxygen from the alveolus will diffuse into the capillaries because theres a lower concentration gradient of oxygen within the capillaries directly
* Will be brought back to the heart into the left atrium
45
New cards
Ventilation-Perfusion Coupling
* **Low oxygen =** Constriction
* **High Oxygen =** Dilation
* If there is no air, your arteries and veins will vasoconstrict i.e. they’ll prevent blood from going to that area
* If you gain a lot of air in the alveolar sac, you will end up having vasodilation where more blood will go into this area in order to dump CO2 and pickup O2
* Goal is to best match the high blood supply and alveoli with the high O2 or low CO2 content
* Want to bring the most amount of blood to the alveolar sac that has the most amount of oxygen in it and least amount of CO2 in it
* **High Oxygen =** Dilation
* If there is no air, your arteries and veins will vasoconstrict i.e. they’ll prevent blood from going to that area
* If you gain a lot of air in the alveolar sac, you will end up having vasodilation where more blood will go into this area in order to dump CO2 and pickup O2
* Goal is to best match the high blood supply and alveoli with the high O2 or low CO2 content
* Want to bring the most amount of blood to the alveolar sac that has the most amount of oxygen in it and least amount of CO2 in it
46
New cards
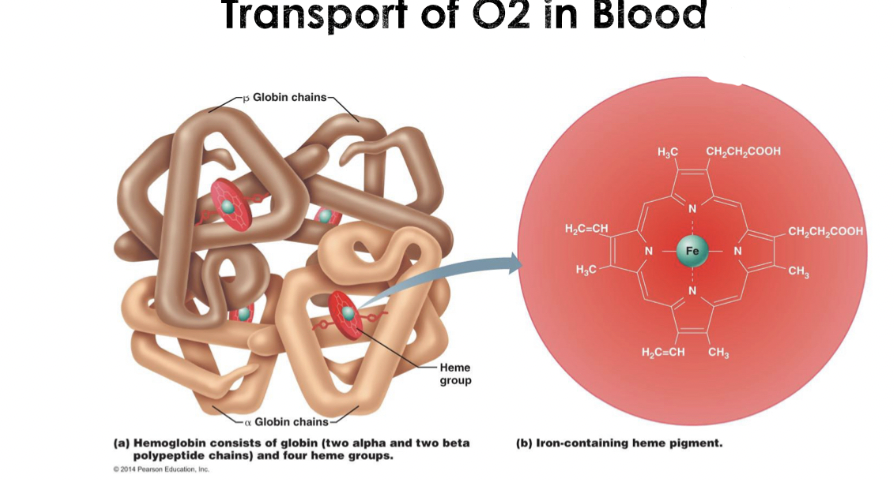
Transports of O2 in Blood
* Blood is our transporter of oxygen from the lungs to the tissue
* ***1 hemoglobin can carry 4 oxygen molecules***
* ***Most of the oxygen is carried through the hemoglobin - total of 8 oxygen molecules, this is before the oxygen molecules are on the hemoglobin***
* **Reversible bonding**: able to carry oxygen from the lungs and able to release and drop it off to the site (i.e. muscle tissue)
* ***1 hemoglobin can carry 4 oxygen molecules***
* ***Most of the oxygen is carried through the hemoglobin - total of 8 oxygen molecules, this is before the oxygen molecules are on the hemoglobin***
* **Reversible bonding**: able to carry oxygen from the lungs and able to release and drop it off to the site (i.e. muscle tissue)
47
New cards
Blood
\
* Red blood cell has hemoglobin
* Hemoglobin is capable of carrying four different oxygen molecules
* Job of red blood cells is to carry respiratory gases such as O2 and CO2
* Hemoglobin is made up of four polypeptides aka. Protein groups (globin chains)
* It has iron in the center, this is where the oxygen is going to bind to this iron
* One red blood cell contains 250 million hemoglobin therefore one red blood cell is capable of carrying 1 billion oxygen
* Capable of carrying 20% of CO2 in the blood
* CO2 binds to the polypeptide chains
* Carbon Monoxide is deadly
* Most oxygen is going to be transported through hemoglobin, only about 1.5% of oxygen is dissolved within the plasma itself but 98.5% of it is carried through the hemoglobin group four oxygen on each hemoglobin
* Red blood cell has hemoglobin
* Hemoglobin is capable of carrying four different oxygen molecules
* Job of red blood cells is to carry respiratory gases such as O2 and CO2
* Hemoglobin is made up of four polypeptides aka. Protein groups (globin chains)
* It has iron in the center, this is where the oxygen is going to bind to this iron
* One red blood cell contains 250 million hemoglobin therefore one red blood cell is capable of carrying 1 billion oxygen
* Capable of carrying 20% of CO2 in the blood
* CO2 binds to the polypeptide chains
* Carbon Monoxide is deadly
* Most oxygen is going to be transported through hemoglobin, only about 1.5% of oxygen is dissolved within the plasma itself but 98.5% of it is carried through the hemoglobin group four oxygen on each hemoglobin
48
New cards
Blood Composition
* **Blood is made up of:**
* **Plasma: non living fluid matrix (mostly water) (no cells in it)**
* **Formed elements - living blood “cells” suspended in plasma**
* ***Erythrocytes*** **(red blood cells, or RBCS)**
* ***Leukocytes*** **(white blood cells, or WBCs)**
* ***Platelets*****: Flowing within your plasma**
* Composes a big amount of our body
* 8% of your body weight
* In males about 5-6L (volume)
* In females 4-5L (volume)
* **Plasma: non living fluid matrix (mostly water) (no cells in it)**
* **Formed elements - living blood “cells” suspended in plasma**
* ***Erythrocytes*** **(red blood cells, or RBCS)**
* ***Leukocytes*** **(white blood cells, or WBCs)**
* ***Platelets*****: Flowing within your plasma**
* Composes a big amount of our body
* 8% of your body weight
* In males about 5-6L (volume)
* In females 4-5L (volume)
49
New cards
Functions of Blood
1. **Distribution**
* Deliver O2 and nutrients to body cells
* Transport waste products from cells to elimination sites (Get rid of waste products like carbon dioxide so blood is a distribution center)
* Transport hormones from endocrine organs to target organs
\
2. **Regulation**
* Maintain body temp (Release heat through the skin, increase blood flow in the skin area)
* Maintain normal pH (Blood can increase or decrease acidity based on what we need to do)
* Maintain fluid volume
\
3. **Protection**
* Prevent blood loss (Blood plasma has proteins and they can initiate clot formation to prevent that blood loss
* Prevent infection (Blood holds all sorts of things in it like antibodies, white blood cells that will defend against foreign invaders that can cause an infection)
50
New cards
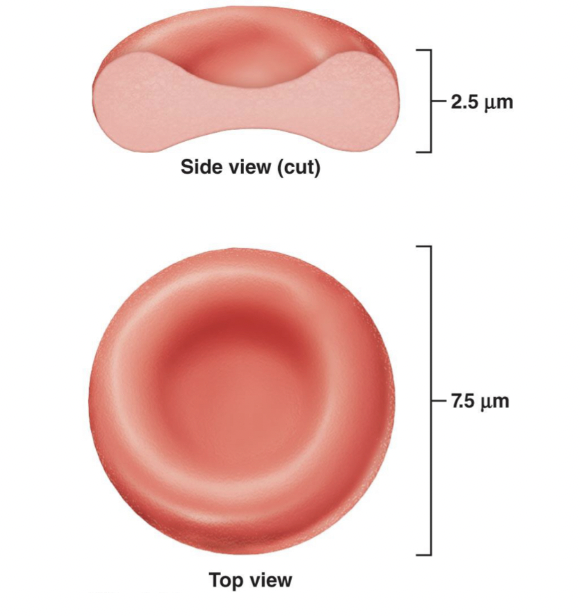
Erythrocytes
* Biconcave disc shape
* Contain plasma membrane but no nucleus (Allows red blood cells to be more squashy that is can fit in places squish and can get into places)
* The protein network maintains flexibility
* Biggest job is that they carry bags of hemoglobin which carries oxygen
* Contain plasma membrane but no nucleus (Allows red blood cells to be more squashy that is can fit in places squish and can get into places)
* The protein network maintains flexibility
* Biggest job is that they carry bags of hemoglobin which carries oxygen
51
New cards
Transport of Carbon Dioxide
* ***Dissolved in plasma (7-10%)***
* ***Bound to hemoglobin (20%)*** (Does not bind at the same location where oxygen binds, but will bind to the protein chains the acid globin chains on the hemoglobin molecule)
* To amino acid globin chains, not to heme
* ***Bicarbonate Ions (70%)***
* *HCO3****-***
* ***Bound to hemoglobin (20%)*** (Does not bind at the same location where oxygen binds, but will bind to the protein chains the acid globin chains on the hemoglobin molecule)
* To amino acid globin chains, not to heme
* ***Bicarbonate Ions (70%)***
* *HCO3****-***
52
New cards
Internal Respiration (Cellular Gas Exchange)
* Tissue is using oxygen in order to manufacture its primary energy source ATP
* Need oxygen for ATP
* Within the tissue youre going to have lower levels of oxygen compared to blood
* Will always have higher level of carbon dioxide when compared to blood
* As blood flows through the capillaries, oxygen is going to be delivered to the tissue which has lower oxygen levels and carbon dioxide and its going to be picked up where diffusion here, simple diffusion based on that concentration gradient
* External Respiration: Oxygen from within alveoli is being diffused into the bloodstream and is being delivered through the cardiovascular system to the tissue with hemoglobin
* Carbon dioxide will leave the tissue, go backwards via veins and eventually be exhausted out of the system
* Need oxygen for ATP
* Within the tissue youre going to have lower levels of oxygen compared to blood
* Will always have higher level of carbon dioxide when compared to blood
* As blood flows through the capillaries, oxygen is going to be delivered to the tissue which has lower oxygen levels and carbon dioxide and its going to be picked up where diffusion here, simple diffusion based on that concentration gradient
* External Respiration: Oxygen from within alveoli is being diffused into the bloodstream and is being delivered through the cardiovascular system to the tissue with hemoglobin
* Carbon dioxide will leave the tissue, go backwards via veins and eventually be exhausted out of the system
53
New cards
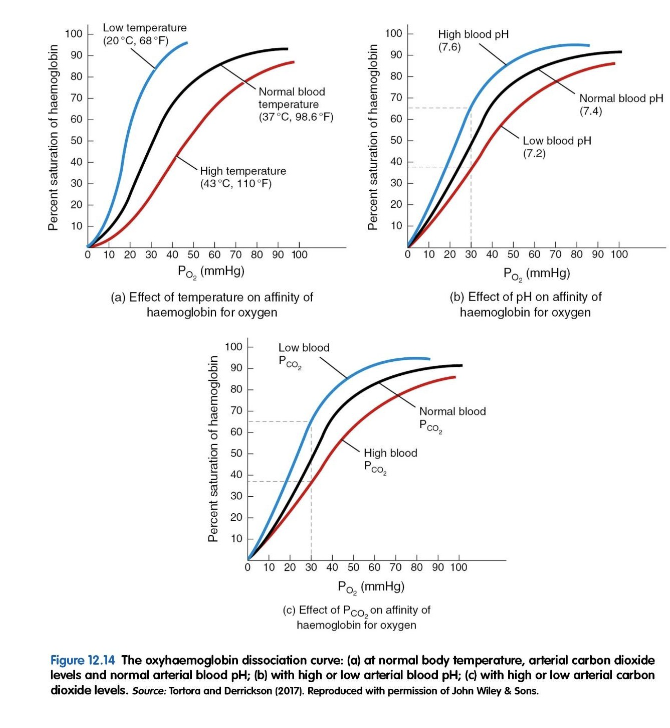
Internal Respiration (Cellular Gas Exchange Graph)
Just focus on the left picture on the top
* Oxygen dissociation curve:
* Showing the affinity of hemoglobin to oxygen
* Affinity: Ability or whether hemoglobin wants to hold on to that oxygen or release it
* Y axis: Percent saturation of hemoglobin, meaning that if were at 100%, hemoglobin is 100% saturated with oxygen
* No available binding sites
* Hemoglobin is filled with oxygen
* 0% means that all the oxygen has been given away, NO MORE oxygen on the hemoglobin
* X-Axis: Pressure of oxygen in the blood
* At the lungs, lots of oxygen and diffusing into the hemoglobin
* When you get down to the distal tissue (the very bottom corner on left side) given away all the oxygen, the oxygen is given away to the tissue
* Oxygen dissociation curve:
* Showing the affinity of hemoglobin to oxygen
* Affinity: Ability or whether hemoglobin wants to hold on to that oxygen or release it
* Y axis: Percent saturation of hemoglobin, meaning that if were at 100%, hemoglobin is 100% saturated with oxygen
* No available binding sites
* Hemoglobin is filled with oxygen
* 0% means that all the oxygen has been given away, NO MORE oxygen on the hemoglobin
* X-Axis: Pressure of oxygen in the blood
* At the lungs, lots of oxygen and diffusing into the hemoglobin
* When you get down to the distal tissue (the very bottom corner on left side) given away all the oxygen, the oxygen is given away to the tissue
54
New cards
Factors that will affect the affinity to hemoglobin
* Temperature
* pH (blood acidity)
* Carbon Dioxide
* Phosphates
* pH (blood acidity)
* Carbon Dioxide
* Phosphates
55
New cards
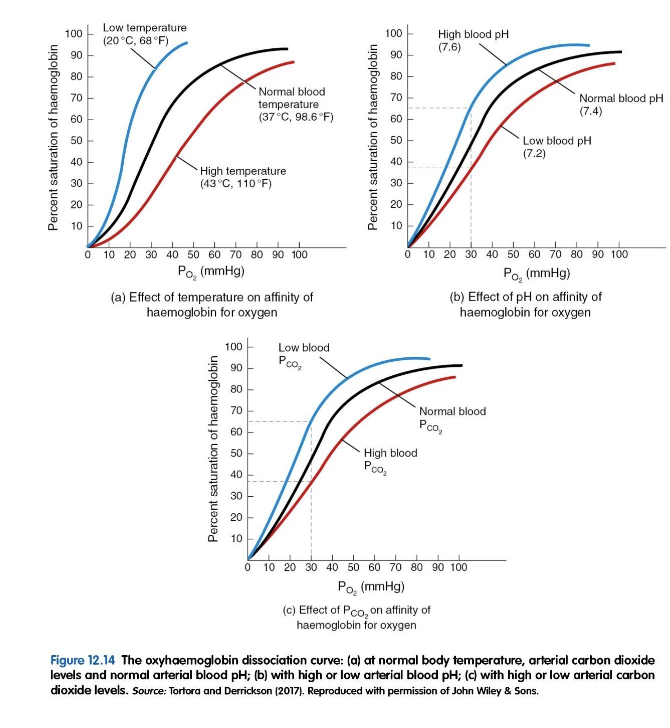
Black Curve of the Graph
* When you have higher temperature, the graph is shifted to the ***right,*** means that hemoglobin is more likely to give away oxygen
* The oxygen has less affinity to oxygen, so the tissues going to get the oxygen, hemoglobin is not going to hold on to the oxygen
* When you have lower temperature, the graph is shifted to the ***left,*** hemoglobin has a really high affinity to oxygen and wants to grab the oxygen, more oxygen in the hemoglobin, less in the tissue
* __**Low Temperature**__, high blood ph and low blood CO2 will increase the affinity of hemoglobin for oxygen (Hemoglobin wants to grab onto that oxygen)
* __**High Temperature**__ low blood ph, high blood CO2= Lower affinity
* The oxygen has less affinity to oxygen, so the tissues going to get the oxygen, hemoglobin is not going to hold on to the oxygen
* When you have lower temperature, the graph is shifted to the ***left,*** hemoglobin has a really high affinity to oxygen and wants to grab the oxygen, more oxygen in the hemoglobin, less in the tissue
* __**Low Temperature**__, high blood ph and low blood CO2 will increase the affinity of hemoglobin for oxygen (Hemoglobin wants to grab onto that oxygen)
* __**High Temperature**__ low blood ph, high blood CO2= Lower affinity
56
New cards
Respiration Summary
\