Arthritis - Therapeutics II
1/86
Earn XP
Description and Tags
Exam V
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
87 Terms
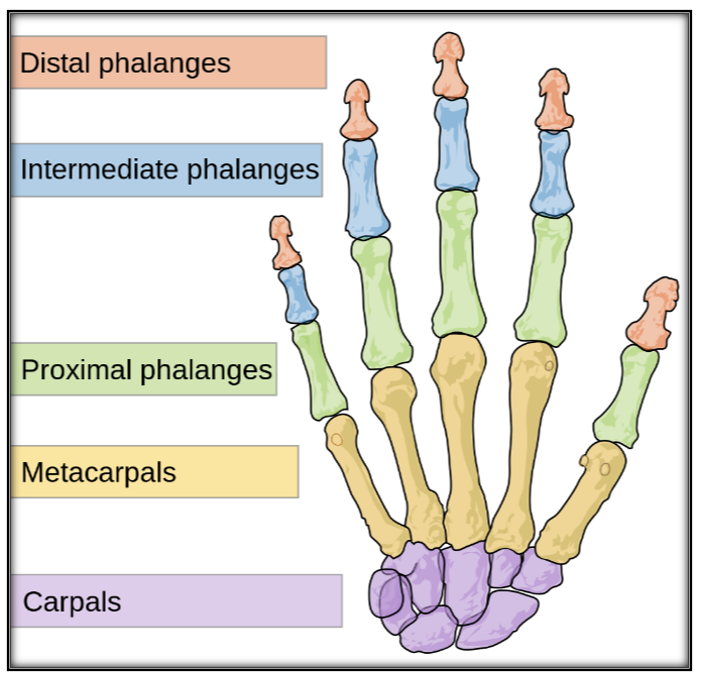
Where does RA vs OA effect the joints of the hand?
RA is more likely to affect the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints
OA is more likely to affect the distal interphalangeal (DIP) and Carbometacarpal phalangeal (CMC) joints.
Describe Systemic Lupus Erythmatosus
Heterogenous autoimmune disorder which can affect any organ system; disease course is characterized by remission and relapses. There are 4 types of lupus erythmatosus:
Systemic Lupus Eryhtematosus (Most common)
Discoid (skin)
Drug-induced
Combination
Describe Scleroderma
Autoimmune disease of connective tissue characterized by excessive collagen deposition in the skin and internal organs. Scleroderma presents as 2 distinct clinical entities:
Diffuse or Generalized form
Limited form called the CREST variant
Calcinosi
Raynaud’s phenomenon
Esophageal dysmotilities
Sclerodactyly
Telangiectasias
Define Seronegative Spondyloarthropathies
Spine disorders. Becuase there is an absence of rheumatoid factor (RF), these disorders are referred to as seronegative spondyloarthropathies
Define Ankylosing spondylitis
Inflammatory erosion of the sites where tendons and ligaments attach to bone which result in posterior fusion (ankylosing) of the spine. Ocassionally, large synovial joints (hips, knees, shoulders) may be involved. The underlying mech appears to be autoimmune.
Define Reactive Anthropathies
Sterile inflammatory joint disorders that are distant in time and place from the inciting infective process
Define Psoriatic arthritis
Heterogenous inflammatory arthritis associated with psoriasis. It is usually, but not always seronegative (RF negative). It may involve appendicular joints, axial joints, or both
Define Enteropathic arthritis
Arthritis assciated with inflammatory bowel disease (ulcerative colitis, chron’s)
Define Crystal-Induced Arthropathies
Metabolic bone and joint disorders which affect the joints; gout and pseudogout are common forms
Define Polymyalgia Rheumatica
Inflammatory condition of unknown origin characterized by aching and morning stiffness in the shoulders and pelvic areas
Describe Osteoarthritis. Where does it affect?
Degenerative Joint Disease—degeneration of cartilage that reflects failure of the chondrocyte to maintain proper balance between formation and destruction
Variable degrees of LOCAL inflammation; no systemic symptoms
Affects weight-bearing joints:
Pain
Limitation of movement
Disability
Decreased QOL
Describe the Pathophysiology of Osteoarthritis
Initial damage to articular cartilage
Increase in chondrocyte activity
Destruction of the major structural components of the articular cartilage
Degradation of Cartilage
Joint space narrowing
Osteophyte (new bone) at joint margins
Describe the Clinical Presentation of OA
Symptoms:
Joint pain, often asymemtrical
Joint stiffness at rest (<30min) which resolves with motion
Gel Phenomenon—thickening of synovial fluid when a joint is at rest for a prolonged period
Signs:
Crepitus — cracking of joints upon movement
Decreased range of motion
Joint enlargement
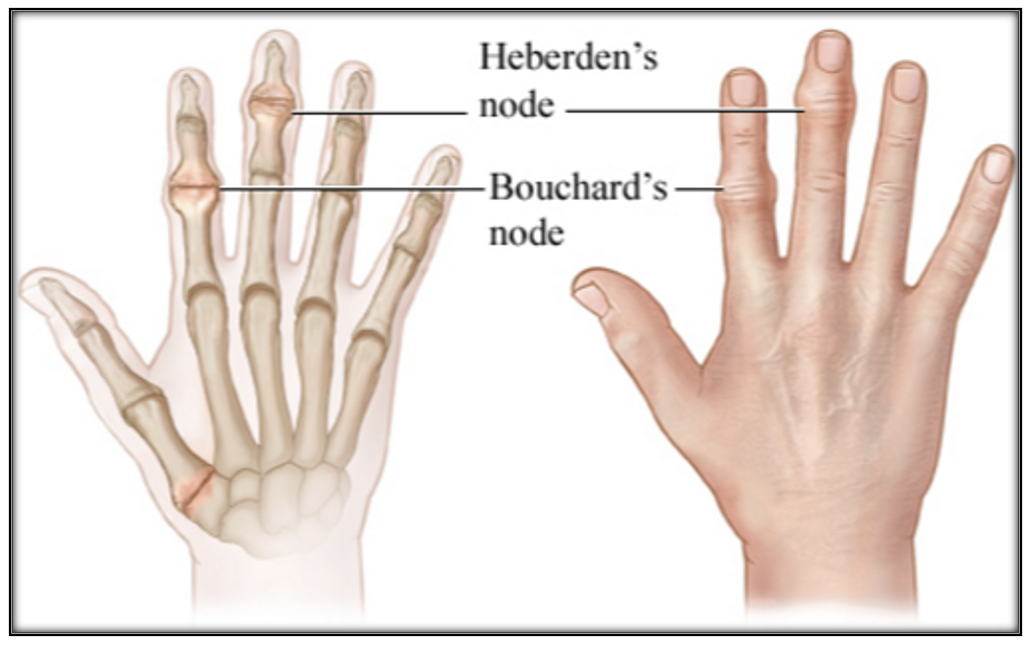
Heberden’s nodes
Bouchard’s nodes
Deformity (late stage)
List Joints involved in OA
Knees
Hips
Hands
Interphalangeal joints
First carpometacarpal joints
Spine
Lower lumbar spine
Cervical spine
How is Joint OA Diagnosed?
May be diagnosed confidently on clinical grounds alone if the following are present:
Persistent usage-related joint pain in one or few joints
Age ≥ 45years
Morning stiffness ≤30min
How is Hip OA Diagnosed?
Hip Pain + 2 of the following:
Erythrocyte sedimentation rate (ESR) <20mm/hour [inflammation]
Osteophytes on radiography
Joint space narrowing on radiography
How is Knee OA Diagnosed?
Knee pain, Osteophytes on Radiography, and at least on of the following:
Age > 50yo
Morning Stiffness < 30min
Crepitus
Bony enlargement or tenderness
Palpable warmth
Describe nonpharm therapy of OA
Education
Diet
Exercise
Land-based exercise
Aquatic exercise
Mind-body exercise (Tai Chi, yoga)
Cognitive behavioral therapy
Orthotics (Devices that support joint movement)
Surgery
Joint replacement
Arthrodesis
Osteotomy (removal of part of a bone)
When is Topical NSAID therapy preferred in OA?
Knee and Hand OA involving 2 or fewer joints
When is Oral NSAID therapy preferred in OA?
Hip OA, OA involving more than 2 joints, and/or those with inadequate response to topical therapy
How long should NSAID therapy be used before reassessment?
2-3 week trial is needed for both topical and systemic NSAIDs
What is the most common AE associated with Systemic NSAIDs
Gastroduodenal toxicity
Minor complaints are common and concomitant food or milk minimizes risk
Nausea, dyspepsia, anorexia, flatulence, diarrhea
Peptic ulcer disease is less common
What are risk factors for NSAID-induced Gastroduodenal toxicity?
History of an uncomplicated ulcer
Age > 65 years
High-dose NSAID
Concurrent use (1 point each)
Aspirin
Systemic corticosteroids
Anticoagulants
When should Standard-dose PPI therapy be started to prevent Gastroduodenal toxicity?
High Risk: complicated ulcer or ≥3 risk factors (Start PPI)
Moderate Risk: 2 risk factors (Start PPI)
Low risk: 0-1 risk factors (no need for PPI)
Describe H2RA use in prevention of Gastroduodenal toxicity?
They really only protect against NSAID-induced duodenal ulcers, but Gastric Ulcers are more common.
Describe Systemic NSAID Therapy Toxicity
Myocardial Infarction, cerebrovascular accident
COX-2 selectivity increases risk
Rofecoxib—clear risk, withdrawn from market
Celecoxib—evidence for risk with higher doses (>400mg/d)
Hemorrhage — increases with COX-1 selectivity
Fluid retention
Edema
Hypertension
Heart Failure
Describe risk factors for Kidney Toxicity with NSAID therapy
Intravascular volume depletion
Chronic kidney disease
Age > 65years
Concomitant nephrotoxins
ACE/ARB
TMP/SMX (Bactrim)
Loop diuretics
Aminoglycosides
Describe the use of Capsaicin in OA
Recommended for hand or knee OA involving 2 joints or less
Available for purchase without a prescription as a topical
AEs generally subside after repeated use
Burning, stinging, erythema at application site
Patient instructions
Must be used regularly (not PRN) (Applied 2-4x/d)
Takes 2wks to work
Wash hands after application
Describe the use of Duloxetine (Cymbalta) in OA
SNRI
Only recommended for Knee OA
Reduction in pain occurs 4 weeks after initiation
Preferred if neuropathic pain and/or depression also present
AEs:
Nausea
Vomiting
Constipation
List the Intraarticular Corticosteroids. Describe their therapy.
Triamcinolone Acetonide or ER
Methylprednisolone acetate
Pharmacokinetics
Onset of relief: 24-72h
Peak effects: 1 week
Duration: 4-8 weeks
Limit injections to 4 times per year to minimize AEs
Joint infection
Osteonecrosis
Tendon rupture
Describe Glucosamine and Chondroitin Therapy in OA
Dietary Supplements
May take 3 months for effects
Precautions:
Glucosamine sulfate salt: cross-sensitivity is unknown
Chondroitin is derived from shark and bovine cartilage
Shellfish allergies
Well tolerated; few AEs
Describe APAP therapy in OA
Not really clinically beneficial
Considered for short-term, episodic therapy for those with limited pharmacologic options due to intolerance or C/I
Should be scheduled, not PRN
Hepatotoxicity is the more significant SE
Interacts with Warfarin when taken for >14d
Describe Trolamine Salicylate therapy in OA
Topical rubefacient available for purchase without a prescription
May help with hand OA, but it’s questionable
Decribe Hyaluronic Acid therapy in OA
Hyaluronate is a naturally occuring component of the cartilage and is responsible for the properties of synovial fluid which enable it to act as a lubricant and shock absorber
This form of therapy is therefore referred to as viscosupplementation
May be beneficial for knee OA in patients who have not responded to other therapies, but the American College of Rheumatology do not recommend the use of intra-articular acid injections for knee OA pain
Expensive
Describe the use of Opioid Agonists in OA
Several studies of paitents with knee OA have found the efficacy of opioids to be similar to systemic NSAIDs
Indicated when other therapies are exhausted
May consider joint replacement over chronic opioid usage
Tramadol is a commonly used opioid for OA
Describe the progression of pharmacotherapy for Knee OA
Mild:
Topical NSAID or Capsaicin
Moderate-to-Severe:
Topical NSAID
Systemic NSAID
Duloxetine
Intraarticular glucocorticoid injection
Describe Hip OA pharmacotherapy
Systemic NSAID
Intraarticular injection — reserved for paitents with moderate-to-severe pain when short-term relief is desired and there are contraindicateions to or failure of other treatments
Topical therapies are not used to manage hip OA
Duloxetine has not been studied in hip OA
Describe Hand OA Pharmacotherapy
Topical: NSAID/Capsaicin
Systemic NSAID: reserved for patients who do not respond to topical therapy or have OA at more than 2 sites
Describe the Pathophysiology of Rheumatoid Arthritis
Inflammation of synovium tissue results in tissue proliferation (Pannus)
Autoantibodies may be detected before clinical disease is present
Rheumatoid Factor (RF)
Anti-citrullinated protein antibody (ACPA)
Inflammatory changes cause loss of cartilage, formation of chronic granulation or scar tissue, and/or tendon deformity
Describe the Clinical Presentation of RA
Symptoms:
Symmetrical joint pain and stiffness (>30 min)
Constitutional
Fatigue
Anorexia
Loss of Appetite
Low-grade fever
Signs
Joint tenderness, erythema, swelling (soft/spongy)
Rheumatoid nodules
Joint subluxation/deformity
Describe the use of EULAR diagnostic Criteria
A score of 6 or higher indicates definite RA — higher the score, the worse it is
Anti-citrullinated protein antibody (ACPA): highly specific and detectable early in disease
Describe the Diagnosis of RA (Aside fro EULAR)
Radiography helps to establish the extent of cartilage destruction and bone errosion, monitor impact of medications, and to determine if therapt needs to be escalated
Radiographic findings
Soft tissue swelling
Osteoporosis near the joint
Erosions (Occur late in the disease)
Describe the Joint Involvement in RA
Usually symetrical and polyarticular
Small joints of the hand, wrist, and feet are most frequently involved
Elbows, shoulders, hips, knees, and ankles are also common but to a lesser extent
Spine involvement usually occurs in the cervical vertebrae
Lumbar spine involvement is rare
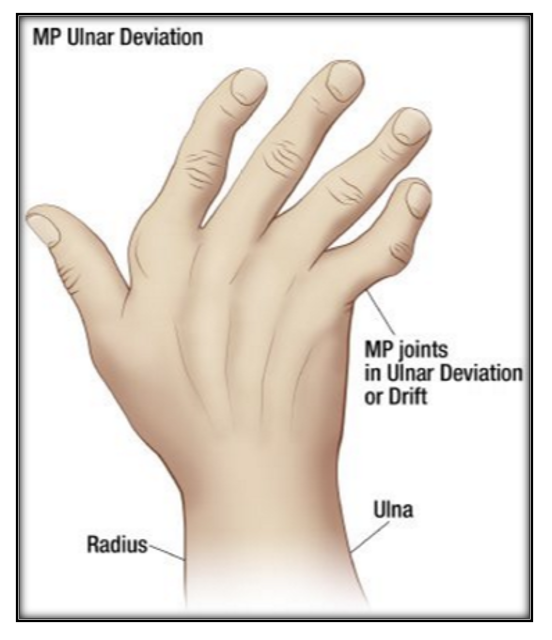
Describe Ulnar Deviation
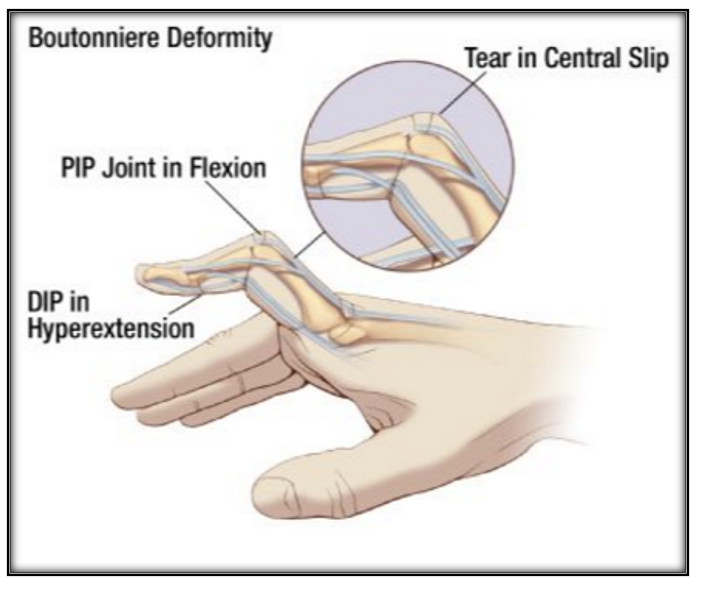
Describe Boutonniere Deformity
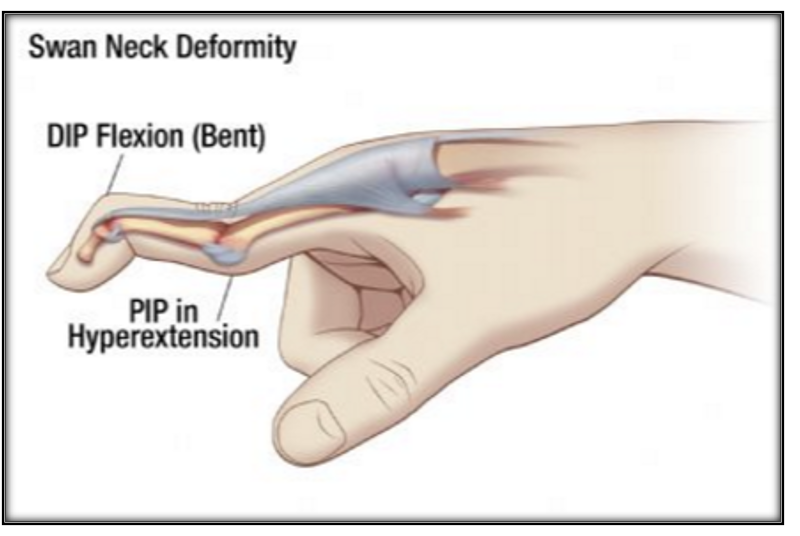
Describe Swan Neck Deformity
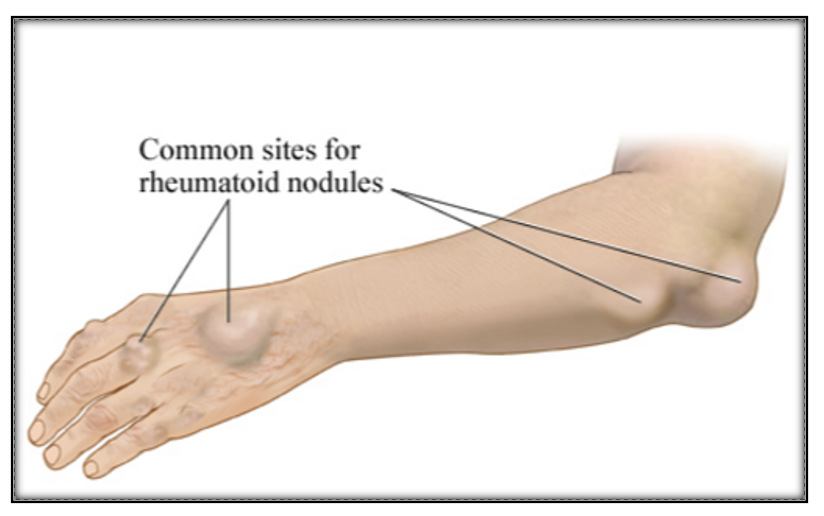
Describe Rheumatoid Nodules
Describe Extravascular Involvement in RA
Systemic disease and other organ systems are involved in about 40% of patients with RA
Extraarticular involvement is associated with release of inflammatory cytokines from the synovium
Extraarticular disease is a marker of disease severity and is associated with increased overall morbidity and premature mortality when compared with those with RA without extraarticular disease
What are some Nonpharm therapies for RA?
Rest
Physical and occupational therapy
Orthotic devices
Weight loss
Surgery
What three classes of Drugs are considered for RA therapy?
csDMARD (Conventional Synthetic)
bDMARD (Biologic)
tsDMARD (Targeted Synthetic)
List the csDMARD drugs discussed in class
Methotrexate
Leflunomide
Hydroxychloroquine
Sulfasalazine
List the bDMARDs discussed in class
TNF-𝛼 antagonists
Etanercept
Infliximab
Adalimumab
Golimumab
Certolizumab
Rituximab
IL-6 Receptor Antagonists
Sarilumab
Tocilizumab
List the tsDMARDs discussed in class
Tofacitinib
Baracitinib
Upadacitinib
Describe the use of Methotrexate in RA
csDMARD — First-line therapy
Usual dose: 7.5-15mg PO/SC/IM once weekly (25mg max)
Onset of symtpom relief occurs 2-3 weeks after initiation
Max benefit seen in 6 months
Oral absorption decreases with increasing doses
Describe the AEs of Methotrexate
GI distress
Bone marrow suppression
Pulmonary (fibrosis, pneumonitis) — rare
Hepatitis — cirrhosis is rare
Photosensitivity
Folic acid deficiency
List contraindications to Methotrexate
Pregnant or contemplating pregnancy
Kidney disease (eGFR <30mL/min/1.73m²)
Liver disease or alcohol use disorder
Bone marrow suppression
Leukopenia (WBC <1000/mm³)
Thrombocytopenia (Platelet count < 75,000/mm³)
Describe the use of Leflunomode in RA
csDMARD
Onset of symptom relief occurs within 1 month after a loading dose
Pharmacokinetics
Long elim t½ → metabolized into an active metabolite
Enterohepatic circulation—cholesteyramine, an anion exchange resin, may be used to clear leflunomide more rapidly — for those who need to be off quickly
List AEs of Leflunomide
GI distress
Hepatitis
Bone Marrow Suppression
Alopecia
Describe the use of Hydroxychloroquine in RA
csDMARD
Studies have demonstrated efficacy in Milder RA, but it does not slow radiographic progression
Onset of symptom relief is delayed up to 6 weeks
Should not be considered failed until 6 months w/o response
Advantages:
May be used in pregnancy
No hepatic, kidney, or bone marrow toxicity
Describe the AEs of Hydroxychloroquine
GI distress
Ocular toxicities
Accommodation defects
Scotomas
Corneal deposits
Increased skin pigmentation
Alopecia
Describe the use of Sulfasalazine in RA
csDMARD
Onset of symptom relief within 2 months (longest)
Metabolized to its active components by colonic bacteria (beneficial for IBS)
Sulfapyridine—antirheumatic activity
5-aminosalicylic acid
Describe AEs of Sulfasalazine
GI distress
Severe dermatologic reactions
Yellow-orange skin/urine discoloration (benign)
Leukopenia
Hepatitis
Drug interactions with Sulfasalazine
Antibiotics can destroy the colonic flora responsible for cleaving the prodrug, thus decreasing the absorption and effectiveness of sulfasalazine
Iron supplements bind with sulfasalazine which decreases absoprtion
Sulfasalazine may displace warfarin from protein-binding sites, thus potentiating the anticoagulant effects of warfarin
In bDMARD therapy, what are the three types of therapeutic molecules?
Soluble receptor antagonists: truncated froms of the cell surface that are devoid of the transmembrane and intracytoplasmic domains; bind their target cytokine while it is in the serum, theraby inhibiting the cytokine’s ability to interact with its cell surface receptor
Monoclonal Antibodies: typically consist of the Fc portion of human IgG1 and chimeric, humanized, or fully human Fab fragments
Cell surface receptor antagonists: biologically inactive proteins that compare for binding to the cytokine’s membrane receptors
What are some safety issues with bDARDS?
Infection risk
Tuberculin skin test at baseline
HBV evaluation
Vaccinations
Avoid live vaccines
Malignancy
Injection site rxn
Infusion-related reactions (for IV dosage forms)
Anti-drug antibody formation (immunogenicity)
Do not combine bDMARD medications
Describe the use of TNF-𝛼 Inhibitors in RA
May be combined with csDMARDs
Less radiographic progression than oral DMARD alone
Variable symptom relief onset
Infliximab: 3-7 days
Adalimumab: 3 months
Heart Failure: avoid TNF-𝛼 inhibitors becayse they are associated with worsening or development of heart failure
Which TNF-𝛼 Inhibitors can be concomitantly used with Methotrexate?
Infliximab and Golimumab
“I Go with Methotrexate”
Describe the use of Rituximab in RA
Monoclonal antibody directed against the CD20 antigen on the surface of B-lymphocytes
Onset of symptom relief within 2 weeks
AEs:
Hepatitis
Neutropenia or thrombocytopenia
GI perforation
Hypertension
Hyperlipidemia
Describe the use of IL-6 Inhibitors in RA
bDMARDS
Sarilumab and Tocilizumab are monoclonal antibodies which antagonize IL-6 recptors
AEs:
Hepatitis
Neutropenia
Thrombocytopenia
Hyperlipidemia
GI perforation
Describe the use of Janus Kinase Inhibitors in RA
tsDMARDS
SHOULD NOT BE USED WITH bDMARDs due to an increased risk for infection and/or malignancy
Available as an oral dosage form
They may be given with or without methotrexate
List the Janus Kinase Inhibitors and their clinical notes
Tofacitinib
Dose adjustment in renal impairment, hepatic impairment, potent 3A4 inhibitors, moderate 3A4 inhibitors of 3A4 and 2C9
Baricitinib
Dose adjustment in renal impairment
Upadacitinib
No notes
Describe the AEs of Janus Kinase Inhibitors
Infection
Malignancy
Venous thromboembolism
Neutropenia
Anemia
Hyperlipidemia
Decribe dosing methods of Corticosteroids in RA
Bridging Therapy: symptom relief before the onset of DMARD
High-dose Burst: use to control acute disease flares
Continuous low-dose: used for maintenance therapy
Describe parenteral admin of Corticosteroids in RA
IM provides 2-6 weeks of relief but associated with systemic AEs
Intraarticular has fewer systemic effects; useful when small number of joints affected
Intravenous is reserved for severe, refractory symptoms.
Describe NSAID therapy in RA
Does not modify the disease
Only used during DMARD initiation and as needed for breakthrough pain
____________ should be started as soon as the diagnosis of RA is established
DMARD therapy
Treatment should be aimed at reaching a target of _____________________ in every patient
sustained remission or low disease activity
Monitoring should be frequent in active disease (every ____ months); if there is no improvement in disease activity by at most ___ months after the start of treatment or the target has not been reached by ____ months, therapy should be adjusted
1-3; 3; 6
______________ should be part of the first treatment strategy
Methotrexate
In patients with a contraindication to Methotrexate, ___________ or ___________ should be considered as part of the first treatment strategy
Leflunomide; Sulfasalazine
Short-term ____________ should be considered when initiating or changing csDMARDs. They should be _______ when low disease activity is achieved.
Glucocorticoids; tapered
If the treatment target is not achieved with the first csDMARD strategy, in the absence of poor prognostic factors, ____________ should be considered
other csDMARDs
If the treatment target is not achieved with the first csDMARD strategy, when poor prognostic factors are present, ____________ should be added
a bDMARD or a tsDMARD
bDMARD or tsDMARD should be combined with a _________; in patients who cannot, __________ and tsDMARDS may have some advantages compared with other bDMARDS
csDMARD; IL-6 pathway inhibitors
If a bDMARD or tsDMARD has failed, treatment with another _________________ should be considered; if one ___ inhibitor therapy has failed, patients may receive an agent with another mode of action or a second ___ inhibitor
bDMARD or a tsDMARD; TNF; TNF
If a patient is in persistent remission after having tapered glucocorticoids, one can consider tapering ________________, especially if this treatment is combined with a csDMARD
bDMARD or tsDMARD
If a patient is in _______________, tapering the csDMARD could be considered
persistent Remission