MOOD or AFFECTIVE DISORDERS AND SUICIDE
1/4
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
5 Terms
🧠 Mood vs. Affect & Mood Disorders
🧠 Mood vs. Affect & Mood Disorders
Internal, sustained emotional state
Describes how a person feels
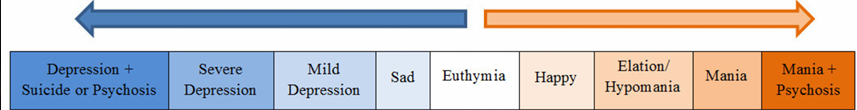
Exists on a continuum (e.g., happy ↔ depressed)
Affect
Outward expression of mood (verbal/nonverbal)
Describes how the person shows their feelings
Examples
Happy Mood
😊 Affect: Smiling, active, well-groomed, cooperative, creative
Depressed Mood😔 Affect: Gloomy, inactive, neglectful, flat, unmotivated, withdrawn
Mood Continuum
Euthymic Mood – Normal, appropriate mood responses
Dysthymic Mood – Mild but chronic depression
Disruptive Mood Dysregulation Disorder (DMDD) – Persistent irritability with temper outbursts (starts before age 10)
Cyclothymia – Mild ups and downs (hypomania ↔ mild depression), no major social/work impairment
Seasonal Affective Disorder (SAD) – Depression during fall/winter; ↑ sleep, appetite, carb cravings
Postpartum Mood Disorders
Blues: Common, mild
Depression: Treated with IV brexanolone
Psychosis: Severe, needs urgent care
Premenstrual Dysphoric Disorder (PMDD)
Severe mood symptoms before menstruation: irritability, anxiety, overwhelm, resolves after period
Key Notes
Mood disorders = exaggerated, prolonged emotional states
More common in women
Linked to high socioeconomic status
Impacts social, physical, and psychological functioning
Depression Overview
Depression Overview
Types of Depression:
Transient Depression: Normal reaction to loss (e.g., death, disappointment); self-limiting.
Reactive Depression: Sadness linked to specific events; relieved when circumstances change.
Major Depression (Unipolar): Persistent sadness, loss of interest, impaired social/occupational function, often with anxiety and substance abuse.
Pathophysiology & Etiology:
Neurotransmitters: Imbalance in serotonin, norepinephrine (NE), and dopamine.
Serotonin: Linked to sadness, obsession, and compulsions.
NE: Causes psychomotor retardation and anxiety.
Dopamine: Affects pleasure and causes guilt, low self-worth.
Neuroendocrine Imbalance: Altered hormone levels from pituitary, thyroid, and adrenal glands, affecting mood.
Genetics: Higher risk in those with family history (3x higher in relatives).
Environmental Factors: Major life losses, chronic illness, violence, and abuse increase risk.
Signs & Symptoms (SADIMAGES):
S: Sad mood
A: Appetite changes
D: Disturbed sleep
I: Inability to concentrate
M: Marked decrease in pleasure
A: Apathy (lack of interest in activities, sex)
G: Guilt feelings
E: Energy changes
S: Suicidal thoughts
Grief vs Depression:
Grief: Self-limiting, linked to real loss, improves with time.
Depression: Can occur without identifiable loss, increases in severity without intervention.
Diagnosis (DSM-V Criteria):
At least 5 symptoms in 2-week period, including depressed mood or loss of interest, with weight changes, psychomotor retardation, fatigue, guilt, poor concentration, and thoughts of death or suicide.
Subtypes:
Post-Partum, Atypical, Melancholic, Dysthymia
Suicidal Client Assessment and Intervention
Suicidal Client Assessment and Intervention
Risk Factors for Suicide:
Demographics: Male (3x higher success rate), ages 15-24 or above 45, separated/divorced individuals, alcoholics, and those with lack of social support or terminal illnesses.
Psychiatric History: Depression, history of prior attempts, and ambivalence about life.
Types of Suicidal Ideation:
Active Suicidal Ideation: Thoughts of suicide with plans.
Passive Suicidal Ideation: Wish to be dead, but no plans to end life.
Myths vs. Facts:
Myth: "People who talk about suicide never commit suicide."
Fact: Suicidal individuals often give subtle or direct cues; threats should always be taken seriously.
Myth: "Suicidal people only want to hurt themselves."
Fact: Suicidal behavior may involve directed anger and ambivalence; intervention can help redirect destructive thoughts.
Client Statements & Nurse Responses:
Example Statements:
"I just want to go to sleep and not think anymore."
"It will just be the end of the story."
Nurse's Response:
"Do you mean you want to die?"
"Are you planning to end your life?"
Behavioral Clues:
Giving away possessions, writing a suicide note, making funeral arrangements, and buying items for self-harm (e.g., pills, gun).
Suicide Triad: Loss of spouse, job, or feeling alone.
Assessment Tools:
Beck Depression Inventory: Self-assessment tool.
Hamilton Rating Scale: Assesses severity of depression and response to treatment.
Risk Levels:
High Lethality Methods: Hanging, shooting, jumping from heights.
Low Lethality Methods: Overdose, wrist cutting.
Key Considerations:
Always take threats and verbal cues seriously.
Assess for suicidal plans and feasibility to gauge risk.
Ambivalence: Suicidal individuals often prefer life over death if they feel hope.
Intervention: Immediate help and support to resolve the suicidal crisis, focusing on situational factors.
Major Depression Nursing Management
Major Depression Nursing Management
Nursing Diagnoses & Interventions
Risk for Suicide
Close observation (1:1 or checks every 10-15 minutes)
Place near nurse’s station; no single rooms
Accompany to off-ward activities
Remove hazardous items
Use an authoritative role, safe environment, and no-suicide contract
Complicated Grieving
Encourage verbalization of feelings
Acknowledge grief stages (guilt, anger, etc.)
Nurse-Patient Relationship
Depressed patients often have low self-esteem
Develop meaningful relationships based on empathy
Avoid reinforcing delusions or hallucinations
Encourage completion of ADLs and emotional expression
Common Nursing Diagnoses for Depressed Clients
Imbalanced Nutrition: Less than body requirements
Disturbed Sleep Pattern
Risk for Suicide
Social Isolation
Low Self-Esteem
Complicated Grieving
Electroconvulsive Therapy (ECT)
Stimulates brain chemistry to correct depression
Indications: major depression, unresponsive schizophrenia
Contraindications: MI, pacemaker, glaucoma, severe osteoporosis
Pre-ECT: NPO 6-8 hours, secure consent, prepare equipment
Post-ECT: Re-orient, monitor vital signs, watch for memory loss or fractures
Medications & Treatment
Antidepressants: SSRIs (e.g., Fluoxetine, Sertraline), SNRIs (e.g., Venlafaxine), TCAs, MAOIs
ECT: Usually 6-15 sessions for sustained improvement
Risk for Suicide: Monitor during early antidepressant treatment
Psychotherapy
Cognitive Behavioral Therapy: Addresses negative thinking patterns
Interpersonal Therapy: Resolves role-related conflicts
Drug Alerts & Side Effects
SSRIs: Milder side effects, quick onset
TCAs: Risk of overdose, severe side effects
MAOIs: Hypertensive crisis with tyramine-rich foods
Key Reminder:
Always monitor suicidal ideation closely in the first weeks of antidepressant therapy.
Summary
Depression:
D – Dahan-dahan (hypoactive)
E – Evasive
P – Puyat
R – Recurrent headaches
E – Eating habits compromised
S – Stressed
S – Suicidal
I – Irritable
O – Cry/sad
N – Nu po un?
Nursing Diagnosis (Depression):
Nutrition, Less than body requirement – Small frequent feeding, Assist in eating.
Risk for injury (self) – SUICIDAL
Use direct and clarify responses.
No HARM CONTRACT.
No curtains, linens, belts, shoelaces, sharps.
1:1 supervision.
History!! (planned) risk.
Impaired Social Interaction
Gradual involvement in activities.
Initially – prepare and assist (1-3 days), then gradually allow independent decision-making.
Antidepressants:
TCA (Tricyclic Antidepressant)
Most sedative (also for panic).
May cause cardiac arrhythmias.
SSRI (Selective Serotonin-norepinephrine Reuptake Inhibitors)
Safest and latest drug.
Physician’s choice.
MAOI (Monoamine Oxidase Inhibitors)
Most effective but with more side effects.
PA – Parnate
NA – Nardil
MA – Marplan/Mannerix
Antidepressant Timeline:
1–2 weeks:
Initial – sedation (antukin).
Depressed pa rin.
2-4 weeks:
Positive/therapeutic response: Initiation of self-care, participation in activities.
Monitor “suicidal risk.”
MAOIs:
Avoid Tyramine-rich foods to prevent hypertensive crisis.
Signs/Symptoms of hypertensive crisis:
Increased BP
Occipital headache
Blurring of vision